Abstract
Purpose
To compare the clinical outcome of different multifocal intraocular lenses (IOLs) based on information reported in the international literature.
Methods
All comparative clinical trials that involved implanting at least one multifocal IOL in patients with cataract or presbyopia were extracted from the literature. Clinical outcomes included uncorrected near visual acuity, uncorrected distance visual acuity, visual acuity, spectacle independence, and halos. Random effects meta-analyses were conducted to compare outcomes for the different IOL types.
Results
Twenty papers were identified describing 11 monofocal IOLs and 35 multifocal IOLs (19 diffractive, including 12 ReSTOR®, 14 refractive, and two accommodative) patient cohorts. Multifocal and monofocal uncorrected distance visual acuity was 0.165 (0.090–0.240) and 0.093 (0.088–0.098), respectively. Compared with monofocal IOLs, multifocal IOLs produced better uncorrected near visual acuity (0.470 [0.322–0.618] versus 0.141 [0.131–0.152]; P < 0.0001), resulting in higher spectacle independence (incidence rate ratio [IRR] 3.62 [2.90–4.52]; P < 0.0001). Compared with refractive multifocal IOLs, diffractive multifocal IOLs produced a similar uncorrected distance visual acuity (0.105 [0.098–0.111] versus 0.085 [0.029–0.140]; P ≤ 0.78, not significant) and better uncorrected near visual acuity (0.217 [0.118–0.317] versus 0.082 [0.067–0.098]; P < 0.0001) resulting in higher spectacle independence (IRR 1.75 [1.24–2.48]; P < 0.001). Compared with other multifocal IOLs, ReSTOR produced a better uncorrected distance visual acuity (0.067 [0.059–0.076] versus 0.093 [0.088–0.098]; P < 0.0001) and better uncorrected near visual acuity (0.064 [0.046–0.082] versus 0.141 [0.131–0.152]; P < 0.006), resulting in higher spectacle independence (IRR 2.06 [1.26–1.36]; P < 0.004). Halo incidence rates with different types of multifocal implants did not differ significantly.
Conclusion
Multifocal IOLs provide better uncorrected near visual acuity than monofocal IOLs, leading to less need for spectacles. Multifocal IOL design might play a role in postsurgical outcome, because better results were obtained with diffractive lenses. ReSTOR showed better uncorrected near visual acuity, uncorrected distance visual acuity, and higher spectacle independence rates compared with other multifocal IOLs.
Keywords: multifocal implants, meta-analysis, uncorrected near visual acuity, uncorrected distance visual acuity, spectacle independence, patient satisfaction
Introduction
An estimated 20.5 million Americans older than 40 years have cataract in at least one eye.1 While cataract is the leading cause of blindness worldwide,2,3 most populations in developed Western countries have access to cataract surgery (eg, 6.1 million [5.1%] of American citizens have pseudophakia/aphakia). The total number of Americans with cataract is predicted to increase to 30.1 million by 2020, of whom 9.5 million are expected to have pseudophakia.1 More than 80% of patients regain good best-corrected visual acuity (visual acuity ≥ 8/10) after cataract surgery, depending on other ocular pathology and duration of follow-up.4–8
Traditional intraocular lenses (IOLs) are monofocal, and after implantation most patients need spectacles, at least for near vision. Multifocal IOLs are intended to free patients from spectacles after presbyopia or cataract surgery by applying the principle of simultaneous vision.9 Early multifocal IOLs were associated with loss of clarity and poor accommodation, reduced contrast sensitivity, and complaints of halos and glare. Improvements in intraocular lens technology have enabled cataract patients to be implanted with multifocal IOLs to provide better visual acuity at various distances and a degree of spectacle independence.10
Today, multifocal IOLs produce functional near and distance vision and acceptable levels of patient satisfaction in everyday practice.11–14 However, reviews on the clinical consequences of multifocal implantations are rare.15
Many IOL clinical trials have been performed, but to our knowledge, no relevant meta-analysis has been reported. Our objective was to conduct a meta-analysis of published comparative clinical trials in which at least one patient group was implanted with multifocal implants bilaterally.
Materials and methods
Bibliographic research
An extensive literature review was performed through Medline and most recently updated on June 30, 2009. The following multifocal IOL names were used as keywords: Acrilisa® (Carl Zeiss Meditec, La Rochelle, France), Diffractiva® (HumanOptics, Erlangen, Germany), Rayner® (Rayner Intraocular Lenses Ltd., Hove, UK), ReSTOR® (Alcon Inc., Fort Worth, TX), Rezoom® (Abbott Medical Optics, Santa Ana, CA), and Tecnis® (Abbott Medical Optics), together with keywords focusing on comparative clinical trials, ie, “cataract surgery”, “comparison”, “multifocal”, and “visual acuity”. Abstracts were scrutinized and full articles ordered and analyzed in depth if they reported comparative studies in adult patients.
Inclusion criteria were publication in the French or English language, bilateral implantation of the same IOL, use of Tecnis, Acrilisa, Rezoom, Diffractiva, Rayner, or ReSTOR implants, and publication from 2000 onwards.
Exclusion criteria included comparison of different populations, double implantation in the same eye, double reporting, explantation of the implant, in vitro studies, no aggregated results, noncomparative studies, unilateral implantation, and use of a refractive procedure (eg, Lasik).
All available data from the selected articles were extracted and tabulated with respect to each study’s identity, its design (prospective or retrospective, randomized or not randomized), IOL names and type (monofocal or multifocal; diffractive or refractive), reasons for IOL implantation, number of patients at baseline and at final follow-up, average follow-up duration, final overall patient satisfaction, spectacle dependency, uncorrected distance visual acuity, uncorrected intermediate visual acuity, uncorrected near visual acuity, and the number of patients reporting “halos”.
Data analysis
Outcome variables of the study were as follows:
Uncorrected distance and near visual acuities converted to LogMAR equivalents, as described in detail elsewhere,16 when expressed in a different unit.
