Abstract
Practical limitations and sample size considerations often lead to broadening of diagnostic criteria for anorexia nervosa (AN) in research. The current study sought to elucidate the effects of this practice on resultant sample characteristics in terms of eating disorder behaviors, psychiatric comorbidities, temperament and personality characteristics, and heritability point estimates. Three definitions of AN were created: meeting all Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria for AN (AN-DSM-IV), meeting all DSM-IV criteria except criterion D, amenorrhea, (AN-noD), and broadening DSM-IV AN criteria by allowing a higher body mass index value, eliminating criterion D, and allowing less stringent body weight concerns (AN-Broad). Using data from the Swedish Twin Registry, 473 women fit one of the three definitions of AN. Women with AN-DSM-IV reported significantly more eating disorder behaviors than women with AN-Broad. Women with AN-noD reported more comorbid psychiatric disorders than women with AN-DSM-IV and AN-Broad. Temperament and personality characteristics did not differ across the three groups. Heritability point estimates decreased as AN definition broadened. Broadening the diagnostic criteria for AN results in an increased number of individuals available for participation in research studies. However, broader criteria for AN yield a more heterogeneous sample with regard to eating disorder symptoms and psychiatric comorbidity than a sample defined by narrower criteria.
Keywords: Anorexia Nervosa, Classification, Diagnostic Criteria, Eating Disorder
Introduction
In general, for psychiatric disorders, diagnostic criteria and criteria used for inclusion in research studies should provide a balance between validity and reliability, encompassing scientific and non-scientific components of the disorder (Kendler, 1990) and should identify a group of individuals who are fairly homogeneous and distinct from other groups (Kendell et al., 2003). Along with being able to distinguish affected from unaffected individuals accurately, diagnostic criteria need to be easily applied (First et al., 2004; Kopelman et al., 2002), provide guidance in choosing an appropriate treatment likely to lead to a positive outcome (First et al., 2004), and, with advancing technology might assist with determining appropriate pharmacologic agents to treat psychiatric disorders.
With reference to anorexia nervosa (AN), criteria for inclusion in research studies should yield a group of individuals who can be easily distinguished from individuals without AN and who are similar in terms of eating disorder symptoms, psychiatric comorbidity, and personality and temperament characteristics. This would result in a homogenous group of individuals for whom treatment could be developed, tested, and applied and yield optimum definitions of cases and controls for genetic studies. Inclusion of individuals with a precise phenotype in genetic studies could lead to improved knowledge about biological origins of the disorder and might provide potential pharmacologic targets. However, broader definitions of psychiatric disorders, which do not lose the central pathological constructs and validators of the disorder, could provide a larger group of individuals to study and might better capture individuals with similar core psychopathologies, thus preventing fragmentation of psychiatric disorders (Kendler, 1990). Although the ideal breadth of diagnostic criteria might differ depending on the purpose of the study, understanding the effect of broadening definitions of illness remains important for interpreting findings and considering generalizability.
Arguments for Relaxation of Inclusion Criteria in Research Studies
Researchers have relaxed diagnostic criteria for AN for a variety of reasons, but most commonly to boost sample size. One justification for relaxing criteria is the view that subthreshold and threshold eating disorders as lie along a continuum of severity (Keel et al., 2005; Lucas et al., 1991; Walters et al., 1995) or a continuum of time as many individuals with subthreshold AN later develop threshold AN (Agras et al., 2009; Milos et al., 2005). It has been argued that women who meet diagnostic criteria for AN do not differ qualitatively from those who meet criteria for subthreshold AN (Cachelin et al., 1998; Crow et al., 2002; Garfinkel et al., 1996; Walters et al., 1995; Watson et al., 2003). In addition, the appropriateness of current measures of criterion A (low weight) (Mitchell et al., 2005) and the usefulness of criterion D (amenorrhea) have been questioned (Attia et al., 2009; Gendall et al., 2006; Mitchell et al., 2005; Poyastro Pinheiro et al., 2007; Wilfley et al., 2007). Decisions to broaden diagnostic criteria usually result from a balanced consideration of the appropriateness, validity, and utility of the specific diagnostic criterion and statistical power.
However, several potential issues arise when criteria are broadened. First, studies have not uniformly relaxed diagnostic criteria rendering the comparison of results across studies difficult (Dellava et al., 2009; Dingemans et al., 2006; Dominguez et al., 2007; Haas et al., 2009; Kaye et al., 2008; Kaye et al., 2000; Keel et al., 2005; Klump et al., 2001; Loeb et al., 2007; Perkins et al., 2005; Reba et al., 2005; Sanci et al., 2008; Schebendach et al., 2008; Wild et al., 2009). Second, women with subthreshold AN differ from women with threshold AN on eating disorder behaviors, psychiatric comorbidities, and some temperament and personality characteristics (Becker et al., 2009; Dalle Grave et al., 2008; Gendall et al., 2006; Santonastaso et al., 2009) and these differences might impact the results of research studies. Third, the extent to which genetic factors influence development of threshold and subthreshold AN might differ (Bulik et al., 2010) and inclusion of subthreshold cases could increase the number of phenocopies in the sample. If women with threshold AN differ from women with subthreshold AN, combining the groups of individuals could dilute the resulting sample, lead to null or false findings, and potentially obscure the scientific understanding of AN.
Adjustments to Criteria in Research Studies
Criteria for AN have generally been altered in three ways. First, criterion A, the weight criterion, has been adjusted (Bulik et al., 2010; Bulik et al., 2009; Dellava et al., 2009; Haas et al., 2009; Kaye et al., 2008; Keel et al., 2005; Klump et al., 2001; Loeb et al., 2007; Perkins et al., 2005). Second, requirements for the number of AN criteria endorsed have varied (Dingemans et al., 2006; Keel et al., 2005; Klump et al., 2001; Perkins et al., 2005; Sanci et al., 2008; Wild et al., 2009). Third, criterion D, amenorrhea, has often been eliminated (Dominguez et al., 2007; Kaye et al., 2008; Kaye et al., 2000; Reba et al., 2005; Schebendach et al., 2008; Wade et al., 2008).
Similarities and Differences between Women with Threshold and Subthreshold AN
Although the practice of relaxing diagnostic criteria for AN in research is common, its impact on the nature of the resultant study samples is unclear and requires further investigation. For example, eating disorder pathology has been reported to be lower in those not meeting criterion B (fear of weight gain at a low weight) (Becker et al., 2009; Thomas et al., 2009) and inconsistent in those not meeting criterion A (Santonastaso et al., 2009; Thomas et al., 2009) or criterion D (Dalle Grave et al., 2008; Gendall et al., 2006), compared with women with threshold AN. Table 1 highlights observed similarities and differences.
Table 1.
