Abstract
Objectives
To fit and evaluate the control of a complex prosthesis for a shoulder disarticulation level amputee subject with targeted muscle reinnervation.
Design
One participant who had targeted muscle reinnervation surgery was fit with an advanced prosthesis and usage with this device was compared to the device used in the home setting.
Setting
The experiments were completed within a laboratory setting.
Participants
The first recipient of targeted muscle reinnervation: a bilateral shoulder disarticulation level amputee.
Interventions
Two years after surgery, the subject was fit with a 6 degree of freedom (DOF) prosthesis (shoulder flexion, humeral rotation, elbow flexion, wrist rotation, wrist flexion, and hand control). Control of this device was compared to his commercially available 3 DOF system (elbow, wrist rotation, and powered hook terminal device).
Main Outcome Measure
In order to assess performance, movement analysis and timed movement tasks were executed.
Results
The subject was able to independently operate all 6 arm functions with good control. He could simultaneously operate 2 DOF of several different joint combinations with relative ease. He operated up to 4 DOF simultaneously, but with poor control. Work space was markedly increased and some timed-tasks were faster with the 6-DOF system.
Conclusions
This proof-of-concept study shows that advances in control of shoulder disarticulation level prostheses can improve the quality of movement. Additional control sources may spur the development of more advanced and complex componentry for these amputees.
Keywords: Artificial limbs, Electromyography, Nerve transfer, Rehabilitation
Current prostheses for shoulder disarticulation amputees are very difficult to control. This is due to the fact that there are many joints lost, and few control input options available. For an externally-powered system the most common types of control are to use myoelectric signals from the chest and back muscles, or to use switches operated with the chin and remnant shoulder. An example of a conventional myoelectric control for an externally powered prosthesis would be to use the pectoralis major to close the hand and supraspinatus to open the hand. A chin switch would then toggle through the controls so that these same 2 muscles operate the wrist rotator and elbow. The operation of each DOF controlled sequentially is slow and tedious. Furthermore, these control inputs are not physiologically mapped to the function (eg, shoulder movement and/or pectoralis contractions do not naturally correspond to hand movement) making operation of the artificial arm difficult for people with these high level amputations.
Targeted muscle reinnervation is a technique developed to increase the number of myoelectric control inputs available for use with a prosthetic device, with the chance to have a greater number of more physiologically appropriate control inputs. Targeted muscle reinnervation transfers the residual nerves to remnant muscles that are no longer biomechanically functional due to the amputation.1,2 The target muscles are first denervated. The remnant peripheral nerves that use to control the elbow and hand functions are then attached to the target muscles and allowed to reinnervate. These reinnervated muscles now serve as biologic amplifiers of the residual nerve commands. A single muscle, innervated by a different nerve branches, can be subdivided into segments for multiple nerve transfers. Targeted muscle reinnervation thus provides physiologically appropriate surface electromyographic control signals that are directly related to functions in the lost arm (eg, using a median nerve transfer to create a signal for closing of the hand). Targeted muscle reinnervation control has made possible a 2- to 6-fold increase of speed in task performance and a self-reported increase in ease of function and use (see www.ric.org/research/centers/necal/index.aspx to view video).3–7
Currently, only 3 powered DOF are commercially available for upper-limb amputees: elbows, wrist rotators, and terminal devices. This is due, at least in part, to a lack of available inputs to control more motorized joints. In this study, we created a prosthesis for use in the laboratory with 6 powered DOF to show that operation of a more highly articulated prosthesis is possible for an individual with targeted reinnervation at the shoulder disarticulation level. It has not been possible to meaningfully control this number of DOFs in the past. Analyses of workspace, simultaneous control, and function were performed.
METHODS
The Subject
Targeted muscle reinnervation surgery was performed on the left (nondominant) side of a 56-year-old male bilateral shoulder-disarticulation level amputee in conjunction with surgery to remove painful split thickness skin grafts. Surgery was performed approximately 9 months after the initial high-power electrical burns. The pectoralis major and minor muscles were denervated and used as recipient muscles for the brachial plexus nerves.4 This created 4 new physiologically appropriate myoelectric signals in the left pectoralis muscle (table 1). An unplanned, but fortuitous result was that the median nerve reinnervated 2 functionally separate regions of the middle segment of the pectoralis major muscle. The hand close and wrist flexors portion of the median nerve reinnervated 1 region of the middle segment and was used to control hand closing, while the thumb abductors portion reinnervated a separate region of the middle segment and was used to control hand opening. The ulnar nerve transfer to the pectoralis minor was unsuccessful.
Table 1.
Location of Targeted Reinnervation Sites and Additional Electromyographic and Analog Inputs Used for Control of the Six–DOF Prosthesis
| Location of input | Control Input Type | Controlled Function |
|---|---|---|
| Median nerve transfer to middle pectoralis* | EMG | Hand open |
| Median nerve transfer to middle pectoralis* | EMG | Hand close |
| Musculocutaneous nerve transfer to superior pectoralis* | EMG | Elbow flexion |
| Radial nerve transfer to inferior pectoralis* | EMG | Elbow extension |
| Middle Deltoid | EMG | Internal humeral rotation |
| Latissimus Dorsi | EMG | External humeral rotation |
| Shoulder contact with anterior location of socket | Force sensing resistor | Wrist flexion/extension |
| Shoulder contact with posertior location of socket | Force sensing resistor | Wrist pronation/supination |
| Shoulder contact with superior location of socket | Digital rocker switch | Shoulder flexion/extension |
Abbrevitations: EMG, electromyographic.