Freedom from spectacles (independence), separately analyzed for distance and reading spectacles. It should be noted, however, that most studies combined all types of spectacles to express an overall need for spectacles, instead of providing specific information on distance versus reading spectacles.
Patient satisfaction; given that variations between studies existed, to assess patient satisfaction, we standardized measurements according to the range of the measurements reported in each study.
Presence of halo, which was reported using various definitions among the studies. Prevalence (presence versus absence of halos) was reported in this study.
We compared the aforementioned outcomes for the following subgroups of IOL implants: monofocal versus multifocal implants; diffractive versus refractive multifocal implants (data were insufficient to assess the effects of accommodative implants separately); and ReSTOR versus other multifocal implants. ReSTOR outcomes were highlighted because they relate to a new type of multifocal apodized IOL.
Statistical analysis
We used random effects models17,18 to obtain pooled estimates of visual acuity with 95% confidence intervals (CI), and tested for statistically significant differences between the estimates with respect to each IOL subgroup.
We used random effects Poisson regression models to compare the effect of IOL implant type on the need for spectacles. The outcome of interest was the number of patients needing spectacles, with study effects taken into account by the random effects component of the models. The exposure variable for the Poisson models was defined as the product of the number of patients receiving a given implant and the average period of follow-up for each study. Similarly, we used random effects Poisson regression models to compare overall patient satisfaction and the presence of halo across subgroups of implants.
Forest plots were used to present the results. The lines represent the estimates from different studies and their CI. The boxes represent graphically the weight given to each study in calculating the pooled estimate for a given outcome. This weight is essentially a function of the number of patients followed up in different studies.
Results
Bibliographic research
Initial electronic searches identified 197 titles or abstracts. Complete copies of all possibly relevant papers were obtained, according to the criteria specified earlier. Fifty-one papers appeared to meet the inclusion criteria for this review.
Twenty of the 51 studies were included in the metaanalysis. The excluded 31 papers finally did not meet the inclusion and exclusion criteria. Reasons for exclusion were, as follows: a different IOL in each eye (n = 7); reimplantation in one eye (n = 1); no comparison IOL (n = 6); double reporting (n = 4); comparison of different populations (n = 1); comparisons of monofocal IOLs (n = 2); either no data or aggregated data (n = 8); results after Lasik or another procedure (n = 2); and in vitro results (n = 1).
Descriptive data analysis
Twenty studies were included in the meta-analysis,19–38 of which 16 were prospective studies (80%) and four were retrospective (Table 1). Eight (50%) of the prospective studies were randomized. Data were collected from 46 patient groups, comprising 35 multifocal implant groups (76.1%) and 11 monofocal implant groups (23.9%). Among the multifocal implant groups, 19 were implanted with diffractive IOLs, 14 with refractive IOLs, and two with accommodative IOLs. ReSTOR was implanted in 12 of these groups (34.3%). Accommodative implants were studied in 26 patients only, and so were not analyzed as a specific group. Uncorrected distance vision acuity was described for 30 groups and near vision acuity for 23 groups.
Table 1.
Characteristics, references, and available results of the published studies
| Reference | Design | IOL | Trt | Satisfaction | Spectacle classification | Halo |
|---|---|---|---|---|---|---|
| Bi et al19 | P | ReSTOR vs Acrysof | N | Satisfaction with reading acuity | Spectacle independence | N |
| SN60AT | ||||||
| Chiam et al20 | P | ReSTOR vs Rezoom | Y | Overall satisfaction | Spectacle independence | Y |
| Toto et al21 | P | ReSTOR vs Tecnis | Y | N | ||
| Souza et al22 | P | ReSTOR vs Acrysof | N | Y | ||
| SA60AT | ||||||
| Vingolo et al23 | R | ReSTOR vs Acrysof | n.m. | Spectacle independence | Y | |
| SA60AT | ||||||
| Alfonso et al24 | P | ReSTOR SA60D3 vs ReSTOR SN60D3 | N | Overall satisfaction | Near distance spectacle independence | N |
| Chiam et al25 | P | ReSTOR vs Acrysof | n.m. | % of patients completely or very satisfied | Spectacle independence | Y |
| SA60AT | ||||||
| Pepose et al26 | P | ReSTOR vs Rezoom vs Crystalens | N | % of patients completely or very satisfied | Near and distance spectacle independence | N |
| Mester et al27 | P | Tecnis vs Array | Y | % of patients completely or very satisfied | Spectacle independence | Y |
| Brydon et al28 | R | Array vs SI-30NB | N | VF14 index | N | |
| Chen et al29 | R | Monofocal Acrysof vs Array | N | % of patients satisfied with results | Spectacle independence | N |
| Sen et al30 | P | Array vs SI-40NB | Y | % of patients completely or very satisfied | Y | |
| Javitt et al31 | P | Array vs AMO | Y | Satisfaction level graded from 0 to 10 | Spectacle independence | N |
| Cochener et al38 | P | ReSTOR vs Acrysof | N | Spectacle independence | Y | |
| MA60BM | ||||||
| Alio et al37 | P | Crystalens (AT45) vs Array SA40N vs Acritec twinset | N | Y | ||
| Cillino36 | P | AR40 (AMO) vs Array SA40N vs Rezoom (AMO) vs Tecnis ZM900 | Y | Overall satisfaction | Full spectacle independence | Y |
| Zelichowska et al35 | R | ReSTOR SN60D3 vs Rezoom | n.m. | N | ||
| Barisic et al34 | P | Tecnis multifocal vs Rezoom | Y | Spectacle independence | N | |
| Chang-David33 | P | ReSTOR vs Rezoom | N | Spectacle independence | Y | |
| Martinez-Palmer et al32 | P | Tecnis Z9000 vs Tecnis ZM900 vs Rezoom vs Acritec twinset | Y | Full spectacle independence | N |
Abbreviations: n.m., not mentioned; P, prospective; R, retrospective; Trt, treatment affected at random; vs, versus; Y, yes; N, no; IOL, imtraocular lens implant.
