Abstract
The incidence of prospective organ donors in the United States and the techniques which are to used to guarantee their optimal use after identification are analyzed. Attitudes of the public and health professionals toward organ donation are discussed.
The organization of the Pittsburgh Organ Procurement Agency and its relationship to other such agencies is described.
Finally, the presently used techniques of liver salvaging and preservation are outlined.
The availability of sufficient numbers of physiologically optimal postmortem donor livers is a major factor contributing to the success of orthotopic liver transplantation. Herein, we report the development of the liver procurement program at the University of Pittsburgh and discuss the factors perceived as important in the development of a greater liver procurement capability.
Liver transplantation was inaugurated at the University of Pittsburgh Health Center in February, 1981, when the program, formerly located at the University of Colorado, was transferred to Pittsburgh. During the first year in Pittsburgh, the number of liver transplants performed (30 grafts in 26 recipients) was 25% greater than the number transplanted during the most active year of the Denver program. The following year (1982), there was a 270% increase in the number of livers transplanted (80 grafts in 63 recipients) over that of the previous year.
The availability of suitable donor organs has not been the single variable which has most limited the number of transplants performed in any given year. The availability of suitable donor livers however, is a major factor which has influenced the number of transplants performed. The supply of acceptable donor livers is dependent upon a number of identifiable variables, some of which are susceptible to change such that the absolute number of such organs can be optimized. These include the incidence of potential postmortem donors; the attitudes of the public and health professionals toward organ donation; the organization and effectiveness of organ procurement programs; the development of intercenter collaboration, particularly with procurement programs not previously or potentially interested in liver procurement; and finally, the temporal limitations inherent in current techniques for successful ex vivo liver preservation.
Identification and Incidence of Potential Donors
Postmortem liver donors are characteristically patients between 2 months and 45 years of age who are victims of brain injuries which eventuate in brain death. In such donors, cardiovascular and respiratory functions are sustained artificially with mechanical ventilation, and death is pronounced on the basis of documented cessation of integrated brain function. The recovery of livers and other vital organs from heartbeating cadavers minimizes the ischemia which occurs at normal body temperature in such organs and thereby contributes importantly to graft success. In addition, acceptable donors should have no present or past history of hepatobiliary or systemic disease which might comprise graft function in the recipient. Obviously, the absence of any traumatic, ischemic, or infectious complication involving the liver are factors which determine donor candidacy. Thus, donor SGPT, total and direct bilirubin levels, prothrombin time, and partial thromboplastin time should be within normal limits at the time of donation. Moreover, prolonged periods of donor hypotension and hypoxia prior to death are factors which contraindicate donation. Therefore hypotension occurring in potential donors should be treated aggressively with volume expansion. Vasoconstricting pressor agents, however, should be avoided as they may contribute to liver ischemia in the absence of systemic hypotension. If a pressor agent is needed, despite adequate hydration and volume expansion, dopamine is the preferred agent. Even when this agent has been the only such agent used, we have found empirically that dopamine infusions at a rate greater than 10 mcg per kilo per min appear to be injurious to the donor liver and should be avoided if at all possible. Similarly, in order to ensure graft function following transplantation, the donor hematocrit should be maintained above 30%, and transfusions with blood or packed cells should be used to maintain this level despite imminent or declared donor death.
No data is available concerning the number of potential liver donors available in the United States or elsewhere. Several studies concerning the potential availability of postmortem renal donors in the United States have been reported. These studies provide some information which is relevant to liver donation because the criteria commonly used for screening potential liver and kidney donors are similar in many ways. They suggest that from 0.77 to 3.5% of patients expiring in hospitals within the United States succumb to brain death and are within the acceptable age range, and do not have other problems which would contradict organ donation (1-3). The 5-fold variation in estimates cited is in large measure explained by the differences in criteria used by the different investigators to screen prospective donors. For example, some programs consider patients up to the age of 65 years as potential donors, while others would not. Limiting liver donation to donors under the age of 45 significantly reduces the number of potential donors toward the lower figure cited above. Despite this relatively lower figure, it should be remembered that there are approximately 1 million hospital deaths each year in this country and because the potential number of postmortem liver donors is probably no more than 2% of this number, thus 20,000 donors annually are potentially available and, therefore, donor availability should not limit organ transplantations, should active steps be made to recruit all potential donors. A recent report by the American Medical Association confirms this donor estimate (4).