Targeted reinnervation site
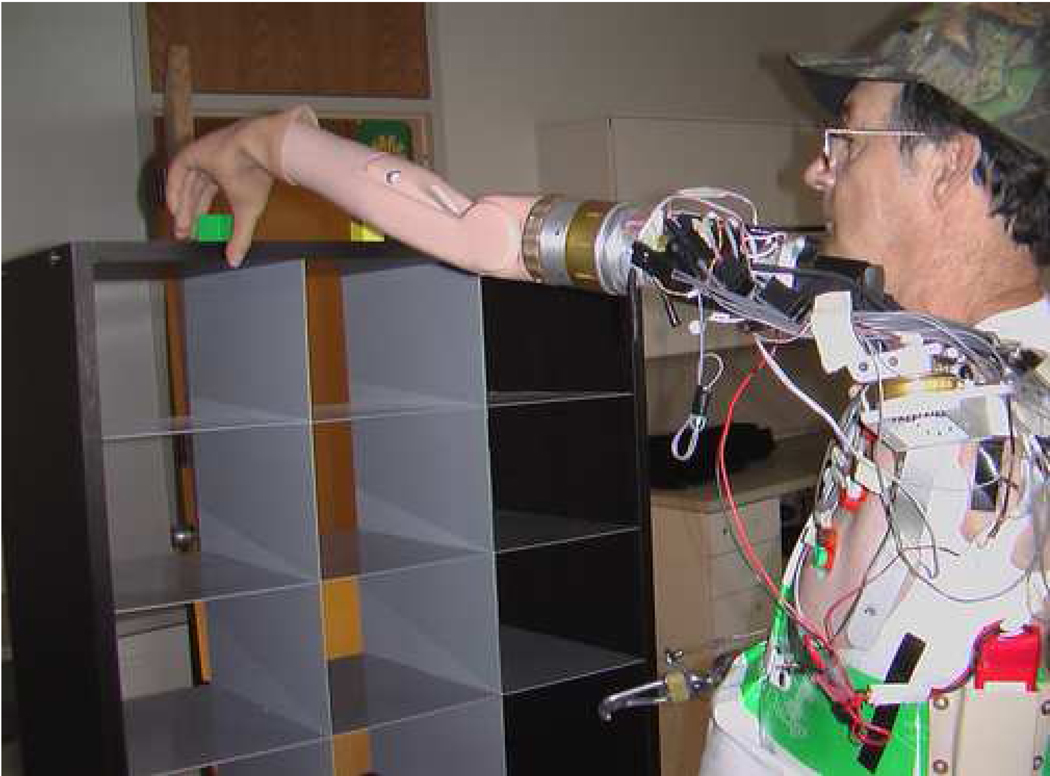
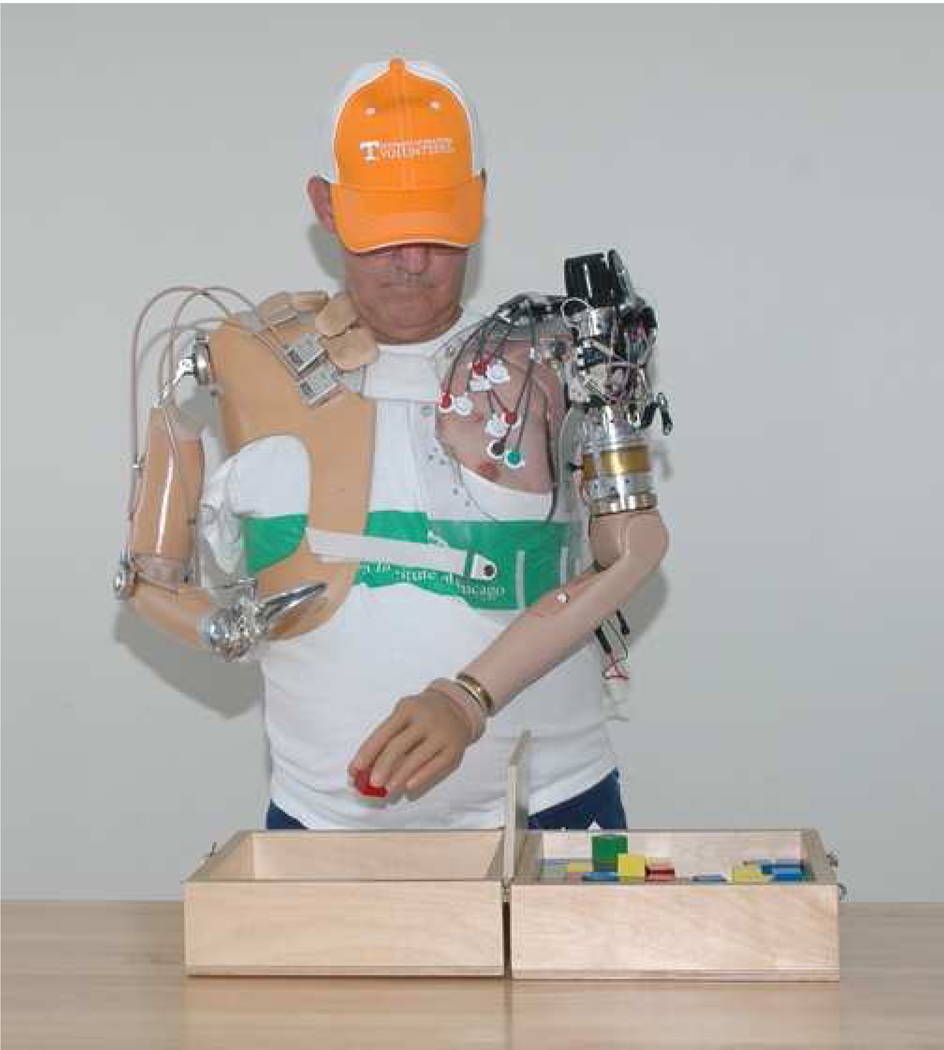
A prosthesis with 3 powered DOF was developed to enable use of the new targeted muscle reinnervation control sites. It consisted of: a manual locking shoulder; Boston Digital Arma modified to accept additional electromyographic inputs with a passive friction humeral rotator; a powered wrist rotator (model #10S17)b and a powered hook (Greifer model #8E32b) (fig 1A). The 4 targeted muscle reinnervation electromyographic control signal sites allowed the subject to simultaneously operate his terminal device (hook or hand) and elbow in an intuitive manner. He could have operated his wrist rotator simultaneously using shoulder inputs, but preferred to use sequential control of the terminal device and wrist with his hand open and close targeted muscle reinnervation electromyographic control signal sites. This was preferred so that he could avoid dropping objects by disabling the terminal device when switching to wrist. The subject uses this prosthesis on a regular basis at home; he wears this device 3 to 5 days a week for 2 to 8 hours at a time.
Fig. 1.