All except six publications reported patient satisfaction as percentages of patients “satisfied” or “very satisfied”. Four papers isolated “patient satisfaction with vision” from a broader assessment of “overall satisfaction”. One paper rated satisfaction on a scale from 0 to 10 (maximal satisfaction). Finally, one paper used a questionnaire yielding a global measure of overall satisfaction that included a validated “VF-14 index of visual function”.
Fourteen (70%) of the 20 publications assessed spectacle independence, expressed in most cases as the number, or percentage, of patients who at the end of the follow-up period needed spectacles for reading or distance vision. Other studies asked patients how often they wore spectacles and gave them the response options of “always”, “occasionally”, or “never”. Distance vision (spectacle independence) was not stated by 10 studies, and only four studies gave both distance and near vision, by indicating patients requiring the respective correction spectacles. Visual disturbances, which could be night-time halos, moderate halos, or severe halos, were reported by 10 studies (50%). Table 2 summarizes the characteristics of all 20 publications included in this metaanalysis and provides references to them.
Table 2.
Characteristics of the implants included in the 20 articles
| # | Reference | IOL | Type | MIOL type | Follow-up (weeks) | Patients (n) |
|---|---|---|---|---|---|---|
| 3 | Bi et al19 | ReSTOR | MIOL | Diffractive | 12 | 20 |
| Acrysof | Mono | 12 | 18 | |||
| SN60AT | ||||||
| 5 | Chiam et al20 | ReSTOR | MIOL | Diffractive | 24 | 50 |
| Rezoom | MIOL | Refractive | 24 | 50 | ||
| 8 | Toto et al21 | ReSTOR | MIOL | Diffractive | 24 | 14 |
| Tecnis ZM 900 | MIOL | Diffractive | 24 | 14 | ||
| 9 | Souza et al22 | ReSTOR | MIOL | Diffractive | 16 | 24 |
| Acrysof | Mono | 16 | 15 | |||
| SA60AT | ||||||
| 10 | Vingolo et al23 | ReSTOR | MIOL | Diffractive | 24 | 50 |
| SA60D3 | ||||||
| Acrysof | Mono | 24 | 20 | |||
| SA60AT | ||||||
| 11 | Alfonso et al24 | ReSTOR | MIOL | Diffractive | 24 | 325 |
| SA60D3 | ||||||
| ReSTOR | MIOL | Diffractive | 24 | 335 | ||
| SN60D3 | ||||||
| 19 | Blaylock41 | ReSTOR | MIOL | Diffractive | 8 | 40 |
| SN60D3 | ||||||
| Acrysof | Mono | 8 | 40 | |||
| SA60AT | ||||||
| 25 | Pepose et al26 | ReSTOR | MIOL | Diffractive | 20 | 12 |
| Rezoom | MIOL | Refractive | 20 | 14 | ||
| Crystalens (AT45) | MIOL | Accommodative | 20 | 14 | ||
| 32 | Mester et al27 | Tecnis ZM900 | MIOL | Diffractive | 24 | 23 |
| Array SA40 | MIOL | Refractive | 24 | 24 | ||
| 36 | Brydon et al28 | Array (SA40N) | MIOL | Refractive | 11 | 15 |
| SI-30NB | Mono | 10 | 13 | |||
| 38 | Chen et al29 | Monofocal | Mono | nm | 20 | |
| Acrysof | ||||||
| Array | MIOL | Refractive | nm | 20 | ||
| 41 | Sen et al30 | Array (SA40N) | MIOL | Refractive | 4 | 35 |
| SI-40NB | Mono | 4 | 40 | |||
| 43 | Javitt et al31 | Array (SA40N) | MIOL | Refractive | 12 | 123 |
| PhacoFlex | Mono | 12 | 109 | |||
| SI40NB | ||||||
| 53 | Cochener et al38 | ReSTOR | MIOL | Diffractive | 21 | 499 |
| Acrysof | Mono | 21 | 173 | |||
| MA60BM | ||||||
| 55 | Alio et al37 | Crystalens AT45 | MIOL | Accommodative | 48 | 12 |
| Array SA40N | MIOL | Refractive | 48 | 16 | ||
| Acritec twinset | MIOL | Diffractive | 48 | 12 | ||
| 56 | Cillino et al36 | AR40 (AMO) | Mono | 48 | 15 | |
| Array SA40N | MIOL | Refractive | 48 | 16 | ||
| Rezoom (AMO) | MIOL | Refractive | 48 | 15 | ||
| Tecnis ZM900 | MIOL | Diffractive | 48 | 16 | ||
| 57 | Zelichowska et al35 | ReSTOR | MIOL | Diffractive | 24 | 23 |
| SN60D3 | ||||||
| Rezoom | MIOL | Refractive | 24 | 23 | ||
| 59 | Barisic et al34 | Tecnis multifocal | MIOL | Diffractive | 24 | 50 |
| Rezoom | MIOL | Refractive | 24 | 50 | ||
| 60 | Chang-David33 | ReSTOR | MIOL | Diffractive | 24 | 15 |
| Rezoom | MIOL | Refractive | 24 | 15 | ||
| 61 | Martinez-Palmer et al32 | Tecnis Z9000 | Mono | 12 | 24 | |
| Tecnis ZM900 | MIOL | Diffractive | 12 | 26 | ||
| Rezoom | MIOL | Refractive | 12 | 32 | ||
| Acritec twinset | MIOL | Diffractive | 12 | 32 |
Abbreviations: IOL, intraocular lens implant; MIOL, multifocal intraocular lens implant; nm, not mentioned.
Visual acuity
Table 3 shows pooled estimates of random effects, with 95% CI, for uncorrected distance and near visual acuity (LogMAR scale) after monofocal and multifocal IOL implants. Separate estimates are shown for diffractive and refractive multifocal implants and for ReSTOR.
Table 3.
