Abstract
Aims/hypothesis
Diabetes increases the risk of cardiovascular disease (CVD) and heart failure, as well as other serious complications, such as renal disease and depression. However, these conditions are often present prior to diabetes diagnosis. We sought to determine whether they increase the risk of developing diabetes independent of other risk factors.
Methods
We identified 58,056 non-diabetic adults aged ≥30 years with no evidence of diabetes. Using electronic medical records, we identified the presence of four conditions at baseline (CVD, heart failure, renal disease and depression) and then estimated diabetes incidence over 5 years separately for patients with and without each of these conditions. Each incidence estimate was adjusted for baseline values of age, sex, fasting glucose, body mass index, systolic blood pressure, triacylglycerol, HDL-cholesterol, smoking and the presence of the other three conditions.
Results
Patients with CVD were 35% (95% CI 23–48%) more likely to develop diabetes after controlling for other risk factors. Heart failure was independently associated with an increase in diabetes incidence of 48% (95% CI 27–73%), and depression was associated with a 10% (95% CI 2–20%) increase. Chronic kidney disease was associated with a non-significant risk increase of 10% (95% CI –2–25%).
Conclusions/interpretation
Complications of diabetes are more prevalent among patients who will ultimately develop diabetes, and increase the risk of diabetes independently of other known risk factors. The apparent bidirectional relationships suggest that primary prevention of CVD may also help prevent diabetes.
Keywords: Comorbidities, Diabetes, Incidence, Risk factors
Introduction
Patients with type 2 diabetes are at elevated risk of cardiovascular disease (CVD), renal disease, heart failure and depression, conditions that dramatically increase costs and mortality relative to patients without diabetes [1]. Because these conditions are often already present when diabetes is diagnosed [2], we examined whether cardiovascular disease, renal disease, heart failure and depression increase the risk of developing diabetes after accounting for other known risk factors, including obesity, hyperglycaemia, hypertension and dyslipidaemia.
Methods
Kaiser Permanente Northwest (KPNW) is a closed group model health maintenance organisation that provides comprehensive medical care to approximately 475,000 individuals in the Portland, Oregon area of the USA. We identified 58,056 non-pregnant adults age 30 or older who did not have a prior diagnosis of diabetes, had a fasting plasma glucose test result <7 mmol/l, and also had blood pressure, obesity (body mass index), HDL-cholesterol and triacylglycerol measured in 2003 or 2004, and who remained members of KPNW for at least 5 years following the date that the last of the clinical variables mentioned above was measured (index date). Those who died or left the health plan were excluded. From electronic medical records, we determined the baseline prevalence of cardiovascular disease (International Classification of Diseases, Clinical Modification [ICD-9-CM; www.icd9data.com/2007/Volume1/240-279/250-259/250/default.htm] codes 410.xx–414.xx, 430.xx–432.xx, 434.xx–436.xx, 437.1, 440.xx, 441.xx, 444.xx, 437.0 and 443.81, and revascularisation codes 36.01, 36.02, 36.05, 36.09 and 36.1x), heart failure (428.xx) and depression (296.2, 296.3, 300.4, 309.1 and 311). We also identified chronic kidney disease (estimated glomerular filtration rate <60 ml min−1 1.73 m−2) from serum creatinine values using the modified Modification of Diet in Renal Disease (MDRD) equation.
All participants were followed for up to 5 years from the index date for new onset of diabetes, defined as an inpatient or outpatient diagnosis (ICD-9-CM codes 250.xx), a dispensing of an anti-hyperglycaemic medication, or two fasting plasma glucose results >7.0 mmol/l. For each condition, we compared the incidence of diabetes per 1,000 person-years among those with and without the conditions. To isolate the independent contributions of the conditions, we adjusted the incidence rates for age, sex, baseline measures of fasting glucose, body mass index, systolic blood pressure, triacylglycerol, HDL-cholesterol, smoking and the presence of the other health conditions in question. For example, when comparing those with and without CVD, we adjusted for the presence of heart failure, chronic kidney disease and depression in addition to age, sex and the metabolic variables. To account for potential ascertainment bias, we further adjusted for the number of fasting glucose tests performed during follow-up. All analyses were conducted with SAS version 8.2 (SAS, Cary, NC, USA), using Poisson regression for incidence densities, a feature of PROC GENMOD that uses time to event (or follow-up time) as an offset variable and allows multivariable adjustment of incidence estimates. The study was reviewed and approved by the Institutional Review Board of Kaiser Permanente Northwest with a waiver of informed consent.
