Abstract
Objective
As perinatally HIV-infected (PHIV+) youth enter adolescence, they are at high risk for poor behavioral and health outcomes. This study examines relationships between youth mental health problems and sexual and substance use risk behavior, the impact of caregiver mental health and family functioning on youth mental health and risk behavior outcomes, and the role of youth HIV status in this process.
Method
Participants were recruited from four medical centers. Individual interviews were administered to 193 PHIV+ and 127 perinatally HIV exposed, but uninfected (PHIV−) 9–16 year old boys and girls and their primary caregivers. Participants were primarily African American and Latino. The interview assessed child sexual and drug risk behavior, child and caregiver mental health and family functioning.
Results
Exploratory latent-variable structural equation modeling revealed no differences in rates of sexual risk behavior or substance use between PHIV+ and PHIV− youth. However, adolescent mental health was significantly associated with sexual risk behavior and substance use. Caregiver mental health was associated with youth mental health and indirectly with sexual risk behavior and drug use through its impact on youth mental health. Family functioning did not significantly predict youth outcomes.
Conclusions
Over and above other key environmental factors and family functioning, youth and caregiver mental health problems are related to sex and drug use risk behaviors in PHIV+ and PHIV-youth. Given high rates of youth and caregiver mental health problems in this population, family-based mental health interventions may be a key component of HIV prevention programs for perinatally-HIV-exposed youth.
Keywords: pediatric HIV, mental health, sex, substance use
With the advent of antiretroviral medication (ART), perinatally HIV-infected (PHIV+) children live longer, healthier lives. The pediatric HIV epidemic in the United States (US) and other developed nations is increasingly an adolescent phenomenon.1 Adolescence is a vulnerable period for mental health problems and a time for experimentation with sexual behavior and substance use.2,3 PHIV+ youth may be a high-risk group for problems in these domains not only because they must cope with a chronic, stigmatizing illness, but because they are overrepresented in high-risk contexts that include poverty, inner-city stress, familial mental health problems, and family disruption.4–6 Although clinical reports indicate emotional and behavioral problems in this population,4–6 very few studies of PHIV+ adolescents exist, as they are only now reaching adolescence in relatively large numbers.7 There is an urgent need to understand the sexual and drug use risk behaviors of PHIV+ youth as these behaviors may not only be detrimental to their health and well-being, but may place others at risk for secondary HIV transmission.
The few published studies of PHIV+ adolescents suggest that although rates of risk behavior may be less than other populations, these youth are engaging in substance use and sexual behaviors, and are doing so at a young age. One cross-sectional study found that 33% of 13– 24 year old PHIV+ youths had initiated vaginal intercourse, 26% of whom reported the first occurrence before age 15 years.8 Another study reported age disparities between PHIV+ youth and the general population in age of first sexual experience (age 15 and 17 years, respectively) and first pregnancy (age 17 and 18–19 years, respectively).9,10 Finally, among PHIV+ youth ages 9–16 years, 16% reported histories of substance use, with alcohol and marijuana use significantly associated with high risk sexual activity.11 Unfortunately, most of these studies do not include comparison groups to examine the role of perinatal HIV infection and other predictors of risk behavior that might inform interventions.
Among general adolescent populations, mental health problems have been key predictors of sexual and drug risk behavior.12–14 Adolescents with psychiatric problems are at increased risk for engaging in unsafe sexual behavior and drug use due to impaired judgment and problem-solving ability, low self-esteem, and poor interpersonal relationships, with some studies showing an increased risk for acquiring HIV infection.15,16 Several investigators have reported high rates of mental health problems among PHIV+ children and adolescents.17–19
Family influences on HIV/AIDS prevention and care have received increasing attention.20 Adolescence marks the time when children begin to move away from their parents towards peers, while they are still reliant on parents for guidance.2 A substantial body of literature has documented the association of parent and child mental health,21–23 although less is understood about the influence of parent mental health on youth substance use24 and sexual risk behavior. Other types of family influences on risk behavior have been identified. For example, increased parental supervision and involvement have been associated with better youth psychological adjustment and less sexual risk behavior and substance use in uninfected adolescents.25–27 Positive, frequent and open parent-child communication also have predicted better youth psychological adjustment,28 and less sexual risk behavior.29,30 To date, the role of family influences and the pathways by which family factors promote well-being and reduce risk behavior in PHIV+ youth is not well understood. PHIV+ youth may have experienced parental loss or parental illness due to HIV.4 Current family influences, such as caregiver well-being (i.e., their current HIV-status and mental health), and caregiver-child relationships may be important determinants of youth risk behavior.
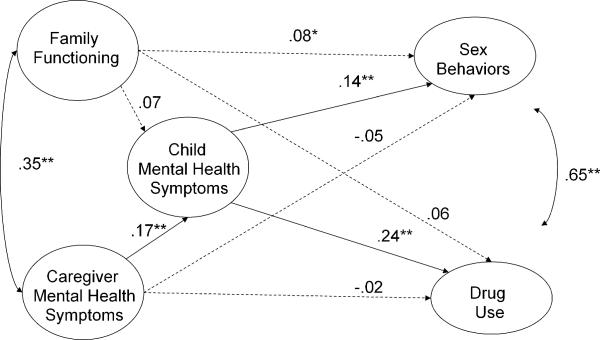
In conclusion, PHIV+ youth may be at high risk for mental health problems and sexual and drug use risk behaviors. The impact of perinatal HIV-infection on these outcomes has been difficult to determine because of the limited number of controlled studies and the confluence of biomedical, genetic, and environmental factors that place this population at risk. Given the significant public health ramifications of poor behavioral outcomes in this population, there is a need to examine PHIV+ youth's mental health and behavioral risk problems utilizing appropriate comparison groups. There is also a need to elucidate determinants of their risk behavior that are amenable to interventions. Using baseline data from one of the largest US-based studies of psychosocial determinants of behavior with a sample composed of PHIV+ and PHIV− (perinatally HIV-exposed, but uninfected ) youth, the goals of this study are to examine 1) the association of youth mental health and sexual and drug risk behaviors; 2) the role of caregiver mental health and family functioning in influencing youth mental health, and sexual and drug risk behavior; and 3) differences in these relationships by youth and current caregiver HIV status. To answer these questions we test a hypothesized model (see Figure 1) using structural equation modeling (SEM) which allows us to examine complex relationships between multiple constructs.31 We examine both the direct effects of family functioning and caregiver mental health on HIV risk behaviors and the indirect effects of these family influences on HIV risk behaviors as mediated by child mental health, a variable associated with both family influences and child risk behaviors.