Characteristics of the 46 groups
| Patients (n) (total patients) | Follow-up (weeks) | Average UDVA (LogMAR) | Average UNVA (LogMAR) | Satisfaction rate | Need for spectacle (all spectacles) | |
|---|---|---|---|---|---|---|
| Monofocal groups | (486) | |||||
| n | 11 | 10 | 5 | 5 | 8 | 7 |
| Mean # of patients (SD) | 44.3 (50.8) | 16.9 (12.4) | 0.27 (0.25) | 0.47 (0.124) | 0.8 (0.23) | 0.78 (0.22) |
| (min–max) | (13–273) | (4–48) | (0.11–0.7) | (0.3–0.61) | (0.31–0.99) | (0.45–0.96) |
| Multifocal groups | (2055) | |||||
| n | 35 | 34 | 25 | 18 | 23 | 19 |
| Mean (SD) | 58.7 (106.5) | 24.4 (12.5) | 0.09 (0.08) | 0.15 (0.098) | 0.87 (0.08) | 0.31 (0.2) |
| (min–max) | (12–499) | (4–48) | (−0.066–0.245) | (0.013–0.403) | (0.64–0.99) | (0.08–0.67) |
| Diffractive groups | (1580) | |||||
| n | 19 | 19 | 14 | 9 | 11 | 11 |
| Mean (SD) | 83.2 (139.3) | 23 (10.3) | 0.109 (0.065) | 0.091 (0.054) | 0.90 (0.06) | 0.2 (0.13) |
| (min–max) | (12–499) | (8–48) | (0.03–0.245) | (0.013–0.156) | (0.82–0.99) | (0.08–0.56) |
| Refractive groups | (448) | |||||
| n | 14 | 13 | 9 | 7 | 11 | 8 |
| Mean (SD) | 32 (29) | 24.8 (14.7) | 0.074 (0.088) | 0.232 (0.099) | 0.93 (0.09) | 0.47 (0.14) |
| (min–max) | (14–123) | (4–48) | (−0.066–0.207) | (0.11–0.403) | (0.64–0.94) | (0.3–0.67) |
| ReSTOR groups | (1408) | |||||
| n | 12 | 12 | 8 | 7 | 8 | 6 |
| Mean (SD) | 117.3 (168) | 20.5 (5.5) | 0.069 (0.031) | 0.08 (0.055) | 0.9 (0.07) | 0.16 (0.06) |
| (min–max) | (12–499) | (8–24) | (0.03–0.13) | (0.013–0.15) | (0.82–0.99) | (0.08–0.27) |
Abbreviations: UDVA, uncorrected distance visual acuity; UNVA, uncorrected near visual acuity; SD, standard deviation; min, minimum; max, maximum.
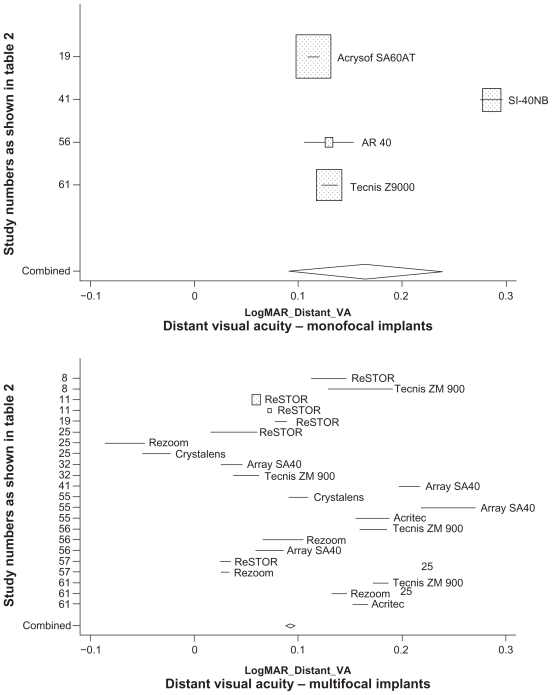
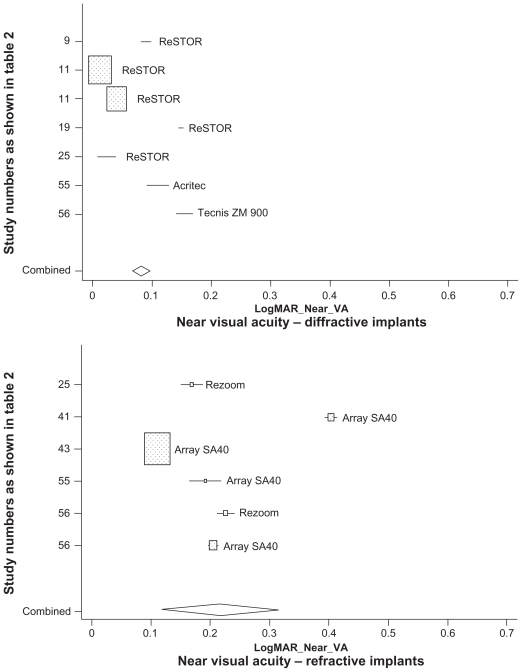
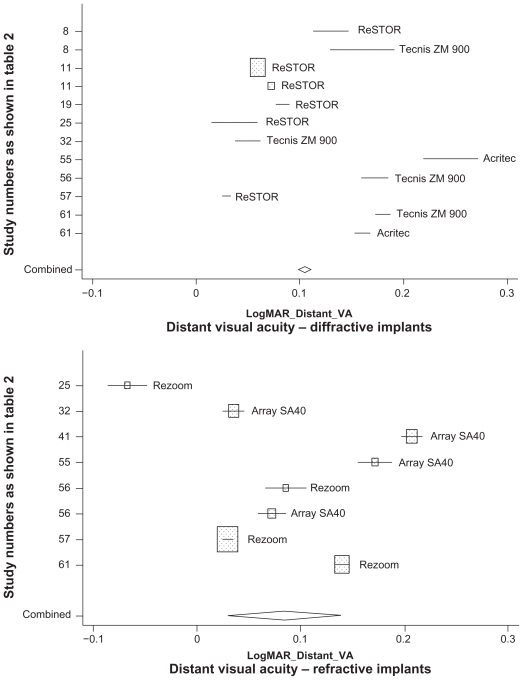
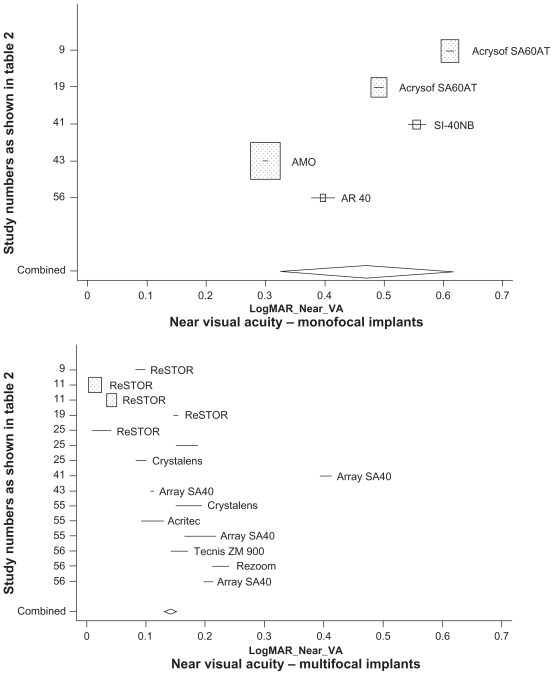
Table 4 shows that multifocal and monofocal uncorrected distance visual acuity was 0.165 and 0.093, respectively. Between the multifocal implants, there was no statistically significant uncorrected distance visual acuity difference (P = 0.78), or between diffractive IOLs (average LogMAR 0.105) and refractive IOLs (average LogMAR 0.085). However, uncorrected distance visual acuity was significantly better with ReSTOR (average LogMAR 0.067) as compared with other multifocal implants (P < 0.001). Table 4 also shows that uncorrected near visual acuity was significantly better (P < 0.001) after multifocal implants (average Log- MAR 0.141) than monofocal IOLs (average LogMAR 0.470). Moreover, with multifocal implants, uncorrected near visual acuity was significantly better (P = 0.002) with diffractive IOLs (average LogMAR 0.082) than refractive IOLs (average LogMAR 0.217). Furthermore, uncorrected near visual acuity was significantly better (P = 0.006) after ReSTOR implants (average LogMAR 0.064) than after all other multifocal IOLs. Forest plots of uncorrected near and distance visual acuity are reported in Figures 1–4.
Table 4.