Despite the active growth of organ transplant programs in recent years, the number of postmortem donors in this country has remained relatively stable. The best estimates concerning the number of potential donors is based on the number of cadaveric kidney transplants performed each year plus approximately 25% of that number which represents donor kidneys discarded due to surgical error, anomalous blood vessels, contamination, etc., during their harvesting. This sum, divided by two, provides the best and probably most conservative estimate of the number of donors presently being used. These calculations indicate that in the United States there are approximately 2,200 postmortem donors from whom kidneys and other vital organs are recovered anually. In other words, these figures suggest that organs are now being recovered from fewer than 1 of every 8 to 10 potential donors. This is clearly an indictment of the present donor identification process and suggests that steps should be taken to improve it.
Attitudes of the Public and Health Professionals toward Organ Donation
The shortage of postmortem organ donors is not due to the American public's unwillingness to donate. Public opinion polls have indicated that at least 70% of the adult public are willing to donate kidneys for renal transplantation (5, 6). Although it initially was found that many families willing to donate kidneys were not amenable to liver donation, the recent widespread media attention given to hepatic transplantation during the past 2 years has largely overcome this problem. More recent experience suggests that families which are willing to donate kidneys are generally also willing to donate the liver, if they are offered the option.
Not surprisingly, grief-stricken families do not spontaneously think to volunteer organ donation. Data from the Pittsburgh organ procurement program suggest that less than 5% of organ donations result from family-initiated requests to donate. However, 8 of 10 (82%) of the families offered a chance to donate decided favorably to do so. These data suggest that of the approximately 20,000 potential postmortem donors from whom kidneys and other vital organs are recovered annually in the United States, fewer than 1 in 10 is actually being recovered and that of the remaining 18,000 as many as 14,400 more could be obtained, were families offered the opportunity to donate.
Thus, the present relative shortage of postmortem organ donors is not due to the American public's unwillingness to donate. Instead, the discrepancy between the number of potential donors and the number of actual donors available nationally is probably due to the fact that organ donation is often not offered to families of patients succumbing to brain death. Although it is not often done, it is the responsibility of the primary physician in each case to have the next of kin informed of donation opportunities (7-9). Medico-legal fears, unfamiliarity with the donation process, unwillingness to assume additional responsibilities, and forgetfulness are the major impediments to be overcome in securing more cooperation from primary care physicians charged with this responsibility.
Organization of the Liver Procurement Program
Aggressive education of both primary care and hospital-based physicians concerning the criteria for brain death, the need for organs for transplantation, and the methods for obtaining next-of-kin consent for organ donation are the essential and immediate goals of all organ procurement programs. Mere information giving, however, is often not sufficient. Service must be provided to the physician and to the hospital where the donor is located which will serve to facilitate the donation process and minimize the additional work required of the referring clinician and hospital. Thus, around-the-clock availability of personnel trained to coordinate the donation process between the donor hospital physicians and families, and the availability of transplant surgeons capable of removing and preserving donor organs at distant sites and at times not likely to disrupt hospital schedules, will lessen the time and effort required of others, will reduce the disruption of normal hospital routines, and will enhance the referring physicians' willingness to identify prospective donors. Empiric experience suggests that both the educational and service functions of an organ procurement program can be most effectively discharged through an organized organ procurement agency staffed full time by trained procurement coordinators under the direction of surgeons affiliated with a transplant center.