Similarities and differences between women who met criteria for subthreshold or threshold anorexia nervosaa
| Study | Main findings |
|---|---|
| Santonastaso, 2009 | Excessive exercise- more likely in subthreshold (no A) than threshold |
| Thomas, 2009 | Overall eating disorder pathology- similar in subthreshold (no A) and threshold Comorbid psychiatric disorders- similar in subthreshold (no A) and threshold |
| Becker, 2009; Thomas, 2009 | Overall eating disorder pathology- lower in subthreshold (no B) than threshold |
| Thomas, 2009 | Comorbid psychiatric disorders- similar in subthreshold (no B) and threshold |
| Cachelin, 1998 | Body image concerns- similar in subthreshold (no D) and threshold |
|
Cachelin, 1998; Dalle Grave, 2008; Gendall, 2006; Thomas, 2009 |
Comorbid psychiatric disorders- similar in subthreshold (no D) and threshold |
| Thomas, 2009 | Overall eating disorder pathology- similar in subthreshold (no D) and threshold |
| Dalle Grave, 2008 | Self-induced vomiting- more likely in subthreshold (no D) than threshold Binge eating- more likely in subthreshold (no D) than threshold |
| Dalle Grave, 2008; Gendall, 2006 | Excessive exercise- less likely in subthreshold (no D) than threshold |
| Dalle Grave, 2008 | Lowest body mass index- higher in subthreshold (noD) than threshold |
| Garfinkel, 1996 | Lowest body mass index- similar in subthreshold (no D) and threshold |
| Gendall, 2006 | Persistence- lower in subthreshold (no D) than threshold Smoking- higher in subthreshold (no D) than threshold |
| Gendall, 2006; Santonastaso, 2009 | Novelty seeking- higher in subthreshold (no D) than threshold |
| Santonastaso, 2009 | Anxiety- more likely in subthreshold (no D) than threshold Obsessionality- more likely in subthreshold (no D) than threshold |
Subthreshold definitions indicated by which criterion was relaxed; no A = did not meet Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criterion A (low weight); no B= did not meet DSM-IV criterion B (fear of weight gain at low weight); no D= did not meet DSM-IV criterion D (amenorrhea)
Diagnostic Criteria and Heritability
The impact of altering diagnostic criteria on heritability estimates for AN remains unknown. The risk of having AN in a cotwin of a twin affected with AN was higher when a narrow, compared with a broad, definition of AN was used (Walters et al., 1995). Although heritability point estimates have exceeded 50% using several subthreshold definitions of AN (Klump et al., 2001; Kortegaard et al., 2001; Wade et al., 2000), higher heritability estimates for threshold than subthreshold AN have also been reported (Bulik et al., 2010). In another approach to exploring the impact of sample homogeneity, Grice et al., found significant linkage in a sample confined to restricting AN only and not in a more inclusive definition of illness including multiple subtypes of AN (Grice et al., 2002).
The aim of the current study was to determine the impact of broadening case definitions of AN on eating disorder symptomatology, psychiatric comorbidities, personality and temperament characteristics, and heritability estimates in the resultant study samples.
Materials and Method
Swedish Twin Registry
For the current study, eligible participants were from The Swedish Twin Registry (STR; http://ki.se/twinreg) subsample, the Swedish Twin study of Adults: Genes and Environment (STAGE; http://ki.se/ki/jsp/polopoly.jsp?d=9610&l=en). STAGE is a large population-based prospective sample of Swedish twins born 1959–1985 (Furberg et al., 2008). Twins were between the ages of 20 years and 47 years at the time of interview. In 2005, data were collected on health, physiological and biological measures, sociodemographic and socioeconomic measures, and life habits and behaviors using web-based questionnaires or telephone interviews if the participant preferred. Of the 43,000 eligible individuals, over 25,000 (59.6%) responded (overall, 43.1% using only the web-based questionnaire; 16.5% using only telephone interview). In order to assess test-retest reliability as well as to compare data collection methods (computer-based vs. telephone interview), 100 twins, who completed the questionnaires via self-report, were re-contacted and interviewed by telephone. There was adequate agreement between methods of data collection (Kappa value=.76) for the eating disorders section (Lichtenstein et al., 2006).
This research is in accord with the Declaration of Helsinki. STAGE was approved by the Regional Ethics Committee at the Karolinska Institutet and by the Biomedical Institutional Review Board at the University of North Carolina at Chapel Hill. A detailed description of the study design can be found elsewhere (Furberg et al., 2008; Lichtenstein et al., 2006).
Zygosity
Zygosity was assigned using a validated algorithm that used both twins’ responses to the following questions: (1) During childhood, were you and your twin partner as like as ‘two peas in a pod’ or no more alike than siblings in general? and (2) How often did strangers have difficulty in distinguishing between you and your twin partner when you were children? Additional details for zygosity assignment can be found in Lichtenstein et al., (2002).
Anorexia Nervosa Diagnosis
Lifetime history of AN was assessed using an expanded, on-line Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV)-based instrument (First et al., 1999). DSM-IV criteria were used to develop algorithms for AN diagnosis. As the explicit aim of our study was to explore the impact of broadening definitions of illness, three definitions of AN were derived to reflect 1) current DSM IV criteria: all DSM-IV criteria for AN (AN-DSM-IV) required; 2) one of the most common alterations to DSM-IV criteria: criteria A, B, and C required but criterion D not required (AN-noD); and 3) a broad and balanced definition of AN: broadening (but not eliminating) criteria A, B and C, with criterion D not required (AN-Broad) (Table 2). A hierarchy was established so that each participant could be assigned to only one AN group as follows: AN-DSM-IV, AN-noD, AN-Broad. Information on use of birth control medication at time of lowest body mass index (BMI) was not available; therefore some women in AN-noD could have been classified as such due to menstruation as a result of birth control medication.
Table 2.
Criteria used for anorexia nervosa (AN) diagnosesa
| AN-DSM-IVa | AN-noDa | AN-Broada | |
|---|---|---|---|
| DSM-IV Criterion A |
BMI<17.55 and endorsed weighing much less than others thought she should weigh in the past or present | BMI<17.55 and endorsed weighing much less than others thought she should weigh in the past or present | BMI<18.55 and endorsed weighing much less than others thought she should weigh in the past or present |
| DSM-IV Criterion B |
Fear of gaining weight or becoming fat indicated by a response of being very afraid or extremely afraid of gaining weight or becoming fat when at a low weight | Fear of gaining weight or becoming fat indicated by a response of being very afraid or extremely afraid of gaining weight or becoming fat when at a low weight | Any fear of gaining weight or becoming fat when at a low weight |
| DSM-IV Criterion C |
Body image disturbance indicated by a response of feeling very or extremely fat when at a low body weight | Body image disturbance indicated by a response of feeling very or extremely fat when at a low body weight | Body image disturbance (expressing feeling slightly, somewhat, very, or extremely fat when at a low weight) |
| DSM-IV Criterion D |
Amenorrhea | --- | --- |
DSM (Diagnostic and Statistical Manual of Mental Disorders); AN-DSM-IV (met full DSM-IV criteria for AN); AN-noD (met all DSM-IV criteria for AN except criterion D); AN-Broad (met broader version of DSM-IV criteria for AN)
Other Measures
Eating disorder behaviors
On the eating disorder portion of the STAGE questionnaire, participants indicated if they engaged in the following eating disorder behaviors: exercising more than two hours daily, binge eating, fasting (24-hours), diet pill use, self-induced vomiting, laxative use, or diuretic use. Response options were ‘never,’ ‘once or twice,’ ‘every week,’ and ‘daily.’ Excessive exercise was scored as present if the participant endorsed the ‘daily’ response for exercise and as absent for all other response options. For all other measures, the behavior was not considered present if ‘never’ was endorsed and present for all other response options. If vomiting, laxative use, or diuretic use was present, then purging was considered present.