Random effects pooled estimates of uncorrected distance and near visual acuity for IOL implants
| IOL implant | Distance visual acuity |
Near visual acuity |
||||
|---|---|---|---|---|---|---|
| Mean LogMAR | 95% CI | P* | Mean LogMAR | 95% CI | P* | |
| Monofocal | 0.165 | 0.090–0.240 | <0.001 | 0.470 | 0.322–0.618 | <0.001 |
| Multifocal, all | 0.093 | 0.088–0.098 | 0.141 | 0.131–0.152 | ||
| Multifocal, diffractive | 0.105 | 0.098–0.111 | 0.78 | 0.082 | 0.067–0.098 | 0.002 |
| Multifocal, refractive | 0.085 | 0.029–0.140 | 0.217 | 0.118–0.317 | ||
| ReSTOR | 0.067 | 0.059–0.076 | <0.001 | 0.064 | 0.046–0.082 | 0.006 |
Notes: P values for statistical test of the significance of the differences between monofocal versus multifocal, diffractive versus refractive, and ReSTOR other multifocal IOL implants, respectively.
Abbreviations: IOL, intraocular lens; CI, confidence interval.
Figure 1.
Uncorrected distant visual acuity: random effects pooled LogMAR estimates for monofocal vs multifocal intraocular lens implants. The y-axis denotes the estimates obtained in different studies as well as the combined (pooled) estimate.
Figure 4.
Uncorrected near visual acuity: random effects pooled LogMAR estimates for diffractive, refractive, and ReSTOR multifocal IOL implants. The y-axis denotes the estimates obtained in different studies as well as the combined (pooled) estimate.
Freedom from spectacles
Table 5 shows the results of random effects Poisson regression models comparing the incidence of no spectacle requirement after different IOL implants. In general, patients with multifocal IOL implants, especially those with diffractive implants, were most likely not to need spectacles. Estimates varied for near and distance vision spectacles, compared with all spectacles combined, with most estimates specific to the two spectacle types not reaching statistical significance, probably because too few specific data were available for analysis. Overall, however, patients with multifocal implants were 3.6 times more likely not to need spectacles (incidence rate ratio [IRR] 3.62, 95% CI: 2.90–4.52).
Table 5.
Random effects Poisson regression estimates for comparison of the probability (incidence) of independence from no distance, reading, and all spectacles combined for different subgroups of IOL implants
| IOL implant | Distance spectacles |
Reading spectacles |
All spectacles |
|||
|---|---|---|---|---|---|---|
| IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | |
| Monofocal | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| Multifocal, all | 1.69 | 1.06–2.70 | 1.37 | 1.02–1.84 | 3.62 | 2.90–4.52 |
| Multifocal diffractive | 1.54 | 0.36–6.61 | 2.61 | 0.82–8.29 | 1.75 | 1.24–2.48 |
| Multifocal refractive | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| ReSTOR* | Not estimable** | 1.51 | 0.43–5.24 | 2.06 | 1.26–3.36 | |
Notes: Comparison between ReSTOR other multifocal IOL implants;
Insufficient data for estimating the IRR.
Abbreviations: IOL, intraocular lens; CI, confidence interval; IRR, incidence rate ratio.