The Transplant Foundation at the University of Pittsburgh was established in 1978. It was founded in an effort to educate and recruit the physicians practicing in the approximately 90 hospitals in the three-state area surrounding greater Pittsburgh about renal transplantation and the need for kidney donations. With the subsequent establishment of the cardiac (1980) and liver transplantation (1981) programs at the University of Pittsburgh, the Transplant Foundation has assumed the additional responsibility of the organ procurement for these programs as well. The Foundation has been responsible for increasing the number of organ donors from 11 in 1977 to over 50 in 1982. Figure 1 summarizes the growth of this program.
Fig. 1.
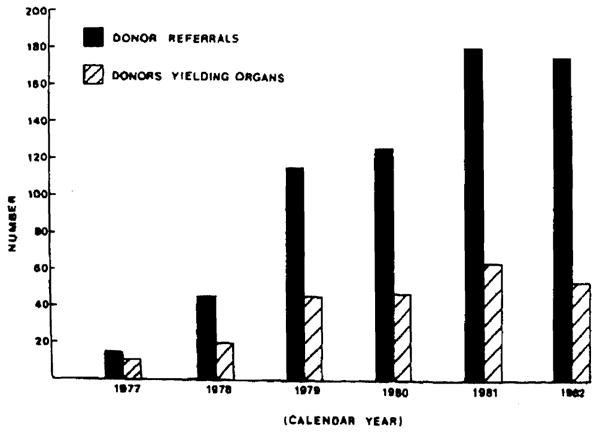
Annual number of donor referrals to the Pittsburgh OPA and number of such donors yielding organs for transplantation during the period from 1977 through 1982.
Although every effort is made to recover and transplant all organs donated, not all donors in our region provide livers for transplantation. The reasons for this are numerous. In some instances, the donor has experienced prolonged hypotension, and the resultant ischemic injury suffered by the organs has prohibited their use. In some such cases, the kidneys will be transplanted anyway because of the availability of posttransplant dialysis which can be used to sustain the recipient until the acute renal injury has reversed. Unfortunately, no such alternative is available for liver recipients and, therefore, the liver cannot be transplanted in such cases. A second factor is that kidneys are accepted from older donors (<55 years) more than are livers (<45 years). In addition, in liver transplantation, compatibility between donor and recipient size and blood group is essential Thus, many otherwise suitable donors are declined for hepatic donation because of incompatibility of any one or more of these three factors with the available pool of liver recipients. In contrast, these factors are seldom considered for renal donation because of the large pool of potential kidney recipients waiting for organs (over 6,000 nationally).
Finally, the simultaneous retrieval of donor pancreas and liver is not possible because of anatomical and vascular considerations. Therefore, the use of one such organ from a donor prohibits use of the other organ. Recently, we have performed two pancreas transplants and, in both instances, it was necessary to decline the opportunity to recover the donor's liver. Figure 2 reveals the number of livers recovered from donors within our region frum January, 1981 through December, 1982.
Fig. 2.
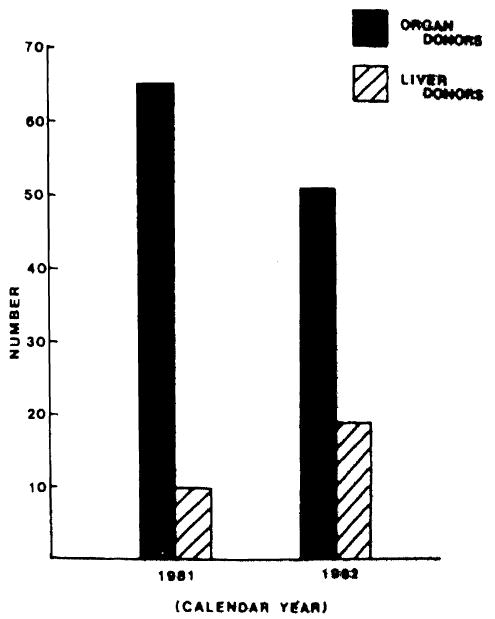
Number of organ donors identified during 1981 and 1982 by the Pittsburgh Organ Procurement Agency contracted with the numbers of such donors yielding liver for transplantation
Finally, hepatic donation from local donors is declined when the Pittsburgh facilities for liver recipient care are saturated.
