Abstract
Venezuelan equine encephalitis virus (VEEV) is a reemerging pathogen and a continuing threat to humans and equines in the Americas. Identification of the genetic determinants that enable epizootic VEEV strains to arise and exploit equines as amplification hosts to cause widespread human disease is pivotal to understanding VEE emergence. The sensitivity to murine alpha/beta interferon-mediated antiviral activity was previously correlated to the epizootic phenotype of several VEEV strains. Infectious cDNA clones were generated from an epizootic subtype IC VEEV strain (SH3) isolated during the 1992 Venezuelan outbreak and a closely related enzootic, sympatric subtype ID strain (ZPC738). These VEEV strains had low-cell-culture-passage histories and differed by only 12 amino acids in the nonstructural and structural proteins. Rescued viruses showed similar growth kinetics to their parent viruses in several cell lines, and murine infections resulted in comparable viremia and disease. Unlike what was found in other studies of epizootic and enzootic VEEV strains, the sensitivities to murine alpha/beta interferon did not differ appreciably between these epizootic versus enzootic strains, calling into question the reliability of interferon sensitivity as a marker of epizootic potential.
Venezuelan equine encephalitis virus (VEEV) is a member of the family Togaviridae, genus Alphavirus. The virus is enveloped and includes a nonsegmented, positive-sense RNA genome of ca. 11.4 kb. The 5′ two-thirds of the genome encodes four nonstructural proteins (nsP1 to nsP4) that are involved in viral genome replication and polyprotein processing. After virus entry into the cytoplasm of cells, a nonstructural polyprotein is translated and utilized in the production of full-length, negative-sense RNA. The negative-sense RNA is used as a template for the generation of genomic RNA, as well as a subgenomic mRNA (26S), which is identical to the 3′ one-third of the genome. The subgenomic RNA is translated directly into a structural polyprotein that is proteolytically cleaved into the capsid and E2/E1 envelope glycoproteins (24). The alphavirus virion contains an icosahedral nucleocapsid that consists of 240 copies of the capsid protein and the genomic RNA, surrounded by a lipid envelope derived from the plasma membrane of infected cells, into which glycoprotein E1/E2 heterodimers are embedded (17, 24).
VEE has been an important human and equine disease for nearly a century, and recent epidemics and equine epizootics (16, 31) indicate that VEEV still poses a serious public and veterinary health threat. Furthermore, VEEV is a highly developed biological weapon and remains a biological warfare and terrorism threat (9). VEE complex alphaviruses are classified into six distinct antigenic subtypes (4, 27). Historically, only viruses in subtype I (varieties AB and C) were associated with major epidemics and equine epizootics, during which horses have always served as the principal amplification host. In contrast, viruses classified in the remaining subtypes and varieties (II to VI and ID to IF) of the VEE complex are considered enzootic. These viruses are usually not associated with equine disease, and they circulate continually in sylvatic cycles among rodent reservoir hosts and enzootic mosquito vectors (27, 30). Both antigenic (32) and genetic (13, 20) similarities support the hypothesis of periodic evolution of epizootic, subtype IAB and IC variants from enzootic subtype ID progenitor viruses. Phylogenetic studies performed in our laboratory indicated that the IC epizootic viruses have emerged from an ID progenitor independently on at least two occasions (18). The first emergence occurred in 1962 in northern Colombia and spread into neighboring Venezuela to generate a major epidemic affecting tens of thousands of humans and equines (3). Viruses with nearly complete conservation in their nucleotide sequences reemerged in 1995 to cause another major outbreak in the same regions of Venezuela and Colombia (2, 31). The remaining subtype IC genotype emerged in 1992 in western Venezuela to cause a smaller epidemic and equine epizootic. Phylogenetic studies with complete genomic sequences suggested that the etiologic agents isolated during this outbreak evolved recently from enzootic, subtype ID strains that circulate in the same region of western Venezuela (28). Experimental infections of equines demonstrated that these closely related enzootic and epizootic strains have typical phenotypes; the enzootic strains produced little or no viremia and little disease, whereas the epizootic IC strains generated high-titer viremia and encephalitis (29).
Previous studies indicated that a resistance to alpha/beta interferon (IFN-α/β) could be responsible for the epizootic phenotypes of several different VEEV strains (10, 25). Higher resistance to murine IFN-α/β in vitro was observed for some epizootic strains compared to enzootic or artificially attenuated strains (25). These observations led to the hypothesis that the ability of the epizootic strains to resist innate equine immunity, IFN-α/β in particular, leads to more efficient virus replication and higher viremia in horses, facilitating epizootic transmission. Jahrling et al. (10) showed a direct correlation between sensitivity to IFN-α/β and the virulence of VEEV strains by using a hamster model. Unfortunately, this model does not faithfully predict equine virulence; most subtype I viruses, including both subtypes IC (epizootic) and ID (enzootic), are uniformly lethal for hamsters. Nevertheless, the present study showed that the level of IFN-α/β production in different tissues of infected hamsters is directly proportional to the level of virus replication (10). This suggested that epizootic VEEV strains do not suppress IFN-α/β production to a greater extent than enzootic strains. A difference in VEEV clearance by reticuloendothelial system in hamsters, in which enzootic viruses have shown faster clearance than epizootic viruses after intravenous injection, was also observed and discussed (11).
In the present study we investigated the role of IFN-α/β sensitivity and resistance in the 1992 VEE emergence in western Venezuela. Two genetically defined viruses, infectious cDNA clones were generated from closely related epizootic (IC) and enzootic (ID) parent strains with low-passage history, and their replication patterns and IFN-α/β sensitivity and resistance were compared in vitro, as well as their virulence in the laboratory rodents (mice). Our results indicate that changes in murine IFN-α/β sensitivity did not accompany the 1992 VEE emergence, suggesting that murine IFN-α/β sensitivity is not a reliable marker of epizootic potential.
MATERIALS AND METHODS
VEE virus strains.