On left side: (A) Three-DOF prosthesis consisting of nonpowered locking shoulder, passive humeral rotator, powered elbow, powered wrist rotator, and powered hook terminal device; (B) Six-DOF prosthesis consisting of powered shoulder, humeral rotator, elbow, wrist rotator, wrist flexor, and hand.
Six DOF Arm System
With the increased number of input signals, a goal was set to build a prosthesis with the maximum number of controlled functions available. Six-motorized components were identified. They included a prototype shoulder,c a prototype humeral rotator,8 a microprocessor controlled elbow (elbow motor, battery, and controller),a a wrist rotator,b and a hand with both open/close and wrist flexion/extension.d These components were integrated into a functional arm system with a highly flexible array of control inputs (fig 1B). Problematic cardiac interference was minimized by using electrodes custom modified to have a 60Hz high pass filter. This proved to be effective in reducing approximately 75% of the cardiac interference.9,10
A list of all the inputs used to control the six DOFs are presented in table 1. The 4 targeted muscle reinnervation myoelectric sites were used to control the hand and elbow as described above. EMG from the subject’s residual latissimus dorsi muscle was used to control external (lateral) humeral rotation and the EMG from his residual deltoid muscle was used to control internal (medial) humeral rotation. A rocker switch was positioned superior to the lateral acromion within the socket to control shoulder movements. Contact with the anterior aspect of the rocker flexed the arm at the shoulder joint and contact with the posterior aspect of the rocker extended the shoulder. A force sensing resistor (a thin, 2-cm diameter Touch Pada) was mounted in the socket anterior to the acromioclavicular joint so that contact with this force sensing resistor using shoulder protraction could control wrist flexion: a soft and slow push on the force sensing resistor flexed the wrist while a hard and fast push extended the wrist. Similarly, a force sensing resistor was mounted at the same level in the posterior aspect of the socket so that shoulder retraction could control wrist rotation; a soft and slow push pronated the wrist while a fast and hard push supinated the wrist. The program for the Boston Digital Arm was modified to accept the additional electromyographic control signal inputs, accept the force sensing resistor inputs and allow simultaneous operation of all DOFs.
A final challenge with this fitting was the movement of the reinnervated pectoral muscle tissue. Because the pectoralis major insertion on the humerus had been disrupted, the various segments of muscle would pull medially during contractions, resulting in electrode sites sliding under and pulling away from the prosthetic socket. With the 3 DOF arm used at home, a custom silicone pad was fabricated and worked sufficiently. This was inadequate for the more complex 6-DOF prosthesis, therefore self-adhesive, snap electrode contactse were used for the electrodes over the pectoral muscles. Standard electrode dome contacts, mounted into the socket, were used over the medial deltoid and latissimus dorsi muscles.
Due to the prototype status, it was not possible to allow use of this device outside of the laboratory. For the results presented in this paper, testing was done over a 2-year period. Over this time period, the prosthesis has been worn for less than 100 hours spread out over 5 to 6 visits, lasting approximately 2 weeks each. Due to weight, he was only comfortable wearing the device a maximum of 4 to 6 hours a day.
Functional Testing
Multiple measures were used to compare the control of the 3 and 6-DOF prostheses. Because the motors of the prosthetic system did not have encoders available for recording the position of the arm in space, the kinematics were monitored using a passive motion capture systemf. To track 3-dimensional joint motion, 3 infrared reflective markers were placed on each rigid segment of the 6-DOF prosthesis, including the socket, the upper arm, the forearm, and the hand (fig 2). Two additional markers were placed on the tip of thumb and index finger of the prosthetic hand for calculating the hand open and close motions. In total, 14 markers were applied and each marker’s position was tracked by 6 infrared sensitive cameras at 120Hz sampling rate. The position of markers was smoothed by a 6-order Butterworth low-pass filter with the cutoff frequency at 18Hz and the joint kinematics of the prosthetic arm were calculated.11 The prostheses were compared to quantify the workspace. In order to evaluate the ability to control joints simultaneously, other tasks performed included: drawing a circle in the frontal plane with the hand, reaching out and up with the arm (to mimic retrieval of an object from a high shelf), pulling back the arm from that reaching position and coordinated movements involving hand open and close and elbow flexion and extension.
Fig. 2.
Marker configuration used in motion analysis. A total of 14 markers were used: 3 infrared reflective markers were placed on each rigid segment of the 6 function prosthesis such as the socket, the prosthetic upper-limb, the forearm, and the hand, and 2 additional markers were placed on the tip of thumb and index finger of the prosthetic hand for calculating the hand open and close motion.
Four timed tasks were performed, with both arm systems. In order to complete these tasks, different combinations of all of the available DOFs were required. A cubicle reach and retrieve test was developed consisting of 15 cubicles, containing 15 one-inch cubes, positioned on an adjustable height table (fig 3A). Before timed testing began, the subject would reach, grasp and place the 1-inch cubes on the table from as many cubicles as he was able to reach successfully, without moving his feet, thus defining the workspace to be used for the timed test. The time to grasp a 1-inch cube, place it on the table and activate a buzzer was recorded. The score consisted of the average time per successful reach and retrieval for all blocks in the workspace. A second timed task involved individually retrieving 11 plastic cups from an inverted stack and positioning them in a prescribed pyramid arrangement; 4 upside down cups on the bottom row, building up to one on the top. The final eleventh cup was placed upright on top of the top upside-down cup of the pyramid. The time required to stack the cups was recorded as was the time required to unstack the cups (fig 3B). The Box and Block test of gross manual dexterity12 required the subject to move 1-inch cubes from 1 compartment to another. This standard test was altered to increase the test interval from 60 seconds to 120 seconds (fig 3C). For the Clothespin Relocation Task, using a Rolyan Graded Pinch Exerciserg commonly found in the occupational therapy setting, the time was recorded for the subject to move 3 clothespins from a horizontal bar to a vertical bar (fig 3D). The subject’s performance of these tasks using his 3-DOF prosthesis was compared to that of the 6-DOF prosthesis.
Fig. 3.
Timed tasks: (A) cubbies, (B) cups, (C) Box and Blocks, and (D) clothespin relocation task.