Figure 1.
Exploratory Structural Equation Model of the association between family influences on youth's mental health and onset of sexual and drug behaviors. Magnitudes of association are presented as standardized Betas.
*p<.10 **p<.05
METHOD
Participants and Procedures
Data for this paper come from the baseline interview of Project CASAH (Child and Adolescent Self-Awareness and Health Study). Participants were recruited from four medical centers in New York City (NYC) providing primary care to HIV-affected families. Inclusion criteria for study participation were: 1) youth ages 9 to 16 years with perinatal exposure to HIV, 2) adequate caregiver and youth cognitive capacity to complete the interview, 3) English or Spanish speaking, and 4) caregiver with legal capacity to sign consent for the child's participation (foster care parents can not consent for child participation in research in NYC). Among 443 eligible participants identified, 6% could not be contacted by providers, and 11% refused contact with the researchers. A total of 367 eligible participants (83%) were approached, of whom 340 (92%) were enrolled, including 206 PHIV+ youths, and 134 PHIV− youths. Data were not collected on patients who were not approached or refused participation.
Data for these analyses come from 1) baseline caregiver and adolescent interviews, and 2) medical charts. Caregivers and youth were interviewed simultaneously but separately over two 60–90 minute interview sessions, approximately 2–4 weeks apart. Data for this paper come from the 320 youths (193 PHIV+,127 PHIV−) and their caregivers who completed both interview sessions (95% of PHIV+ and 96% of PHIV− youths of those enrolled) and had no missing data on key study variables (5 caregivers had missing data).
Institutional Review Board approval was received from all participating sites. All caregivers provided written informed consent for themselves and youths. Youths provided written assent. Monetary reimbursement for time and transportation was provided.
Measures
Child sexual behavior was assessed with the Adolescent Sexual Behavior Assessment (ASBA; C.D., unpublished data, 2006), developed by the authors based on The Sexual Risk Behavior Assessment Schedule for Youths (SERBAS-Y)32 and interviews with HIV+ youths and their primary care providers. The ASBA is a relatively brief measure of sexual behavior appropriate for younger children in the study (via gateway questions). The assessment was randomly administered via ACASI (audio computer assisted self-interview) or face-to-face interview as part of a sub-study. Mixed results have been found in the literature comparing self-reported sexual behavior via ACASI or face-to-face interviews.33, 34 We found no differences in youths' sexual behavior reported across these two procedures in this set of analyses and in several other analyses11,35 and therefore have combined the data. The following sexual behaviors (yes/no) were examined: lifetime kissing, touching a partner's genitals, oral sex, penetrative (vaginal or anal) sex, and unprotected penetrative sex. We aggregated reports of vaginal and anal sex behavior into one variable (“penetrative sex”) given the low frequency of anal sex and the co-occurrence of vaginal and anal sex.35 We were unable to distinguish consensual from non-consensual sex.
Child substance use was assessed using modules from The Diagnostic Interview Schedule for Children-IV (DISC-IV),36 one of the most extensively used and well-validated structured diagnostic instruments to assess diagnoses defined by the American Psychiatric Association's DSM system.37 Youth were interviewed about lifetime and recent use of cigarettes, alcohol, marijuana, and other illicit drugs (e.g. cocaine, heroin). Scoring follows DSM criteria for substance use disorders. We examined two dichotomous (yes/no) variables: 1) has ever used drugs or alcohol and 2) meets criteria for alcohol or drug use disorder in the past year.
Youth mental health was assessed with the Child Depression Inventory (CDI),38 a 28 item measure of depression symptoms developed for children ages 7–19 years, and the Trait Scale of the State-Trait Anxiety Inventory-Child Version (STAI)39, a 20-item measure that assesses how anxious the child generally feels. Youth reported on their experience of symptoms using 3 (CDI) or 4 (STAI) point Likert-type scales. Total scores are created for each measure with excellent psychometric properties.38,39
Caregiver mental health was assessed with two well-validated self-report measures, the Beck Depression Inventory (BDI)40,41 and the trait scale of the State-Trait Anxiety Inventory (STAI),39 corresponding with the youth measures. The BDI was designed to assess the intensity of 21 depressive symptoms experienced in the past two weeks. The trait scale of the STAI consists of 20 items measuring how the respondent feels in general. For each measure, a total score was created.
Demographics included child and caregiver age, gender, ethnicity, and HIV status; caregiver work, education, and relationship to child; and household composition and income.
Family Functioning was assessed with the Parent Child Relationship Inventory (PCRI)42, a self-report instrument for caregivers acting in a parental role. Two subscales were used: 1) involvement (i.e., spending time with and showing interest in the child) and 2) quality of communication (i.e., parent empathy and conversation across situations). Each item is rated on a 4-point scale (0=Strongly Agree to 3=Strongly Disagree). High scores on communication and involvement scales indicate poor communication and low caregiver involvement with youth.