The enzootic strain ZPC738 (subtype ID), epizootic strain SH3 (subtype IC), epizootic strain 3908 (subtype IC), and vaccine strain TC-83 of VEEV were used in this study. ZPC738 was isolated from the heart of a sentinel hamster exposed in a tropical lowland forest of Zulia State, Venezuela, in 1997 (15, 28). The strain was characterized antigenically as a subtype ID with monoclonal antibodies as described previously (21). This strain was passaged once in BHK-21 cells to generate RNA for the present study. Strain SH3 was isolated during an equine epizootic and epidemic that occurred in western Venezuela from 1992 and 1993 (20). It was passaged once in Vero76 cells and once in BHK-21 cells to generate RNA. Strain 3908 was isolated from human in Zulia State, Venezuela, on 16 September 1995 during a major epidemic (31). This strain was passaged once in C6/36 mosquito cells. The live-attenuated TC-83 vaccine strain was obtained from the World Arbovirus Reference Center at the University of Texas Medical Branch.
Cell cultures.
BHK-21 (baby hamster kidney), Vero76 (African green monkey kidney), and L929 (mouse fibroblast) cells were obtained from the American Type Tissue Culture Collection. All cell lines were maintained at 37°C under 5% CO2 in Eagles minimal essential medium (MEM) supplemented with 5% fetal bovine serum (FBS) and gentamicin (10 μg/ml). Cells with identical passage numbers were used for each comparison among virus strains. The same lot of FBS was used in all of the experiments described here.
RNA isolation.
For viral RNA isolation, Vero cells were seeded into T-150 flasks and allowed to grow to ca. 95% confluence. Then, cells were infected with ZPC738 and SH3 VEEV strains at a multiplicity of infection (MOI) of 5 PFU/cell. At 15 h postinfection, the cell monolayers were treated with Trizol LS reagent (Gibco-BRL, Bethesda, Md.), followed by chloroform extraction and ethanol precipitation of the aqueous phase. Nucleic acids were dissolved in water and stored at −80°C with 40 U of RNase inhibitor (Promega, Madison, Wis.). At least 2 μg of total nucleic acids was used for each reverse transcription-PCR (RT-PCR).
RT-PCR.
The genomes of the ZPC738 and SH3 VEEV strains were divided into six overlapping fragments spanning appropriate unique restriction sites (Fig. 1). Viral cDNAs were synthesized from RNA by using reverse transcriptase (SuperScript II; Invitrogen, Carlsbad, Calif.). Primers used for amplification are listed in Table 1. PCR fragments were amplified by using the high-fidelity Pfu Turbo polymerase (Stratagene, La Jolla, Calif.). The following conditions were used for the PCR: 30 cycles of denaturation at 95°C for 30 s, primer annealing for 30 s at temperatures from 59 to 63°C, followed by extension at 72°C for 2 min per 1 kb amplified.
FIG. 1.
Representation of the VEEV genome showing the positions of the RT-PCR amplicons used to construct the pM1-738 and pM1-SH3 infectious cDNA clones.
TABLE 1.
Primers utilized for VEE virus genome amplification
| Primera | Sequence (5′-3′)b | Annealing temp (°C) |
|---|---|---|
| F1 | ccacTCTAGAgatttaggtgacactatagatgggcggcgcatgagagaagcccacaccaattacc | 58 |
| R1 | ccacGCGGCCGCttgtagcatcaagtcaacatcggcttcca | 58 |
| F2 | ccacTCTAGActctcattactgccgaggacgtacaagaagctaag | 57 |
| R2 | ccacGCGGCCGCggaacagtgggtgcagaaaatagaccggaatc | 57 |
| F3 | ccacTCTAGAgtgttgggccaaggccttggtgccggtactg | 57 |
| R3 | ccacGCGGCCGCgaaaaagcacgattcacactagatgaatacaaag | 57 |
| F4 | ccacTCTAGAcctgctaacagaagcagataccagtccaggagg | 59 |
| R4 | ccacGCGGCCGCtcggcccgcatgttctgtggcacatctgcatac | 59 |
| F5 | ccacTCTAGActatgcttgcgtggtcggagggaagttattcagg | 58 |
| R5 | ccacGCGGCCGCcgcctgcactgaggctgtgtgcgctttgtatgc | 58 |
| F6 | ccacTCTAGAgtttacccgttcatgtggggaggcgcatattgc | 61 |
| R6 | ccacGCGGCCGCtttttttttttttttttttttttttgaaatattaaaaa | 61 |
F, forward or positive (genomic) sense; R, reverse or negative sense.
Capital letters indicate restriction sites used for cloning.
Cloning and sequencing of PCR fragments.
RT-PCR fragments of predicted size were cloned into the pCR-XL-TOPO vector (Invitrogen) according to the manufacturer's protocol. Sequencing was performed by using an Applied Biosystems (Foster City, Calif.) Prism 377 sequencer by using the BigDye terminator cycle sequencing kit according to the manufacturer's protocol.
Plasmid constructs.
Standard recombinant DNA techniques (23) were used for all plasmid constructions with the TOP10 strain of Escherichia coli (Invitrogen). Detailed maps and sequences are available upon request. To clone viral cDNA into the final constructions, the special low-copy-number, ampicillin-resistant vector pM1, with convenient unique restriction sites, was created. Appropriate fragments were sequentially cloned into the pM1 plasmid. Each cloning step was verified by restriction analysis, followed by sequencing of junctions. Final constructions were named pM1-738 (infectious cDNA clone of enzootic strain ZPC738) and pM1-SH3 (infectious cDNA clone of epizootic strain SH3).
RNA transcription.
Both cDNA clones were purified by using the Qiagen MiniPrep kit. Prior to transcription, DNAs were linearized with NotI (New England BioLabs, Beverly, Mass.). RNAs were transcribed in the presence of m7G(5′)ppp(5′)G RNA cap structure analog (New England BioLabs) by using SP6 RNA polymerase (Invitrogen). The yield and integrity of the RNA transcripts were monitored by agarose gel electrophoresis. Transcribed RNAs were maintained at −80°C.
Transfection.
