Abstract
We studied human immunodeficiency virus type 1 (HIV-1) chimeric viruses altering in their gp120 V1V2 and V3 envelope regions to better map which genetic alterations are associated with specific virus phenotypes associated with HIV-1 disease progression. The V1V2 and V3 regions studied were based on viruses isolated from an individual with progressing HIV-1 disease. Higher V3 charges were linked with CXCR4 usage, but only when considered within a specific V1V2 and V3 N-linked glycosylation context. When the virus gained R5X4 dual tropism, irrespective of its V3 charge, it became highly resistant to inhibition by RANTES and highly sensitive to inhibition by SDF-1α. R5 viruses with higher positive V3 charges were more sensitive to inhibition by RANTES, while R5X4 dualtropic viruses with higher positive V3 charges were more resistant to inhibition by SDF-1α. Loss of the V3 N-linked glycosylation event rendered the virus more resistant to inhibition by SDF-1α. The same alterations in the V1V2 and V3 regions influenced the extent to which the viruses were neutralized with soluble CD4, as well as monoclonal antibodies b12 and 2G12, but not monoclonal antibody 2F5. These results further identify a complex set of alterations within the V1V2 and V3 regions of HIV-1 that can be selected in the host via alterations of coreceptor usage, CC/CXC chemokine inhibition, CD4 binding, and antibody neutralization.
Human immunodeficiency virus type 1 (HIV-1) belongs to the family of lentiviruses that cause slow degenerative diseases (16, 17, 36). The high rate of mutation associated with HIV-1 allows for the generation of viruses that can evade the host immune responses and that give rise to variant biological properties, such as cell tropism. HIV-1 predominantly enters the cell types that it infects through an initial interaction between the gp120 envelope of the virus and the CD4 molecule, followed by an interaction with a specific CC/CXC chemokine receptor, thereby mediating membrane fusion and viral entry (3, 42). Although a multitude of coreceptors can be utilized by HIV-1, the two most significant for virus transmission and pathogenesis are the CC chemokine receptor CCR5 and the CXC chemokine receptor CXCR4, respectively (2, 57). The preferred phenotypic classifications for HIV-1 are R5 for isolates using CCR5, X4 for those using CXCR4, and R5X4 for those capable of using both coreceptors (3). The association of X4 variants with disease progression and the maintenance of R5 variants throughout infection suggest that X4 viruses are either a cause of or evolve in response to progressive immunosuppression, while R5 variants make up the reservoir responsible for persistent infection (45, 46, 48, 52). Detection of X4 viruses is also predictive of rapid CD4 cell decline (9, 28). Although X4 isolates can occasionally be detected early, they usually appear later in infection and are associated with progression to AIDS (10, 49).
The CC chemokines RANTES, MIP-1α, and MIP-1β, the natural ligands for the CCR5 chemokine receptor, and SDF-1α, the natural ligand for the CXCR4 coreceptor, have been shown to successfully block the replication of HIV-1 in vitro (4, 8). Furthermore, the association between a large array of genetic polymorphisms within chemokine and chemokine receptor genes and disease progression indicates a strong association between the chemokine network and viral replication in vivo (53). Moreover, loss of sensitivity to the CC chemokines correlates with characteristic changes in V3 amino acid residues that have been described in the virus phenotype switch from R5 to X4 (14, 15). Initial adaptation of an HIV-1 population to strong selective pressures can result in a compromised replication rate. In subsequent rounds of replication under continued selection, occurrence of second-site mutations that compensate for part or all of the lost fitness can be observed (6, 44). In the case of gp120, changes needed for immune escape should not compromise vital mechanisms of virus entry.
The gp120 molecule is extensively glycosylated and contains approximately 24 N-linked glycosylation sites, and alterations within N-linked glycosylation sites have previously been shown to alter the coreceptor usage, CD4 binding, and antibody neutralization profiles of HIV-1 (1, 7, 27, 30, 33, 34, 37, 38, 41, 51, 55). However, despite the wide range of information on the issue, a lot of questions with regard to the specific associations between the gp120 elements, e.g., glycosylation patterns and the V3 loop charge, and their effects with regard to altered phenotypic characteristics of the virus need to be answered. Here we elected to study chimeric molecularly cloned viruses based on virus isolates generated from a patient with progressing disease in order to identify what effect specific altered genotypes have on the virus phenotype and how these alterations may be selected in the host.