Other psychopathology
Lifetime presence of several disorders was assessed. Participants were asked “Do you have or have you ever had any of the following problems?” and were instructed to respond ‘yes’ or ‘no’ to each disorder in a list which included panic disorder, phobias, and obsessive compulsive disorder. More detailed self-report assessments were available for bulimia nervosa (BN), major depression, generalized anxiety disorder, and alcohol problems; thus algorithms were developed to determine a history of these disorders from each participant’s responses. BN was considered present if all DSM-IV diagnostic criteria were met. Generalized anxiety disorder was considered present if criterion A (excessive anxiety and worry) and criterion C (at least three symptoms resulting from anxiety and worry) were met. Major depression was considered present if criterion A (five symptoms of depression associated with a change of functioning) and criterion C (significant impairment caused by the symptoms) were met. Alcohol problems were considered present if the participant met DSM-IV criteria for either abuse or dependence. Heavy drinking was considered present if the participant endorsed consuming more than three bottles of beer, more than three glasses of wine, or more than two large shots of hard liquor in one drinking occasion (Root et al., 2010).
Tobacco and drug use
Regular tobacco use was coded present if the participant indicated smoking cigarettes at least once per day or using snus (Swedish smokeless tobacco) at least once per day. Drug use was considered present if the participant reported using any drug 10 times or more within one month.
Personality and temperament
Personality and temperament characteristics were measured using items from several questionnaires: 10 items from the Temperament and Character Inventory for self-directedness (Cloninger et al., 1994); four items from each of the subscales concern over mistakes, personal standards, and doubts about actions from the Frost Multidimensional Perfectionism Scale (Frost et al., 1990); and nine items for extraversion and 18 items for neuroticism scales from the short form of the Eysenck Personality Inventory (Schapiro et al., 2001). The items were scored and summed according to their respective criteria.
Analysis Sample
Of the 23,818 individuals who completed the eating disorder section of the STAGE questionnaire, 482 (~2%) met criteria for one of the AN definitions: 473 females and nine males. No males in the sample met the definition for AN-DSM-IV even though males were not required to meet AN criterion D. The nine males were removed from the sample as meaningful analyses could not be conducted with so few cases.
Statistical Analyses
For dichotomous variables, the number and percent of individuals endorsing an item was calculated for each AN group. Continuous measures were standardized, and the means and standard deviations were computed for each AN group. Age was entered as a covariate in all models except lowest BMI, where age at lowest BMI was entered as a covariate. Differences among AN groups were assessed using PROC GENMOD in the SAS/STAT® 9.1 software (SAS Institute Inc., 2004). To account for the non-independence of the data due to the inclusion of both members of twin pairs in the analyses, generalized estimating equations were applied to all models with the following exceptions: fasting, purging, and major depression where model failures resulted from errors in the computation of the variance and parameter estimates of the covariance in these models, likely due to the distribution of the twins. False discovery rate corrections were applied to account for multiple testing (Benjamini et al., 1995).
Biometrical twin modeling was conducted using Mx (Neale et al., 2001) to estimate the contribution of additive genetic effects (heritability, a2), shared (or common) environmental effects (c2), and unique environmental effects, including error (e2) to the liability of AN: a2 + c2 + e2 = 1 (total variance of AN phenotype). From the proportion of phenotypic variation in AN attributable to genetic variation among individuals (heritability) and the proportions of shared and unique environmental factors were estimated. Only the full model, estimating a2, c2, and e2 were fit to the data (Sullivan et al., 2002).
To estimate heritability in a population, data from all affected and unaffected individuals were entered into the models regardless of the response of the cotwin. The sample for twin modeling included 1926 MZ twin pairs and 1365 same-sex DZ twin pairs with complete data, and 207 MZ and 146 DZ individuals without cotwin information. For these analyses, groups were reconfigured and nested to represent samples with increasingly broad definitions of illness that also included individuals with more narrow definitions. Thus, the full model was applied to three definitions of AN as follows: (1) only individuals in the AN-DSM-IV group were considered to have AN, all other individuals were entered into the model as unaffected; (2) all individuals who were in the AN-DSM-IV group and the AN-noD group were considered affected; and, (3) all individuals in the AN-DSM-IV, the AN-noD, and the AN-Broad groups were considered to have AN.
Results
Of the 473 women with AN in our sample, 92 (19.5%) met criteria for AN-DSM-IV, an additional 71 (15.0%) met criteria for AN-noD, and an additional 310 (65.5%) met criteria for AN-Broad in these non-overlapping samples. Eating disorder behaviors and characteristics endorsed by women in each group are presented in Table 3. Significant group effects were found for all eating disorder behaviors except binge eating, diet pill use, and diuretic use. Post hoc pairwise comparisons indicated that women with AN-DSM-IV were more likely to endorse laxative use (p<0.002) than women with AN-Broad. Compared with women with AN-Broad, women with AN-DSM-IV and those with AN-noD were more likely to endorse excessive exercise (p<0.001 and p<0.048, respectively), fasting (p<0.001 and p<0.001, respectively), vomiting (p<0.032 and p<0.001, respectively), and purging (p<0.013 and p<0.001, respectively). Lowest BMI differed significantly across groups (p<0.001) and all pairwise comparisons were significant: women with AN-DSM-IV had the lowest BMI, followed by women with AN-noD, and women with AN-Broad.
Table 3.
Means [standard deviation (SD)] of eating disorder characteristics and number (%) for endorsed eating disordered behaviors are presented by anorexia nervosa (AN) groupa. Results of analysis of variance and logistic regressions predicting the characteristics and behaviors, respectively, from AN group. All p-values are false discovery rate corrected; significant pairwise comparisons are listed.