A total of 95% confluent BHK-21 cell monolayer was washed twice in phosphate-buffered saline (PBS), treated with trypsin, resuspended in 25 ml of ice-cold PBS, counted, and centrifuged. Each pellet was washed again in 25 ml of ice-cold PBS, and cells were resuspended in PBS at the concentration of 2 × 107 cells/ml. A portion (400 μl) of the cell suspension was mixed with 4 μg of in vitro synthesized RNA in a 0.2-cm cuvette, and electroporation was performed. After electroporation the cells were incubated for 10 min at room temperature, transferred into T-150 flasks with MEM supplemented with 5% FBS and gentamicin (10 μg/ml), and incubated at 37°C under 5% CO2. Viruses were harvested for 24 h after transfection.
Infectious center assays.
Immediately after electroporation as described above, appropriate aliquots of cells were diluted 10, 100, 1,000, and 10,000 times in MEM and placed immediately into cell monolayers prepared in advance. After 1 h of incubation at 37°C, the cells were covered with MEM containing 1.0% Noble agar (Sigma) and incubated 48 h (until plaques appeared).
Plaque assay.
Vero cells were seeded into six-well tissue culture plates and allowed to grow to 90% confluence. Viruses were diluted in PBS supplemented with 1% FBS, and appropriate dilutions were adsorbed to the cell monolayers for 1 h at 37°C. Then, 2 ml of MEM with 1.0% Noble agar was added to each well, and the cells were incubated at 37°C for 48 h. Agar plugs were removed, and the cells were stained with a 20% methanol-0.25% crystal violet solution.
Virus replication curves.
Vero 76 and L929 cells were used to measure viral replication rates. Cells were seeded into six-well tissue culture plates and infected at an MOI of 0.1 or 1.0 PFU/cell. Plates were incubated at 37°C for 1 h. After three washes with PBS, 2 ml of MEM was added, followed by incubation at 37°C. Then, at 8, 24, and 48 h postinfection, samples of medium were harvested, and plaque assays were performed as described above.
In vivo characterization of viruses.
Adult NIH Swiss mice (6 to 8 weeks old, female) from Harlan (Indianapolis, Ind.) were maintained on standard lab chow and water ad libitum. Animals were held for 1 week in the BSL-3 facility for acclimatization prior to experimental infections. Mice were inoculated subcutaneously with 1,000 PFU of virus in 100 μl of PBS in the left medial thigh. Inocula were retitered by plaque assay immediately after the challenge. Mice were observed twice daily for clinical illness (ruffled, depressed, anorexia, and/or paralysis) and death. Blood was collected via cardiac puncture after inoculation of the animals intraperitoneally with pentobarbital (10 mg/mouse). Mice used for the survival study were not exposed to any narcotics.
IFN sensitivity assay.
Monolayers of L929 mouse fibroblast or Vero76 cells (National Institutes of Health [NIH]; lot no. 82017, catalog no. 20161) in 12-well plates were primed for 24 h with 10, 25, 50, and 100 U of mouse or human IFN-α/β (LEE Biomolecular Research Laboratories, San Diego, Calif.)/ml. After priming, 105 PFU of each virus was added to each well (MOI = 1) in triplicate, and the virus was allowed to adsorb for 1 h at 37°C under 5% CO2. After three washes with PBS, 2 ml of MEM was added to each well. Controls included unprimed, washed L929 cells infected with each virus. A 100-μl volume of medium was taken at 8, 24, and 48 h after infection. Plaque assays were performed to determine the titer of virus produced at selected IFN concentrations.
IFN CPE protection assay.
The methods used initially for quantifying IFN sensitivity with cytopathic effect (CPE) as an endpoint were essentially those described by Spotts et al. (25). Monolayers of L929 mouse fibroblast cells grown in 96-well plates were pretreated in quadruplicate with 10, 25, 50, and 100 U of murine IFN-α/β from the same source as described above for 24 h. Upon treatment with IFN, cells were washed three times with PBS and infected with 1,000 PFU of virus per well. Treated infected, treated uninfected, and untreated infected cells were observed for CPE for 4 days postinfection. The concentration of IFN-α/β that protected >50% of cells was estimated at 4 days postinfection.
RESULTS
Construction of pM1-738 and pM1-SH3 infectious clones.
Six overlapping fragments spanning the complete viral genomes of both VEEV strains were generated by RT-PCR (Fig. 1). The fragments were flanked by XbaI restriction sites at the 5′ ends and NotI restriction sites at the 3′ ends. The 5′ end of the first fragments from each virus also had an SP6 promoter immediately upstream of the viral sequence. Each fragment was cloned into the high-copy-number kanamycin-resistant pCR-XL-TOPO vector, and three independent clones for each fragment were sequenced and analyzed. Compared to the previously reported sequences (28), one synonymous nucleotide difference was found in the third fragment of strain ZPC738 in genome position 5076, and three synonymous differences were found in genome positions 2384, 7579, and 8653 in the fragments of the SH3 clones.
To create the full-length infectious cDNA clones pM1-738 and pM1-SH3, the appropriate fragments were cloned sequentially into the low-copy-number, ampicillin-resistant pM1 vector with unique restriction sites XbaI and NotI. After in vitro transcription, the efficiency of virus production of the newly created infectious cDNA clones pM1-738 and pM1-SH3 was compared to a well-characterized Sindbis virus infectious cDNA clone Toto1101 (19). The in vitro-synthesized RNAs of the pM1-738 and pM1-SH3 infectious cDNA clones were electroporated into BHK-21 cells. Rescued viruses were harvested 24 h later and used for all subsequent experiments. By that time, all cells exhibited profound CPE. The infectious center assay results indicated the absence of lethal mutations in created infectious clones; in vitro-synthesized RNAs from both VEEV infectious cDNA clones had an infectivity similar to that of Toto1101 (data not shown), indicating that pM1-738 and pM1-SH3 clones were not attenuated in vitro.
