A nine-year-old girl presented to the emergency department in the fall of 2009 with a one-week history of cough, neck swelling, sore throat and mild diarrhea, but no fever or vomiting. She had a history of asthma, which was treated with montelukast. Her physical examination showed subcutaneous emphysema above the clavicles. A chest radiograph showed pneumomediastinum (Figure 1). She was discharged home but returned several hours later with worsening symptoms. A neck radiograph showed massive subcutaneous emphysema in the prevertebral space (Figure 2). An echocardiogram showed a very small localized pneumopericardium over the left ventricle. Polymerase chain reaction testing of nasal secretions was positive for pandemic (H1N1) 2009 virus. She was admitted to the pediatric intensive care unit and given 100% oxygen therapy, inhaled salbutamol and oral oseltamivir. She was also given antibiotics empirically, because of the potential loss of sterility of the prevertebral space. Apart from lingering fever, she recovered uneventfully and was discharged after five days.
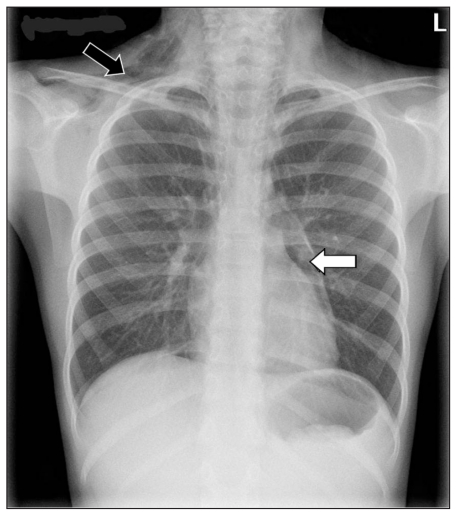
Figure 1:
Chest radiograph of a nine-year-old girl showing subcutaneous emphysema (black arrow) and pneumomediastinum (white arrow).
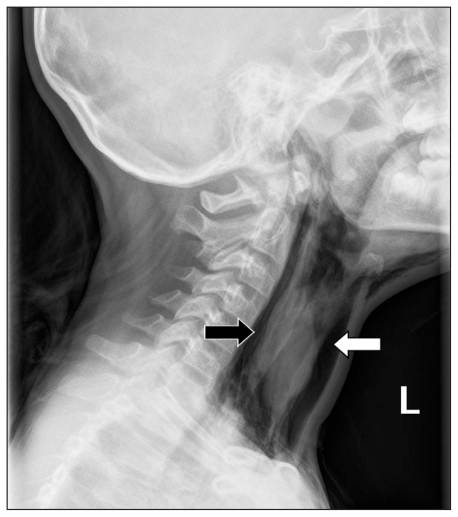
Figure 2:
Lateral radiograph of the neck showing prevertebral air (black arrow) and massive subcutaneous emphysema (white arrow).
A 14-year-old boy presented to the emergency department in the fall of 2009 with a five-day history of fever, cough, sore throat, abdominal pain and fatigue. There was no history of vomiting. He had a history of very mild asthma, having last used inhaled salbutamol over a year earlier. He had mild tachypnea. There was limitation in lateral neck movement, but no subcutaneous emphysema on palpation. Neck and chest radiographs showed subcutaneous air at the sternoclavicular notch and anterior to the cervical vertebra, but no pneumomediastinum or pneumopericardium. Testing of nasal secretions by polymerase chain reaction was positive for pandemic (H1N1) 2009 virus. He was given oral oseltamivir; he rapidly improved and was discharged within three days.
A three-year-old boy presented to the emergency department in the fall of 2009 with a four-day history of fever, cough, runny nose and sudden-onset neck swelling. He had vomited once. He had been diagnosed with asthma six months earlier, but had been using inhaled corticosteroids and bronchodilators inconsistently for the past five months. He was tachycardic, with a maximum heart rate of 160 beats/min, and tachypneic, with a maximum respiratory rate of 62 breaths/min. He required supplemental oxygen to maintain oxygen saturation above 92%. There was palpable subcutaneous emphysema at the face, neck, chest and upper abdomen. He had increased respiratory effort and a prolonged expiratory phase. His chest radiograph showed subcutaneous emphysema and pneumomediastinum. Testing of his nasal secretions by polymerase chain reaction was positive for pandemic (H1N1) 2009 virus. He was given oral oseltamivir, 100% oxygen therapy, antibiotics, inhaled salbutamol and oral corticosteroids. He had an uncomplicated course and was discharged after four days.