| AN-DSM-IVa (n=92) |
AN-noDa (n=71) |
AN-Broada (n=310) |
Results | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | Mean (SD) | N | Mean (SD) | N | Mean (SD) | N | X2 (p-value) | Pairwise Comparisons |
| Age | 32.8 (7.5) | 91 | 29.4 (7.2) | 71 | 32.0 (7.5) | 310 | 9.53 (.028) | AN-DSM-IV, AN-Broad > AN-noD |
| Age at Low Weight |
18.3 (4.3) | 92 | 18.9 (4.9) | 71 | 19.7 (5.2) | 306 | 11.72 (.012) | AN-Broad > AN-DSM- IV |
| Lowest body mass index (BMI) |
14.8 (1.8) | 92 | 15.6 (1.6) | 71 | 16.9 (1.5) | 310 | 79.22 (.001) | AN-Broad > AN-noD > AN-DSM-IV |
| Highest body mass index (BMI) |
23.9 (4.7) | 84 | 23.9 (5.2) | 63 | 23.8 (4.1) | 277 | 1.09 (.624) | --- |
| No N (%) |
Yes N (%) |
No N (%) |
Yes N (%) |
No N (%) |
Yes N (%) |
|||
| Excessive Exercise |
39 (42.9) | 52 (57.1) | 38 (53.5) | 33 (46.5) | 223 (71.9) | 87 (28.1) | 26.87 (.001) | AN-DSM-IV, AN-noD > AN-Broad |
| Binge Eating |
60 (65.2) | 32 (34.8) | 55 (77.5) | 16 (22.5) | 247 (79.7) | 63 (20.3) | 7.72 (.052) | --- |
| Fasting | 44 (48.4) | 47 (51.6) | 32 (45.1) | 39 (54.9) | 224 (72.3) | 86 (27.7) | 27.72 (.001) | AN-DSM-IV, AN-noD > AN-Broad |
| Diet Pill Use | 62 (67.4) | 30 (32.6) | 41 (57.8) | 30 (42.2) | 233 (75.2) | 77 (24.8) | 7.82 (.052) | --- |
| Vomiting | 40 (43.5) | 52 (56.5) | 21 (29.6) | 50 (70.4) | 180 (58.1) | 130 (41.9) | 21.95 (.001) | AN-DSM-IV, AN-noD > AN-Broad |
| Laxative Use |
65 (70.6) | 27 (29.4) | 59 (83.1) | 12 (16.9) | 273 (88.1) | 37 (11.9) | 11.57 (.014) | AN-DSM-IV > AN-Broad |
| Diuretic Use | 77 (83.7) | 15 (16.3) | 62 (87.3) | 9 (12.7) | 277 (89.4) | 33 (10.6) | 1.91 (.432) | --- |
| Purgingb | 36 (39.1) | 56 (60.9) | 21 (29.6) | 50 (70.4) | 164 (52.9) | 146 (47.1) | 15.16 (.005) | AN-DSM-IV, AN-noD > AN-Broad |
AN-DSM-IV [met full Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria for AN]; AN-noD (met all DSM-IV criteria for AN except criterion D); AN-Broad (met broader version of DSM-IV criteria for AN)
Purging includes any of the following: vomiting, laxative use, diuretic use
Comorbid psychopathology is presented in Table 4. Overall, there were significant group effects, indicating prevalence differences for major depression and phobias. Women with AN-DSM-IV or AN-Broad were less likely to meet criteria for major depression (p<0.016 and p<0.001, respectively) and phobias (p<0.005 and p<0.035, respectively), than women with AN-noD.
Table 4.
Prevalence [Number (%)] of psychological comorbidity for each anorexia nervosa (AN) groupa. Results from logistic regressions predicting comorbid disorder from AN group. All p-values are false discovery rate corrected; significant pairwise comparisons are listed.
| AN-DSM-IVa (n=92) |
AN-noDa (n=71) |
AN-Broada (n=310) |
Results | |||||
|---|---|---|---|---|---|---|---|---|
| No N (%) |
Yes N (%) |
No N (%) |
Yes N (%) |
No N (%) |
Yes N (%) |
X2 (p-value) | Pairwise Comparisons |
|
| Bulimia Nervosa | 78 (84.8) | 14 (15.2) | 62 (87.3) | 9 (12.7) | 291 (93.9) | 19 (6.1) | 6.38 (.091) | --- |
| Major Depression | 40 (48.2) | 43 (51.8) | 18 (26.9) | 49 (73.1) | 159 (56.6) | 122 (43.4) | 17.98 (.001) | AN-noD > AN-DSM-IV, AN-Broad |
| Generalized Anxiety Disorder |
47 (74.6) | 16 (25.4) | 31 (83.8) | 6 (16.2) | 174 (80.6) | 42 (19.4) | 1.96 (.432) | ---- |
| Panic Disorder | 53 (71.6) | 21 (28.4) | 31 (50.8) | 30 (49.2) | 182 (68.2) | 85 (31.8) | 6.11 (.096) | --- |
| Phobias | 49 (92.4) | 4 (7.6) | 35 (66.0) | 18 (34.0) | 182 (83.9) | 35 (16.1) | 8.21 (.048) | AN-noD > AN-DSMIV, AN-Broad |
| Obsessive Compulsive Disorder |
59 (80.8) | 14 (19.2) | 49 (80.3) | 12 (19.7) | 237 (88.4) | 31 (11.6) | 4.18 (.205) | --- |
| Tobacco Useb | 53 (72.6) | 20 (27.4) | 32 (71.1) | 13 (28.9) | 188 (82.1) | 41 (17.9) | 4.90 (.153) | --- |
| Alcohol Problems | 78 (84.8) | 14 (15.2) | 55 (77.5) | 16 (22.5) | 274 (88.4) | 36 (11.6) | 3.08 (.317) | --- |
| Heavy Drinking | 90 (97.8) | 2 (2.2) | 64 (90.1) | 7 (9.9) | 290 (93.6) | 20 (6.4) | 5.17 (.142) | --- |
| Drug Use (10 times or more) |
83 (90.2) | 9 (9.8) | 58 (81.7) | 13 (18.3) | 281 (90.6) | 29 (9.4) | 3.80 (.234) | --- |
AN-DSM-IV [met full Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria for AN]; AN-noD (met all DSM-IV criteria for AN except criterion D); AN-Broad (met broader version of DSM-IV criteria for AN)
Defined as daily use of cigarettes or snus
Personality and temperament characteristics are presented in Table 5. No significant differences across groups were found for any measure.
Table 5.
Means [standard deviation (SD)] of personality and temperament characteristics by anorexia nervosa (AN) groupa. Results from analysis of variance predicting the personality and temperament characteristics from AN group. All p-values are false discovery rate corrected.