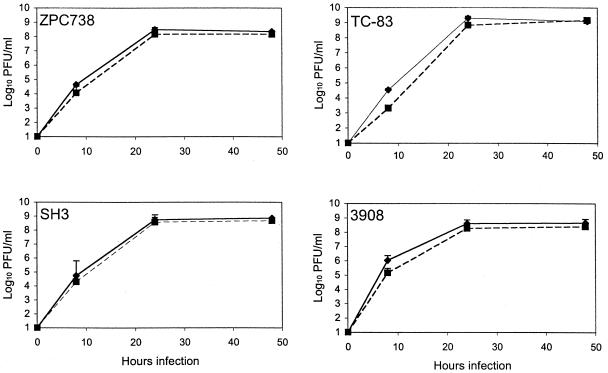
Virus replication kinetics.
In initial experiments, we compared the basic replication characteristics of the rescued viruses from the infectious cDNA clones pM1-738 and pM1-SH3, respectively, with their appropriate parent viruses. All viruses replicated efficiently in Vero76 cells infected at an MOI of 0.1 (data not shown). Both pairs of viruses reached titers of 3 to 8 × 105 PFU/ml 8 h postinfection, with nearly identical titers of rescued versus parent viruses. Titers measured 24 h postinfection were 0.9 × 108 to 3 × 108 PFU/ml, and by 48 h postinfection reached 3 × 108 to 8 × 108 PFU/ml. An MOI of 1 produced similar results (data not shown), with nearly identical titers among pairs of the strains (rescued and original parent virus) at every time point. However, at both MOIs, the SH3 and 3908 epizootic strains replicated to slightly but consistently higher titers than the ZPC738 enzootic strain (values for 3908 are not shown).
We also analyzed the replication of all four viruses in mouse fibroblast L929 cells. All viruses replicated efficiently at an MOI of 0.1 (data not shown) and reached titers of 8 log10 PFU/ml by 48 h postinfection. However, we noticed a difference between the enzootic ZPC738 (subtype ID) and epizootic SH3 strain (subtype IC) in final titers in the media. Both ZPC738 viruses, the original parent and rescued infectious clone virus, reached titers of 0.8 104 PFU/ml to 1 × 104 PFU/ml by 8 h postinfection. At the same time both SH3 viruses showed titers of 0.8 × 105 to 1.5 × 105 PFU/ml, i.e., 10-fold more than the ZPC738 viruses. This difference increased to ∼100-fold (3 × 106 PFU/ml for strain ZPC738 strain versus 3 × 108 PFU/ml for SH3) 24 h postinfection and disappeared by 48 h postinfection; at this point all four viruses reached titers of 8 log10 PFU/ml. Similar results were obtained at an MOI of 1 (data not shown); at 8 and 24 h postinfection, the ZPC738 viruses produced lower titers of virus than strain SH3, but the differences were less pronounced than those observed at an MOI of 0.1. All four viruses had titers >108 PFU/ml at 48 h postinfection. Titers of viruses rescued from infectious clones and their parents were nearly identical. These differences in replication were not observed in Vero cells at any MOI tested.
Comparative plaque size analysis.
Because plaque size has been shown previously to correlate inversely with the epizootic phenotype (14, 28), plaque sizes for the rescued infectious clone viruses pM1-738 and pM1-SH3 and their corresponding parent viruses were determined. A total of 20 plaques were measured for each virus. For irregularly shaped plaques, two measurements were made at right angles to each other and averaged. The plaque sizes of the rescued infectious clone viruses and appropriate original parent viruses were almost identical. The mean plaque diameters of both viruses of the enzootic ZPC738 strain were 3.9 to 4.0 mm and correspond to a plaque size of typical enzootic VEEV strains (3 to 4 mm). The mean plaque diameters of both viruses of the epizootic SH3 strain were 1.7 mm and correspond to plaque sizes of typical of epizootic strains (1 to 2 mm) (14, 28). There was no significant difference between either rescued infectious clone virus and its parent strain (Student t test, P ≥ 0.7).
Experimental infections of mice.
To compare the virulence of viruses generated from the newly created infectious cDNA clones with that of the corresponding parent viruses, adult NIH Swiss mice (6 to 8 weeks old) were infected subcutaneously in the medial thigh with 1,000 PFU of each virus strain. All viruses used in our experiments produced a high-titer viremia that was detectable for at least 3 days (Fig. 2). All parent viruses and rescued infectious clone viruses were able to generate high levels of viremia within 24 h, and the titers were nearly identical. However, the epizootic SH3 viruses consistently produced higher viremia than the enzootic ZPC738 strains at 24 and 48 h. All infected mice were hunched and less active by day 3 or 4 postinfection with either the pM1-738 or pM1-SH3 rescued viruses or with the parent viruses. Between days 4 and 7, the mice developed anorexia, lethargy, and hind limb paralysis, and the central nervous system signs always progressed to stupor and finally to coma. Except for one animal infected with the SH3 parent virus (death on day 8 postinfection), all animals died by day 7 (mean survival time of 7 days). The cause of death was confirmed by isolating VEEV from the brains of the dead animals. These results agreed with previous studies of VEEV pathogenesis with these and other strains (5, 29).
FIG. 2.
Viremia titers of infectious clone-derived viruses and their parent strains in the sera of NIH Swiss mice after subcutaneous inoculation of 1,000 PFU. Bars represent standard deviations of the means from three replicates.
IFN protection assay.
We tested the potential of murine IFN-α/β to protect L929 cells from death upon infection with the different VEEV strains. Different concentrations of murine IFN-α/β (10, 25, 50, and 100 U/ml) were examined for their ability to protect >50% of VEEV-infected L929 cells from CPE. After pretreatment with 100 U/well, all cells infected with the TC-83 vaccine strain were protected, and >50% of cells infected with three natural VEEV strains (enzootic ID ZPC738 and epizootic IC SH3 and 3908) were also protected. This outcome changed at 50 U of IFN-α/β/well, whereas only cells infected with TC-83 were completely protected and cells infected with rescued infectious clone viruses (pM1-SH3 and pM1-738) and 3908 virus developed complete CPE 4 days postinfection. However, 25 U of IFN-α/β/well was still sufficient to protect 50% of cells infected with TC-83, whereas the pM1-SH3, pM1-738, and 3908 strains were completely lethal. The 3908 strain always produced the fastest CPE in untreated cells, and almost no unaffected cells were detected at 24 h postinfection regardless of the MOI used (data not shown).
IFN sensitivity assay.