The V3 charge, the V1V2 region, and V3 N-linked glycosylation alter HIV-1 coreceptor usage and CC/CXC chemokine inhibition.
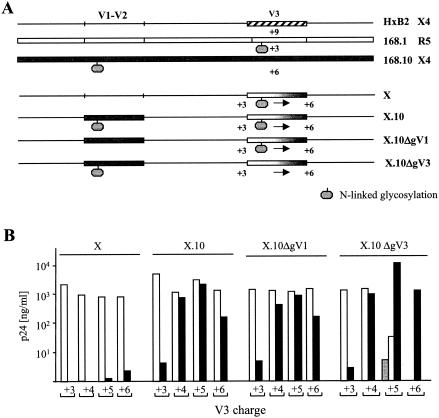
We have previously reported on the generation and characterization of a panel of molecularly cloned HIV-1 strains that varied with respect to their V1V2 and V3 gp120 regions and that altered in their coreceptor usage phenotypes (38). These viruses were composed of different combinations of V1V2 and V3 sequences within the context of the HxB2 gp120 envelope and the LAI viral backbone. In summary, the V1V2 and V3 regions studied were based on primary virus isolates generated from an individual with a progressing disease course who had undergone a switch in the virus phenotype from the non-syncytium-inducing to the syncytium-inducing phenotype (11, 12). A schematic representation of the chimeric viruses studied is depict in Fig. 1A. Alterations within the V1V2 and V3 regions, corresponding to the observed amino acid differences between the early and late viruses from the patient, were introduced by site-directed mutagenesis as previously described (11, 12, 38). Replication-competent virus stocks were used to analyze coreceptor usage patterns on U87.CD4 cells expressing different coreceptors (Fig. 1B). Modifications of the V3 charge alone (in viruses designated the X panel) had little effect in switching the virus from use of the CCR5 coreceptor to use of the CXCR4 coreceptor, whereas addition of the late-stage V1V2 region (X.10 viruses) had a marked effect in providing CXCR4 usage at V3 charges of +4, +5, and +6. CCR5 usage was significantly reduced when the V3 charge was high and was eliminated at a charge of +6 when it was accompanied by loss of the V3 loop N-linked glycosylation event (X.10ΔgV3).
FIG. 1.
Viruses used in this study and their coreceptor usage profiles. (A) Schematic representation of the chimeric molecularly cloned viruses generated from patient ACH168 and used in this study (11, 12, 38). (B) Coreceptor usage patterns of the viruses on U87.CD4 cells expressing CCR3, CCR5, or CXCR4. CCR3 is represented by grey bars, CCR5 is represented by white bars, and CXCR4 is represented by black bars. Cells of the U87.CD4+ line (3.0 × 104) expressing CCR3, CCR5, or CXCR4 were infected with the viruses from each panel (0.1 to 1 μg of p24/ml). Cells were infected for 18 h before being washed twice with phosphate-buffered saline and fed with fresh medium. On day 10 of culture, the p24 levels in the culture supernatants were determined by using a standard enzyme-linked immunosorbent assay. Data are expressed as mean p24 values of triplicate wells, and the intersample standard deviation did not exceed 10%.
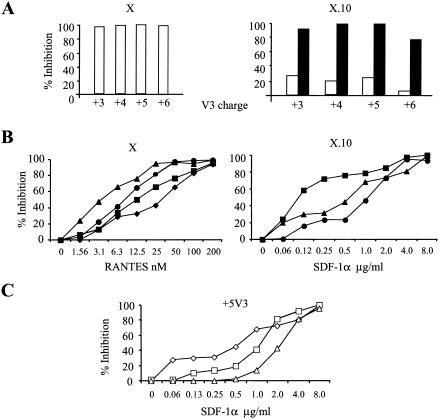
We studied the inhibition of the X and X.10 panels of viruses by a single high-dose concentration of CC or CXC chemokines on CD4+-enriched lymphocytes (Fig. 2A) by using chemokine concentrations previously identified as inhibitory (50). As expected, all of the X viruses, irrespective of their V3 charge, were completely inhibited by the high concentration of RANTES (Fig. 2A), while the X.10 viruses lost their inhibition by RANTES and demonstrated a high degree of inhibition by SDF-1α (Fig. 2A), even though they had been shown to utilize the CCR5 coreceptor as efficiently as CXCR4 on U87.CD4 cells (Fig. 1B). The effect of SDF-1α virus inhibition and loss of virus replication caused by RANTES was again irrespective of the V3 charge.