Analytic strategy
We tested for differences across study measures by youth HIV status using t-tests and χ2 statistics, respectively, and tested the bivariate association between study variables. Using Fisher's r-to-Z conversion, with a Z critical value of 1.96 (two-tailed test; p < .05), we tested whether the magnitude of the observed correlations were statistically significant by HIV status. Due to the multiple comparisons conducted, we performed a post-hoc correction to decrease Type-I error using the Bonferroni correction. The absence of statistically-significant differences by youth HIV status in the observed correlations (even without bonferroni correction) provided us with evidence that it was not appropriate to run SEM analyses separately by youth HIV status. Consequently, the full sample was used in all subsequent analyses.
We used EQS version 6.1 for exploratory latent-variable structural modeling,43 an approach that permits the testing of various endogenous factors simultaneously.44 For example, we were able to adjust for the co-occurrence of sexual behaviors and substance use among youth while testing their association with family variables. This strategy allowed us to examine multiple structural path models (e.g., direct effects and mediation) while adjusting for the reliability of the observed measures.45 Our estimation of model coefficients was improved by using an estimated covariance matrix generated from the variables' observed covariance matrix. The comparisons between the observed and estimated covariance matrices provided overall goodness-of-fit measures, allowed for model modifications, and provided a straightforward approach for group comparisons. We present our findings following proposed guidelines46 for adequate reporting of SEM and provide three goodness-of-fit indices: Bentler-Bonnet's Normed Fit Index (NFI), Bentler-Bonnet's Non-Normed Fit Index (NNFI), and the Comparative Fit Index (CFI). We provide information on the root mean-square error of approximation (RMSEA) as an index of misfit.47 Hu & Bentler (1999) suggest values of .90 or higher among fit indices and values of .06 or lower for RMSEA as acceptable indications of well-fitting models.48 We determined statistical significance based on one-sided t-tests (p≤.05) given our existing theoretical and empirical understanding of the associations between study variables; however, in light of the scarce data available for this population, we also inform trend-like data (p≤.10).
Results
Demographic Characteristics and Differences by HIV Status
PHIV+ (n=193) and PHIV− (n=127) youths were comparable for all child demographics and the majority of caregiver variables. Each group had approximately 50% boys and girls and younger (9–12 years) and older (13–16) age groups (M = 12.15 years; SD=2.26). The majority of youth in both groups were African American (55%) and Latino (31%) with predominantly female caregivers (87% women) who received a high school education (M=11th grade) and had a mean age of 48.33 years (SD = 12.15). The two groups differed on three caregiver variables. Families of PHIV+ youth reported a slightly higher average annual income ($25,000–30,000 vs.$20,000–25,000; t=−2.44, p≤.05), yet the average across both groups was under the NYC poverty line for a family of four people. While all participants were born to HIV+ mothers, significantly fewer PHIV+ youth were living with a birth parent (36% vs. 70%;χ2= 36.09; p≤.001), and thus, fewer were living with an HIV+ caregiver (31% vs. 69%;χ2= 43.96, p≤.001). Corresponding with this finding, more PHIV+ youth reported that a long term primary caregiver (e.g. biological or adoptive parent) was deceased (53% vs. 24%; χ2 = 9.84; p=.001, n=297). Among PHIV+ youths, the majority was taking ART (84%) and knew their HIV status (70%).
Descriptive data on substance use and sexual behavior
The most prevalent substance used by both groups was alcohol (13% of PHIV+ and 16% of PHIV− youth). Use of marijuana (4% for each group) and cigarettes (8% of PHIV+ and 7% of PHIV− youth) was less frequent. Only 3% of youth met criteria for a substance abuse disorder (1% alcohol; 3% marijuana). Fifty-eight percent of the youth reported no sexual behavior; 35% reported kissing, 17% reported touching, 7% reported oral sex, 11.1% reported vaginal and 2.9% reported anal sex. Among the sexually active, 33% reported unprotected sex (40% PHIV+ and 26% PHIV−;χ2= .821; ns). As noted, we found no differences across mental health, sexual and substance use risk behavior, and family variables by youth HIV status. Consequently, we tested the structural equation models using the full sample. Table 1 presents an intercorrelation matrix of all study variables by HIV status; Table 2 details study variables' descriptive statistics.
Table 1.