Because of the different CPE phenotypes exhibited by the vaccine, enzootic and epizootic strains, we compared more directly their IFN sensitivity by examining the replication kinetics in murine L929 cells after they were primed with different concentrations of IFN-α/β (100, 50, 25, and 10 U/ml). Control, untreated, infected cells were included to estimate the ability of IFN-α/β to suppress virus replication. The results for pretreatment with 100 U of IFN-α/β/ml are shown in Fig. 3. Replication of all VEEV strains was consistently suppressed in comparison to control, unprimed, infected cells. With 100 U of IFN-α/β/ml, the viruses were not able to establish prolonged replication with efficient virus production, as reflected by the decrease of the virus titers over a period of 2 days for most strains. In all cases, the fluctuation of virus titers occurred within the limits of approximate 1 log10. However, at 8 h postinfection after pretreatment with 100 U of IFN/ml, the 3908 epizootic strain showed at least 3-log10-higher virus titers versus the TC-83 vaccine strain and a 1.5-log10-higher titer versus the rescued infectious clone viruses pM1-738 and pM1-SH3 (ca. 5 × 104, 1 × 101, and 1 × 103 PFU/ml higher, respectively). With 50 U of IFN-α/β/ml, replication was again suppressed compared to the unprimed, infected control cells. The virus replication curves were highly similar to those in the experiment with 100 U of IFN-α/β/ml (Fig. 3), but the titers of all viruses except for epizootic strain 3908 were slightly higher. In contrast to the experiment with 100 U/ml, the titer of TC-83 virus increased approximately 1.5 log10 from 24 to 48 h postinfection (4 × 102 and 1 × 104 PFU/ml, respectively), and at 48 h postinfection the titers for TC-83 reached 104 PFU/ml, a level almost equal to the titers of the other viruses.
FIG. 3.
Replication of infectious clone-derived VEEV strains after mock pretreatment (control) or pretreatment of mouse L929 cells with 10, 25, 50, or 100 U of IFN-α/β/ml. Cells were infected with 1,000 PFU of VEEV strains at 24 h after IFN treatment. Bars represent the standard deviations of the means from three replicates.
Again, very similar results were obtained with all four virus strains with 25 U of IFN-α/β/ml for L929 cell priming (Fig. 3). One marked difference was observed at 24 h postinfection; the titer of TC-83 was approximately 1 log10 higher after treatment with 25 U/ml than with 50 U/ml (3 × 103 and 4 × 102 PFU/ml, respectively). However, the experiment with 10 U of IFN-α/β/ml yielded quite different results; the replication curves for all four viruses were highly similar to one another and to the untreated control curves (Fig. 3), indicating that 24 h of cell priming with 10 U of IFN-α/β/ml had little or no effect on VEEV replication.
With the exception of the attenuated vaccine strain TC-83, which was consistently more sensitive to murine IFN-α/β than the wild-type viruses, there was consistent difference in the levels of suppression of virus replication among VEEV strains. When the titers were compared after pretreatment with 25 to 100 U of IFN-α/β/ml (10 U/ml yielded no detectable suppression of VEEV replication), there was no reproducible difference in sensitivity among enzootic strain ZPC738 versus epizootic strains SH3 and 3908 when measured as the log reduction in virus titer (Table 2). In contrast, the TC-83 vaccine strain consistently showed 1 to 2 logs more IFN-induced reduction in titer compared to the wild-type strain.
TABLE 2.
Mean levels of suppression of virus replication in L929 cells pretreated with IFN-α/β
| Virus strain | Pretreatment with IFN-α/βa (U/ml) | Log10 reduction in virus titer compared to untreated controls atb:
|
||
|---|---|---|---|---|
| 8 h | 24 h | 48 h | ||
| ZPC738 | 25 | 2.0 | 4.3 | 3.9 |
| SH3 | 2.6 | 3.6 | 3.0 | |
| 3908 | 1.2 | 3.4 | 3.6 | |
| TC-83 | 3.4 | 6.2 | 4.5 | |
| ZPC738 | 50 | 2.0 | 4.8 | 4.2 |
| SH3 | 2.4 | 4.1 | 3.2 | |
| 3908 | 2.9 | 3.2 | 3.8 | |
| TC-83 | 3.8 | 6.2 | 6.3 | |
| ZPC738 | 100 | 2.1 | 5.4 | 4.4 |
| SH3 | 2.4 | 5.2 | 3.6 | |
| 3908 | 1.3 | 3.9 | 4.3 | |
| TC-83 | 4.3 | 6.2 | 6.3 | |
That is, pretreatment 24 h prior to infection.
Time postinfection with 1,000 PFU of virus.
To rule out any complicating effects of autocrine IFN in the mouse L929 cultures and to test the effect of IFN-α/β pretreatment of another species cell line, we used Vero76 cells, which are unable to produce IFN (6). Cells were primed with 100 U of human IFN-α/β per ml for 24 h and then infected at an MOI of 1.0 with strains ZPC838, SH3, and 3908, rescued from infectious cDNA clones, and the TC-83 vaccine strain. Little or no detectable virus remained in the medium after the inoculum was washed away, indicating that residual virus did not complicate the results (Fig. 4). All virus strains showed an approximately 0.5- to 1.0-log reduction in virus titers at 8 and 24 h postinfection, with differences showing a reduction by 48 h. These results indicated that all VEEV strains tested had a similar sensitivity to human IFN.
FIG. 4.
Replication of infectious clone-derived VEEV strains (except for strain TC-83) after mock pretreatment (control) or pretreatment of Vero76 cells with 100 U of IFN-α/β/ml. Cells were infected with 1,000 PFU of VEEV strains at 24 h after IFN treatment. The bars represent the standard deviations of the means from three replicates.
DISCUSSION
Potential determinants of the epizootic phenotype.