Intercenter Collaboration in Liver Procurement
Patients accepted for liver transplantation are frequently moribund and subject to progressive debilitation during their terminal course. In order to provide as many recipients as possible with potentially life-saving livers, the Pittsburgh Foundation has been impelled to seek help from other regional organ procurement associations (OPAs). Approximately 110 such regional procurement programs have been established during the past decade.
As was the case with our program, the stimulus for the development of almost all of these OPAs was the need to provide more kidneys for renal transplantation at local renal transplant centers. Prior to 1981, the recovery of extrarenal organs (primarily hearts) from kidney donors identified by these programs was only an occasional experience. It is obvious that the approximately 2,200 kidney donors nephrectomized each year could serve as a source of many hundreds of donor livers for transplantation were the cooperation of other OPAs to be enlisted and a central directory of potential liver recipients created and made available to these OPAs.
The development of standardized techniques for removing donor kidneys and the necessary cooperation between OPAs had been developed to allow kidneys to be shared between the many existent OPAs. In contrast, because the knowledge and skill required in performing a donor hepatectomy has been limited to very few surgeons, we have found that many procurement programs are reluctant to share their donors for liver procurement. This same lack of experience in hepatic recovery has required the Pittsburgh hepatic transplant team to perform the surgical removal of the donor liver as well as performing the transplant. Moreover, in some cases, allowing our surgeons to collaborate with local renal procurement teams has been somewhat threatening to some OPAs. The fear was expressed that donor kidneys would be jeopardized by the techniques required to remove and preserve the liver. Because our hepatonephrectomy technique can be adapted to the requirements of local renal procurement surgeons, this fear was unfounded. In fact, experience has shown us that kidneys recovered from liver donors have a lower incidence of acute tubular necrosis (ATN) than do kidneys recovered from donors of kidneys alone at many centers (10).
These initial concerns have been overcome through various personal communications and the results published by the Pittsburgh team. As a result, during 1981, 176 referrals of potential liver donors were received from other organ procurement programs, and we were able to recover 20 livers from these donors. During 1982, we received 523 referrals of potential liver donors from other programs, of which 64 resulted in recovery and transplantation of the liver. During the first 5 months of 1983, we have received 304 referrals (annual rate of 730), 35 of which resulted in recovery of the liver for transplantation. Figure 3 illustrates the geographic location of the 49 OPAs in the 28 states with which we have worked cooperatively in recovering donor livers for transplantation from January, 1981 through May, 1983.
Fig. 3.
Map of the continental United States identifying the location of the 49 organ procurement agencies in 28 states which have cooperated with the Pittsburgh Agency during the period from January 1981 through May 1983.
The annual increase in liver donor referrals from colleagues at other OPAs illustrates the overwhelming support we have received in our efforts to make liver transplantation available to more recipients. These figures are very encouraging also in view of the development of the several liver transplantation programs at other centers and the resultant growing need for hepatic donors. Unfortunately, many excellent donors have to be declined for reasons other than suitability of the donor. Table 1 indicates the reasons for declining donors referred to us by other programs since January, 1981. Hopefully, with more centers performing liver transplantation, such organs will be used and not wasted in the future.
Table 1. University of Pittsburgh Disposition of Liver Donor Referrals from Organ Procurement Agencies in the United States and Canada (January, 1981 Through May, 1983).
| Donor referral disposition | 1981 | 1982 | 1983a |
|---|---|---|---|
| Liver recovered and transplanted | 20 (30)b | 64 (80)b | 35 (41)b |
| Donor declined by Pittsburgh | |||
| Concurrent donor | 10 | 74 | 49 |
| Liver transplant team exhausted, understaffed, and unavailable | 40 | 102 | 50 |
| OR or anesthesis unavailable | 3 | 4 | 2 |
| No ICU beds | 4 | 43 | 14 |
| Donor history or clinical condition unacceptable | 14 | 54 | 48 |
| Donor age unacceptable | 6 | 34 | 14 |
| Donor hospital too distant | 7 | 3 | 4 |
| No ABO or size-compatible recipient | 44 | 96 | 63 |
| Blood shortage | 3 | 0 | 0 |
| Liver not recovered for other reasons | |||
| Donor family refused to donate | 17 | 35 | 21 |
| Medical examiner refused permission | 2 | 3 | 0 |
| Donor arrested | 4 | 6 | 3 |
| Designated recipient expired before donor available | 2 | 5 | 0 |
| Pittsburgh deferred to center with more urgent need | 0 | 0 | 1 |
| Total no. of referrals | 176 | 523 | 304 |
Data, are for the first 5 months of 1983 only.