Study Variable intercorrelation matrix, by HIV statusa
| Measured Variable+ | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | --- | −.13 | −.04 | .19* | .28* | −.02 | −.02 | −.06 | −.23* | .41* | .19* | .24* | .17* | .32* | .24* | .32* |
| 2. Gender | .07 | --- | .01 | −.09 | −.11 | −.10 | −.13 | .17* | .15* | .04 | .10 | −.01 | −.04 | −.15* | −.13 | −.13 |
| 3. Caregiver HIV | −.12 | .03 | --- | .01 | −.07 | .27* | .30* | .10 | .04 | .07 | .03 | .03 | .01 | .11 | .15* | .19* |
| 4. Communication | .09 | .20* | .06 | --- | .64* | .20* | .32* | .13 | −.02 | .09 | .04 | .03 | .13 | .15* | .04 | .17* |
| 5. Involvement | .08 | −.03 | −.09 | .67* | --- | .13 | .20* | .13 | −.02 | .12 | .06 | .11 | .15* | .16* | .10 | .16* |
| 6. Caregiver Depression | .07 | −.17 | .23* | .21* | .12 | --- | .75* | .12 | .04 | −.02 | .05 | −.02 | .03 | −.03 | .02 | .01 |
| 7. Caregiver Anxiety | .06 | −.01 | .23* | .38* | .19* | .72* | --- | .25* | .13 | .03 | .06 | −.07 | .03 | −.02 | .01 | .03 |
| 8. Child Depression | .30* | .19* | −.09 | .13 | .13 | .14 | .13 | --- | .55* | .08 | .19* | .18* | .16* | .08 | .08 | .08 |
| 9. Child Anxiety | −.06 | .17 | −.02 | −.05 | .01 | .12 | .08 | .58* | --- | −.02 | .06 | −.01 | −.04 | −08 | .01 | −.03 |
| 10. Alcohol | .52* | −.01 | −.07 | .12 | .05 | .10 | .20 | .22* | .09 | --- | .38* | .46* | 20* | .34* | .28* | .39* |
| 11. Cigarettes | .36* | .12 | .11 | .01 | .04 | −.15 | −.02 | .33* | .17 | .51* | --- | .48* | .18* | .35* | .27* | .19* |
| 12. Marijuana | .41* | .05 | .08 | .11 | .03 | −.04 | .06 | .19* | .06 | .52* | .53* | --- | .39* | .28* | .49* | .37* |
| 13.DISC Diagnosis | .36* | .03 | .02 | −.02 | −.05 | .02 | .09 | .25* | .18 | .56* | .51* | .83* | --- | .15* | .32* | .24* |
| 14. Touching | .49* | −.03 | .01 | −.09 | −.03 | −.06 | −.09 | .19* | .07 | .49* | .44* | .45* | .48* | --- | .51* | .66* |
| 15. Oral | .40* | .02 | .03 | .05 | .10 | −.02 | .04 | .18* | .08 | .56* | .50* | .64* | .66* | .66* | --- | .71* |
| 16. Penetration | .47* | −.01 | −.10 | −.02 | .07 | .02 | .01 | .15 | .03 | .44* | .36* | .38* | .40* | .78* | .68* | --- |
Top diagonal refers to HIV-positive youth (N = 193); bottom diagonal refers to HIV-negative youth (N = 127).
p < .05
Table 2.
Descriptive statistics of study variables by HIV status
| Subscale | HIV− (N=127) | HIV+ (N=193) | Total (N=320) | t/χ2 | Cronbach's Alpha |
|---|---|---|---|---|---|
| Mean (sd) | |||||
| Family Functioning | .78 | ||||
| Communication | .75(.43) | .74(.41) | .74(.42) | .19 | |
| Involvement | .70(.35) | .74(.33) | .73(.34) | .19 | |
| Caregiver Mental Health symptoms | .74 | ||||
| Depression | 8.84(8.54) | 7.18(7.18) | 7.84(7.78) | 1.80 | |
| Anxiety | 34.92(11.46) | 32.62(10.75) | 33.54(11.08) | 1.82 | |
| Child Mental Health Symptoms | .70 | ||||
| Depression | 6.22(5.25) | 6.65(5.93) | 6.48(5.67) | −.66 | |
| Anxiety | 33.35(7.55) | 32.99(7.92) | 33.14(7.76) | .40 | |
| N(%) | |||||
| Child Substance Use | .74 | ||||
| Alcohol | 20(16%) | 25(13%) | 45(14%) | .50 | |
| Cigarette | 8(6%) | 8(4%) | 16(5%) | .75 | |
| Marijuana | 10(8%) | 8(4%) | 18(6%) | 2.01 | |
| DISC diagnosis | 7(6%) | 3(2%) | 10(3%) | 3.96* | |
| Child Sexual Behaviors | .83 | ||||
| Touching | 19(15%) | 39(20%) | 58(18%) | 1.42 | |
| Oral | 11(9%) | 12(6%) | 23(7%) | .69 | |
| Penetration | 18(14%) | 19(10%) | 37(12%) | 1.40 | |
| Caregiver Type: Bio parent | 88 (69%) | 68 (35%) | 156 (49%) | ||
| Relative | 20 (16%) | 52 (27%) | 72 (22%) | ||
| Non-Relative | 19 (15%) | 73 (38%) | 92 (29%) | ||
p ≤ .05;
p ≤ .01
Testing the measurement model
Prior to testing the structural models, we estimated the indicators' appropriateness for the latent factors in our analyses (i.e., measurement model). The error variances for family communication, caregiver anxiety symptoms, and child depression score were close to zero in the measurement model. Consequently, we fixed the residual variance for both terms to .005. The measurement model converged in 9 iterations and showed the data had an acceptable fit, [χ2(58, N = 320) = 143.67, p < .05; NFI = 1.0, NNFI = 1.0, CFI = 1.0, RMSEA = .07]. In light of the model's fit, we used this measurement model in our subsequent structural model tests. Table 3 and Table 4 present the factor loadings for all indicators, and the estimated correlations among latent-variables, respectively.
Table 3.
Factor Loadings of Indicators for Family Functioning, Caregiver Mental Health Symptoms, Child Mental Health Symptoms, Child Substance Use, and Child Sexual Behavior.
| Factor | Indicator | Loading | Error |
|---|---|---|---|
| Family Functioning | 1. Communication | .985 | .174 |
| 2. Involvement | .657 | .754 | |
| Caregiver Mental Health Symptoms | 3. Depression | .750 | .661 |
| 4. Anxiety | .992 | .130 | |
| Child Mental Health Symptoms | 5. Depression | 1.0 | .013 |
| 6. Anxiety | .562 | .827 | |
| Child Substance Use | 7. Alcohol | .621 | .784 |
| 8. Cigarettes | .646 | .763 | |
| 9. Marijuana | .871 | .492 | |
| 10.DISC Diagnosis | .765 | .644 | |
| Child Sexual Behaviors | 11. Touching | .759 | .651 |
| 12. Oral | .801 | .598 | |
| 13. Penetration | .873 | .488 |
Table 4.