The molecular determinants that regulate the epizootic potential of different VEEV strains, resulting in differential abilities to produce high-level equine viremia necessary for efficient amplification, remain enigmatic. Phylogenetic studies indicate that epizootic IAB and IC viruses evolved or emerged from enzootic progenitors at least three times and that these emergence events have been associated with only one of six major ID enzootic lineages, which circulates in Colombia, Venezuela, and northern Peru (18, 22). The emergence events (evolution of epizootic strains from enzootic progenitors) were associated with changes in the E2 glycoprotein that resulted in the increase in the positive charge of the virion surface (1). Two amino acid substitutions in the E2 glycoprotein—one in the capsid protein and four in the nonstructural region—have been associated with the emergence of the epizootic IC strain implicated in the 1992 and 1993 Venezuelan outbreak (28). To date, the only consistent pattern of amino acid substitutions associated with VEE emergence is positive charge E2 substitutions, including position 213, which is involved in all three epizootic IAB/C lineages (1).
VEEV strain SH3 was isolated from a human patient with severe headache and fever on 6 January 1993 during the Venezuelan outbreak. This epizootic occurred after a 19-year hiatus and ended speculation that IAB/C VEEV had become extinct. Sequencing of the SH3 genome and comparison to that of its equine-avirulent close relative, strain ZPC738 (subtype ID) from the same region of western Venezuela, revealed 77 nucleotide differences resulting in only 12 amino acid differences. This information, coupled with the low-passage history of both viruses, makes these strains ideal candidates for a unique model system investigating natural virulence determinants of VEE emergence (28, 29).
Replication kinetics of the infectious clones in vitro and in vivo.
The pM1-738 and pM1-SH3 infectious cDNA clones we produced are fully functional and have an infectivity similar to that of the Sindbis virus infectious cDNA clone Toto1101 (19). Viruses rescued from these clones also have replication kinetics comparable to those of the original parent viruses in Vero76 and L929 cells and in mice. The average plaque sizes, markers that correlate with the epidemiological phenotype of the pM1-SH3 and pM1-738 infectious cDNA clones, were statistically indistinguishable from those of their respective parent viruses, as well as values reported for other epizootic and enzootic viruses. The average plaque size of the enzootic phenotype of the infectious cDNA clone was also statistically indistinguishable from that of its original parent virus ZPC738, as well as values reported for other enzootic viruses (14, 28). However, both epizootic strains initiated replication faster in L929 cells at low MOI than did the enzootic or vaccine strains. These results were reproducible, but not at the higher MOI (1 PFU/cell) in L929 cells or in Vero76 cells at any MOI tested. A possible explanation is that the levels of endogenous, virus-induced IFN in the L929 cells differ after infection with the viruses tested. In this case, induction of IFN-α/β, rather than resistance, may be important. This hypothesis is currently under investigation in our laboratory. It is also possible that epizootic strains replicate faster at the single-cell level, which might explain the ability of some epizootic strains to kill cells faster (within 24 h) while producing the lower final virus titers in the cell culture at 48 h postinfection. TC-83 is an attenuated vaccine strain and a prototype of IFN-α/β sensitivity. However, this strain produces slowly developing CPE in L929 cells and yet the highest final virus titers at 48 h. This suggests that attenuation (in vivo) of VEEV by cell culture adaptation can improve its replication in vitro. This is always important to consider when in vitro markers of virulence are being investigated, especially when new virus isolates have to be compared to cell culture-adapted laboratory strains. It is also important to emphasize that the final virus titers derived in the cell culture might be misleading regarding the virulence of the isolates tested. Fast-replicating VEEV strains are able to kill cells much faster, and yet the difference in replication kinetics might be visible only at early time points.
Infection of adult female NIH Swiss mice resulted in comparable viremia levels in serum and in death 6 to 8 days postinfection for both original parents and corresponding rescued infectious clone viruses. These results confirm that the pM1-738 and pM1-SH3 infectious cDNA clones have indistinguishable characteristics in comparison with their original parental viruses, in vitro as well as in vivo.
Resistance to IFN-α/β.
Previous studies have indicated that IFN resistance might be a crucial factor in VEE emergence (10, 25). The epizootic VEEV transmission cycle is undoubtedly associated with strong selective pressure on these viruses to resist the innate immunity in the equine host and produce the high viremia titers necessary for the infection of epizootic mosquito vectors, many of which are only marginally susceptible to oral infection (30). Jahrling et al. observed a correlation between IFN resistance and the virulence of VEEV strains (10). The attenuation of the TC-83 (vaccine) strain of VEEV was also associated with a decrease in IFN-α/β resistance (12, 25), and mutations responsible for VEEV attenuation, described in several different studies, are almost always associated with a decrease in IFN-α/β resistance (7, 8).
Spotts et al. compared the sensitivity of different VEEV strains to IFN-α/β by testing for CPE inhibition in pretreated mouse cell cultures (25). It is obvious in the case of VEE emergence, where epizootic viruses replicate more efficiently in equines and produce high viremia, that virus production is very important. Therefore, a strong correlation between cell survival and the suppression of virus production is essential for correctly interpreting CPE results. However, our results indicate that different VEEV strains can cause CPE at different time points after infection, making direct comparison of different virus strain in cell protection assays more difficult. We believe that a direct measurement of the reduction of virus production in the presence of different concentrations of IFN-α/β provides more relevant information about the potential resistance or sensitivity of viruses to antiviral effects of IFN. Moreover, the comparison of IFN-α/β-mediated cell protection over 5 days provides the opportunity for the accumulation of mutations in the virus genome, which could confound results.