Discussion
Infection with pandemic (H1N1) 2009 virus has been associated with severe respiratory complications in children, including secondary bacterial pneumonia and respiratory failure.1 A recent report described the association of pandemic (H1N1) influenza and pneumomediastinum in two Japanese children.2 Although there is a well-established link between underlying respiratory illnesses, especially asthma, and spontaneous pneumomediastinum,3,4 our experience with the three patients we have described supports the association of pandemic (H1N1) influenza with air leak syndrome, including pneumomediastinum, and subcutaneous and prevertebral emphysema in a different pediatric population.
Spontaneous pneumomediastinum
Spontaneous pneumomediastinum is related to Valsalva manoeuvres (e.g., coughing, vomiting, labour, sneezing, use of inhaled medication), severe bronchopulmonary infection (e.g., measles, mycoplasma pneumonia), foreign body ingestion, esophageal rupture and dental surgery, although there can be no identifiable cause. Pneumomediastinum can also occur secondary to chest injury, mechanical ventilation and thoracic surgery.3,4 Because an inciting event may be identifiable in up to 70%–90% of cases,3 the absence of an obvious event in all of our patients is unusual.
Previous reviews have recommended excluding serious underlying causes such as esophageal perforation due to vomiting or ingesting a foreign body (Boerhaave syndrome), as well as other serious causes of chest pain, including pulmonary embolism and pericarditis.3,4
Spontaneous pneumomediastinum is rare in children. Its precise incidence is unknown, but estimates range from 1 in 800 to 1 in 42 000 patients presenting to an emergency department, or 3 per 1000 children presenting with asthma to an emergency department.3 We observed three instances of spontaneous pneumomediastinum among 110 children admitted during the second wave of pandemic (H1N1) 2009. In contrast, five patients were admitted with pneumomediastinum in each of the two preceding years out of a total of 6083 patients in 2007 and 6266 patients in 2008 (Nicole Beaulieu, Certified Health Information Management Professional, Decision Support, Children’s Hospital of Eastern Ontario: personal communication, 2009), suggesting the incidence is markedly increased in children with pandemic (H1N1) influenza.
Pneumomediastinum usually results from mechanisms that increase alveolar pressure, which leads to alveolar rupture. By direct extension, air enters interstitial tissues and extends easily into mediastinal borders. Air can then readily communicate with connective tissues in the cervical, endothoracic, peritoneal and even vertebral areas.3,4 In severe pneumomediastinum, the trapped air can cause airway obstruction or impingement in venous return via tamponade.4
Spontaneous pneumomediastinum may be missed because of its subtle clinical findings. Signs and symptoms include cough, dyspnea, subcutaneous emphysema and chest pain.3,4 Subtler symptoms include sore throat, neck pain, voice change and odynophagia.3,4
Diagnosis is confirmed with imaging. Radiographic findings include air streaks outlining mediastinal structures, especially around cardiac landmarks. Two views are helpful; findings may be present only on a lateral radiograph.3 Computed tomography (CT) has greater sensitivity for the detection of pneumomediastinum and is considered the gold standard for its diagnosis.4 If a serious underlying cause is suspected, such as perforation of the esophagus, or if signs such as fever, hypotension and leukocytosis are present, then CT or contrast-enhanced swallow radiography (or both) is indicated.3
The rate of complications of pneumomediastinum, such as pneumopericardium, pneumothorax and pseudotamponade, is unknown, but complications are thought to be rare. Pneumomediastinum on its own is generally not harmful and has a low rate of recurrence.3,4 It usually resolves within a few days with supportive care, which includes analgesia, rest and treatment of the underlying medical condition.3,4
Inhalation of 100% oxygen is used to replace nitrogen in the escaped air with oxygen; nitrogen is absorbed slowly by capillaries while oxygen is absorbed rapidly. Although oxygen has been suggested as a potential treatment for spontaneous pneumomediastinum in children, the evidence supporting its use is inconclusive.3 It was used in the care of two of our patients. Oral intake can be discontinued if there is respiratory distress or suspicion of esophageal perforation.4
