Abstract
Background
Acetabular labral tears are being diagnosed with increasing frequency and there is a growing consensus that these tears rarely occur in the absence of osseous abnormalities.
Questions/purposes
We therefore determined the presence of structural abnormalities in patients with acetabular labral tears using a standardized CT protocol.
Methods
We evaluated 135 consecutive patients with labral tears diagnosed by MRI with CT scans of the symptomatic hip. The CT scans were evaluated in a standardized fashion to determine acetabular and femoral pathomorphologic features. Acetabular evaluation included version measurements and anterior and lateral center-edge angles. Femoral parameters evaluated included version, alpha angle, and neck-shaft angle.
Results
One hundred twenty-two (90%) of the 135 hips had structural abnormalities. One hundred two (76%) had an alpha angle greater than 50°, 18 (13%) had femoral version less than 5°, 22 (16%) had femoral version greater than 25º, and five (4%) had coxa valga. Fifty-eight (43%) patients had acetabular retroversion and five (4%) had a lateral center-edge angle less than 20º. Of the 58 patients with acetabular retroversion, 23 had isolated cranial retroversion, 12 had isolated central retroversion, and 23 had combined cranial and central retroversion. Sixty-seven of the 121 hips (55%) with bony abnormalities had a combination of abnormalities.
Conclusions
Ninety percent of patients with labral tears had structural abnormalities seen on CT scans. These structural abnormalities frequently occur in combination, and understanding these underlying morphologic features of the hip can help guide treatment.
Level of Evidence
Level IV, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Acetabular labral tears are a potential source of hip pain in young adults. With improvements in diagnostic imaging and clinical examination, labral tears are being diagnosed with increasing frequency [3]. Multiple etiologies of labral tears have been proposed, including trauma, femoroacetabular impingement (FAI), capsular laxity, dysplasia, and degeneration [15]. However, there is a growing consensus that labral tears rarely occur in the absence of bony abnormalities and that neglecting these underlying structural abnormalities may result in treatment failure [12, 25]. In support of this theory, Wenger et al. reported 87% of patients with labral tears had an identifiable underlying structural abnormality seen on plain radiographs [33].
Plain radiographs traditionally have been used to evaluate bony abnormalities in patients with hip pain. However, plain radiographic evaluation of the hip is dependent on patient positioning and subject to inconsistencies in radiographic technique and image quality [14, 29]. Furthermore, many of the standard radiographic parameters used to diagnose hip disorders in young adults have limited reliability [6]. MRI is used to supplement plain radiographs and identify soft tissue disorders, labral tears, and articular cartilage damage that could explain the etiology of hip pain but is not the optimal imaging modality for defining bony anatomy. CT allows accurate evaluation of the bony anatomy of the hip with an accuracy of 1° to 4.5º [1, 7]. Unlike plain radiographs, CT precisely assesses anatomic relationships independent of patient position, can quantify femoral and acetabular version, and through postprocessing techniques can render a 3-D model of the hip that facilitates observation of bony morphologic features in multiple planes.
The purpose of this observational study was to determine the percentage of patients with abnormal bony morphologic features as detected by a standardized CT protocol in a consecutive series of patients with acetabular labral tears.
Patients and Methods
Between January and April 2009, 137 consecutive patients with acetabular labral tears diagnosed by MRI or MRA also underwent a CT scan of the hip. Eighty percent (110) of the patients presented with the diagnosis of a labral tear based on an MRA already performed at an outside institution. The remaining 27 patients had a noncontrast MRI using a previously reported protocol [20]. Indications for MRI included a history of recalcitrant groin or hip pain and physical examination findings consistent with an intraarticular disorder. Along with plain radiographs, MRI/MRA, and an intraarticular injection, CT with 3-D reformatting is part of the senior author’s (BTK) standard preoperative evaluation for patients undergoing arthroscopic hip surgery for an acetabular labral tear. Based on a preoperative screening algorithm, we excluded patients with classic hip dysplasia (Wiberg center-edge angle less than 15°, Tönnis angle greater than 15°) or advanced osteoarthritis (marked joint space loss), because these patients were not considered candidates for arthroscopic treatment of the labral tear. Two additional patients with a history of femoral osteotomy were excluded from the study group, leaving a total of 135 patients with CT scans for analysis. There were 78 males and 57 females with an average age of 30 years (range, 14–55 years). Institutional Review Board approval was obtained to review the patients’ CT scans.
