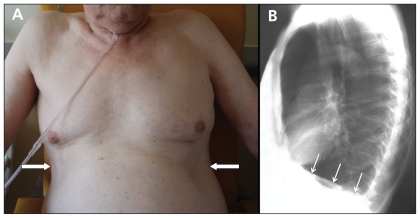
A 72-year-old man with a 70 pack-year history of smoking was referred to our emergency department for an exacerbation of chronic obstructive pulmonary disease (COPD). On examination, he breathed through pursed lips and had paradoxical indrawing of the lower rib cage margin with inspiration (Hoover sign)1 (Figure 1A, Appendix 1, video available at www.cmaj.ca/cgi/content/full/cmaj.092092/DC1). A chest radiograph showed distension of the lungs and flattening of the diaphragm (Figure 1B). Repeated flow-volume loops at rest and during an incremental exercise test (Appendix 2, available at www.cmaj.ca/cgi/content/full/cmaj.092092/DC1) showed severe airflow obstruction (one-second forced expired volume 0.9 L, 30% predicted value; curve 0) and dynamic pulmonary hyperinflation with a leftward shift of the flow-volume loops at higher ventilation levels (curves 1–4).
Figure 1:
(A) Paradoxical retraction of the lower intercostal spaces on inspiration (arrows) in a 72-year-old man with chronic obstructive pulmonary disease. (B) Lateral chest radiograph showing distention of the lungs associated with flattening of the diaphragm (arrows).
Expiratory flow limitation is a hallmark finding in patients with severe airflow obstruction, as in COPD. It is extremely difficult for these patients to increase their expiratory flow above its resting value. In healthy controls, lung volume at the end of expiration approximates the relaxation volume of the respiratory system (i.e., functional residual capacity) (Appendix 3, available at www.cmaj.ca/cgi/content/full/cmaj.092092/DC1). By contrast, in patients with limited flow, expiratory flow limitation leads to incomplete lung emptying and gas trapping; the end-expiratory lung volume exceeds the predicted functional residual capacity, causing dynamic pulmonary hyperinflation. This phenomenon increases the work of breathing and is currently considered the main mechanism explaining dyspnea in patients with COPD.
Pulmonary hyperinflation can cause flattening of the diaphragm and impairs its piston-like downward displacement capacity. When this occurs, the inspiratory contraction of the flattened diaphragm decreases the transverse diameter of the lower rib cage. Originally described by Hoover,1 the resulting eponymous sign may be overlooked, although it may be present in up to 76% of patients with severe COPD.2 The frequency of the sign increases with the severity of airflow obstruction.2 In addition, it is one of the most easily reproducible clinical findings for detection of obstructive airway disease (sensitivity 58%, specificity 86%).3 Hoover sign may be a useful clinical marker of severe airway obstruction to assist at the bedside in patient triage and management in emergency settings.3
Supplementary Material
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
REFERENCES
- 1.Hoover CF. The diagnostic significance of inspiratory movemens of the rib costal margins. Am J Med Sci 1920;159:633–46 [Google Scholar]
- 2.Garcia-Pachon E, Padilla-Navas I. Frequency of Hoover’s sign in stable patients with chronic obstructive pulmonary disease. Int J Clin Pract 2006;60:514–7 [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Pachon E. Paradoxical movement of the lateral rib margin (Hoover sign) for detecting obstructive airway disease. Chest 2002;122:651–5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.