FIG. 2.
CC/CXC chemokine inhibitions. (A) Bulk inhibition of the X (R5) panel of viruses with a high concentration of RANTES (200 nM) and of the X.10 (R5X4) panel of viruses with a high concentration of RANTES (200 nM) or SDF-1α (2 μg/ml). The experiments were performed with CD4+-enriched lymphocytes isolated from a CCR5+/+ individual. The white bars represent percent inhibition by RANTES, and the black bars represent percent inhibition by SDF-1α. (B) Inhibition of the X and X.10 panels of viruses carrying the different V3 charges (symbols: diamonds, +3 V3 charge; squares, +4 V3 charge; triangles, +5 V3 charge; circles, +6 V3 charge) by RANTES and SDF-1α, respectively. (C) Inhibition of the +5 V3 viruses carrying the different glycosylation pattern (symbols: diamonds, X.10; squares, X.10ΔgV1; triangles, X.10ΔgV3). CD4+-enriched lymphocytes isolated from a CCR5+/+ individual were used in the RANTES inhibition assays, while CD4+-enriched lymphocytes isolate from a CCR5−/− individual were used in the SDF-1α inhibition experiments. The respective CD4+ lymphocytes (2.0 × 105) were preincubated with serial dilutions of the chemokine for 1 h, and then the viruses were added. The day chosen for calculating inhibiting response was based on the day the p24 value of the positive control well peaked (not longer than 14 days), and percent inhibition was calculated by determining the reduction in p24 production in the presence of the agent compared to that for the cultures with virus only. For each inhibition experiment, a positive control, virus incubated with cells in the absence of the agent, and a negative control, virus in the absence of cells, was included. The negative control p24 concentration was subtracted from all of the test results. Each experiment was repeated at least twice with CD4+-enriched lymphocytes from different donors. Data are expressed as mean p24 values of triplicate wells, and the intersample SD did not exceed 10%.
We wished to further identify whether alterations in the V3 charge alone have the capacity to influence virus inhibition by the CC chemokine RANTES. Since the group of X viruses (V3 charges of +3, +4, +5, and +6) utilize predominantly the CCR5 coreceptor and could be completely neutralized by high concentrations of RANTES, we tested the inhibition of these viruses on CD4+ lymphocytes by using limiting dilutions of RANTES. The viruses with the lower V3 charges were more resistant to the inhibitory effects of RANTES than were the viruses with the higher V3 charges (Fig. 2B). Similar results were obtained with viruses with the same charge but different amino acid substitutions (data not shown), suggesting that this phenomenon is indeed charge related and not due to the specific single amino acid substitutions made to generate the charge alterations.
In order to assess the influence of the V3 charge and its effect on CXCR4 usage, we performed inhibition assays with limiting dilutions of SDF-1α, the natural ligand for CXCR4. Since the X.10 viruses that we used in these assays both use CCR5 and CXCR4, we performed the assays with CD4+-enriched lymphocytes isolated from an individual homozygous for the bp 32 deletion in the CCR5 gene (CCR5−/−). Since viruses with a +3 V3 charge did not demonstrate significant CXCR4 usage, they were excluded from the experiment. When we compare the effects of different V3 charges (+4, +5, and +6), we identified a difference in inhibition by SDF-1α, with the +4 V3 lower charge being more sensitive to the blocking effects (Fig. 2B). We also compared the SDF-1α inhibition of the viruses altering with respect to the N-linked glycosylation patterns in the V1 and V3 regions and encompassing the different V3 charges. Figure 2C depicts the inhibition of the +5 V3 panel of viruses altering with respect to the V1 and V3 N-linked glycosylation patterns, demonstrating that the viruses missing the V1 or V3 N-linked glycosylation events were more resistant to inhibition by SDF-1α than the virus with both the V1 and V3 N-linked glycosylation events.