The CT scans were performed according to a standard protocol, and each reading was completed by one of four radiologists (GD, SA, DD, RL) with more than 10 years of experience assessing CT of the hip. The hips were scanned using a GE VCT 64 channel CT scanner (GE Healthcare, Milwaukee, WI, USA) with the patient lying supine using 2.5-mm axial cuts, and images were obtained of the pelvis and the distal femur to allow for evaluation of femoral version. Computer software was used to create interpolated images at 0.625-mm intervals and coronal, sagittal, and radial reformatted images. A GE Volume viewer workstation was used for all reformations and 3-D volume renderings performed. The average dose of radiation for the CT scan was 16.48 mGy, and the national average 2010 Medicare reimbursement for CT Hip is $241.73 (CPT 73700).
Standard measurements were made on each CT scan using the axial and reformatted images on a GE Centricity PACS-IW workstation (GE Healthcare). By convention, many measurements used to evaluate morphologic features of the hip include the center of the femoral head. An ellipse measurement tool was used to trace the femoral head on a coronal reformatted image that captured the largest diameter of the femoral head and cross-referenced to the oblique axial image to bisect the femoral head and neck in one plane. This point then was saved and used in other planes to keep the center of the head constant while performing various measurements.
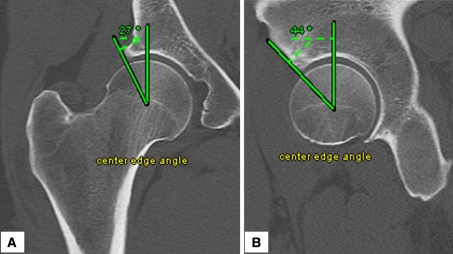
Four radiologists (GD, SA, DD, RL) evaluated all images for several measurements. The lateral center-edge angle (CEA) on coronal reformatted images was determined by measuring the angle between two lines: a line through the center of the femoral head perpendicular to the transverse axis of the pelvis and a line connecting the center of the femoral head to the most superolateral point of the acetabulum [5, 34]. The anterior CEA was calculated on sagittal reformatted images by measuring the angle between a vertical line passing through the center of the femoral head and a line connecting the center of the femoral head and the most anterior part of the acetabulum [5, 16] (Fig. 1). The average lateral CEA was 31.4º ± 6.9º and the average anterior CEA was 51.8º ± 10.3º (Table 1).
Fig. 1A–B.
The sample measurements made for the (A) lateral center-edge angle and (B) anterior center-edge angle are shown.
Table 1.
Range of values obtained in CT evaluations of hips
| Measurement | Value | Number of patients |
|---|---|---|
| α angle | < 42º | 7 |
| 42º–50º | 26 | |
| 51º–55º | 15 | |
| 56º–60º | 19 | |
| > 60º | 68 | |
| Lateral center edge angle | < 15º | 1 |
| 16º–19º | 4 | |
| 20º–24º | 10 | |
| > 25º | 120 | |
| Neck-shaft angle | < 120º | 0 |
| 120º–124º | 7 | |
| 125º–135º | 103 | |
| 136º–140º | 18 | |
| > 140º | 7 | |
| Femoral version | < 0º | 11 |
| 0º–5º | 9 | |
| 5º–25º | 93 | |
| 25º–30º | 10 | |
| > 30º | 12 | |
| Cranial acetabular version | < 0º | 46 |
| 0º–5º | 32 | |
| > 5º | 57 | |
| Central acetabular version | < 0º | 7 |
| 0º–9º | 28 | |
| 10º–20º | 81 | |
| > 20º | 19 |
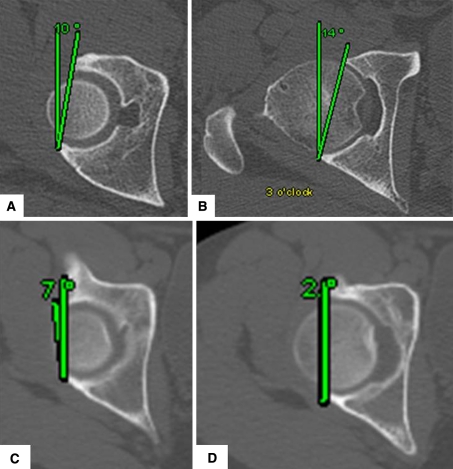
Acetabular version (AV) was obtained in the axial plane by measuring the angle made by a line connecting the anterior and posterior rims of the acetabulum and a line extending anteriorly from the posterior wall [28]. To control for pelvic rotation, a transverse line connecting the ischial spines was used. Acetabular version measurements were made at two different transverse planes: through the center of the femoral head (ie, 3 o’clock position) and more cranially through the plane corresponding to the 1 o’clock position of the femoral head (Fig. 2). The average cranial AV was 3.2º ± 8.6º and the average central AV was 13.7º ± 7.6º (Table 1).