Estimated correlations among latent factors.
| Latent factor | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Family Functioning | - | ||||
| 2. Caregiver Mental Health Symptoms | .35* | - | |||
| 3. Child Mental Health Symptoms | .13* | .20* | - | ||
| 4. Drug Use | .08 | .05 | .24* | - | |
| 5. Sexual Behavior | .08 | .01 | .14* | .66* |
p ≤ .05
Testing the structural model
The structural model in Figure 1 had a good fit. Consideration was given to potential model modifications suggested by the Lagrange Multiplier Test for adding parameters and the Wald Test for dropping parameters, but we opted to avoid making any changes because they were unsubstantiated by the literature and reduced the likelihood of capitalizing on chance.49
Given the clustering effect typically found between youth substance use and sexual behaviors,50 our model accounted for the correlation between these two outcomes' error terms (r = .65; p ≤ .05). Youth mental health symptoms were directly associated with youth substance use (b = .007, se = .002; β =.24; p ≤ .05) and sexual behavior (b = .009, se = .004; β =.14; p ≤ .05).
After adjusting for the covariance between caregiver mental health and family functioning (r = .35; p ≤ .05), we found caregiver mental health had a direct effect on youth mental health (b = 1.36, se = .48; β =0.17; p ≤ .05). We found no support that youth mental health was associated with family functioning after accounting for caregiver's mental health (b = 1.40, se = 1.16; β = 0.07; n.s.). We also found no direct association between caregiver mental health and youth sexual behavior (b = −.02, se = .03; β =−.05; n.s.). However, we found an indirect (mediational) effect of caregiver mental health symptoms on youth sexual behavior via youth mental health symptoms (b = .01, se = .007; β =.02; p ≤ .05). Although not statistically significant, we found a marginal association between family functioning and youth sexual behavior (b = 0.10, se = .08; β = .08; p ≤ .10). We did not find an indirect effect of family functioning and youth sexual behavior via youth mental health (b = .01, se = .01; β =.01; n.s.).
We found no direct association of either caregiver mental health (b = −.004, se = .02; β = .02; n.s.) or family functioning (b = 0.03, se = .04; β =.06; n.s.) with youth substance use, and no indirect effect of family functioning on youth substance use through youth mental health (b = .01, se = .008; β =.02; n.s.). We did find an indirect effect of caregiver mental health symptoms on youth substance use via youth mental health symptoms (b = .01, se = .004; β =.04; p ≤ .05).
Examination of caregiver HIV status effects
As a final step, we compared the structural model's adequacy based on caregivers' HIV− status to test whether HIV+ and HIV− caregivers had comparable models in the associations between family variables and the three youth outcomes. The caregiver HIV status differences model indicated an acceptable fit for both models [χ2 (df= 124, PHIV+ N = 146, PHIV− N = 174) = 240.80; NFI = 1.0, NNFI = 1.0, CFI = 1.0, RMSEA = .08]; however, we found no statistically-significant differences by caregiver HIV status in the model estimates.
Discussion
Given the epidemiology of HIV disease in US women, the majority of PHIV+ and PHIV− youths live in the inner-city, confronted by stress, poverty, and disrupted families, all of which have been associated with risk behavior in other populations.4 Our data suggest that PHIV+ and PHIV− youth are engaging in sexual behaviors and substance use, although prevalence rates may be slightly lower than other populations, with no differences between PHIV+ and PHIV− groups. Among the modest number of sexually-active youth, both groups reported high rates of unprotected sex and substance use. Although we did not find an association between HIV status and mental health symptoms or risk behaviors, our findings underscore that youth and caregiver mental health may play critical roles in influencing the risk behaviors of perinatally HIV− exposed youths, and may be important targets for family-based HIV prevention programs.
Similar to studies of youth unaffected by HIV,12,50–53 adolescent mental health was a significant predictor of youth's onset of sexual behavior and substance use. Our study focused on internalizing mental health problems, including youth depression and anxiety symptoms. Interestingly, some investigators have found externalizing behaviors to be more strongly associated with sex and drug risk behaviors compared to internalizing behaviors.5,53 Additional studies that examine the impact of externalizing symptoms (e.g., aggression, attention difficulties, delinquent behavior) on risk behaviors in perinatally HIV-exposed youths are needed.
Caregiver mental health was also significantly associated with youth mental health, reflecting the extant literature in various adolescent populations.21,22 Our study was also able to go beyond the current literature and examine the impact of caregiver mental health on youth sex and drug risk outcomes. Our data suggest that the impact of caregiver mental health on youth risk behavior occurs through child mental health, rather than having a direct association on sexual or drug risk behavior. Taken together with the youth mental health findings, our data highlight the importance of caregiver mental health in influencing youth risk behavior and support efforts to integrate mental health services and risk reduction efforts.
While for the most part our indicators of family functioning -- parent-child communication and involvement -- were not significantly associated with the study outcomes, there was an associative trend between family functioning and onset of sexual behavior. In contrast to several previous studies, we did not find an association between family functioning and either child mental health or substance use. There are several possible interpretations. Caregiver mental health may be the more critical predictor of child mental health. In fact, we found that the significant bivariate association between family functioning and child mental health was no longer significant in the SEM model when the correlation of caregiver mental health and family functioning was taken into account. Alternatively, our measure of family functioning was based on caregiver self-report and may be confounded with caregiver mental health. It is also possible that other family processes not assessed in our study (e.g., parental monitoring and supervision, parent-child bonding) may have a greater impact on the onset of youth sexual and drug use risk behaviors. Finally, it is possible that a relationship between family functioning and youth risk behaviors exists, but may differ by age, gender, or other sociodemographic characteristics. Studies with larger samples and sufficient statistical power to stratify the data by age and gender, as well as other potential covariates, are needed.