| AN-DSM-IVa (n=92) |
AN-noDa (n=71) |
AN-Broada (n=310) |
Results | ||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | N | Mean (SD) | N | Mean (SD) | N | X2 (p-value) | |
| Self Directedness (TCIa) | 18.1 (3.3) | 66 | 17.5 (3.5) | 59 | 17.8 (3.2) | 239 | 0.10 (.988) |
| Concern Over Mistakes (MPSa) | 12.6 (4.3) | 69 | 12.0 (4.2) | 59 | 11.5 (4.1) | 249 | 2.01 (.432) |
| Personal Standards (MPSa) | 14.6 (3.0) | 69 | 14.0 (3.3) | 60 | 13.2 (3.5) | 243 | 2.03 (.432) |
| Doubts about Actions (MPSa) | 9.6 (3.9) | 67 | 9.6 (3.5) | 62 | 9.3 (3.8) | 252 | 2.00 (.432) |
| Neuroticism (EPI-Qa) | 8.3 (5.2) | 64 | 8.9 (4.7) | 50 | 8.2 (4.7) | 222 | 2.96 (.320) |
| Extraversion (EPI-Qa) | 5.1 (2.2) | 59 | 5.0 (2.2) | 52 | 4.9 (2.3) | 216 | 0.01 (.993) |
AN-DSM-IV [met full Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria for AN]; AN-noD (met all DSM-IV criteria for AN except criterion D); AN-Broad (met broader version of DSM-IV criteria for AN);TCI (Temperament and Character Inventory); MPS (Multidimensional Perfectionism Scale); EPI-Q (Eysenck Personality Inventory-short form)
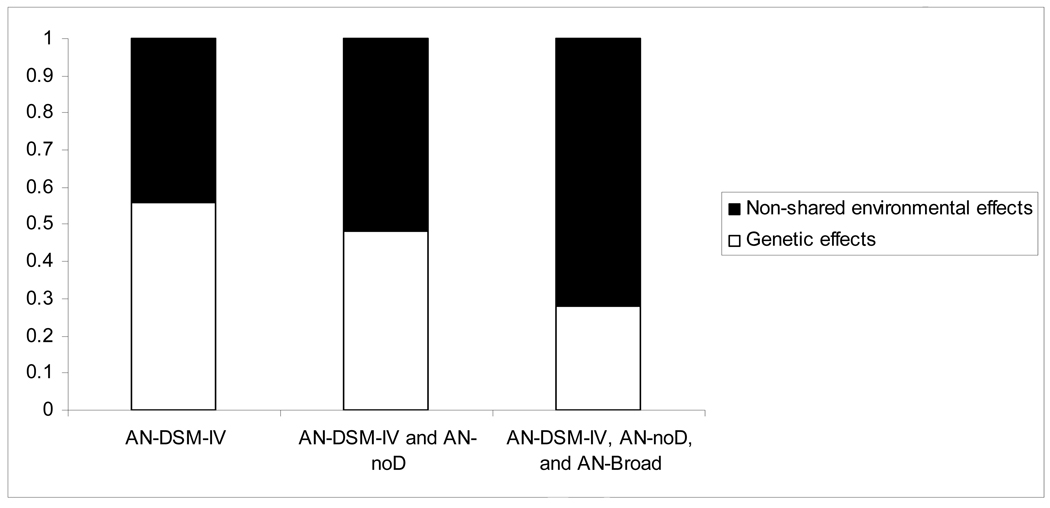
To assess heritability, the groups were reconfigured and nested: the broader definitions of illness included individuals with more narrow definitions. As shown in Figure 1, estimates for the genetic, shared environmental, and unique environmental effects for each model are as follows: for the most narrow sample where all met threshold AN-DSM-IV [a2=.56, 95% confidence interval (CI): (.00, .80), c2=.00, 95%CI: (.00, .72), and e2=.44, 95%CI: (.20, .79); model fit statistics: −2LL=493.4, degrees of freedom (df)=6932; Akaike’s Information Criterion (AIC)=−13370.6]; for a broader sample including those who met AN-DSM-IV and AN-noD [a2=.48, 95%CI: (.00, .70), c2=.00, 95%CI: (.00, .60), and e2=.52, 95%CI= (.30, .82); model fit statistics: −2LL=818.7, df=6932; AIC=−13045.4]; and for the broadest sample that included those who met AN- DSM-IV, AN-noD, and AN-Broad [a2=.28, 95%CI:(.00, .45), c2=.00, 95%CI:(.00, .28), and e2=.72, 95%CI= (.55, .90); model fit statistics: −2LL=2057.4, df=6932; AIC=−11806.6].
Figure 1.
Point estimates of percent of variance accounted for by genetic effects and non-shared environmental effects for broadening definitions of anorexia nervosa (AN)
AN-DSM-IV [met full Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria for AN]; AN-noD (met all DSM-IV criteria for AN except criterion D); AN-Broad (met broader version of DSM-IV criteria for AN)
Discussion
Differences in eating disorder symptomatology, comorbidity, and heritability emerge when varyingly stringent definitions of AN are applied. Thus, the common practice of relaxing diagnostic criteria for AN in research does influence the composition of study samples used, and is likely to impact subsequent results.
Eating disorder symptoms and behaviors
Lifetime lowest BMI displayed a monotonic decrease as AN definition narrowed. The mean BMI values in all three groups of women were below the 17.50 kg/m2 cut-off value that is used to diagnose AN in International Classification of Disease-10, yet the lowest lifetime minima varied by stringency of case definition. Attainment and maintenance of a very low BMI might be an important endophenotype of AN (Bulik et al., 2007). Previous investigations have noted that individuals who attain a very low BMI tend to be more fearful and anxious as children (Dellava et al., 2010), and lifetime minimum BMI has also yielded suggestive linkage signals in AN genetic linkage analyses (Bacanu et al., 2005). Single nucleotide polymorphisms in the serotonin 5-HT1B receptor gene have been associated with lower BMIs in individuals with BN (Levitan et al., 2001). Broadening the diagnostic criteria for AN clearly results in a sample of individuals with less extreme low BMI and might obscure important characteristics and biological mechanisms which characterize the ability to attain and maintain low BMIs in individuals with AN.
No significant differences were found in eating disorder behaviors between women with AN-DSM-IV and AN-noD. In addition, women with AN-DSM-IV and AN-noD exhibited more eating disorder behaviors than women with AN-Broad. Collectively, these observations suggest that broadening case definition might provide a different picture of clinical course and features of AN.
Psychiatric comorbidities
Women with AN-noD were more likely to exhibit comorbid psychopathology including major depression and phobias than women with AN-DSM-IV or AN-Broad. The reasons for these patterns are not entirely clear but could include differences in hormone levels across women with AN-DSM-IV, AN-noD, and AN-Broad.
Temperament and personality characteristics
No significant differences in temperament or personality characteristics emerged across the three groups. Personality and temperament characteristics have been shown to cluster together, independent of AN subtype (Jacobs et al., 2009), lending support to the notion that the same underlying personality and temperament structure might not discriminate according to the severity of AN despite differences in eating disorder symptomatology and psychiatric comorbidity.
Heritability estimates
The point estimates for heritability in the current study decreased as the diagnostic criteria for AN were broadened. The heritability estimates for the AN-DSM-IV only group and the group combining AN-DSM-IV with AN-noD were similar to those of previous studies (i.e., Bulik et al., 2006; Bulik et al., 2010). However, the estimate for the group combining AN-DSM-IV, AN-noD, and AN-Broad was lower than previous studies (i.e., Klump et al., 2001; Kortegaard et al., 2001; Wade et al., 2000). Possible reasons for the lower heritability estimates in the current study include increased measurement error with broadening criteria. This would result in an attenuation of the heritability estimate. Also, each AN symptom is differentially heritable (Mazzeo et al., 2009) so differences in criteria employed in each study could result in differences in heritability estimates across studies.
The decreasing heritability estimates with broadening definitions of AN found in the current study indicate that the criteria used for defining AN samples might influence the results of twin and molecular genetic studies. A narrower definition of AN would provide a clearer partitioning between affected and unaffected individuals which could result in a more homogeneous affected population, but a broader definition of AN would provide greater statistical power. Future studies will have to carefully weigh the pros and cons of large sample size versus case definition.
Limitations
These results must be considered in the context of the study limitations. First, diagnostic algorithms were constructed from data derived from a computer-administered self-report study. Although agreement between self-report and telephone was adequate, the complete impact of this approach is unclear as participants might be more forthcoming with sensitive information using computer-administered assessments and responses might be more reliable (Parks et al., 2006; Rankin et al., 2008), whereas the precision and detail provided by interview-based assessment could be lost. Second, individuals who responded to the invitation to participate could be inherently different from those who did not. However, these data appear to be representative of the population as the prevalence of AN in the STAGE data fell within the prevalence confidence intervals of other population-based Scandinavian samples (Bulik et al., 2006; Götestam et al., 1995; Isomaa et al., 2009). Third, generalizability could be limited because this sample was comprised of female Swedish Twins born between 1959 and 1985. Fourth, we were unable to correct for non-independence of these data in several models due to model failure which might result in false positive findings for those measures. Fifth, we did not know whether women were using birth control during their time of low weight. If women in the AN-noD group were menstruating because of the use of birth control medications, additional differences between the AN-noD group and the AN-DSM-IV group might have been obscured.