Fig. 2A–D.
The measurements made for (A) normal cranial and (B) central acetabular version and (C) cranial and (D) central acetabular retroversion are shown.
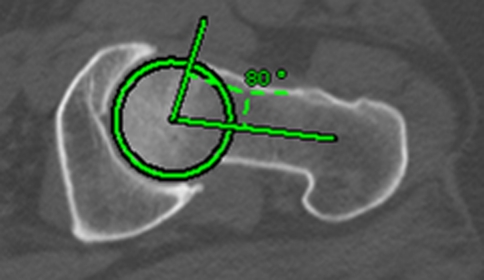
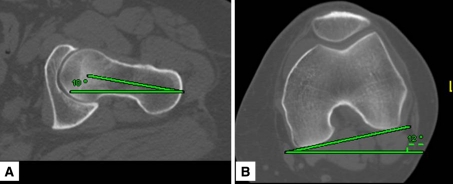
The neck-shaft angle was measured on coronal images using the image that best captured the femoral head, neck, and shaft in one image. The angle created by the intersection of a line through the center of the femoral head passing through the center of the femoral neck and a line bisecting the femoral shaft was recorded (Fig. 3). The alpha angle was determined on axial oblique images taken in the plane of the femoral neck. The angle was determined by two lines: a line connecting the center of the femoral head to the center of the femoral neck and a second line connecting the center of the femoral head and the point at which the femoral head prominence exits the normal radius of the femoral head [22] (Fig. 4). Femoral version was measured on axial images by measuring the angle formed by a line through the center of the femoral head passing through the center of the femoral neck and a line connecting the posterior condyles of the femur [21] (Fig. 5). For the femur, the average values were: alpha angle 59.5º ± 11.5º, neck shaft angle 130.7º ± 4.3º, and version 15.5º ± 10.6º (Table 1).
Fig. 6.
A 3-D reconstruction of a CT scan shows detail of osseous morphologic features.
Fig. 3.
A sample CT measurement of the neck shaft angle is shown.
Fig. 4.
The alpha angle was measured by a line connecting the center of the femoral head to the center of the femoral neck and a second line connecting the center of the femoral head and the point at which the femoral head prominence exits the normal radius of the femoral head.
Fig. 5A–B.
The technique for measuring the femoral version angle is shown. (A) A line is made from the base of the femoral neck through the center of the femoral head that is 10° anteverted relative to the reference line. (B) A line is made connecting the posterior femoral condyles that is 12° internally rotated relative to the reference line. In this example the patient has femoral anteversion of 22°.
The measured values from the CT scan were classified as abnormal using values that exceeded published limits of normal measurements and were drawn from previous studies to allow for comparison with the current literature [2, 5, 12, 15, 18, 19, 21, 25, 27, 31–33] (Table 2). For the CT evaluation, acetabular retroversion was defined as cranial retroversion with a negative value at 1 o’clock and as central retroversion with a value of less than 10º at 3 o’clock. Abnormal values for the other CT measurements included lateral CEA less than 20º, anterior CEA less than 20º, alpha angle greater than 50º, neck-shaft angle less than 120º or greater than 140º, and femoral version less than 5° or greater than 25°.
Table 2.