By using full-length infectious cDNA clones derived from low-passage, closely related enzootic and epizootic strains, we were able to test the role of IFN-α/β resistance in natural VEE emergence, avoiding possible artificial mutations selected by cell culture passage and potentially altering the natural phenotype. Two different methods were used to evaluate IFN-α/β resistance: (i) L929 cell protection after IFN-α/β pretreatment and (ii) evaluation of the reduction in infectious virus production after IFN-α/β pretreatment of L929 cells. As described above, we believe that the latter assay is superior because some of the epizootic VEEV strains produce CPE faster in cell culture than others, and the CPE phenotype is not always well correlated with virus production at some time points. By measuring the effect of IFN-α/β pretreatment on viral replication in both murine and primate cells, we were not able to detect any difference in the IFN-α/β sensitivity or resistance between strain SH3 (subtype IC, epizootic) and the closely related sympatric strain ZPC738 (subtype ID, enzootic). Experiments with Vero cells, which do not produce IFN, indicated that this lack of difference between enzootic and epizootic strains was not explained by autocrine effects. Both epizootic strains used, SH3 (subtype IC, 1992) and 3908 (subtype IC, 1995), which did not show any difference in the IFN-α/β resistance compared to strain ZPC738 (subtype ID), are highly virulent in horses, producing high viremia and high mortality rates (29; R. A. Bowen, Colorado State University, unpublished data). In contrast, strain ZPC738 (subtype ID) is avirulent in horses, and serum viremia was barely detectable (29). Therefore, when we consider the authentic phenotypes exhibited by these viruses, our results indicate that the IFN-α/β resistance was probably not an important factor in the 1962/1995 or 1992/93 subtype IC VEE emergence events. These results need to be confirmed with equine IFN and cells, and these studies are under way in our laboratory.
Our results indicate that the resistance to IFN-α/β of VEEV strains is not a reliable in vitro marker of the epizootic phenotype. The ZPC738 enzootic strain exhibited similar resistance to IFN-α/β as the epizootic strains and much higher resistance than the TC-83 vaccine strain. However, in horses, the ZPC738 and TC-83 strains are both avirulent, causing a mild, self-limiting febrile illness with little or no viremia (26, 29). However, the importance of the IFN-α/β sensitivity and/or resistance for efficient replication in equines is still not well understood. It is probably necessary for VEEV to have a “basic resistance” to the IFN system for efficient initial replication in every vertebrate host. However, IFN-α/β resistance alone is not sufficient to explain the equine virulence of epizootic VEEV. Even if some enzootic, subtype ID strains exhibit lower murine IFN-α/β resistance than epizootic strains (25), no difference in mouse virulence has been observed (29).
To understand virulence and pathogenesis differences exhibited by enzootic and epizootic VEEV strains, tissue and cell tropism, mechanisms of early, viremia-independent virus dissemination in horses, and species specificity of IFN resistance deserve further study. Our model system utilizing infectious cDNA clones of closely related, low-passage, epizootic and enzootic viruses may prove helpful in addressing these seminal questions. Reverse genetic studies under way in our laboratory may also facilitate the mapping of viral genetic determinants responsible for the epizootic phenotype and a better understanding of VEE emergence.
Acknowledgments
We thank Ilya Frolov for providing RNA of Sindbis virus Toto1101 for the infectious center assay.
S.P. was supported by NIH Emerging Tropical Diseases T32 training grant AI-107536. This research was supported by NIH grants AI39800 and AI48807.
REFERENCES
- 1.Brault, A. C., A. M. Powers, E. C. Holmes, C. H. Woelk, and S. C. Weaver. 2002. Positively charged amino acid substitutions in the E2 envelope glycoprotein are associated with the emergence of Venezuelan equine encephalitis virus. J. Virol. 76:1718-1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brault, A. C., A. M. Powers, G. Medina, E. Wang, W. Kang, R. A. Salas, J. De Siger, and S. C. Weaver. 2001. Potential sources of the 1995 Venezuelan equine encephalitis subtype IC epidemic. J. Virol. 75:5823-5832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Briceno Rossi, A. L. 1967. Rural epidemic encephalitis in Venezuela caused by a group A arbovirus (VEE). Prog. Med. Virol. 9:176-203. [PubMed] [Google Scholar]
- 4.Calisher, C. H., and N. Karabatsos. 1988. Arbovirus serogroups: definition and geographic distribution, p. 19-57. In T. P. Monath (ed.), The arboviruses: epidemiology and ecology, vol. I. CRC Press, Boca Raton, Fla.
- 5.Davis, N. L., F. B. Grieder, J. F. Smith, G. F. Greenwald, M. L. Valenski, D. C. Sellon, P. C. Charles, and R. E. Johnston. 1994. A molecular genetic approach to the study of Venezuelan equine encephalitis virus pathogenesis. Arch. Virol. 9:99-109. [DOI] [PubMed]
- 6.Emeny, J. M., and M. J. Morgan. 1979. Regulation of the interferon system: evidence that Vero cells have a genetic defect in interferon production. J. Gen. Virol. 43:247-252. [DOI] [PubMed] [Google Scholar]
- 7.Grieder, F. B., and H. T. Nguyen. 1996. Virulent and attenuated mutant Venezuelan equine encephalitis virus show marked differences in replication in infection in murine macrophages. Microb. Pathog. 21:85-95. [DOI] [PubMed] [Google Scholar]
- 8.Grieder, F. B., and S. N. Vogel. 1999. Role of interferon and interferon regulatory factors in early protection against Venezuelan equine encephalitis virus infection. Virology 257:106-118. [DOI] [PubMed] [Google Scholar]
- 9.Hawley, R. J., and E. M. Eitzen, Jr. 2001. Biological weapons—a primer for microbiologists. Annu. Rev. Microbiol. 55:235-253. [DOI] [PubMed] [Google Scholar]
- 10.Jahrling, P. B., E. Navarro, and W. F. Scherer. 1976. Interferon induction and sensitivity as correlates to virulence of Venezuelan encephalitis viruses for hamsters. Arch. Virol. 51:23-35. [DOI] [PubMed] [Google Scholar]