Findings from this study suggest that women with AN-DSM-IV, AN-noD, and AN-Broad exhibited differences in terms of lowest BMI, eating disorder symptomatology, and psychopathology. In addition, heritability estimates decreased as criteria were broadened. Broader inclusion criteria yield a substantially larger sample of women thereby increasing statistical power, but result in samples that differ in symptom profiles and comorbid psychiatric conditions. Although broadening of diagnostic criteria for rare disorders is often unavoidable, researchers should carefully justify the broadening of inclusion criteria and, when possible, evaluate differences that emerge in sample characteristics when broadening is applied.
Acknowledgements
We express our gratitude to all families who participated in this research.
Funding Source: This research was supported by NIH grants DK UO1 DK 066134 (NLP), R01 CA085739 (PF Sullivan: PI) T32MH076694-03 JED (CMB) Bethesda, MD, USA. Funding for the Swedish Twin Registry is provided by grants from the Swedish Department of Higher Education, Stockholm and the Swedish Research Council, Stockholm, Sweden. None of the funding sources had any role in this study other than providing funding.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interests: None
Contributors:
Jocilyn E. Dellava, Laura M. Thornton, and Cynthia M. Bulik contributed to the design of the study, planning of statistical analyses, and preparation of the manuscript. Jocilyn E. Dellava and Laura M. Thornton performed the statistical analyses. Paul Lichtenstein and Nancy L. Pedersen oversee the Swedish Twin Registry, obtained funding for STAGE, supervised data collection, and assisted with the design of the study and preparation of the manuscript. All authors have contributed to and approved the final manuscript.
References
- Agras WS, Crow S, Mitchell JE, Halmi KA, Bryson S. A 4-year prospective study of eating disorder NOS compared with full eating disorder syndromes. International Journal of Eating Disorders. 2009;42:565–570. doi: 10.1002/eat.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attia E, Roberto CA. Should amenorrhea be a diagnostic criterion for anorexia nervosa? International Journal of Eating Disorders. 2009;42:581–589. doi: 10.1002/eat.20720. [DOI] [PubMed] [Google Scholar]
- Bacanu S, Bulik C, Klump K, Fichter M, Halmi K, Keel P, Kaplan A, Mitchell J, Rotondo A, Strober M, Treasure J, Woodside D, Bergen A, Berrettini W, Kaye W, Devlin B. Linkage analysis of anorexia and bulimia nervosa cohorts using selected behavioral phenotypes as quantitative traits or covariates. American Journal of Medical Genetics. Part B Neuropsychiatric Genetics. 2005;139:61–68. doi: 10.1002/ajmg.b.30226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker AE, Thomas JJ, Pike KM. Should non-fat-phobic anorexia nervosa be included in DSM-V? International Journal of Eating Disorders. 2009;42:620–635. doi: 10.1002/eat.20727. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B. 1995;57:289–300. [Google Scholar]
- Bulik CM, Hebebrand J, Keski-Rahkonen A, Klump KL, Reichborn-Kjennerud T, Mazzeo SE, Wade TD. Genetic epidemiology, endophenotypes, and eating disorder classification. International Journal of Eating Disorders. 2007;40 Suppl:S52–S60. doi: 10.1002/eat.20398. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Tozzi F, Furberg H, Lichtenstein P, Pedersen NL. Prevalence, heritability, and prospective risk factors for anorexia nervosa. Archives of General Psychiatry. 2006;63:305–312. doi: 10.1001/archpsyc.63.3.305. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Thornton LM, Root TL, Pisetsky EM, Lichtenstein P, Pedersen NL. Understanding the relation between anorexia nervosa and bulimia nervosa in a Swedish national twin sample. Biological Psychiatry. 2010;67:71–77. doi: 10.1016/j.biopsych.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulik CM, Von Holle A, Siega-Riz AM, Torgersen L, Lie KK, Hamer RM, Berg CK, Sullivan P, Reichborn-Kjennerud T. Birth outcomes in women with eating disorders in the Norwegian Mother and Child cohort study (MoBa) International Journal of Eating Disorders. 2009;42:9–18. doi: 10.1002/eat.20578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cachelin R, Maher B. Is amenorrhea a critical criterion for anorexia nervosa? Journal of Psychosomatic Research. 1998;44:435–440. doi: 10.1016/s0022-3999(97)00268-7. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. The Temperament and Character Inventory (TCI): A Guide to its Development and Use. St. Louis, MO: Center for Psychobiology of Personality. Washington University; 1994. [Google Scholar]
- Crow SJ, Agras WS, Halmi K, Mitchell JE, Kraemer HC. Full syndromal versus subthreshold anorexia nervosa, bulimia nervosa, and binge eating disorder: a multicenter study. International Journal of Eating Disorders. 2002;32:309–318. doi: 10.1002/eat.10088. [DOI] [PubMed] [Google Scholar]
- Dalle Grave R, Calugi S, Marchesini G. Is amenorrhea a clinically useful criterion for the diagnosis of anorexia nervosa? Behaviour Research and Therapy. 2008;46:1290–1294. doi: 10.1016/j.brat.2008.08.007. [DOI] [PubMed] [Google Scholar]
- Dellava JE, Policastro P, Hoffman DJ. Energy metabolism and body composition in long-term recovery from anorexia nervosa. International Journal of Eating Disorders. 2009;42:415–421. doi: 10.1002/eat.20619. [DOI] [PubMed] [Google Scholar]
- Dellava JE, Thornton LM, Hamer RM, Strober M, Plotnicov K, Klump KL, Brandt H, Crawford S, Fichter MM, Halmi KA, Jones I, Johnson C, Kaplan AS, Lavia M, Mitchell J, Rotondo A, Treasure J, Woodside DB, Berrettini WH, Kaye WH, Bulik CM. Childhood anxiety associated with low BMI in women with Anorexia Nervosa. Behaviour Research and Therapy. 2010;48:60–67. doi: 10.1016/j.brat.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingemans AE, Spinhoven P, van Furth EF. Maladaptive core beliefs and eating disorder symptoms. Eating Behaviors. 2006;7:258–265. doi: 10.1016/j.eatbeh.2005.09.007. [DOI] [PubMed] [Google Scholar]
- Dominguez J, Goodman L, Sen Gupta S, Mayer L, Etu SF, Walsh BT, Wang J, Pierson R, Warren MP. Treatment of anorexia nervosa is associated with increases in bone mineral density, and recovery is a biphasic process involving both nutrition and return of menses. American Journal of Clinical Nutrition. 2007;86:92–99. doi: 10.1093/ajcn/86.1.92. [DOI] [PubMed] [Google Scholar]