Definitions of measured radiographic parameters
| Parameter | Definition | Abnormal values | Normal values | Reference study |
|---|---|---|---|---|
| Alpha angle | Angle formed by the femoral neck axis and a line connecting the center of the femoral head with the point of beginning asphericity | > 50° | < 50° | Notzli et al. [22] |
| Neck shaft angle | Angle formed by the axis of the femoral neck and the proximal femoral diaphysis | < 120° and > 140° | 125° < neck shaft angle < 135° | Tonnis & Heinecke [32] |
| Femoral version | Angle between the femoral neck axis and the posterior condylar axis of the knee | < 5° (retroverted) and > 25° (anteverted) | 15°–20 | Tonnis & Heinecke [32] |
| 9.8° | Maruyama et al. [19] | |||
| 13° | Reikeras et al. [26] | |||
| Cranial acetabular version | Angle made by a line connecting the anterior and posterior rims of the acetabulum and a line extending anteriorly from the posterior wall perpendicular to the transverse plane of the pelvis, as measured at a point corresponding to the 1 o’clock position on the femoral head | < 0° (retroverted) | 5° | Reynolds et al. [28] |
| 8.5° | Jamali et al. [13] | |||
| Central acetabular version | Angle made by a line connecting the anterior and posterior rims of the acetabulum and a line extending anteriorly from the posterior wall perpendicular to the transverse plane of the pelvis, as measured at a point corresponding to the 3 o’clock position on the femoral head | < 10° (retroverted) | 20° | Reynolds et al. [28] |
| 13.7° | Jamali et al. [13] | |||
| Lateral center edge angle | Angle formed by a line perpendicular to the transverse pelvic axis and by the line connecting the center of the femoral head with the lateral edge of the acetabulum | < 20° | > 25° | Wiberg [34] |
| Anterior center edge angle | Angle formed by a line perpendicular to the transverse pelvic axis and by the line connecting the center of the femoral head with the anterior edge of the acetabulum | < 20° | > 20° | Lequesne & de Seze [16] |
The average value and SD were calculated for each of the parameters measured. The percentage of patients with an abnormal finding and the percentage of patients with a combination of abnormal findings were calculated.
Results
One hundred twenty-two (90%) of the 135 hips had structural abnormalities. One hundred two patients (76%) had an alpha angle greater than 50º, 18 (13%) had femoral version less than 5º, 22 (16%) had femoral version greater than 25º, five (4%) had coxa valga, 58 (43%) had acetabular retroversion, and five (4%) had a lateral CEA less than 20º. Of the 58 patients with acetabular retroversion, 23 had isolated cranial retroversion, 12 had isolated central retroversion, and 23 had combined cranial and central retroversion. Sixty-seven of the 121 hips (55%) with bony abnormalities had a combination of other abnormalities. Of these 67 hips, 51 had two abnormal findings and 16 had three structural abnormalities. The most common combination of abnormal findings, an alpha angle greater than 50º and acetabular retroversion, was found in 26 patients. Fourteen of the 16 patients with three structural abnormalities had abnormal femoral version (Table 3).
Table 3.
Various combinations of abnormalities in the patients with three structural abnormalities
| Combination of structural abnormalities | Number of patients |
|---|---|
| Elevated α angle, acetabular retroversion, femoral anteversion | 9 |
| Elevated α angle, acetabular retroversion, femoral retroversion | 3 |
| Elevated α angle, acetabular retroversion, coxa valga | 2 |
| Elevated α angle, coxa valga, femoral retroversion | 1 |
| Elevated α angle, decreased center edge angle, femoral anteversion | 1 |
Discussion
During the last decade, the understanding of acetabular labral tears has been advanced by increased physician awareness, improvements in clinical examination, and advanced imaging techniques, most notably MRI and arthrography. Although multiple etiologies of labral tears have been proposed, there is a growing consensus that labral tears rarely occur in the absence of bony abnormalities [9, 11, 16, 32]. Plain radiographs and MRI often are used in the initial evaluation of patients with labral tears, however CT may be helpful in evaluating the subtle osseous abnormalities that underlie these tears and provide additional information regarding femoral version. Therefore, the purpose of this study was to report on the structural abnormalities detected by CT in a consecutive series of patients with labral tears.
Our findings must be viewed in the context of several limitations. First, we lacked a control group and cannot comment on the incidence of these structural abnormalities in a healthy population. Second, we had no clinical outcomes for this patient cohort and therefore cannot comment on the long-term implications of these structural abnormalities. However, all patients were symptomatic and all had MRI diagnosis of a labral tear. Third, we decided to use values that exceeded the proposed normal limits to classify a measurement as abnormal. Although this may have underestimated the number of structural abnormalities reported, the values were chosen based on previous studies of morphologic features of the hip [2, 5, 11, 13, 16, 19, 21, 22, 26, 28, 32–34]. Furthermore, the CT measurements of the lateral and anterior CEAs have not been validated. Specifically, the anterior CEA, measured in the current study on sagittal reformatted CT images, differs from the projection on a standing false profile radiograph, and the values presented here are likely higher than would be obtained on the standard false profile view. The CT measurements taken by the radiologists also are subject to error and interobserver and intraobserver variabilities. Clohisy et al. evaluated similar measurements applied to plain radiographs and found many of these standard measurements have limited reliability [6].