There are several other limitations to this study. Although, we were able to interview 77% of participants from HIV primary care clinics who met criteria for our study, our convenience sample may not reflect all perinatally HIV-exposed adolescents. Also, although we attempted to recruit both groups from similar communities based on the demographics of pediatric HIV disease, other factors (e.g., access to services) may have altered the group effects. We did not match groups on study variables (e.g., age, gender). However, with the exception of only three caregiver demographics, we have found few differences by demographic variables across the three outcomes (i.e., youth mental health, sexual behavior, and substance use) in this cohort.11,31,35 We did not examine caregiver substance use which, given the high rate of comorbidity with mental health problems, may have confounded the indirect association between caregiver mental health and youth risk behaviors. Moreover, the data are self-report and are subject to issues of social desirability, particularly reports of sex and drug use. Finally, we have presented cross-sectional data. Given the wide age range and focus on onset of risk behaviors, the data do not allow us to make determinations of long term patterns of risk. Longitudinal studies are needed to confirm causal priority of variables and identify predictors of risk patterns. Also, studies with larger sample sizes and a comparison groups not affected by maternal HIV would help to disentangle the effects of caregiver HIV status, parental loss, and child HIV status which was difficult to do in this study given that 100% of children had HIV+ biological mothers.
The youth in our sample were relatively young, with many not yet engaging in risk behavior. As they grow older, their HIV may become a more salient factor in influencing sex and drug use risk behaviors as they grapple with sexuality, long term relationships, and child bearing desires in the context of having a communicable, stigmatized illness. Following cohorts such as CASAH participants as they transition from adolescence to young adulthood is necessary for examining pathways of risk and developing interventions to prevent risk-taking behaviors and promote health in an increasingly older cohort of pediatric HIV cases, domestically as well as internationally, where the epidemic has not subsided.54
The limitations not withstanding, this is one of the first studies to explore psychosocial correlates of PHIV+ and PHIV− youths' mental health, and drug and sex behaviors concurrently through SEM. SEM is an under utilized statistical technique in the field of pediatric psychology and a potentially important tool for helping advance theoretically based intervention research.55 Unlike multiple regression analyses, our SEM analyses help us build upon the existing literature by testing the adequacy of our model while adjusting for measurement error (i.e., every latent factor had perfect reliability).56
Our data suggest that incorporating HIV prevention interventions into ongoing mental health programs may be an effective strategy to reach PHIV+ youth and reduce HIV transmission risk. HIV prevention programming has typically not focused on child mental health and youth mental health programs have typically not focused on HIV prevention. Child mental health providers could incorporate HIV risk reduction into ongoing treatment, using therapeutic strategies to impart risk reduction skills to these youth and their families.5 Alternatively, incorporating family-based mental health strategies into more traditional sexual and drug risk reduction efforts could promote individual wellbeing of HIV+ individuals and reduce overall rates of HIV-transmission. However, it is also noteworthy that the PHIV− youths were at equal risk to the PHIV+ youths for initiating sexual and drug use behavior, including unprotected sex. These uninfected children of HIV+ mothers are from similar stressful environments, at risk for their own HIV infection, but difficult to identify and ignored in most clinical and research efforts.4 Our data suggest that efforts need to be made to identify and engage this population in family-based prevention programs.
Acknowledgments
This work was supported by three grants from the National Institute of Mental Health: 1) R01-MH069133 (PI: C.A.Mellins, Ph.D.), 2) P30 MH43520 (Center PI: A.A. Ehrhardt, Ph.D.), and 3) T32 MH19139 Behavioral Sciences Research in HIV Infection (PI: A.A. Ehrhardt, Ph.D.).
Footnotes
This article is the subject of an editorial by Dr. Alan Flischer in this issue.
Disclosure: The authors report no conflicts of interest.
References
- 1.Abrams EJ, Weedon TP, Bertolli J, et al. for the New York City Pediatric Spectrum of Disease Consortium. Aging cohort of HIV-infected children in New York City. Pediatr Infec Dis J. 2001;20:511–517. doi: 10.1097/00006454-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Hamburg BA. Life Skills Training: Preventive Interventions for Young Adolescents. Carnegie Council on Adolescent Development. Working Papers; New York: Carnegie Corporation: 1990. [Google Scholar]
- 3.Heath PA, Camarena PM. Patterns of depressed affect during early adolescence. The Journal of Early Adolescence. 2002;22:252–276. [Google Scholar]
- 4.Havens JF, Mellins CA. Psychiatric aspects of HIV/AIDS in childhood and adolescence. In: Rutter M, Taylor E, editors. Child and Adolescent Psychiatry. Fifth Edition Vol. 2008. Oxford; Oxford, UK Blackwell: pp. 945–955. [Google Scholar]