It is generally accepted that the R5-to-X4 phenotype switch of HIV-1 is associated with an increase in the overall positive charge of the V3 region during disease progression (43). We have previously shown that the rise in the V3 charge alone is not sufficient for CXCR4 utilization, and here we demonstrate further that a virus with a +6 V3 charge can be altered to use CXCR4 exclusively by insertion of the late-stage disease V1V2 region in combination with loss of the V3 N-linked glycosylation event (Fig. 1B) (38). Without the alteration in V3 N-linked glycosylation, the V1V2 region from late-stage disease is significant in determining the R5X4 dualtropic phenotype but not in reducing CCR5 usage. The late-stage V1V2 region has an amino acid insertion coding for an extra N-linked glycosylation site; however, removing this site had no obvious effect on altering coreceptor utilization. Lengthening of the V1 region has been previously described, and a number of studies have suggested that length alterations of this region are observed in patients undergoing disease progression (19, 23, 47). Our results further indicate a specific interaction between the V1V2 and V3 regions required for CCR5 coreceptor utilization and that the V3 N-linked glycosylation event is significant for this interaction (30, 32, 37).
Our results suggest that as the R5X4 phenotype emerges, even at a low V3 charge, the virus may have lost its ability to be controlled by CC chemokines. This observation may be a reflection of the high expression levels of CXCR4 at the surface of the CD4+ lymphocyte and not a true reflection of the ability of these viruses to use either the CCR5 or CXCR4 coreceptor. When we studied the dose-inhibitory effect of the CC chemokine RANTES on the X panel of viruses, we found that increasing the V3 charge increased sensitivity to the blocking effects of RANTES (Fig. 2B); therefore, without the combined alteration of V1V2, there may be a selective advantage to a virus with a lower V3 charge. Viruses that evolve with higher V3 charges will be more restricted in their replication by the blocking CC chemokines, maybe helping to further explain why some individuals can remain for longer periods of time with R5 viruses. The same argument can be used for the X4 viruses, where we have found that those with the lower V3 charges are more sensitive to the controlling effects of SDF-1α. Although it is unlikely that levels of SDF-1α in the circulation can control HIV-1 replication, there may be some control exerted within different compartments, such as within lymph nodes. If SDF-1α can more efficiently control the viruses with lower V3 charges, then there may be a selection pressure providing for viruses with higher V3 charges to emerge once the switch in coreceptor usage has been initiated.
For CXCR4 usage, loss of the N-linked glycosylation site at a +5 V3 charge rendered the virus more resistant to inhibition by SDF-1α, providing an explanation for the preferential loss of this glycosylation event as the V3 charge increases. It is tempting to speculate that what we have observed is a modification of coreceptor affinity and that the viruses with the lower or higher charges have increased affinities for their respective coreceptors, CCR5 and CXCR4. However, without the corresponding biochemical analysis, we refer to our viruses as possessing alterations of coreceptor utilization. The interaction between the V1V2 and V3 regions will determine how efficiently the gp120 envelope interacts with the CCR5 and CXCR4 coreceptors. A shift in coreceptor affinity could have significant consequences for virus evolution, with a higher-affinity gp120, either R5 or X4, being that preferentially transmitted or associated with late-stage disease, respectively.
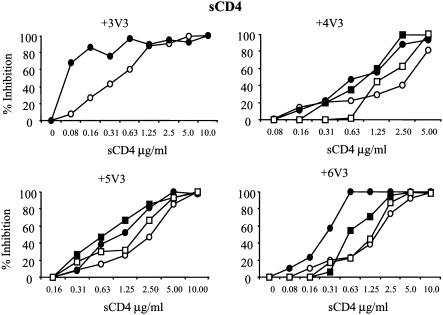
Modifications in the V3 charge and V1V2 and V3 N-linked glycosylation differentially alter HIV-1 neutralization by sCD4.