Diffractive IOL implants were associated with a 1.75-times higher likelihood of spectacle independence (IRR 1.75, 95% CI: 1.24–2.48) than refractive implants. Also, patients implanted with ReSTOR had a more than two-fold higher incidence of spectacle independence compared with other multifocal IOLs (IRR 2.06, 95% CI: 1.26–3.36).
Patient satisfaction and halo
Results of patient satisfaction and presence of halo analyses are shown in Tables 5 and 6. No statistically significant differences between implant types were found for patient satisfaction or halo reports. In most cases, point estimates (IRRs) were close to the null value (1.0), except between diffractive versus refractive IOL implants with regard to halo. Diffractive implants were associated with a lower incidence rate of halo as compared with refractive implants (IRR 0.71, 95% CI: 0.48–1.05), but the difference did not reach statistical significance (P = 0.087).
Table 6.
Random effects Poisson regression estimates for comparison of the probability (incidence) of satisfaction and of presence of halo for subgroups of IOL implants
| IOL implant | Satisfaction |
Halo |
||
|---|---|---|---|---|
| IRR | 95% CI | IRR | 95% CI | |
| Monofocal | 1.00 | Reference | 1.00 | Reference |
| Multifocal all | 1.03 | 0.90–1.17 | 1.13 | 0.91–1.39 |
| Multifocal diffractive | 1.05 | 0.85–1.31 | 0.71 | 0.48–1.05 |
| Multifocal refractive | 1.00 | Reference | 1.00 | Reference |
| ReSTOR | 1.01 | 0.75–1.36 | 0.93 | 0.54–1.60 |
Note: Comparison between ReSTOR and other multifocal IOL implants.
Abbreviations: CI, confidence interval; IRR, incidence rate ratio.
Discussion
Our study compared vision outcomes after multifocal IOL or monofocal IOL implants, and outcomes after multifocal implants differing in physical properties and other characteristics. In this meta-analysis, because we found very few trials comparing head to head monofocal IOLs, we made the decision to use monofocal IOL arms as a common arm to do indirect comparisons among multifocal IOLs. We did not compare the different types of monofocal IOLs, because this was not our objective and because the experimental design was not appropriate for us to do so.
Although we identified an important number of relevant studies (n = 20), it should be noted that most did not randomize treatments, which could be considered as poor evidence reporting. However, this can be explained by certain ethical constraints. Randomization is acceptable in the early development of an IOL, from the patient’s point of view, because the associated benefit–risk ratio has to be quantified. Subsequently, however, it is much more difficult to promise patients spectacle independence when treatments are randomized in a clinical trial and knowing that only patients given a multifocal IOL implant can enjoy freedom from spectacles. This explains why most trials analyzed by this meta-analysis were not randomized.
We found better uncorrected distance visual acuity following multifocal IOL implants than after monofocal implants, which was unexpected from an optics standpoint. It might be that surgeons implanting multifocal IOLs promised their patients freedom from spectacles, although this did not apply to monofocal implants. Perhaps they then performed more precise biometric assessments after the multifocal IOLs in order to ensure that the patients would not need spectacles. This would explain the better uncorrected distance visual acuity findings.
Patient satisfaction was high for all implants, with no difference observed between IOLs. On the top of this ceiling effect, it must be recalled that satisfaction reports were not obtained in a uniform manner across studies, which was likely to engender high uncontrolled variability. Also, satisfaction questions concerned surgical outcomes and did not refer to the IOLs implanted. Patients undergoing simple cataract surgery always express high levels of satisfaction because their corrected visual acuity improves dramatically. Hence, an outcome questionnaire dedicated to refraction evaluation, such as the NEI-RQL-42, would be more appropriate to capture a patient’s perceived benefit of being free from spectacles.39,40
The main limitation of our study was the distribution of patients between the clinical trials of the different IOL implants. In particular, the numerically superior diffractive multifocal IOLs was especially due to a high number of patients implanted with ReSTOR as compared with the alternative diffractive implant, Tecnis, which was studied in almost 10 times fewer patients than ReSTOR. Also, the total number of patients recruited in clinical trials of all refractive multifocal IOL implants was half that for ReSTOR. Given the aforementioned figures, it would appear that our statistical analysis was more powerful with regard to objective findings for ReSTOR than for the other multifocal IOLs when taken separately. Another limitation was the variability of measurement parameters, especially with respect to spectacle independence which was not expressed similarly across studies.
To our knowledge, no previous meta-analysis has been applied to the present outcomes with multifocal implants. The single existing review article15 did not involve statistical analysis. Consequently, we could not compare our results with other scientific sources.
On the basis of the present results, we can conclude that multifocal IOLs offer patients better near uncorrected visual acuity than do monofocal implants. Also, ReSTOR provided significantly better visual acuity than other multifocal IOLs.
Spectacle independence was achieved more frequently with multifocal implants than monofocal IOLs, and by multifocal diffractive implants than refractive IOLs. ReSTOR patients also experienced greater freedom from spectacles than patients implanted with other multifocal IOLs. The number of patients observed was insufficient to achieve statistical significance with respect to types of spectacles required (near or distance vision). Also, statistical significance was not attained for patient satisfaction or halo reports. A trend (P = 0.087) was observed, suggesting fewer halos with multifocal diffractive implants compared with refractive IOLs. Hence, the design of an implant could also play a role in the outcome following a multifocal IOL implant.
Figure 2.
Uncorrected distant visual acuity: random effects pooled LogMAR estimates for diffractive, refractive, and ReSTOR multifocal intraocular lens implants. The y-axis denotes the estimates obtained in different studies as well as the combined (pooled) estimate.
Figure 3.
Uncorrected near visual acuity (VA): random effects pooled LogMAR estimates for monofocal vs multifocal intraocular lens implants. The y-axis denotes the estimates obtained in different studies as well as the combined (pooled) estimate.
Acknowledgments
This study received a grant from Alcon, France. The analysis was conducted by Cemka Eval, Bourg-la-Reine, France.
Footnotes
Disclosure
GB is an employee of Alcon, France. The other authors disclose no conflicts of interest.