Serial chest radiographs are not recommended unless there is a deterioration in the patient’s condition; instead, clinical status may be used to indicate improvement or resolution.3 Expert opinion recommends avoiding activities in the recovery period that increase the risk of developing a pneumomediastinum, such as excessive physical exercise or playing of a wind instrument.3
Spontaneous pneumomediastinum and pandemic (H1N1) influenza
As mentioned previously, Hasegawa and colleagues recently reported on two Japanese children with pandemic (H1N1) influenza and pneumomediastinum.2 The patients were six and eight years of age, and neither had a history of asthma. Soto-Abraham and coworkers reported that pathologic features of fatal pandemic (H1N1) influenza included hemorrhage and necrosis of the upper respiratory tract and necrosis of the bronchiolar walls.1 Air leak associated with this infection could be due to airway necrosis, severe cough or both. However, there are no reports of air leak complicating pandemic (H1N1) influenza in adults. All three of our patients had a history of mild asthma. A recent retrospective study conducted at a pediatric hospital in Canada suggested that even mild asthma is a risk factor for severe pandemic (H1N1) influenza and admission to hospital.5 Asthma may augment the risk of airway epithelial injury or increase the risk of alveolar rupture due to pre-existing lung hyperinflation. Pandemic (H1N1) influenza appears to be associated with pneumomediastinum and subcutaneous and prevertebral emphysema in children. These conditions should be excluded in children with pandemic (H1N1) influenza, particularly if they have a history of asthma of any degree of severity.
Key points
Pneumomediastinum should be considered in children with pandemic (H1N1) influenza who have dyspnea or chest pain, particularly if they have a history of asthma.
In a child with pneumomediastinum, serious underlying causes, such as esophageal perforation or foreign body ingestion, should be excluded.
In most children, isolated spontaneous pneumomediastinum can be managed with careful clinical observation.
The section Cases presents brief case reports that convey clear, practical lessons. Preference is given to common presentations of important rare conditions, and important unusual presentations of common problems. Articles start with a case presentation (500 words maximum), and a discussion of the underlying condition follows (1000 words maximum). Generally, up to five references are permitted and visual elements (e.g., tables of the differential diagnosis, clinical features or diagnostic approach) are encouraged. Written consent from patients for publication of their story is a necessity and should accompany submissions. See information for authors at www.cmaj.ca.
See also practice article by Yazer and colleagues, page 215
Footnotes
Competing interests: None declared for Sharmila Udupa and Tahir Hameed. Tom Kovesi has received payment for lectures from Nycomed Canada Inc. and Merck Frosst Canada Ltd., and payment for educational presentations from AstraZeneca Canada Inc.
This article has been peer reviewed.
Contributors: All authors contributed to the conception and design of the manuscript. Sharmila Udupa, Tahir Hameed and Tom Kovesi drafted the article. All authors critically revised the manuscript for important intellectual content and approved the final version submitted for publication.
References
- 1.Soto-Abraham MV, Soriano-Rosas J, Díaz-Quiñónez A, et al. Pathological changes associated with the 2009 H1N1 virus. N Engl J Med 2009;361:2001–3 [DOI] [PubMed] [Google Scholar]
- 2.Hasegawa M, Hashimoto K, Morozumi M, et al. Spontaneous pneumomediastinum complicating pneumonia in children infected with the 2009 pandemic influenza A (H1N1) virus. Clin Microbiol Infect 2010;16:195–9 [DOI] [PubMed] [Google Scholar]
- 3.Bullaro FM, Bartoletti SC. Spontaneous pneumomediastinum in children: a literature review. Pediatr Emerg Care 2007;23:28–30 [DOI] [PubMed] [Google Scholar]
- 4.Caceres M, Ali SZ, Braud R, et al. Spontaneous pneumomediastinum: a comparative study and review of the literature. Ann Thorac Surg 2008;86:962–6 [DOI] [PubMed] [Google Scholar]
- 5.O’Riordan S, Barton M, Yau Y, et al. Risk factors and outcomes among children admitted to hospital with pandemic H1N1 influenza. CMAJ 2010;182:39–44 [DOI] [PMC free article] [PubMed] [Google Scholar]