- First M, Gibbon M, Williams J, Spitzer P, Staff M. SCID Screen Patient Questionnaire (SSPQ) and SCID SCREEN Patient Questionnaire-Extended (SSPQ-X), Computer Program for Windows TM, Software Manual. Washington, D.C: American Psychiatric Press, Inc; 1999. [Google Scholar]
- First MB, Pincus HA, Levine JB, Williams JB, Ustun B, Peele R. Clinical utility as a criterion for revising psychiatric diagnoses. American Journal of Psychiatry. 2004;161:946–954. doi: 10.1176/appi.ajp.161.6.946. [DOI] [PubMed] [Google Scholar]
- Frost R, Marten P, Lahart C, Rosenblate R. The dimensions of perfectionism. Cognitive Therapy and Research. 1990;14:449–468. [Google Scholar]
- Furberg H, Lichtenstein P, Pedersen NL, Thornton L, Bulik CM, Lerman C, Sullivan PF. The STAGE cohort: a prospective study of tobacco use among Swedish twins. Nicotine and Tobacco Research. 2008;10:1727–1735. doi: 10.1080/14622200802443551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfinkel P, Lin E, Goering P, Spegg C, Goldbloom D, Kennedy S, Kaplan A, Woodside D. Should amenorrhoea be necessary for the diagnosis of anorexia nervosa? Evidence from a Canadian community sample. British Journal of Psychiatry. 1996;168:500–506. doi: 10.1192/bjp.168.4.500. [DOI] [PubMed] [Google Scholar]
- Gendall K, Joyce P, Carter F, McIntosh V, Jordan J, Bulik C. The psychobiology and diagnostic significance of amenorrhea in patients with anorexia nervosa. Fertility and Sterility. 2006;85:1531–1535. doi: 10.1016/j.fertnstert.2005.10.048. [DOI] [PubMed] [Google Scholar]
- Götestam K, Agras W. General population-based epidemiology study of eating disorders in Norway. International Journal of Eating Disorders. 1995;18:119–126. doi: 10.1002/1098-108x(199509)18:2<119::aid-eat2260180203>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Grice DE, Halmi KA, Fichter MM, Strober M, Woodside DB, Treasure JT, Kaplan AS, Magistretti PJ, Goldman D, Bulik CM, Kaye WH, Berrettini WH. Evidence for a susceptibility gene for anorexia nervosa on chromosome 1. American Journal of Human Genetics. 2002;70:787–792. doi: 10.1086/339250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas VK, Kohn MR, Clarke SD, Allen JR, Madden S, Muller MJ, Gaskin KJ. Body composition changes in female adolescents with anorexia nervosa. American Journal of Clinical Nutrition. 2009;89:1005–1010. doi: 10.3945/ajcn.2008.26958. [DOI] [PubMed] [Google Scholar]
- Isomaa R, Isomaa AL, Marttunen M, Kaltiala-Heino R, Bjorkqvist K. The prevalence, incidence and development of eating disorders in Finnish adolescents-a two-step 3-year follow-up study. European Eating Disorder Review. 2009;17:199–207. doi: 10.1002/erv.919. [DOI] [PubMed] [Google Scholar]
- Jacobs MJ, Roesch S, Wonderlich SA, Crosby R, Thornton L, Wilfley DE, Berrettini WH, Brandt H, Crawford S, Fichter MM, Halmi KA, Johnson C, Kaplan AS, Lavia M, Mitchell JE, Rotondo A, Strober M, Woodside DB, Kaye WH, Bulik CM. Anorexia nervosa trios: behavioral profiles of individuals with anorexia nervosa and their parents. Psychological Medicine. 2009;39:451–461. doi: 10.1017/S0033291708003826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye WH, Bulik CM, Plotnicov K, Thornton L, Devlin B, Fichter MM, Treasure J, Kaplan A, Woodside DB, Johnson CL, Halmi K, Brandt HA, Crawford S, Mitchell JE, Strober M, Berrettini W, Jones I. The genetics of anorexia nervosa collaborative study: methods and sample description. International Journal of Eating Disorders. 2008;41:289–300. doi: 10.1002/eat.20509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye WH, Lilenfeld LR, Berrettini WH, Strober M, Devlin B, Klump KL, Goldman D, Bulik CM, Halmi KA, Fichter MM, Kaplan A, Woodside DB, Treasure J, Plotnicov KH, Pollice C, Rao R, McConaha CW. A search for susceptibility loci for anorexia nervosa: methods and sample description. Biological Psychiatry. 2000;47:794–803. doi: 10.1016/s0006-3223(99)00240-1. [DOI] [PubMed] [Google Scholar]
- Keel P, Klump K, Miller K, McGue M, Iacono W. Shared transmission of eating disorders and anxiety disorders. International Journal of Eating Disorders. 2005;38:99–105. doi: 10.1002/eat.20168. [DOI] [PubMed] [Google Scholar]
- Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. American Journal of Psychiatry. 2003;160:4–12. doi: 10.1176/appi.ajp.160.1.4. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Toward a scientific psychiatric nosology. Archives of General Psychiatry. 1990;47:969–973. doi: 10.1001/archpsyc.1990.01810220085011. [DOI] [PubMed] [Google Scholar]
- Klump KL, Miller KB, Keel PK, McGue M, Iacono WG. Genetic and environmental influences on anorexia nervosa syndromes in a population-based twin sample. Psychological Medicine. 2001;31:737–740. doi: 10.1017/s0033291701003725. [DOI] [PubMed] [Google Scholar]
- Kopelman MD, Fleminger S. Experience and perspectives on the classification of organic mental disorders. Psychopathology. 2002;35:76–81. doi: 10.1159/000065123. [DOI] [PubMed] [Google Scholar]
- Kortegaard LS, Hoerder K, Joergensen J, Gillberg C, Kyvik KO. A preliminary population-based twin study of self-reported eating disorder. Psychological Medicine. 2001;31:361–365. doi: 10.1017/s0033291701003087. [DOI] [PubMed] [Google Scholar]
- Levitan R, Kaplan AS, Masellis M, Basile V, Walker M, Lipson N, Siegel G, Woodside B, Macciardi F, Kennedy SH, Kennedy J. Polymorphism of the Serotonin 5-HT1B receptor gene (HTR1B) associated with minimum lifetime body mass index in women with bulimia nervosa. Biological Psychiatry. 2001:640–643. doi: 10.1016/s0006-3223(01)01201-x. [DOI] [PubMed] [Google Scholar]
- Lichtenstein P, De Faire U, Floderus B, Svartengren M, Svedberg P, Pedersen N. The Swedish Twin Registry: a unique resource for clinical, epidemiological and genetic studies. Journal of Internal Medicine. 2002;252:184–205. doi: 10.1046/j.1365-2796.2002.01032.x. [DOI] [PubMed] [Google Scholar]
- Lichtenstein P, Sullivan PF, Cnattingius S, Gatz M, Johansson S, Carlstrom E, Bjork C, Svartengren M, Wolk A, Klareskog L, de Faire U, Schalling M, Palmgren J, Pedersen NL. The Swedish Twin Registry in the third millennium: an update. Twin Research and Human Genetics. 2006;9:875–882. doi: 10.1375/183242706779462444. [DOI] [PubMed] [Google Scholar]
- Loeb KL, Walsh BT, Lock J, le Grange D, Jones J, Marcus S, Weaver J, Dobrow I. Open trial of family-based treatment for full and partial anorexia nervosa in adolescence: evidence of successful dissemination. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:792–800. doi: 10.1097/chi.0b013e318058a98e. [DOI] [PubMed] [Google Scholar]