Results
Within 5 years of follow-up, 6.1% (n = 3,537) of the study sample developed diabetes (Table 1). These patients were older and more likely to be men, non-white and to smoke compared with patients who did not develop diabetes. Baseline metabolic variables (fasting glucose, body mass index, systolic blood pressure, triacylglycerol and HDL-cholesterol) were all significantly more adverse among those who developed diabetes than among those who did not. In addition, CVD, heart failure, chronic kidney disease and depression were all significantly more prevalent at baseline among patients who subsequently developed diabetes compared with those who did not. Patients who developed diabetes had slightly more fasting glucose tests on average than those who did not develop diabetes.
Table 1.
Baseline characteristics of patients who did and did not develop diabetes within 5 years
| Developed diabetes | No diabetes | p value | |
|---|---|---|---|
| n (%) | 3,527 (6.1%) | 54,529 (93.9%) | – |
| Mean age (years) | 58.7 (11.3) | 56.8 (12.0) | <0.0001 |
| Men | 51.5% | 44.1% | <0.0001 |
| Non-white | 10.1% | 8.2% | <0.0001 |
| Current smoker | 14.5% | 12.4% | <0.0001 |
| Metabolic variables | |||
| Fasting plasma glucose (mmol/l) | 6.0 (0.8) | 5.2 (0.5) | <0.0001 |
| Body mass index (kg/m2) | 34.3 (7.2) | 29.6 (6.2) | <0.0001 |
| Systolic blood pressure (mmHg) | 137 (18) | 130 (18) | <0.0001 |
| HDL-cholesterol (mmol/l) | 1.2 (0.3) | 1.4 (0.4) | <0.0001 |
| Triacylglycerol (mmol/l) | 2.3 (1.8) | 1.6 (1.2) | <0.0001 |
| Complications (%) | |||
| Cardiovascular disease | 21.6 | 13.0 | <0.0001 |
| Heart failure | 5.5 | 2.0 | <0.0001 |
| Chronic kidney disease | 9.9 | 7.1 | <0.0001 |
| Depression | 24.0 | 20.4 | <0.0001 |
| Mean number of fasting glucose tests during follow-up | 2.7 (2.0) | 2.4 (2.0) | <0.0001 |
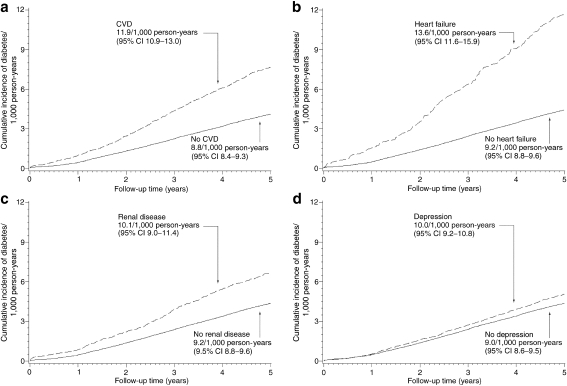
Figure 1 displays the adjusted cumulative incidence of diabetes for patients with CVD (panel a), heart failure (panel b), chronic kidney disease (panel c) and depression (panel d). After adjustment for all other risk factors, patients with CVD developed diabetes at a rate of 11.9/1,000 person-years (95% CI 10.9–13.0), compared with 8.8 (95% CI 8.4–9.3) among patients without CVD, for an increased risk of 35% (RR 1.35, 95% CI 1.23–1.48). Heart failure was associated with an increase in the risk of diabetes of 48% (RR 1.48, 95% CI 1.27–1.73). Depression was independently associated with an increase in the risk of diabetes of 10% (RR 1.10, 95% CI 1.02–1.20). The relationship between chronic kidney disease and diabetes did not reach statistical significance (RR 1.10, 95% CI 0.97–1.24).
Fig. 1.
Cumulative incidence of diabetes by presence (dashed line) or absence (continuous line) of CVD (a; RR 1.35 [95% CI 1.23–1.48]), heart failure (b; RR 1.48 [95% CI 1.27–1.73]), renal disease (c; RR 1.10 [0.97–1.24] and depression (d; RR 1.10 [95% CI 1.02–1.20]). Analyses are adjusted for age, sex, body mass index, fasting glucose, systolic blood pressure, triacylglycerol, HDL-cholesterol, smoking and the presence of the other conditions shown
Discussion
To our knowledge, no studies to date have simultaneously analysed cardiovascular disease, heart failure, chronic kidney disease and depression as predictors of incident diabetes while also controlling for known metabolic predictors of diabetes risk. The complex interplay between cardiometabolic risk factors, such as hyperglycaemia, obesity, hypertension, dyslipidaemia and diabetes and its complications, requires a large sample with sufficient follow-up to isolate the independent contributions of each factor. In this observational cohort study of 58,056 non-diabetic patients, we found that the presence of each of these complications increased the risk of developing diabetes independently of one another and of other known risk factors.