RESULTS
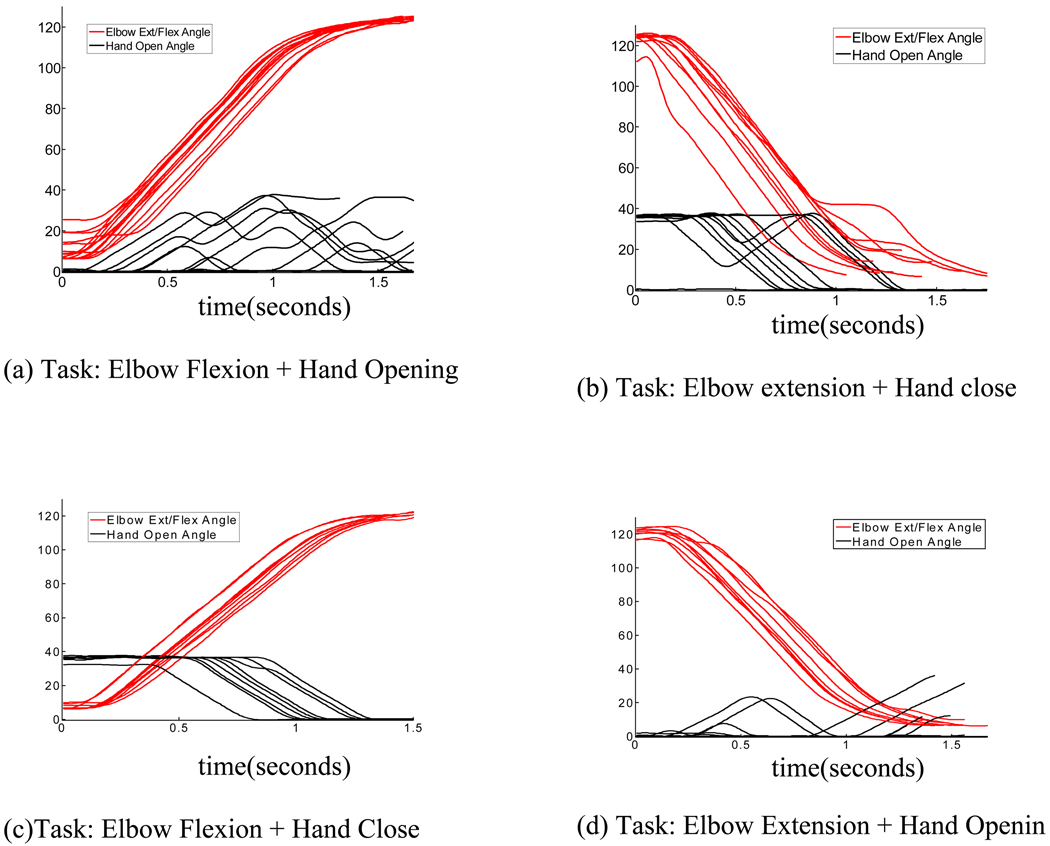
New actions were possible with the 6-DOF prosthesis. The workspace was increased in the 6-DOF arm by the ability to actively raise the shoulder, rotate the upper arm, and flex the wrist. With a conventional prosthesis a user can unlock a nonpowered shoulder, bend forward allowing shoulder flexion through gravity, and then relock the shoulder. This allows use of the prosthesis with the shoulder in a fixed angle from 0° to 90°, making reaching objects above the head difficult. The powered shoulder allowed much faster and easier operation with an operating range from −15° to 185° of flexion. The vertical work space was effectively doubled with the powered shoulder and allowed the subject to reach items above his head. The passive humeral rotator had full ROM, but obviously control was very limited and could only be manipulated by pushing the arm against objects with the arm down and the elbow flexed to approximately 90°. However, the powered humeral rotor allowed dynamic control of a full ROM. It allowed the subject to reduce compensatory movements, such as moving his torso and stand in a fixed position. More importantly, it allowed the device to cross the midline for bimanual activities and to reach parts of the right (contralateral) side of his body. The wrist flexion unit allowed the subject to bring his terminal device farther towards his body (an option not present, even passively, with the 3-DOF prosthesis). Compared to a hand without wrist flexion and extension, this hand flexed and extended approximately 60° in either direction. This amount of flexion translates to over 11cm in additional workspace in either direction. The wrist flexion and extension unit allowed better prepositioning of the hand, especially with respect to high and low surfaces. For example, this was necessary for picking up a small object off of a high shelf. Note the fully flexed wrist in figure 3A. This pick-up could not be done without this function. To evaluate overall ROM, various tasks were performed, including putting on a hat, removing items off of a shelf, and stacking items. An example of the movements for increasing the unctional workspace is shown in figure 4 (series of putting on a hat). Although putting on a baseball cap might not be a particularly important activity of daily living, it demonstrates the subject’s ability to coordinate the various DOF in a workspace related to the head and face and would thus relate to feeding and hygiene activities, while being a more engaging task. With the addition of independent control signals, one goal was to demonstrate that it was possible for the subject to control many combinations of these joints simultaneously. With the 6-DOF prosthesis, 3 of the 6 joints (wrist flexion/extension, wrist rotation, and shoulder flexion/extension) could still not be operated at the same time. Given this restriction, and with the addition of the other 3 joints able to be operated at the same time, it is possible to calculate how many combinations of simultaneous control are theoretically possible:, there were 12 possible combinations of 2 DOF at a time (eg, hand and wrist, hand and elbow), 12 combinations of 3 DOF (eg, hand, wrist, and elbow), and 3 combinations of 4 simultaneous joint movements. As seen in figures 5 through 7, the motion analysis data showed the simultaneous control of various DOFs. Although many combinations were possible only a few examples of the various 2 DOF coordinated movements were selected for testing. To demonstrate the ability to coordinate movements with the targeted reinnervation sites, trials were performed for elbow flexion and hand open, elbow extension and hand close, elbow flexion and hand close, and elbow extension and hand open (see fig 5). For this set of trials, both joints were controlled using myoelectric signals of targeted muscle reinnervation muscles. Each curve does not stop and start at the same time and some synergies are more successful than others. For example, there is inadvertent hand closing during elbow movement (see fig 4A and D). It is much easier for him to close the hand with elbow movement (fig 5B and C). Although these graphs show simultaneous control, it is also still possible for him to move the elbow without opening or closing the hand so that he does not drop items or crush fragile items. It should be noted that this coordinated hand and elbow function is also possible with the 3-DOF system.3
Fig. 4.