References
- 1.Congdon N, Vingerling JR, Klein BE, et al. Prevalence of cataract and pseudophakia/aphakia among adults in the United States. Arch Ophthalmol. 2004;122:487–494. doi: 10.1001/archopht.122.4.487. [DOI] [PubMed] [Google Scholar]
- 2.Javitt JC, Wang F, West SK. Blindness due to cataract: Epidemiology and prevention. Ann Rev Public Health. 1996;17:159–177. doi: 10.1146/annurev.pu.17.050196.001111. [DOI] [PubMed] [Google Scholar]
- 3.Agency for Health Care Policy and Research. Cataract in Adults: Management of functional impairment. Rockville, MD: Agency for Health Care Policy and Research; 1993. [Google Scholar]
- 4.Anmarkrund N, Bergaust B, Bulie T, Sand AB. Evaluation of a flexible one-piece open-loop anterior chamber lens Symflex 350B 3–4 years after implantation. Acta Ophthalmol. 1993;71:796–800. doi: 10.1111/j.1755-3768.1993.tb08603.x. [DOI] [PubMed] [Google Scholar]
- 5.Pötzsch DK, Lösch-Pötzsch M. Four year follow-up of the Memorylens. J Cataract Refract Surg. 1996;22:1336–1341. doi: 10.1016/s0886-3350(96)80094-0. [DOI] [PubMed] [Google Scholar]
- 6.Schmack WH, Gerstmeyer K. Long-term results of the foldable CeeOn edge intraocular lens. J Cataract Refract Surg. 2000;26:1172–1175. doi: 10.1016/s0886-3350(00)00522-8. [DOI] [PubMed] [Google Scholar]
- 7.Milazzo S, Turut P, Artin B, Charlin JF. Long-term follow-up of threepiece, looped, silicone intraocular lenses. J Cataract Refract Surg. 1996;22 (Suppl 2):1259–1262. doi: 10.1016/s0886-3350(96)80080-0. [DOI] [PubMed] [Google Scholar]
- 8.Linnola RJ, Holst A. Evaluation of a 3-piece silicone intraocular lens with poly(methyl methacrylate) haptics. J Cataract Refract Surg. 1998;24:1509–1514. doi: 10.1016/s0886-3350(98)80175-2. [DOI] [PubMed] [Google Scholar]
- 9.Simpson MJ. The diffractive multifocal intraocular lens. Eur J Implant Refract Surg. 1989;1:115–121. [Google Scholar]
- 10.Javitt JC, Steinert RF. Cataract extraction with multifocal intraocular lens implantation: A multinational clinical trial evaluating clinical, functional, and quality-of-life outcomes. Ophthalmology. 2000;107:2040–2048. doi: 10.1016/s0161-6420(00)00368-7. [DOI] [PubMed] [Google Scholar]
- 11.Javitt JC, Wang F, Trentacost DJ, et al. Outcomes of cataract extraction with multifocal intraocular lens implantation: Functional status and quality of life. Ophthalmology. 1997;104:589–599. doi: 10.1016/s0161-6420(97)30265-6. [DOI] [PubMed] [Google Scholar]
- 12.Rossetti L, Carraro F, Rovati M, et al. Performance of diffractive multifocal intraocular lenses in extracapsular cataract surgery. J Cataract Refract Surg. 1994;20:124–128. doi: 10.1016/s0886-3350(13)80150-2. [DOI] [PubMed] [Google Scholar]
- 13.Vaquero M, Encinas JL, Jimenez F. Visual function with monofocal versus multifocal IOLs. J Cataract Refract Surg. 1996;22:1222–1225. doi: 10.1016/s0886-3350(96)80071-x. [DOI] [PubMed] [Google Scholar]
- 14.Gimbel HV, Sanders DR, Raanan MG. Visual and refractive results of multifocal intraocular lenses. Ophthalmology. 1991;98:881–888. doi: 10.1016/s0161-6420(91)32205-x. [DOI] [PubMed] [Google Scholar]
- 15.Auffarth GU, Dick HB. Multifocal intraocular lenses. A review. Ophthalmologe. 2001;98:127–137. doi: 10.1007/s003470170172. [DOI] [PubMed] [Google Scholar]
- 16.Khoshnood B, Mesbah M, Jeanbat V, et al. Transforming scales of measurement of visual acuity at the group level. Ophthalmic and Physiological Optics. 2010;30:816–823. doi: 10.1111/j.1475-1313.2010.00766.x. [DOI] [PubMed] [Google Scholar]
- 17.Mosteller F, Colditz GA. Understanding research synthesis (metaanalysis) Ann Rev Public Health. 1996;17:1–23. doi: 10.1146/annurev.pu.17.050196.000245. [DOI] [PubMed] [Google Scholar]
- 18.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 19.Bi H, Cui Y, Ma X, et al. Early clinical evaluation of Acrysof ReSTOR Multifocal lens for treatment of cataract. Ophthalmologica. 2008;222:11–16. doi: 10.1159/000109272. [DOI] [PubMed] [Google Scholar]
- 20.Chiam PJ, Cahn JH, Haider SI, et al. Functional vision with bilateral Rezoom and ReSTOR intraocular lenses 6 months after cataract surgery. J Cataract Refract Surg. 2007;33:2057–2061. doi: 10.1016/j.jcrs.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 21.Toto L, Falconio G, Vecchiarino L, et al. Visual performance and biocompatibility of 2 multifocal diffractive IOLs. Six-month comparative study. J Cataract Refract Surg. 2007;33:1419–1425. doi: 10.1016/j.jcrs.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Souza CE, Muccioli C, Soriano ES, et al. Visual performance of Acrysof ReSTOR apodized diffractive IOL: A prospective comparative trial. Am J Ophthalmol. 2006;141:827–832. doi: 10.1016/j.ajo.2005.12.031. [DOI] [PubMed] [Google Scholar]