Total no. of liver transplants performed is in parentheses.
Obviously, the inauguration of liver transplantation programs at additional centers requires that a mechanism be established for matching available donors with ABO and size-compatible recipients throughout the country. The computer system which has been used for years to distribute kidneys nationally is available for this purpose. More frequently utilized is a 24-hr hotline which was established by the North American Transplant Coordinators Organization (NATCO) in September, 1982. NATCO's 24-ALERT extrarenal hotline is available to the nation's procurement programs from any telephone, at any time, whereas the computer system must be accessed from a terminal generally located in a transplant center. Moreover, the 24-ALERT hotline provides the caller with all of the essential information concerning extrarenal donor needs. Table 2 indicates the information available to procurement programs and physicians through the NATCO 24-ALERT hotline.
Table 2. Information Available Thru NATCO 24-alert Hotline for Matching of Extrarenal Donors and Recipients.
| Name and phone no. of requesting transplant center |
| Organ(s) needed and number of recipients waiting |
| Recipients' priority codes |
| 1 = Hospitalized and critical |
| 2 = Hospitalized and stable |
| 3 = At home and stable |
| Acceptable donor ABO |
| Acceptable donor weight |
| Prospective donor/recipient cross-match needed (yes/no) |
| Other important donor criteria |
| Distance procurement team is willing to fly |
| Name of contact person |
During the first 8 months of its availability, the NATCO 24-ALERT system has made possible the recovery of 81 (121 annual rate) livers which were transplanted at six centers in the United States and Canada. The considerable success of the system has resulted in the establishment of a second 24-hr extrarenal donor hotline for the western United States.
Postmortem Donor Liver Preservation
Preservation of the donor liver has been described elsewhere (11). Starzl has demonstrated that donor livers may be preserved for up to 12 hr with simple cold storage in an electrolyte solution having a composition similar to that found intracellulary. The liver does suffer some injury during the preservation period and at our center, the cold storage time is limited to a period of 8 hr or less. This time is considerably less than is the time considered acceptable for donor kidneys which may be preserved safely using the same techniques for up to 48 hr.
The first step in liver preservation is the in situ infusion of cold lactated Ringers' through a cannula inserted into the splenic vein. This precooling phase using the portal venous system is initiated after all of the liver's attachments have been divided and the various vascular structures entering and leaving the liver have been skeletonized, but before the systemic circulation has been terminated. After approximately 1 to 2 liters of Ringers' solution has been infused, the aorta is cross-clamped above the celiac artery, and cold electrolyte solution is flushed through the distal aorta. This aortic flush allows for simultaneous cooling of the donor kidneys and the liver. A cannula placed in the distal inferior vena cava provides a vent for the venous outflow. After removal, the cold liver is again flushed with an intracellular type solution (Travenol electrolyte solution for kidney preservation) through the splenic vein cannula and is then placed in a sterile plastic bag which is placed in an ice slush and portable cooler (10). At this point, it is ready for transport to the transplant center.
Temporal limitations imposed by current preservation techniques have prevented us from recovering livers from donors more than 1,200 miles from Pittsburgh. The majority of donors from whom we have recovered livers have been identified in hospitals east of the Mississippi River. Thus, a large number of donors, west of the Mississippi, are as yet underutilized.