Images of the subject reaching to his head to put on or take off a baseball cap.
Fig. 5.
Four plots indicating the simultaneous control of elbow flexion/extension and hand open and close. Both joints were controlled by electromyographic control signal activity over targeted muscle reinnervation muscles.
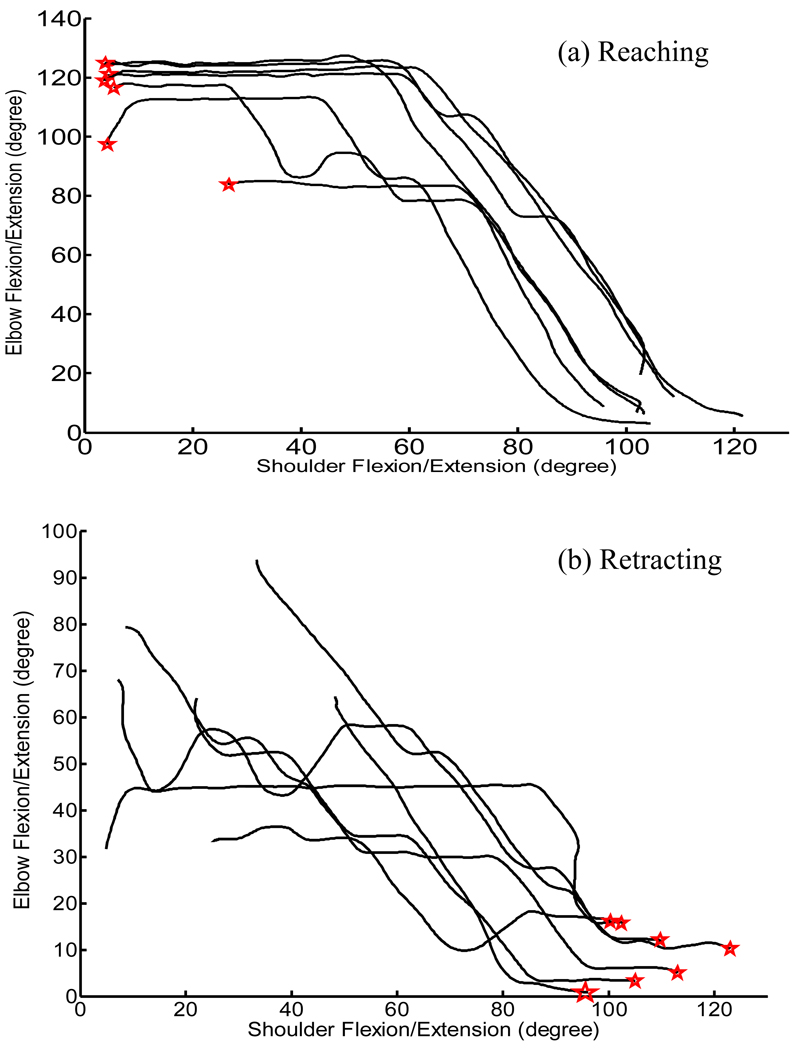
Fig. 7.
Joint phase plot between elbow flexion/extension angle and shoulder flexion/extension angle while the subject was performing (A) arm reaching up task and (B) then arm retracting. Zero in the vertical axis for elbow flexion and extension denotes full elbow extension. Horizontal and vertical lines indicate a single DOF moving, while slope areas are the phases of coactivation or joint synergy (ie, 2 joints moving together). The red stars indicate the initial joint position.
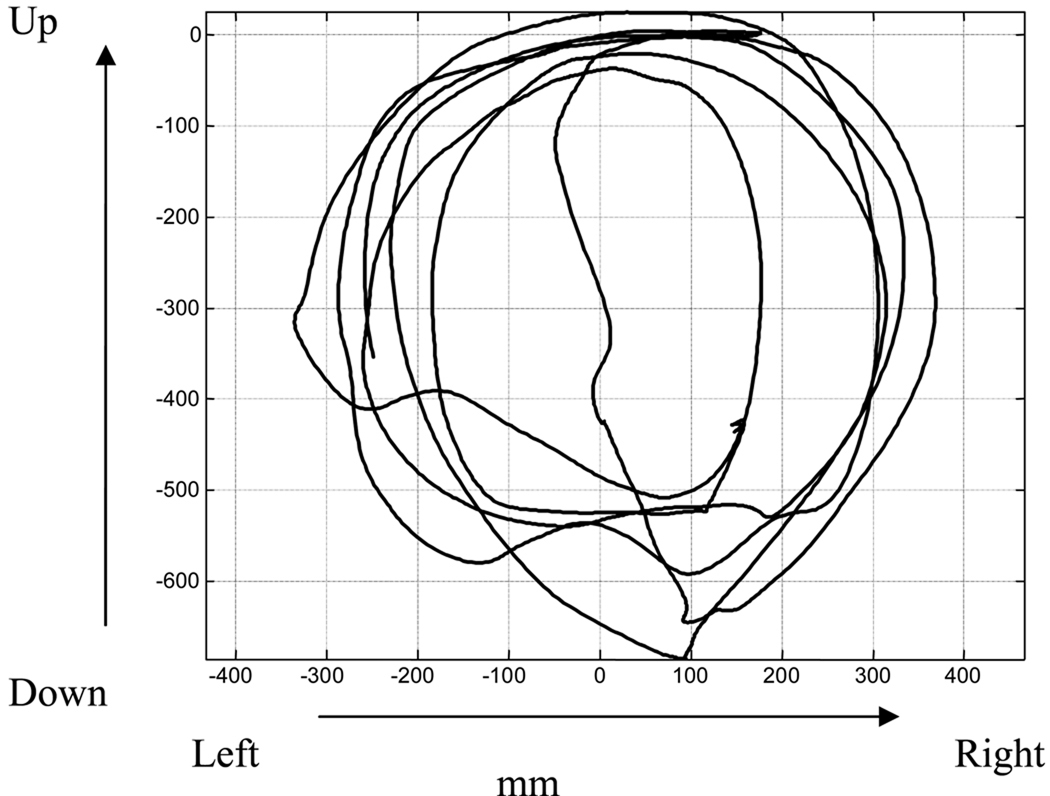
In another test the subject drew a circle in space with the hand (see fig 6); it clearly demonstrates the ability to move the humeral rotator and elbow together. Without simultaneous movement, the shape drawn would be rectangular. To eliminate the potential of body movement to influence the shape, the shoulder joint (which was not actuated by the subject in this test) was used as the center of the coordinate system in this graph. The overall time was 23.7 seconds to draw 2.5 circles clockwise and 3.5 circles counter-clockwise (1 circle took approximately 3.5s). In more functional tasks, he was also able to reach out to grasp an item. Figure 7 shows him reaching and retracting the arm. Elbow angle is shown with respect to shoulder angle. Horizontal and vertical lines indicate a single DOF moving, while areas with a slope are the points of coactivation. Although there is some independent movement, especially at the beginning and end of the movements, the coordination can be seen. It is noteworthy that the linear slope depicted in the plots indicate that the motors were operating at constant velocities during periods of these tasks. This subject had limited ability to control proportionately and, based on clinical practice, preferred the operating speeds of the motors to be capped and constant in order to improve accuracy and smoothness of movement. To achieve this, large gains were applied to the proportional DOF command signal, effectively saturating the associated voltage being sent to motors. Although the exact software settings were not recorded to verify the gains, an estimation of the actual elbow speeds during the testing (by calculating slope of these lines) was within approximately 10° per second of the manufacture’s stated specifications. The shoulder joint utilized a digital input switch, so the shoulder velocity is expected to be constant.