- 5.Donenberg GR, Pao M. Youths and HIV/AIDS: Psychiatry's Role in a Changing Epidemic. J Am Acad Child Adolesc Psychiatry. 2005;44:728–747. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gaughan DM, Hughes MD, Oleske JM, et al. Psychiatric hospitalizations among children and youths with human immunodeficiency virus infection. Pediatrics. 2004;113:e544–51. doi: 10.1542/peds.113.6.e544. [DOI] [PubMed] [Google Scholar]
- 7.New York City Department of Health and Mental Hygiene . Pediatric and adolescent HIV/AIDS Surveillance update. Department of Health and Mental Hygiene; New York City: 2007. [Google Scholar]
- 8.Ezeanolue EE, Wodi AP, Patel R, Dieudonne A, Oleske J. Sexual behaviors and procreational intentions of adolescents and young adults with perinatally acquired human immunodeficiency virus infection: Experience of an urban tertiary care center. J Adolesc Health. 2006;38:719–725. doi: 10.1016/j.jadohealth.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 9.McConnell M, Clark H, Zorrilla C, et al. Pregnancy in perinatally HIV-infected youth. 3rd International AIDS Society Conference on HIV Pathogenesis and Treatment; Rio de Janeiro. July 24 – 27, 2005. [Google Scholar]
- 10.Alan Guttmacher Institute . Teenage sexual and reproductive behavior in developed countries: Can more progress be made? Executive summary. Alan Guttmacher Institute; New York: 2001. [Google Scholar]
- 11.Elkington K, Bauermeister JA, Brackis-Cott E, Dolezal C, Mellins CA. Substance use and sexual risk behaviors in perinatally human immunodeficiency virus-exposed youth: The role of caregivers, peers and HIV status. J Adolesc Health. doi: 10.1016/j.jadohealth.2009.01.004. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. J Am Acad Child Adolesc Psychiatry. 2001;40:642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elkington KS, Teplin LA, Mericle AM, Welty LJ, Romero EG, Abram KM. HIV/STI Risk Behaviors in Delinquent Youth With Psychiatric Disorders: A Longitudinal Study. J Am Acad Child Adolesc Psychiatry. 2008;47:901–911. doi: 10.1097/CHI.0b013e318179962b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tolou-Shams M, Brown LK, Houck C, Lescano CM, Project Shield Study Group The Association Between Depressive Symptoms, Substance Use, And HIV Risk Among Youth With an Arrest History. Journal of the Study on Alcohol and Drugs. 2008;69:58–64. doi: 10.15288/jsad.2008.69.58. [DOI] [PubMed] [Google Scholar]
- 15.Brown LK, Danovsky MB, Lourie KJ, DiClemente RJ, Ponton LE. Adolescents with psychiatric disorders and the risk of HIV. J Am Acad Child Adolesc Psychiatry. 1007. 36:1609–1617. doi: 10.1016/S0890-8567(09)66573-4. [DOI] [PubMed] [Google Scholar]
- 16.Walter HJ, Vaughan RD, Cohall AT. Psychosocial influences on acquired immunodeficiency syndrome-risk behaviors among high school students. Pediatrics. 1991;88:846–852. [PubMed] [Google Scholar]
- 17.Havens J, Whitaker A, Feldman J, Ehrhardt A. Psychiatric morbidity in school-age children with congenital HIV-infection: A pilot study. J Dev Behav Pediatr. 1994;15:S18–S25. [PubMed] [Google Scholar]
- 18.Mellins CA, Brackis-Cott E, Dolezal C, Abrams EJ. Psychiatric disorders in youth with perinatally acquired HIV-infection. Pediatri Infect Dis J. 2006;25:432–437. doi: 10.1097/01.inf.0000217372.10385.2a. [DOI] [PubMed] [Google Scholar]
- 19.Gaughan DM, Hughes MD, Oleske JM, Malee K, Gore CA, Nachman S, Pediatric AIDS Clinical Trials Group 219C Team Psychiatric hospitalizations among children and youths with human immunodeficiency virus infection. Pediatrics. 2004;113:e544–51. doi: 10.1542/peds.113.6.e544. [DOI] [PubMed] [Google Scholar]
- 20.Pequegnat W, Szapocznik J, editors. Working With Families in the Era of HIV/AIDS. Thousand Oaks, CA: 2000. pp. 67–87. [Google Scholar]
- 21.Goodman SH, Brogan D, Lynch ME, Fielding B. Social and emotional competence in children of depressed mothers. Child Dev. 1993;64:516–531. doi: 10.1111/j.1467-8624.1993.tb02925.x. [DOI] [PubMed] [Google Scholar]
- 22.Miller L, Warner V, Wickramaratne P, Weissman M. Self-esteem and depression: Ten year follow-up of mothers and offspring. Journal of Affective Disorders. 1999;52:41–49. doi: 10.1016/s0165-0327(98)00042-1. [DOI] [PubMed] [Google Scholar]
- 23.Weissman MM, Pilowsky DJ, Wickramaratne P, et al. Remission of Maternal Depression is Associated with Reductions in Psychopathology in their Children: A Star*D-Child Report. JAMA. 2006;295:389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- 24.Beardslee W, Schlultz L, Sleman R. Level of social cognitive development, adaptive functioning and DSM-III diagnosies in adolescent offspring of parents with affective disorders: Implications of the development of the capacity for mutulality. Dev Psychol. 1987;23:807–815. [Google Scholar]
- 25.Brooks-Gunn J, Furstenberg FF. Adolescent sexual behavior. American Psychologist. 1989;44:249–253. [PubMed] [Google Scholar]
- 26.Cohen DA, Farley TA, Taylor SN, et al. When and where do youths have sex? The potential role of adult supervision. Pediatrics. 2002;110:e66. doi: 10.1542/peds.110.6.e66. [DOI] [PubMed] [Google Scholar]
- 27.McNeely CA, Shew ML, Beuhring T, et al. Mother's Influence on adolescents sexual debut. J Adolesc Health. 2002;31:256–265. doi: 10.1016/s1054-139x(02)00350-6. [DOI] [PubMed] [Google Scholar]
- 28.Amerikaner M, Monks G, Wolfe P, Thomas S. Family interaction and individual psychological health. Journal of Counseling and Development. 1995;72:614–620. [Google Scholar]