- Lucas AR, Beard CM, O'Fallon WM, Kurland LT. 50-year trends in the incidence of anorexia nervosa in Rochester, Minn.: a population-based study. American Journal of Psychiatry. 1991;148:917–922. doi: 10.1176/ajp.148.7.917. [DOI] [PubMed] [Google Scholar]
- Mazzeo SE, Mitchell KS, Bulik CM, Reichborn-Kjennerud T, Kendler KS, Neale MC. Assessing the heritability of anorexia nervosa symptoms using a marginal maximal likelihood approach. Psychological Medicine. 2009;39:463–473. doi: 10.1017/S0033291708003310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milos G, Spindler A, Schnyder U, Fairburn CG. Instability of eating disorder diagnoses: prospective study. British Journal of Psychiatry. 2005;187:573–578. doi: 10.1192/bjp.187.6.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JE, Cook-Myers T, Wonderlich SA. Diagnostic criteria for anorexia nervosa: looking ahead to DSM-V. International Journal of Eating Disorders. 2005;37 Suppl:S95–S97. doi: 10.1002/eat.20125. [DOI] [PubMed] [Google Scholar]
- Neale M, Boker S, Xie G, Maes H. Mx: Statistical Modeling. 5th ed. Richmond, VA: Medical College of Virginia, Department of Psychiatry; 2001. [Google Scholar]
- Parks KA, Pardi AM, Bradizza CM. Collecting data on alcohol use and alcohol-related victimization: a comparison of telephone and Web-based survey methods. Journal of Studies on Alcohol and Drugs. 2006;67:318–323. doi: 10.15288/jsa.2006.67.318. [DOI] [PubMed] [Google Scholar]
- Perkins PS, Klump KL, Iacono WG, McGue M. Personality traits in women with anorexia nervosa: evidence for a treatment-seeking bias? International Journal of Eating Disorders. 2005;37:32–37. doi: 10.1002/eat.20064. [DOI] [PubMed] [Google Scholar]
- Poyastro Pinheiro A, Thornton LM, Plotonicov KH, Tozzi F, Klump KL, Berrettini WH, Brandt H, Crawford S, Crow S, Fichter MM, Goldman D, Halmi KA, Johnson C, Kaplan AS, Keel P, LaVia M, Mitchell J, Rotondo A, Strober M, Treasure J, Woodside DB, Von Holle A, Hamer R, Kaye WH, Bulik CM. Patterns of menstrual disturbance in eating disorders. International Journal of Eating Disorders. 2007;40:424–434. doi: 10.1002/eat.20388. [DOI] [PubMed] [Google Scholar]
- Rankin KM, Rauscher GH, McCarthy B, Erdal S, Lada P, Il'yasova D, Davis F. Comparing the reliability of responses to telephone-administered versus self-administered Web-based surveys in a case-control study of adult malignant brain cancer. Cancer Epidemiology Biomarkers and Prevention. 2008;17:2639–2646. doi: 10.1158/1055-9965.EPI-08-0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reba L, Thornton L, Tozzi F, Klump KL, Brandt H, Crawford S, Crow S, Fichter MM, Halmi KA, Johnson C, Kaplan AS, Keel P, LaVia M, Mitchell J, Strober M, Woodside DB, Rotondo A, Berrettini WH, Kaye WH, Bulik CM. Relationships between features associated with vomiting in purging-type eating disorders. International Journal of Eating Disorders. 2005;38:287–294. doi: 10.1002/eat.20189. [DOI] [PubMed] [Google Scholar]
- Root TL, Pisetsky EM, Thornton L, Lichtenstein P, Pedersen NL, Bulik CM. Patterns of co-morbidity of eating disorders and substance use in Swedish females. Psychological Medicine. 2010;40:105–115. doi: 10.1017/S0033291709005662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanci L, Coffey C, Olsson C, Reid S, Carlin JB, Patton G. Childhood sexual abuse and eating disorders in females: findings from the Victorian Adolescent Health Cohort Study. Achieves of Pediatric and Adolescent Medicine. 2008;162:261–267. doi: 10.1001/archpediatrics.2007.58. [DOI] [PubMed] [Google Scholar]
- Santonastaso P, Bosello R, Schiavone P, Tenconi E, Degortes D, Favaro A. Typical and atypical restrictive anorexia nervosa: Weight history, body image, psychiatric symptoms, and response to outpatient treatment. International Journal of Eating Disorders. 2009;42:464–470. doi: 10.1002/eat.20706. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT® Software: Version 9. Cary, NC: SAS Institute, Inc; 2004. [Google Scholar]
- Schapiro IR, Ross-Petersen L, Saelan H, Garde K, Olsen JH, Johansen C. Extroversion and neuroticism and the associated risk of cancer: A Danish cohort study. American Journal of Epidemiology. 2001;153:757–763. doi: 10.1093/aje/153.8.757. [DOI] [PubMed] [Google Scholar]
- Schebendach JE, Mayer LE, Devlin MJ, Attia E, Contento IR, Wolf RL, Walsh BT. Dietary energy density and diet variety as predictors of outcome in anorexia nervosa. American Journal of Clinical Nutrition. 2008;87:810–816. doi: 10.1093/ajcn/87.4.810. [DOI] [PubMed] [Google Scholar]
- Sullivan PF, Eaves LJ. Evaluation of analyses of univariate discrete twin data. Behavior Genetics. 2002;32:221–227. doi: 10.1023/a:1016025229858. [DOI] [PubMed] [Google Scholar]
- Thomas JJ, Vartanian LR, Brownell KD. The relationship between eating disorder not otherwise specified (EDNOS) and officially recognized eating disorders: meta-analysis and implications for DSM. Psychological Bulletin. 2009;135:407–433. doi: 10.1037/a0015326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade TD, Bulik CM, Neale M, Kendler KS. Anorexia nervosa and major depression: shared genetic and environmental risk factors. American Journal of Psychiatry. 2000;157:469–471. doi: 10.1176/appi.ajp.157.3.469. [DOI] [PubMed] [Google Scholar]
- Wade TD, Tiggemann M, Bulik CM, Fairburn CG, Wray NR, Martin NG. Shared temperament risk factors for anorexia nervosa: a twin study. Psychosomatic Medicine. 2008;70:239–244. doi: 10.1097/PSY.0b013e31815c40f1. [DOI] [PubMed] [Google Scholar]
- Walters EE, Kendler KS. Anorexia nervosa and anorexic-like syndromes in a population-based female twin sample. American Journal of Psychiatry. 1995;152:64–71. doi: 10.1176/ajp.152.1.64. [DOI] [PubMed] [Google Scholar]
- Watson T, Andersen A. A critical examination of the amenorrhea and weight criteria for diagnosing anorexia nervosa. Acta Psychiatrica Scandinavia. 2003;108:175–182. doi: 10.1034/j.1600-0447.2003.00201.x. [DOI] [PubMed] [Google Scholar]
- Wild B, Friederich HC, Gross G, Teufel M, Herzog W, Giel KE, de Zwaan M, Schauenburg H, Schade-Brittinger C, Schafer H, Zipfel S. The ANTOP study: focal psychodynamic psychotherapy, cognitive-behavioural therapy, and treatment-as-usual in outpatients with anorexia nervosa--a randomized controlled trial. Trials. 2009;10:23. doi: 10.1186/1745-6215-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilfley DE, Bishop ME, Wilson GT, Agras WS. Classification of eating disorders: toward DSM-V. International. Journal of Eating Disorders. 2007;40 Suppl:S123–S129. doi: 10.1002/eat.20436. [DOI] [PubMed] [Google Scholar]