Fig. 6.
Frontal view of endpoint trajectory while the subject was performing circle drawing task. To remove any artifact from body movement impacting the graph, the point of reference is marker located on the shoulder (which was not actuated by the subject in this test).
Functional testing was performed with the 3- and 6-DOF arms (table 2). For the clothes-pin test, to move 1 pinch pin from the horizontal bar to the vertical bar, the subject was required to flex the shoulder forward once, then sequentially activate terminal device, elbow and wrist rotations. This test showed the subject was faster with the 6-DOF arm than the 3-DOF arm. The Box and Blocks test showed a decrease in the number of blocks moved with the 6-DOF arm. Though the main DOFs used for this test were the elbow and hand, the humeral rotator was occasionally used to move from 1 side to the other, and the wrist was kept in a flexed position to give a more functional position of the hand.
Table 2.
Results Timed Tests
| Tests | Time to Move Three Clothes Pins (s) |
Number of Blocks Moved in 120 Seconds |
Average Retrieval Time (s) |
Stacking Time for 11 Cups (s) |
Unstacking Time for 11 Cups (s) |
|---|---|---|---|---|---|
| Three-motor prosthesis | 79.2±14.3 (n=12) | 15.0±.1 (n=15) | 18.6±2.5 (n=3) | 169±58 (n=3) | 83±13 (n=3) |
| Six-motor prosthesis | 58.0±9.2 (n=3) | 13.7±2.5 (n=3) | 15.3±9.5 (n=4) | 357±36 (n=3) | 89±29 (n=3) |
NOTE: Results include the time to move 3 clothes pins from a horizontal bar to a vertical bar, the number of blocks moved from 1 side of a divider to the other in 120s, the average retrieval time for the cubical workspace (see text for identification of workspace) and the stacking and unstacking times for 11 plastic cups. Units are listed above each column and 1 SD is listed after the average. The number of trials is indicated as n.
The ROM for the cubicle evaluation test was greater with the 6-DOF device due to the shoulder and wrist motors. With the 3-DOF prosthesis, he was only able to access 12 of the cubbies, while with the 6-DOF device he was able to access all 15. Even with the increased workspace, the time per cubby was approximately the same.
Using the 6-DOF compared to the 3-DOF prosthesis, the cup stacking exercise showed an increase in the amount of time required to stack all 11 cups into an inverted pyramid, though the times for unstacking were almost the same.
The subjective opinions were supportive of a commercial device that would provide these DOFs. Often, during repeat visits to the lab for testing, the subject was asked which additional motor he would choose if he had to pick one. This was not an easy choice for him. His comments regarding the wrist flexion unit are that it would be necessary if he was ever to use a hand. The Greifer hook that he has on his home prosthesis has similar movement (radial/ulnar deviation) as a passive DOF, and the orientation of the grasping surface is better oriented to picking items off of a flat surface. Though he often said the shoulder joint was the one he would use the most, he relayed that when using his 3-DOF home prosthesis he would often catch himself trying to actuate the humeral rotator. This was the motor he said he most often inadvertently tried to use with the home prosthesis.
DISCUSSION
The targeted reinnervation technique creates new electromyographic control signals for more complex prosthetic systems. With little training, this subject and others have demonstrated an ability to operate a prosthesis using these additional electromyographic control signals added through the nerve transfers. 3–7
This study provides an exciting demonstration of the multiple DOF control that is possible by combining targeted muscle reinnervation electromyographic control signals, residual limb electromyographic control signals and conventional shoulder switches and force sensing resistors. With this new device the subject was able to easily control 2 DOF simultaneously in many different combinations. Control of 3 DOFs was not quantified but clinically observed. Three DOFs seemed harder to control concurrently, but were possible for gross movements such as reaching out with the arm (elbow and shoulder) while opening the hand. Additionally, simultaneous actuation of 4 DOFs was theoretically possible but rarely done because the device does not provide any proprioceptive feedback and positioning this many DOFs required significant cognitive demands. It is acknowledged that this is not an ideal control system and that the cognitive demand is still great. This is confirmed by the fact that the subject rarely used more than 2 motors at a time, even though it was theoretically possible for him to operate 4 and he preferred to use the limbs at relatively slow speeds. This demand will undoubtedly remain great for high level amputees due to the lack of proprioceptive feedback and the need to use visual feedback to place the device. However, this may not negate the benefits of additional control signals with more physiologically appropriate control. Although the subject might not consistently exhibit simultaneous control of the larger number of motors, the ease of physiologically appropriate myoelectric control was likely beneficial in the fluidity of seamless sequential movements that could be observed with use. This work clearly demonstrated that patients are able to control many more than the 3 DOFs that are available on current devices. While the current system is too complex for broad clinical application, it is clear the patients could robustly control a subset of the 6 DOFs such as adding just a wrist flexion/extension component or a powered shoulder flexion/extension component. This work also motivates the development of more advanced prostheses for commercial use.