Jet transportation of our surgical team is required when we travel to donor hospitals over 400 miles from Pittsburgh. This has been accomplished by securing the cooperation of several Pittsburgh-based corporations which have volunteered their corporate aircraft for liver procurement if an aircraft is available. When a corporate airplane cannot be secured, chartered air services have been utilized.
Summary
Liver transplantation is now performed in the United States and Canada at major centers in Pittsburgh, Minneapolis, Memphis, Sacramento, Boston, and London, Ontario. It is expected that at least six additional hepatic transplantation programs will be inaugurated within the next 6 months and 18 additional centers may be active within the next 2 years. Clearly, as a result of this increased activity, the need for postmortem livers for transplantation will certainly increase.
The experience at the University of Pittsburgh in postmortem liver procurement has been outlined above. The major factors which have influenced the availability of suitable donors at our institution have been identified. The success of the program has been in a large part attributable to the invaluable collaboration of other regional renal procurement programs, and it is expected that any new center embarking upon liver transplantation will necessarily have to establish similar cooperative efforts with these OPAs.
The fact that many more donors were referred to us than we were able to accept, obscures somewhat the fact that a serious shortage of donor organs does prevail. This is best documented by the fact that during the first 2 years of the liver transplantation program in Pittsburgh, 110 livers have been transplanted while 71 patients died waiting for a suitable donor organ. Twenty-seven of these were pediatric patients whose lives could have been saved if a size and ABO compatible donor had been identified and referred in time for successful transplantation. The fact remains that many otherwise acceptable donors which are referred to us are incompatible with our waiting pool of recipients.
National concern has been expressed recently by congress and the United States Surgeon General regarding the embarrassing fact that no more than 1 of 8 potential donors now yields organs for transplantation in this country. This lamentable fact is not due to a shortage of organ procurement personnel, funding, or technical competence. It is due principally to the lack of awareness and cooperation of practicing physicians and other health care professionals who must assume the primary responsibility of identifying and directing potential donors and their families to OPAs.
References
- 1.Cooper KD, et al. The potential supply of cadaveric kidneys for transplantation. Trans Am Soc Artif Intern Organs. 1977;23:416–421. doi: 10.1097/00002480-197700230-00108. [DOI] [PubMed] [Google Scholar]
- 2.Transplantation Society of Michigan Project to reduce waiting time for cadaveric kidney transplantation in Michigan phase I final report. 1982. [Google Scholar]
- 3.Barb KJ. Cadaveric kidneys for transplantation: a paradox of shortage in the face of plenty. Transplantation. 1981;35:379–382. [PubMed] [Google Scholar]
- 4.Council on Scientific Affairs of the American Medical Association. Organ donor recruitment. JAMA. 1981;246:2157–2158. [PubMed] [Google Scholar]
- 5.Gallup G. The Gallup Report. Princeton, New Jersey: American Institute for Public Opinion; 1968. Crucial questions answered: eighty million Americans are willing to donate vital organs to science. [Google Scholar]
- 6.The Gallup Organization, Inc. Attitudes and opinions of the American Public toward kidney donations, Prepared for the American Kidney Foundation. 1983. [Google Scholar]
- 7.Abram HS, Vender Zwaag R, Johnson HK. Physicians' attitudes toward organ donation. South Med J. 1975;68:443–446. doi: 10.1097/00007611-197504000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Kidney Foundation of Eastern Missouri and Metro East, Inc. Assessment of public and professional attitudes regarding organ donation. 1975. [Google Scholar]
- 9.Kaufman HH, Huchton JD, McBride MM, et al. Kidney donation: needs and possibilities. Neurosurgery. 1979;5:237–244. doi: 10.1227/00006123-197908000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Shaw BW, Hakala T, Rosenthal JT, et al. Combination donor hepatectomy and nephrectomy and early functional results of allografts. Surg Gynecon Obstet. 1982;155:321–325. [PMC free article] [PubMed] [Google Scholar]
- 11.Benichou J, Halgrimson CG, Weil R, et al. Canine and human liver preservation for 6-18 hours by cold infusion. Transplantation. 1977;24:407–411. doi: 10.1097/00007890-197712000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]