Cardiovascular disease is recognised as an independent risk factor for diabetes [3]. Heart failure has also been shown to increase the risk of diabetes [4], as has depression [5]. Although each of these studies reported higher risks than we found, this was probably due to insufficient control for known risk factors, such as fasting glucose, or for health conditions other than those being tested. Indeed, our results were stronger in models that did not include metabolic variables or the other health conditions (data not shown). Thus, our results probably represent a more accurate estimate of the independent contributions to diabetes risk of CVD, heart failure, kidney disease and depression.
In addition to the observational study design, our study has several limitations. First, the data are limited by the inclusion of only clinic attendees who had the necessary metabolic variables measured and the opportunity for assessment of the health conditions we analysed. It is possible that non-attendees without the necessary measurements were less likely to have the studied conditions, and were also at lower risk of developing diabetes. If so, the incidence rates we report for patients without the conditions could be overestimated. However, it is also possible that the risk of developing diabetes would be unaffected if the relative relationship between the conditions studied and diabetes is the same in attendees and non-attendees. Second, we assessed the presence of CVD, heart failure, renal disease and depression at baseline. We did not attempt to account for the development of these conditions prior to diabetes onset. If patients who developed the conditions were at an elevated risk of diabetes similar to the risk in those who had the conditions at baseline, this higher risk would have been mis-assigned to those without the conditions, which would have resulted in underestimation of the relative risk. Though this is speculative, we believe that, for this reason, the relative risks of incident diabetes associated with the studied conditions are conservative. Third, patients with the studied conditions received fasting glucose tests somewhat more frequently, thereby increasing their opportunity for a diabetes diagnosis. Although our estimates adjusted for the number of follow-up tests, some unmeasured ascertainment bias might remain. Finally, our assessment of diabetes status both at baseline (as an exclusion criterion) and at follow-up (as the outcome measure) did not include oral glucose tolerance tests. Therefore, some patients with clinical diabetes but with fasting glucose <7 mmol/l were probably included in the study, while others may have developed clinical diabetes but remained undetected because of subdiagnostic fasting glucose levels. We cannot determine how this limitation would have affected our results.
Lifestyle interventions have been repeatedly shown to prevent or delay the onset of type 2 diabetes in at-risk individuals [6], and also improve CVD risk factors [7]. Furthermore, the benefits of early intervention last well beyond the duration of the intervention itself [8–10]. Of course, the presence of serious comorbidities, such as those we examined, may reduce patients’ willingness or ability to engage in intensive exercise programmes. In any case, the bidirectional relationship between diabetes and its complications calls for accurate assessment of health risk well before diabetes onset so that the maximum benefits of early intervention can be realised. Furthermore, it is possible that primary prevention of CVD and other complications will reduce the risk of subsequent diabetes.
Acknowledgements
This research was supported by Tethys Bioscience. GA Nichols had full access to the data and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Duality of interest
GA Nichols has received research funding from GlaxoSmithKline, Novartis Pharmaceuticals, Novo Nordisk, and Takeda Pharmaceuticals America. EJ Moler is an employee of Tethys Bioscience.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviation
- CVD
Cardiovascular disease
References
- 1.Association AD. Economic costs of diabetes in the U.S. in 2007. Diab Care. 2008;31:596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 2.Nichols GA, Arondekar B, Herman WH. Complications of dysglycemia and medical costs associated with nondiabetic hyperglycemia. Am J Manag Care. 2008;14:791–798. [PubMed] [Google Scholar]
- 3.American Diabetes Association Standards of medical care in diabetes—2010. Diab Care. 2010;33:S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kostis JB, Saunders M. The association of heart failure with insulin resistance and the development of type 2 diabetes. Am J Hypertens. 2005;18:731–737. doi: 10.1016/j.amjhyper.2004.11.038. [DOI] [PubMed] [Google Scholar]
- 5.Golden SH, Williams JE, Ford DE, et al. Depressive symptoms and the risk of type 2 diabetes: the atherosclerosis risk in communities study. Diab Care. 2004;27:429–435. doi: 10.2337/diacare.27.2.429. [DOI] [PubMed] [Google Scholar]
- 6.American Diabetes Association. National Institute of Diabetes and Digestive and Kidney Disorders Prevention or delay of type 2 diabetes. Diab Care. 2004;27(Suppl 1):S47–S54. doi: 10.2337/diacare.27.2007.s47. [DOI] [PubMed] [Google Scholar]
- 7.Diabetes Prevention Program Research Group Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the Diabetes Prevention Program. Diab Care. 2005;28:888–894. doi: 10.2337/diacare.28.4.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lindstrom J, Ilanne-Parikka P, Peltonen M, et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006;368:1673–1679. doi: 10.1016/S0140-6736(06)69701-8. [DOI] [PubMed] [Google Scholar]
- 9.Diabetes Prevention Program Research Group 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1167–1186. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 2008;371:1783–1789. doi: 10.1016/S0140-6736(08)60766-7. [DOI] [PubMed] [Google Scholar]