The subject preferred the speed of the motors to be relatively slow. This gave him greater accuracy. In many tasks, especially larger movement tasks, the subject appeared to quickly hit the maximum speed of the functions being controlled. This is particularly apparent in figures 5 and 7. Much of the time the relative speed of the 2 movements are constant as depicted with a straight slope; this is likely due to both DOFs operating at their maximum speed. Clearly the subject can operate 2 functions simultaneously at less then maximal speed. This is depicted well in figure 6 where the subject was able to draw a very good circle using the elbow and humeral rotator in combination.
The increased cognitive demands in part came from the need to control 3 of the DOFs using 1 dual-action rocker switch and 2 bidirectional force sensing resistors. Considerable effort was required on the part of the subject to properly aim the shoulder at 4 separate switches with the correct pressure in order to allow the arm to function in the intended way. Further research is being explored on how to better use the motion of the shoulder to control movements, since the current design clearly has too many functions controlled with the residual shoulder. Ideally, only shoulder functions would be controlled with shoulder movement. This would be more physiologically appropriate and intuitive.
The 6-DOF arm allowed the subject to perform many tasks that were not possible with the 3-DOF system such as high reaching, pushing up his glasses, and donning a hat. The powered shoulder facilitated the increased work space in the environment, but the wrist flexion/extension function was critical for prepositioning the hand and being able to functionally use the increased workspace. The humeral rotator allowed the workspace to include the subject’s body; this is very important for activities such as dressing, hygiene and simple, but important, tasks like scratching ones own nose.
In functional testing, times were not consistently less for the 6-DOF system over the 3-DOF system. A few possible explanations exist. The increase in cognitive demands required for controlling these additional functions likely slowed operation. Another issue is that the subject was often able to accomplish the same gross positioning movements of the powered shoulder through trunk movement and knee flexion. For example, during cup stacking experiments while using the 3-DOF arm, he would manually move the shoulder up, and leave it in that locked position; when he needed the arm lower, he would then bend at the waist and bend his knees. Although this movement was faster, it required greater physical effort and made use of the device appear less natural. For activities where such trunk and knee movement would not be possible (eg, if sitting or otherwise constrained), the 3-DOF device would be less functional. The subject had much less practice with the 6-DOF arm since his use of this device was limited to time spent in the laboratory. Conversely, the 3-DOF system was used on a regular basis at home. Finally, for tasks that only required use the hand, wrist rotation, and elbow, the extra functions of the 6 function arm allowed joints to be mistakenly activated and slow performance. For example, the blocks and box test only required the use of the hand and elbow, thus inadvertent wrist or shoulder movement slowed performance.
The powered shoulder and humeral rotator clearly had functional value to this subject by increasing his access to high objects. Similarly the humeral rotator allowed him to work the midline space of his body with great ease. His appreciation for these joints may be due to the fact that he has bilateral upper-limb loss and cannot reach high objects or work in his midline well with a sound limb. The relative value of these functions which add weight and complexity remains to be determined with unilateral amputees that can compensate with a sound limb to a large extent.
The amount of control demonstrated by our subject in this study was remarkable. Because of the concentration and practice needed to operate 2 force sensing resistors and a rocker with the shoulder to control 3 different DOFs, he is clearly an exceptional user, and we would not expect a typical user to be so adept with such limited wear time. For a 6 DOF upper-limb prosthesis to be clinically viable an easier, a more intuitive control system must be developed and move away from using of the shoulder to control wrist movements. One way to potentially improve control is to use advanced electromyographic signal processing techniques such as pattern recognition algorithms.13 The targeted muscle reinnervation electromyographic contains much more information than just open and close hand and flex and extend elbow. Motoneurons of wrist, thumb, and finger muscles reinnervate the target muscle and this information is embedded in the surface electromyographic. Using pattern recognition techniques we have been able to extract control information related to wrist, finger, and thumb movements.14 This will hopefully provide an easy and intuitive method for users to control a prosthetic wrist with 2 or 3 DOFs and multifunction hands that provide the user a choice of many different hand-grasp patterns.
Study Limitations
Better prostheses are also needed. This 6-DOF prosthesis is only an experimental device and not described as a potentially clinically viable product: it is too heavy (≈5.75kg), it is not durable and the battery life is a 2 to 3 hours when used during these tests, and new socket/electrode systems are an area of current research since self-adhesive electrodes are not a clinically viable solution. The purpose of this work was to demonstrate that more functions can be controlled in a useful way. Since only 3 powered functions are commercially available—elbows, wrist rotators, and terminal devices, hopefully this work gives a greater impetus for developing commercial devices with greater dexterity for individuals with upper-limb amputation.
CONCLUSIONS
With the use of targeted reinnervation electromyographic control signal sites, residual limb electromyographic control signal sites and shoulder switches, and force sensing resistors, this subject was able to demonstrate good control of a prosthetic arm with 6 DOFs. Although these components and the current configuration would not be a clinically viable system because they are not sufficiently robust, it has been shown that the additional DOFs can effectively be controlled in a simultaneous and functional manner. With additional control inputs made available through targeted reinnervation, there now exists increased incentive to develop more advanced components that will allow those people with high level amputations, especially bilateral amputees, to improve their functional abilities and independence.
Acknowledgments
Grant & Financial Support
This work was supported by the NIH National Institute of Child and Human Development (Grant # R01 HD043137-01) and the Keiser Family Foundation
List of Abbreviations
- DOF
degree of freedom
- EMG
electromyography
- ROM
range of motion
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Partially reported at the Myoelectric Controls Symposium, New Brunswick, Canada, August 2005 and the 12th World Congress of the International Society for Prosthetics and Orthotics (ISPO), Vancouver, July 29-August 3, 2007.