Since variations in the V3 charge and N-linked glycosylation could confer alterations of relative CCR5 and CXCR4 coreceptor utilization, we wished to identify whether the same viruses altered with respect to their affinity for CD4. To this end, we measured the neutralization of the viruses by limiting dilutions of soluble CD4 (sCD4) on CD4+ lymphocytes isolated from an individual homozygous for the wild-type CCR5 allele, CCR5+/+. We selected for study the four panels of viruses (X, X.10, X.10ΔgV1, and X.10ΔgV3) and those altering with respect to the V3 charge (+3, +4, +5, and +6). For the +3 panel of viruses, the X.10ΔgV1 and X.10ΔgV3 viruses were excluded because of their poor replication profile on CD4+ lymphocytes (data not shown). The neutralization of these viruses with sCD4 can be seen in Fig. 3. Irrespective of the V3 charge, all of the X viruses are neutralized with lower concentrations of sCD4 than the X.10 viruses, suggesting that addition of the V1V2 region from a late stage of infection increases the affinity of the gp120 protein for the CD4 molecule. When the N-linked glycosylation event is removed from the V1 region, the shift in sCD4 neutralization remains, indicating that insertion of this event does not modulate sCD4 binding. However, when the N-linked glycosylation event within the V3 region is removed (for all of the V3 charges tested [+4, +5, and +6]), then the viruses demonstrate the same inhibition profiles as the original X panel of viruses. These results suggest that, irrespective of the V3 charge and coreceptor usage patterns, the affinity of gp120 for CD4 can be modulated by the V1V2-V3 interaction and that the V3 N-linked glycosylation event can be significant for determining CD4 binding strength. Although the shift in sCD4 neutralization appears to be small, it should be considered that we are studying molecularly cloned viruses.
FIG. 3.
sCD4 neutralization of viruses altering in V3 charge and pattern of gp120 N-linked glycosylation (symbols: closed circles, X; open circles, X.10; open squares, X.10ΔgV1; closed squares, X.10ΔgV3). The assays were carried out by using a scheme similar to that described for the chemokine inhibition assay (Fig. 2) but with preincubation of the viruses with sCD4, followed by addition of CD4+-enriched lymphocytes.
It has previously been found that gp120 V2 and V3 N-linked glycosylation events can modulate CD4, as well as coreceptor binding (7, 18, 25, 26, 33, 34), with the V3 charge also influencing coreceptor usage (21, 54). Here we identified that the virus with the lower +3 V3 charge was more sensitive to inhibition by sCD4 than were the viruses with the higher +4, +5, and +6 V3 charges, but it is not known whether this is specifically charge related or whether the effect is a result of the specific D324N replacement encountered, although the V3 region has not been shown to interact with the CD4 binding site (CD4BS). Alterations of the V1V2 region, but not its N-linked glycosylation event, and loss of the V3 N-linked glycosylation site both influenced the ability of gp120 to interact with the CD4 molecule, irrespective of the V3 charge. This result could be explained by either an alteration of CD4 affinity or a change in the gp120 structure that results in either better exposure or occlusion of the CD4BS. The V1V2 region alterations could result in a virus with greater CD4 affinity with a more open CD4BS structure that is lost, or closed, when the V3 N-linked glycosylation site is removed. These results again demonstrate intermediate viruses whose phenotype is dependent on the combination of events encountered between the V1V2 and V3 regions. It is of interest that the more dualtropic viruses, or those with the lowest coreceptor affinity or utilization patterns, are the viruses with the higher affinity or which posses more accessible binding for CD4. During disease progression, compensatory mutations may therefore occur in gp120 that heighten CD4 affinity in order to compensate for the weakened CCR5 and/or CXCR4 coreceptor interactions or, alternatively, occlude the CD4BS, as has been previously proposed (33).
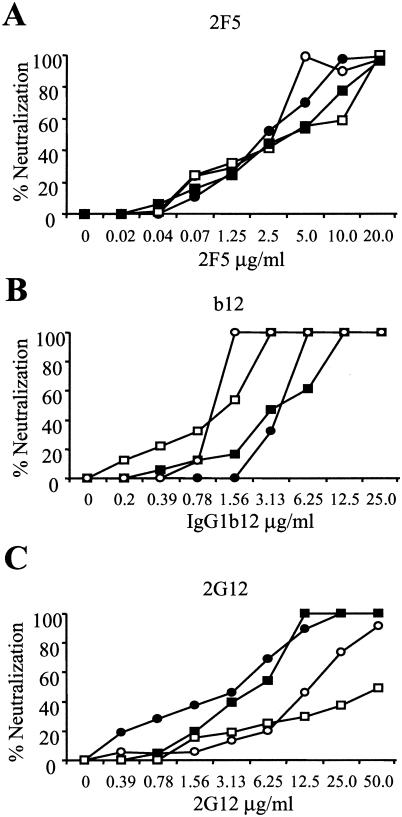
Modifications in V1V2 and V3 N-linked glycosylation can differentially alter neutralization by MAbs b12 and 2G12.