Previous studies have used plain radiographs to study structural abnormalities in patients with labral tears. Wenger et al. reported 87% of patients with labral tears had at least one structural abnormality observed on plain radiographs [33]. Peelle et al. evaluated 78 patients treated arthroscopically for acetabular labral tears and found 49% of patients with labral tears had at least one radiographic abnormality [23]. The patients in the current study more closely resemble the cohort of patients in the study by Wenger et al., because both attempted to exclude patients with classic hip dysplasia.
Structural abnormalities of the acetabulum, including acetabular retroversion and coxa profunda, can result in acetabular labral tears [17, 24, 30, 33]. Acetabular retroversion can result in impingement of the labrum between the acetabulum and femur, leading to crushing, degeneration, and eventual ossification of the labrum [9, 30]. This form of focal pincer impingement frequently is localized to the superior, or cranial, portion of the acetabulum, and previous authors have differentiated between cranial and central AV when studying acetabular retroversion. Reynolds et al. defined these measurements using CT in a group of 174 normal hips as the roof edge (RE) angle (at the proximal opening of the acetabulum) and equatorial edge (EE) angle (at the maximum diameter of the femoral head) [28]. They reported median values of 5º for the RE angle and 20º for the EE angle in this group of normal hips. Jamali et al. evaluated 43 pelvic specimens (86 acetabuli) with CT and calculated AV at the cranial acetabulum (5 mm distal to the acetabular roof) and central acetabulum (through the longitudinal center of the acetabulum) with the pelvic specimens aligned in the anatomic frontal plane [13]. They reported mean values of cranial AV of 8.5° ± 9.1º and central AV of 20.1° ± 6.4º. Cranial retroversion (AV less than 0º) was present in 22% of the hips in their study compared with 34% of the hips in our study. The average cranial AV (3.2º ± 8.6º) and average central AV (13.7° ± 7.6º) of our patients were less than in the previously mentioned studies, likely because our study consisted primarily of patients with underlying structural hip abnormalities, the majority of whom had findings consistent with FAI. Differentiating between cranial and central acetabular retroversion has implications for treatment. Isolated cranial retroversion may be addressed through acetabular rim trimming, whereas the more global central retroversion may be treated more appropriately through a pelvic reorientation osteotomy.
Thirty percent of the patients with labral tears in the current study had femoral version abnormalities with a slightly greater incidence of increased femoral anteversion (16.3%) than retroversion (13.3%). Normal femoral version is commonly cited as 15° to 20° anteversion; however, values have been reported outside this range in a study of healthy adults [32]. Reikeras et al., for example, used CT to evaluate femoral anteversion in 47 healthy adults and found a mean value of 13° ± 7º [26]. Maruyama et al. evaluated 100 pairs of cadaveric femurs and found the mean femoral anteversion to be 9.8° ± 8.5º [19]. The CT measurements made for femoral version in the current study follow a similar protocol used by Reikeras et al. [26], and the values chosen for abnormal fall outside their average values. Some studies have supported the hypothesis that abnormal femoral version leads to osteoarthritis of the hip [10, 26, 27, 31, 32]. Although we were unable to address causation in the current study, the role of femoral version in the etiology of labral tears and alterations in hip mechanics are areas of potential future study.
We used numerous acetabular and femoral measurements to evaluate the mechanical alterations present in the hips with labral tears. This systemic approach has been applied to the evaluation of plain radiographs [5], and although CT has certain advantages over radiographs in evaluating morphologic features of the hip, plain radiographs remain the standard screening tool. CT adds an additional cost and is associated with substantial radiation exposure, even when using modern scanning protocols [4]. However, CT can detect and quantify subtle structural abnormalities, including femoral and acetabular version that may influence treatment. By interpreting these findings in conjunction with a detailed clinical history and physical examination, a mechanical diagnosis can be obtained that then can lead to the appropriate treatment.
We found a high incidence (90%) of structural abnormalities in patients with acetabular labral tears. These findings support the concept that labral tears rarely occur in isolation and their presence should alert the clinician to search for altered hip mechanics and underlying osseous pathomorphology.
Acknowledgments
We thank Steven Albert MD, Douglas Decorato MD, and Robert Ludwig MD for assistance in evaluating CT scans for this study.