- 23.Vingolo EM, Grenga P, Iacobelli L, Grenga R. Visual acuity and contrast sensitivity: Acrysof ReSTOR apodized diffractive versus Acrysof SA60AT monofocal intraocular lenses. J Cataract Refract Surg. 2007;33:1244–1247. doi: 10.1016/j.jcrs.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 24.Alfonso JF, Fernandez-Vega L, Baamonde B, Montés-Mico R. Prospective visual evaluation of apodized diffractive intraocular lenses. J Cataract Refract Surg. 2007;33:1235–1243. doi: 10.1016/j.jcrs.2007.03.034. [DOI] [PubMed] [Google Scholar]
- 25.Chiam PJT, Chan JH, Aggarwal RK, Kasaby S. ReSTOR intraocular lens implantation in cataract surgery: Quality of vision. J Cataract Refract Surg. 2006;32:1459–1463. doi: 10.1016/j.jcrs.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 26.Peposee JS, Qazi MA, Davies J, et al. Visual performance of patients with bilateral vs combination Crystalens, Rezoom, and ReSTOR intraocular lens implants. Am J Ophthalmol. 2007;144:347–357. doi: 10.1016/j.ajo.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 27.Mester U, Hunold W, Wesendahl T, Kaymak H. Functional outcomes after implantation of Tecnis ZM900 and Array SA40 multifocal intraocular lenses. J Cataract Refract Surg. 2007;33:1033–1040. doi: 10.1016/j.jcrs.2007.02.037. [DOI] [PubMed] [Google Scholar]
- 28.Brydon KW, Tokarewicz AC, Nichols BD. AMO array multifocal lens versus monofocal correction in cataract surgery. J Cataract Refract Surg. 2000;26:96–100. doi: 10.1016/s0886-3350(99)00335-1. [DOI] [PubMed] [Google Scholar]
- 29.Chen M, Atebara NH, Chen TT. A comparison of a monofocal Acrysoft IOL using the “blended monovision” formula with the multifocal array IOL for glasses independence after cataract surgery. Ann Ophthalmol (Skokie) 2007;39:237–240. doi: 10.1007/s12009-007-0035-4. [DOI] [PubMed] [Google Scholar]
- 30.Sen HN, Sarikkola AU, Uusitalo RJ, Laatikainen L. Quality of vision after AMO Array multifocal intraocular lens implantation. J Cataract Refract Surg. 2004;30:2483–2493. doi: 10.1016/j.jcrs.2004.04.049. [DOI] [PubMed] [Google Scholar]
- 31.Javitt JC, Steinert RF. Cataract extraction with multifocal intraocular lens implantation: A multinational clinical trial evaluating clinical, functional, and quality-of-life outcomes. Ophthalmology. 2000;107:2040–2048. doi: 10.1016/s0161-6420(00)00368-7. [DOI] [PubMed] [Google Scholar]
- 32.Martinez-Palmer A, Gomez-Faina P, Espana-Albelda A, et al. Visual function with bilateral implantation of monofocal and multifocal intraocular lenses: A prospective, randomized, controlled clinical trial. J Refractive Surg. 2008;24:257–264. doi: 10.3928/1081597X-20080301-07. [DOI] [PubMed] [Google Scholar]
- 33.Chang-David F. Prospective functional and clinical comparison of bilateral Rezoom and ReSTOR intraocular lenses in patients 70 years or younger. J Cataract Refract Surg. 2008;34:934–941. doi: 10.1016/j.jcrs.2007.12.053. [DOI] [PubMed] [Google Scholar]
- 34.Barisic A, Dekaris I, Gabric N, et al. Comparison of diffractive and refractive multifocal intraocular lenses in presbyopia treatment. Coll Antropol. 2008;32 (Suppl 2):27–31. [PubMed] [Google Scholar]
- 35.Zelichowska B, Rekas M, Stankiewicz A, et al. Apodized diffractive versus refractive multifocal intraocular lenses: Optical and visual evaluation. J Cataract Refract Surg. 2008;34:2036–2042. doi: 10.1016/j.jcrs.2008.06.045. [DOI] [PubMed] [Google Scholar]
- 36.Cillino S, Casuccio A, DiPace F, et al. One year outcomes with new- generation multifocal intraocular lenses. Ophthalmology. 2008;115:1508–1516. doi: 10.1016/j.ophtha.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 37.Alio JL, Tavolato M, de la Hoz F, et al. Near vision ReSTORation with refractive lens exchange and pseudoaccomodating and multifocal refractive and diffractive intraocular lenses: Comparative clinical study. J Cataract Refract Surg. 2004;30:2494–2503. doi: 10.1016/j.jcrs.2004.04.052. [DOI] [PubMed] [Google Scholar]
- 38.Cochener B, Arnould B, Viala M, Roborel de Climens A, Berdeaux G. Corrected and uncorrected near and distance vision with ReSTOR compared to monofocal intraocular lens implantation after cataract surgery: A pooled analysis. Ophthalmologica. 2009;223:128–135. doi: 10.1159/000183845. [DOI] [PubMed] [Google Scholar]
- 39.McDonnell PJ, Mangione C, Lee P, et al. Responsiveness of the National Eye Institute Refractive Error Quality of Life instrument to surgical correction of refractive error. Ophthalmology. 2003;110:2302–2309. doi: 10.1016/j.ophtha.2003.02.004. [DOI] [PubMed] [Google Scholar]
- 40.Nichols JJ, Mitchell GL, Saracino M, Zadnik K. Reliability and validity of refractive error-specific quality-of-life instruments. Arch Ophthalmol. 2003;121:1289–1296. doi: 10.1001/archopht.121.9.1289. [DOI] [PubMed] [Google Scholar]
- 41.Blaylock JF, Si Z, Vickers C. Visual and refractive status at different focal distances after implantation of the ReSTOR multifocal intraocular lens. J Cataract Refract Surg. 2006;32:1464–1473. doi: 10.1016/j.jcrs.2006.04.011. [DOI] [PubMed] [Google Scholar]