We certify that we have affiliations with or financial involvement (eg, employment, consultancies, honoraria, stock ownership or options, expert testimony, grants and patents received or pending, royalties) with an organization or entity with a financial interest in, or financial conflict with, the subject matter or materials discussed in the manuscript AND all such affiliations and involvements are disclosed on the title page of the manuscript.
T. Walley Williams III is an employee of Liberating Technologies, Inc, maker of the Boston Digital Arm, used in this study. This component was purchased by the Neural Engineering Center for Artificial Limbs from Liberating Technologies, Inc for this study.
The Neural Engineering Center for Artificial Limbs and Liberating Technologies, Inc have applied for an SBIR together.
We certify that no other party has a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified.
Presented to the Myoelectric Controls Symposium, August 2005, New Brunswick, Canada, and the International Society for Prosthetics and Orthotics, July 29–August 3, 2007, Vancouver, BC, Canada.
A commercial party having a direct financial interest in the results of the research supporting this article has conferred or will confer a financial benefit on the author or one or more of the authors. Williams III is an employee of Liberating Technologies, Inc, maker of the Boston Digital Arm, used in this study. This component was purchased by the Neural Engineering Center for Artificial Limbs from Liberating Technologies, Inc for this study.
Suppliers
Liberating Technologies Inc, 325 Hopping Brook Rd, Ste A, Holliston, MA, 01746-1456.
Otto Bock Healthcare, 2 Carlson Pkwy, Ste 100, Minneapolis, MN 55447-4467.
Touch Bionics, Unit 3, Ashwood Ct, Oakbank Park Way, Livingston, EH53 0TH UK.
MH22 hand; Shanghai Keshen Artificial Limb Co, No 527, Maotai Rd, Changning, Shanghai, 200336 China.
Noraxon Dual Electrodes; Noraxon USA Inc, 13430 N Scottsdale Rd #104, Scottsdale, AZ, 85254.
Motion Analysis Corp, 3617 Westwind Blvd, Santa Rosa, California 95403.
Roylan Graded Pinch Excerciser; Sammons Preston, PO Box 5071, Bolingbrook, IL 60440-5071.
REFERENCES
- 1.Kuiken TA. Consideration of nerve-muscle grafts to improve the control of artificial arms. J Technol Disabil. 2003;15:105–111. [Google Scholar]
- 2.Hoffer JA, Loeb GE. Implantable electrical and mechanical interfaces with nerve and muscle. Ann Biomed Eng. 1980;8:351–360. doi: 10.1007/BF02363438. [DOI] [PubMed] [Google Scholar]
- 3.Kuiken TA, Dumanian GA, Lipschutz RD, Miller LA, Stubblefield KA. The use of targeted muscle reinnervation for improved myoelectric prosthesis control in a bilateral shoulder disarticulation amputee. Prosthet Orthot Int. 2004;28:245–253. doi: 10.3109/03093640409167756. [DOI] [PubMed] [Google Scholar]
- 4.Hijjawi JB, Kuiken TA, Lipschutz RD, Miller LA, Stubblefield KA, Dumanian GA. Improved myoelectric prosthesis control accomplished using multiple nerve transfers. Plast Reconstr Surg. 2006;118:1573–1578. doi: 10.1097/01.prs.0000242487.62487.fb. [DOI] [PubMed] [Google Scholar]
- 5.Lipschutz RD, Kuiken TA, Miller LA, Dumanian GA, Stubblefield KA. Shoulder Disarticulation Externally Powered Prosthetic Fitting Following Targeted Muscle Reinnervation for Improved Myoelectric Control. J Prosthet Orthot. 2006;18:28–34. doi: 10.3109/03093640409167756. [DOI] [PubMed] [Google Scholar]
- 6.Kuiken TA, Miller LA, Lipschutz RD, et al. Targeted reinnervation for enhanced prosthetic arm function in a woman with a proximal amputation: a case study. Lancet. 2007;369:371–380. doi: 10.1016/S0140-6736(07)60193-7. [DOI] [PubMed] [Google Scholar]
- 7.O'Shaughnessy KD, Dumanian GA, Lipschutz RD, Miller LA, Stubblefield KA, Kuiken TA. Targeted reinnervation to improve prosthesis control in transhumeral amputees: a report of three cases. J Bone Joint Surg Am. 2008;90:393–400. doi: 10.2106/JBJS.G.00268. [DOI] [PubMed] [Google Scholar]
- 8.Weir RF, Grahn EC. Powered humeral rotator for persons with shoulder disarticulation amputations; Proceedings of the Myoelectric Control Symposium; Fredericton (Canada): 2005. [Google Scholar]
- 9.Zhou P, Kuiken TA. Eliminating cardiac contamination from myoelectric control signals developed by targeted muscle reinnervation. Physiol Meas. 2006;27:1311–1327. doi: 10.1088/0967-3334/27/12/005. [DOI] [PubMed] [Google Scholar]
- 10.Miller LA, Lipschutz RD, Weir RF, et al. Shoulder Disarticulation Fitting With 6 Independently controlled motors after targeted hyper-reinnervation nerve transfer surgery; Proceedings of the Myoelectric Controls Symposium; New Brunswick (Canada): 2005. [Google Scholar]
- 11.Huang H. Development of a novel immersive and interactive therapeutic tool for neurorehabilitation. Tempe: Arizona State Univ Pr; 2006. [Google Scholar]
- 12.Mathiowetz V, Volland G, Kashman N, Weber K. Adult norms for the Box and Block Test of manual dexterity. Am J Occup Ther. 1985;39:386–391. doi: 10.5014/ajot.39.6.386. [DOI] [PubMed] [Google Scholar]
- 13.Englehart K, Hudgins B. A robust, real-time control scheme for multifunction myoelectric control. IEEE Trans Biomed Eng. 2003;50:848–854. doi: 10.1109/TBME.2003.813539. [DOI] [PubMed] [Google Scholar]
- 14.Zhou P, Englehart K, Lowery MM, Kuiken TA. Classification of high density surface electromyographic signals developed by targeted muscle reinnervation; Proceedings of the 16th Congress of the International Society of Electrophysiological Kinesiology; Torino (Italy): 2006. [Google Scholar]