- 11.Jahrling, P. B., and W. F. Scherer. 1973. Growth curves and clearance rates of virulent and benign Venezuelan encephalitis viruses in hamsters. Infect. Immun. 8:456-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kinney, R. M., G. J. Chang, K. R. Tsuchiya, J. M. Sneider, J. T. Roehrig, T. M. Woodward, and D. W. Trent. 1993. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5′-noncoding region and the E2 envelope glycoprotein. J. Virol. 67:1269-1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kinney, R. M., K. R. Tsuchiya, J. M. Sneider, and D. W. Trent. 1992. Genetic evidence that epizootic Venezuelan equine encephalitis (VEE) viruses may have evolved from enzootic VEE subtype I-D virus. Virology 191:569-580. [DOI] [PubMed] [Google Scholar]
- 14.Martin, D. H., W. H. Dietz, O. Alvaerez, Jr., and K. M. Johnson. 1982. Epidemiological significance of Venezuelan equine encephalomyelitis virus in vitro markers. Am. J. Trop. Med. Hyg. 31:561-568. [DOI] [PubMed] [Google Scholar]
- 15.Moncayo, A. C., G. M. Medina, Z. Kalvatchev, A. C. Brault, R. Barrera, J. Boshell, C. Ferro, J. E. Freier, J. C. Navarro, R. Salas, J. De Siger, C. Vasquez, R. Walder, and S. C. Weaver. 2001. Genetic diversity and relationships among Venezuelan equine encephalitis virus field isolates from Colombia and Venezuela. Am. J. Trop. Med. Hyg. 65:738-746. [DOI] [PubMed] [Google Scholar]
- 16.Oberste, M. S., M. Fraire, R. Navarro, C. Zepeda, M. L. Zarate, G. V. Ludwig, J. F. Kondig, S. C. Weaver, J. F. Smith, and R. Rico-Hesse. 1998. Association of Venezuelan equine encephalitis virus subtype IE with two equine epizootics in Mexico. Am. J. Trop. Med. Hyg. 59:100-107. [DOI] [PubMed] [Google Scholar]
- 17.Paredes, A., K. Alwell-Warda, S. C. Weaver, W. Chiu, and S. J. Watowich. 2001. Venezuelan equine encephalomyelitis virus structure and its divergence from old world alphaviruses. J. Virol. 75:9532-9537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powers, A. M., M. S. Oberste, A. C. Brault, R. Rico-Hesse, S. M. Schmura, J. F. Smith, W. Kang, W. P. Sweeney, and S. C. Weaver. 1997. Repeated emergence of epidemic/epizootic Venezuelan equine encephalitis from a single genotype of enzootic subtype ID virus. J. Virol. 71:6697-6705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rice, C. M., R. Levis, J. H. Strauss, and H. V. Huang. 1987. Production of infectious RNA transcripts from Sindbis virus cDNA clones: mapping of lethal mutations, rescue of a temperature-sensitive marker, and in vitro mutagenesis to generate defined mutants. J. Virol. 61:3809-3819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rico-Hesse, R., S. C. Weaver, J. de Siger, G. Medina, and R. A. Salas. 1995. Emergence of a new epidemic/epizootic Venezuelan equine encephalitis virus in South America. Proc. Natl. Acad. Sci. USA 92:5278-5281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roehrig, J. T., and R. A. Bolin. 1997. Monoclonal antibodies capable of distinguishing epizootic from enzootic varieties of subtype 1 Venezuelan equine encephalitis viruses in a rapid indirect immunofluorescence assay. J. Clin. Microbiol. 35:1887-1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salas, R. A., C. Z. Garcia, J. Liria, R. Barrera, J. C. Navarro, G. Medina, C. Vasquez, Z. Fernandez, and S. C. Weaver. 2001. Ecological studies of enzootic Venezuelan equine encephalitis in north-central Venezuela, 1997-1998. Am. J. Trop. Med. Hyg. 64:84-92. [DOI] [PubMed] [Google Scholar]
- 23.Sambrook, J., and D. Russell. 2001. Molecular cloning: a laboratory manual, 3rd ed. Cold Spring Harbor Press, Cold Spring Harbor, N.Y.
- 24.Schlesinger, S., and M. J. Schlesinger. 2001. Togaviridae: the viruses and their replication, p. 895-916. In D. M. Knipe and P. M. Howley (ed.), Fields virology, 4th ed. Lippincott/The Williams & Wilkins Co., Philadelphia, Pa.
- 25.Spotts, D. R., R. M. Reich, M. A. Kalkhan, R. M. Kinney, and J. T. Roehrig. 1998. Resistance to alpha/beta interferons correlates with the epizootic and virulence potential of Venezuelan equine encephalitis viruses and is determined by the 5′ noncoding region and glycoproteins. J. Virol. 72:10286-10291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walton, T. E., O. Alvarez, Jr., R. M. Buckwalter, and K. M. Johnson. 1972. Experimental infection of horses with an attenuated Venezuelan equine encephalomyelitis vaccine (strain TC-83). Infect. Immun. 5:750-756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walton, T. E., and M. A. Grayson. 1988. Venezuelan equine encephalomyelitis, p. 203-231. In T. P. Monath (ed.), The arboviruses: epidemiology and ecology, vol. IV. CRC Press, Boca Raton, Fla.
- 28.Wang, E., R. Barrera, J. Boshell, C. Ferro, J. E. Freier, J. C. Navarro, R. Salas, C. Vasquez, and S. C. Weaver. 1999. Genetic and phenotypic changes accompanying the emergence of epizootic subtype IC Venezuelan equine encephalitis viruses from an enzootic subtype ID progenitor. J. Virol. 73:4266-4271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang, E., R. A. Bowen, G. Medina, A. M. Powers, W. Kang, L. M. Chandler, R. E. Shope, and S. C. Weaver. 2001. Virulence and viremia characteristics of 1992 epizootic subtype IC Venezuelan equine encephalitis viruses and closely related enzootic subtype ID strains. Am. J. Trop. Med. Hyg. 65:64-69. [DOI] [PubMed] [Google Scholar]
- 30.Weaver, S. C. 1998. Recurrent emergence of Venezuelan equine encephalomyelitis, p. 27-42. In W. M. Scheld and J. Hughes (ed.), Emerging infections I. ASM Press, Washington, D.C.
- 31.Weaver, S. C., R. Salas, R. Rico-Hesse, G. V. Ludwig, M. S. Oberste, J. Boshell, R. B. Tesh, et al. 1996. Re-emergence of epidemic Venezuelan equine encephalomyelitis in South America. Lancet 348:436-440. [DOI] [PubMed] [Google Scholar]
- 32.Young, N. A., and K. M. Johnson. 1969. Antigenic variants of Venezuelan equine encephalitis virus: their geographic distribution and epidemiologic significance. Am. J. Epidemiol. 89:286-307. [DOI] [PubMed] [Google Scholar]