The observations that coreceptor usage and CD4 affinity can be modulated by combinations of V3 charge, variant V1V2 regions, and V3 N-linked glycosylation led us to postulate that these alterations may also modulate the ability of HIV-1 to be neutralized by antibodies. In order to address this issue, we studied the profiles of neutralization of selected molecularly cloned viruses by well-characterized, envelope-directed, monoclonal antibodies (MAbs). We used three MAbs with defined epitopes (2F5, b12, and 2G12). Other MAbs were tested (15e, 17b, and 48d), but none was shown to possess neutralizing activity (data not shown). Since the +5 V3 panel of viruses (X, X.10, X.10ΔgV1, and X.10ΔgV3) covered the virus phenotypes we were interested in studying, we tested these viruses in neutralization assays with CD4+ lymphocytes isolated from an individual homozygous for the wild-type CCR5 allele, CCR5+/+, with the results shown in Fig. 4.
FIG. 4.
Virus neutralization by MAbs 2F5, b12, and 2G12. The +5 V3 array of viruses (symbols: closed circles, X; open circles, X.10; open squares, X.10ΔgV1; closed squares, X.10ΔgV3) were tested for neutralization by MAbs 2F5 (A), b12 (B), and 2G12 (C). Other MAbs were tested (15e, 17b, and 48d), but none was shown to possess neutralizing activity (data not shown). The assays were carried out by using the same scheme as described for the sCD4-mediated neutralization assay.
Different patterns of neutralization were observed for the three different MAbs. MAb 2F5, directed against an epitope in the gp41 region (39), demonstrated no specific inhibitory profile, with all of the viruses showing similar neutralization profiles (Fig. 4A). For MAb b12, with its discontinuous epitope in the gp120 structure containing residues from the CD4BS of gp120 (24, 40), we found the neutralization profile of the X and X.10ΔgV3 viruses to be similar, with the X.10 and X.10ΔgV1 viruses clustering together (Fig. 4B). This distinctive pattern was the opposite of that observed for inhibition by sCD4 (Fig. 3), where the “intermediate” dualtropic viruses were more resistant to neutralization than the more extreme R5 and X4 viruses. For MAb 2G12, directed against specific carbohydrate determinants (41, 51), the same virus clustering pattern was observed, but with the reverse profile (Fig. 4C). The observation of a reverse neutralization profile indicates that the results obtained are not due to general differences in the replication profiles of the viruses on CD4+ lymphocytes. With both b12 and 2G12 neutralization, we have identified an association between the V1V2 region and loss of N-linked glycosylation within the V3 region. Addition of the late-stage V1V2 region alters neutralization, which cannot be explained by the addition of the N-linked glycosylation event in the V1 region, with the effect being reversed by the loss of N-linked glycosylation within the V3 region.
Changes in HIV-1 tropism have previously been shown to have a tight association with HIV-1 neutralization profiles that can have a major influence on HIV-1 pathogenesis (35). A number of recent reports have demonstrated that alterations of gp120 can be linked to HIV-1 immune escape from neutralizing-antibody responses (22, 55). The term “glycan shield” has been coined to describe the phenomenon in which alterations in N-linked glycosylation shift responses from appropriate sites on the gp120 envelope (55). The gp120 conformation is highly dependent on the type of glycosylation events present and their distribution on the surface of the molecule (27, 31). Tight cooperation between gp120 structural elements, e.g., between the V1V2 and V3 loops, have previously been shown to mediate different structural states and functions (7, 18, 25, 26, 34). We demonstrate here that alterations of the V1V2 and V3 regions can differentially modulate the response of the virus to different MAbs with variant specificities. Previous reports have stated that alterations of glycosylation events in the V2 region can modulate recognition by both anti-V3 and anti-CD4BS antibodies (33). The opening of the gp120 envelope structure to reveal the CD4BS would have obvious implications for pathogenesis, with these viruses being open for antibody recognition and control.