- 29.Fox GL, Inazu JK. Patterns and outcomes of mother-daughter communication about sexuality. Journal of Social Issues. 1980;36:7–29. [Google Scholar]
- 30.Kotchick BA, Dorsey S, Miller KS, Forehand R. Adolescent sexual risk-taking behavior in single-parent ethnic minority families. J Fam Psychol. 1999;13:93–102. [Google Scholar]
- 31.Mellins CA, Brackis-Cott E, Leu CS, et al. Rates and Types of Psychiatric Disorders in Perinatally Human Immunodeficiency Virus-Infected Youth and Seroreverters. J Child Psychol Psychiatry. doi: 10.1111/j.1469-7610.2009.02069.x. available on line February, 2009. http://dx.doi.org/10.1111/j.1469-7610.2009.02069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meyer-Bahlburg HFL, Ehrhardt AA, Exner TM, Gruen RS, Dugan T. Sexual Risk Behavior Assessment Schedule - Youth, Depressed Females, Baseline (SERBAS-Y-DEPR-F-1) 1995 edition [Google Scholar]
- 33.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998);280(5365):867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 34.Morrison-Beedy D, Carey M, Tu X. Accuracy of Audio Computer-Assisted Self-Interviewing (ACASI) and Self-Administered Questionnaires for the assessment of sexual behavior. AIDS and Behavior. 2006;10(5):541–552. doi: 10.1007/s10461-006-9081-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bauermeister JA, Elkington K, Brackis-Cott E, Dolezal C, Mellins C. Sexual behavior and perceived peer norms: Comparing perinatally infected and affected youth. [Accessed January 20, 2009];Journal of Youth and Adolescence. doi: 10.1007/s10964-008-9315-6. available on line August 5, 2008. http://dx.doi.org/10.1007/s10964-008-9315-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shaffer D, Fisher P, Lucas C, Dulcan M, Schwab-Stone M. NIMH Diagnostic Interview Schedule for Children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 37.American Psychological Association . Diagnostic and Statistical Manual of Mental Disorders. 4th Ed. American Psychiatric Assocation; Washington DC: 1994. [Google Scholar]
- 38.Kovacs M. Rating Scale to assess depression in school-age children. Acta Paedopsychiatr. 1981;46:305–315. [PubMed] [Google Scholar]
- 39.Spielberger CD. State-Trait Anxiety Inventory. Consulting Psychologist Press, Inc; California: 1987. [Google Scholar]
- 40.Beck AT, Beck RW. Screening depressed patients in family practice. A rapid technique. Post Grad Med. 1972;52:81–85. doi: 10.1080/00325481.1972.11713319. [DOI] [PubMed] [Google Scholar]
- 41.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 42.Gerard AB. Parent-Child Relationship Inventory (PCRI) Western Psychological Services; Los Angeles: 1994. [Google Scholar]
- 43.Bentler PM. EQS 6.1 for Windows. Version 6.1 Multivariate Software, Inc; Encino, CA: 2008. [Google Scholar]
- 44.Klem L. Structural Equation Modeling. In: Grimm LG, Yarnold PR, editors. Reading and understanding more multivariate statistics. American Psychological Association; Washington, DC: 2000. pp. 227–260. [Google Scholar]
- 45.Bedeian AG, Day DV, Kelloway EK. Correcting for measurement error attenuation in structural equation models: Some important reminders. Educational and Psychological Measurement. 1997;57:785–799. [Google Scholar]
- 46.Raykov T, Tomer A, Nesselroade JR. Reporting structural equation modeling results in Psychology and Aging: Some proposed guidelines. Psychol Aging. 1991;6:499–503. doi: 10.1037//0882-7974.6.4.499. [DOI] [PubMed] [Google Scholar]
- 47.Boomsma A. Reporting analyses of covariance structures. Structural Equation Modeling. 2000;7:461–483. [Google Scholar]
- 48.Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 49.Kline RB. How to fool yourself with SEM. In: Kline RB, editor. Principles and practice of structural equation modeling. The Guildford Press; New York: 1998. pp. 273–281. [Google Scholar]
- 50.Brown LK, Tolou-Shams M, Lescano C, et al. Project SHIELD Study Group Depressive symptoms as a predictor of sexual risk among African American adolescents and young adults. J Adolesc Health. 2006;39:444.e1–444.e8. doi: 10.1016/j.jadohealth.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 51.Houck C, Lescano CM, Brown L, et al. “Islands of Risk”: Subgroups of adolescents at risk for HIV. J Pediatr Psychol. 2006;31:619–6290. doi: 10.1093/jpepsy/jsj067. [DOI] [PubMed] [Google Scholar]
- 52.Guilamo-Ramos V, Litardo HA, Jaccard J. Prevention programs for reducing adolescent problem behaviors: Implications of the co-occurrence of problem behaviors in adolescence. J of Adolescent Health. 2005;36:82–86. doi: 10.1016/j.jadohealth.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 53.Donenberg GR, Wilson HW, Emerson E, Bryant FB. Holding the line with a watchful eye: The impact of perceived parental monitoring on risky sexual behavior among adolescents in psychiatric care. AIDS Educ Prev. 2002;14:138–157. doi: 10.1521/aeap.14.2.138.23899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.UNAIDS [accessed January 20, 2008];AIDS Epidemic Update December, 2008. www.UNAIDS.org.
- 55.Nelson T, Brandon S, Aylward MA, Steele RG. Structural equation modeling in pediatric psychology: Overview and review of applications. J Pediatr Psychol. 2008;33:679–687. doi: 10.1093/jpepsy/jsm107. [DOI] [PubMed] [Google Scholar]
- 56.Bryan A, Schmiege SJ. Broaddus MR Mediational analysis in HIV/AIDS research: Estimating multivariate path analytic models in a structural equation modeling framework. AIDS & Behavior. 2007;11:365–383. doi: 10.1007/s10461-006-9150-2. [DOI] [PubMed] [Google Scholar]