Footnotes
One or more of the authors (BTK) is a paid consultant for Pivot Medical, Inc, Smith & Nephew, and Shriners Hospitals for Children Clinical Outcomes Studies Advisory Board and holds stock or stock options in Pivot Medical, Inc and Smith & Nephew. One or more of the authors (AB) is a paid consultant for Smith & Nephew.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Hospital for Special Surgery, New York, NY, USA.
References
- 1.Abel MF, Sutherland DH, Wenger DR, Mubarak SJ. Evaluation of CT scans and 3-D reformatted images for quantitative assessment of the hip. J Pediatr Orthop. 1994;14:48–53. doi: 10.1097/01241398-199401000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Allen D, Beaule PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91:589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 3.Bedi A, Chen N, Robertson W, Kelly BT. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24:1135–1145. doi: 10.1016/j.arthro.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91:1882–1889. doi: 10.2106/JBJS.H.01199. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P, Steger-May K, Schoenecker PL, Millis M. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467:666–675. doi: 10.1007/s11999-008-0626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen MS, Gelberman RH, Griffin PP, Kasser JR, Emans JB, Millis MB. Slipped capital femoral epiphysis: assessment of epiphyseal displacement and angulation. J Pediatr Orthop. 1986;6:259–264. doi: 10.1097/01241398-198605000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15:475–481. doi: 10.1097/00005131-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 10.Giunti A, Moroni A, Olmi R, Rimondi E, Soldati D, Vicenzi G. The importance of the angle of anteversion in the development of arthritis of the hip. Ital J Orthop Traumatol. 1985;11:23–27. [PubMed] [Google Scholar]
- 11.Guevara CJ, Pietrobon R, Carothers JT, Olson SA, Vail TP. Comprehensive morphologic evaluation of the hip in patients with symptomatic labral tear. Clin Orthop Relat Res. 2006;453:277–285. doi: 10.1097/01.blo.0000246536.90371.12. [DOI] [PubMed] [Google Scholar]
- 12.Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007;23:1295–1302. doi: 10.1016/j.arthro.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 14.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504. doi: 10.1016/j.arthro.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 16.Lequesne M, Seze S. [False profile of the pelvis: a new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies] [in French] Rev Rhum Mal Osteoartic. 1961;28:643–652. [PubMed] [Google Scholar]
- 17.Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616–622. doi: 10.1007/s11999-008-0646-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leunig M, Casillas MM, Hamlet M, Hersche O, Notzli H, Slongo T, Ganz R. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71:370–375. doi: 10.1080/000164700317393367. [DOI] [PubMed] [Google Scholar]
- 19.Maruyama M, Feinberg JR, Capello WN, D’Antonio JA. The Frank Stinchfield Award: Morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res. 2001;393:52–65. doi: 10.1097/00003086-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Mintz DN, Hooper T, Connell D, Buly R, Padgett DE, Potter HG. Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using non-contrast imaging. Arthroscopy. 2005;21:385–393. doi: 10.1016/j.arthro.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 21.Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT. Femoral anteversion. J Bone Joint Surg Am. 1987;69:1169–1176. [PubMed] [Google Scholar]
- 22.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 23.Peelle MW, Della Rocca GJ, Maloney WJ, Curry MC, Clohisy JC. Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res. 2005;441:327–333. doi: 10.1097/01.blo.0000181147.86058.74. [DOI] [PubMed] [Google Scholar]
- 24.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults. J Bone Joint Surg Am. 2006;88:1735–1741. doi: 10.2106/JBJS.E.00514. [DOI] [PubMed] [Google Scholar]
- 25.Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 26.Reikeras O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta Orthop Scand. 1983;54:18–23. doi: 10.3109/17453678308992864. [DOI] [PubMed] [Google Scholar]
- 27.Reikeras O, Hoiseth A. Femoral neck angles in osteoarthritis of the hip. Acta Orthop Scand. 1982;53:781–784. doi: 10.3109/17453678208992292. [DOI] [PubMed] [Google Scholar]
- 28.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 29.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 30.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 31.Terjesen T, Benum P, Anda S, Svenningsen S. Increased femoral anteversion and osteoarthritis of the hip joint. Acta Orthop Scand. 1982;53:571–575. doi: 10.3109/17453678208992260. [DOI] [PubMed] [Google Scholar]
- 32.Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 33.Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]
- 34.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939;83(suppl 58):7–38. [Google Scholar]