The binding site for MAb 2G12 is known to have a conformation- and carbohydrate-dependent epitope on the gp120 surface, and this is the first description of an alteration in the V3 N-linked glycosylation altering neutralization by this antibody, likely through disruption of the structure of the gp120 envelope (41, 51). Whether similar antibodies directed against carbohydrate sites are commonly induced in vivo has yet to be established. The results described here indicate that the V3 N-linked glycosylation site can somewhat protect the 2G12 epitope from recognition and that there may be selective pressure for its presence when the immune system is intact. Since we have shown that loss of the V3 N-linked glycosylation event can alter relative coreceptor usage and favor stronger CXCR4 utilization, its removal may be preferentially selected when the immune system is weakened later in the disease course. This same effect may also help explain why the V3 N-linked glycosylation site is preserved in individuals with intact immune responses and why these viruses remain relative CCR5 users. It is of interest that the V1V2 and V3 changes we examined did not overlap any of the binding sites of the MAbs studied. A likely explanation is therefore conformational changes within the MAb binding sites (including CD4BS) induced by the V1V2 and V3 changes, similar to what has been previously shown (5). Another explanation is that modified V1V2 and V3 can interact with residues that are close to these binding sites and that modify antibody recognition.
These results could indicate a short-term transitional state during the coreceptor shift process that renders the envelope open to neutralization by antibodies targeting the CD4BS. Xiang et al. have shown that an amino acid alteration within the gp120 molecule, S375W, can affect virus neutralization in a manner similar to what was observed for the X.10ΔgV1 viruses (56). Moreover, the S375W mutants demonstrated a decreased affinity for the CCR5 receptor (56). The replacement of serine 375 is a rare event among HIV-1 strains, while at the same time, S375H replacement is widespread among AE native recombinants, which possess a high rate of the syncytium-inducting phenotype, as well as the ΔgV3 N-linked glycosylation genotype. The similarity, in terms of phenotypic properties, of subtype D viruses also correlates with a high frequency of the ΔgV3 N-linked glycosylation mutation (HIV Sequence Compendium 2001, available at the hiv-web.lanl.gov website) (13, 29, 52). These observations indicate that deglycosylation of the V3 region is a functional mechanism correlating with the X4 phenotype. These results should be considered with those indicating that the pattern of tropism is highly related to both neutralization susceptibility and CD4 binding (20, 35). These results suggest that a shift in HIV-1 coreceptor usage can result from compensatory alterations within gp120 selected through pressures such as CC/CXC chemokine and neutralizing-antibody responses.
In summary, the gp120 modifications that occur during disease progression and that coincide with the R5-to-X4 switch have consequences for in vivo viral fitness. This fitness will depend on an array of host responses, both innate and adaptive, that coincide with alterations in coreceptor usage and envelope structure.
Acknowledgments
This work was supported by grants from the European Union (QLK2-CT-1999-01321 “EuroVac”) and the Nederlands AIDS Fond (4019) and a fellowship from the Royal Dutch Academy for Arts and Sciences (awarded to W.A.P.). All neutralizing MAbs were supplied through the EU Program EVA/MRC Centralized Facility for AIDS Reagents, National Institute for Biological Standards and Control, United Kingdom (grants QLK2-CT-1999-00609 and GP828102).
We thank M. P. de Baar for critical review of the manuscript.
REFERENCES
- 1.Back, N. K. T., L. Smit, J. J. de Jong, W. Keulen, M. Schutten, J. Goudsmit, and M. Tersmette. 1994. An N-glycan within the human immunodeficiency virus type 1 gp120 V3 loop affects virus neutralization. Virology 199:431-438. [DOI] [PubMed] [Google Scholar]
- 2.Berger, E. A. 1997. HIV entry and tropism: the chemokine receptor connection. AIDS 11(Suppl. A):S3-S16. [PubMed] [Google Scholar]
- 3.Berger, E. A., R. W. Doms, E. M. Fenyo, B. T. Korber, D. R. Littman, J. P. Moore, Q. J. Sattentau, H. Schuitemaker, J. Sodroski, and R. A. Weiss. 1998. A new classification for HIV-1. Nature 391:240. [DOI] [PubMed] [Google Scholar]
- 4.Bleul, C. C., M. Farzan, H. Choe, C. Parolin, I. Clark-Lewis, J. Sodroski, and T. A. Springer. 1996. The lymphocyte chemoattractant SDF-1 is a ligand for LESTR/fusin and blocks HIV-1 entry. Nature 382:829-833. [DOI] [PubMed] [Google Scholar]
- 5.Bouma, P., M. Leavitt, P. F. Zhang, I. A. Sidorov, D. S. Dimitrov, and G. V. Quinnan, Jr. 2003. Multiple interactions across the surface of the gp120 core structure determine the global neutralization resistance phenotype of human immunodeficiency virus type 1. J. Virol. 77:8061-8071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyer, P. L., H. Q. Gao, and S. H. Hughes. 1998. A mutation at position 190 of human immunodeficiency virus type 1 reverse transcriptase interacts with mutations at positions 74 and 75 via the template primer. Antimicrob. Agents Chemother. 42:447-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carrillo, A., and L. Ratner. 1996. Cooperative effects of the human immunodeficiency virus type 1 envelope variable loops V1 and V3 in mediating infectivity for T cells. J. Virol. 70:1310-1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cocchi, F., A. L. DeVico, A. Garzino-Demo, S. K. Arya, R. C. Gallo, and P. Lusso. 1995. Identification of RANTES, MIP-1α, and MIP-1β as the major HIV-suppressive factors produced by CD8+ T cells. Science 270:1811-1815. [DOI] [PubMed] [Google Scholar]
- 9.Connor, R. I., H. Mohri, Y. Cao, and D. D. Ho. 1993. Increased viral burden and cytopathicity correlate temporally with CD4+ T-lymphocyte decline and clinical progression in human immunodeficiency virus type 1-infected individuals. J. Virol. 67:1772-1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cornelissen, M., G. Mulder-Kampinga, J. Veenstra, F. Zorgdrager, C. Kuiken, S. Hartman, J. Dekker, L. van der Hoek, C. Sol, R. Coutinho, and J. Goudsmit. 1995. Syncytium-inducing (SI) phenotype suppression at seroconversion after intramuscular inoculation of a non-syncytium-inducing/SI phenotypically mixed human immunodeficiency virus population. J. Virol. 69:1810-1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Jong, J. J., A. de Ronde, W. Keulen, M. Tersmette, and J. Goudsmit. 1992. Minimal requirements for the human immunodeficiency virus type 1 V3 domain to support the syncytium-inducing (SI) phenotype: analysis by single amino acid substitution. J. Virol. 66:6777-6780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Jong, J. J., J. Goudsmit, W. Keulen, B. Klaver, W. Krone, M. Tersmette, and A. de Ronde. 1992. Human immunodeficiency virus type 1 clones chimeric for the envelope V3 domain differ in syncytium formation and replication capacity. J. Virol. 66:757-765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Wolf, F., E. Hogervorst, J. Goudsmit, E.-M. Fenyö, H. Rübsamen-Waigmann, H. Holmes, B. Galvao-Castro, E. Karita, C. Wasi, S. D. K. Sempala, E. Baan, F. Zorgdrager, V. Lukashov, S. Osmanov, C. Kuiken, M. Cornelissen, and WHO Network on HIV Isolation and Characterization. 1994. Syncytium-inducing and non-syncytium-inducing capacity of human immunodeficiency virus type 1 subtypes other than B: phenotypic and genotypic characteristics. AIDS Res. Hum. Retrovir. 10:1387-1400. [DOI] [PubMed] [Google Scholar]
- 14.Doranz, B. J., J. Rucker, Y. Yi, R. J. Smyth, M. Samson, S. C. Peiper, M. Parmentier, R. G. Collman, and R. W. Doms. 1996. A dual-tropic primary HIV-1 isolate that uses fusin and the beta-chemokine receptors CKR-5, CKR-3, and CKR-2b as fusion cofactors. Cell 85:1149-1158. [DOI] [PubMed] [Google Scholar]
- 15.Fouchier, R. A. M., M. Groenink, N. A. Kootstra, M. Tersmette, H. G. Huisman, F. Miedema, and H. Schuitemaker. 1992. Phenotype associated sequence variation in the third variable domain of the human immunodeficiency virus type 1 gp120 molecule. J. Virol. 66:3183-3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gallo, R. C., S. Z. Salahuddin, M. Popovic, G. M. Shearer, M. Kaplan, B. F. Haynes, T. J. Palker, R. Redfield, J. Oleske, B. Safai, G. White, P. Foster, and P. D. Markham. 1984. Frequent detection and isolation of cytopathic retroviruses (HTLV-III) from patients with AIDS and at risk for AIDS. Science 224:500-503. [DOI] [PubMed] [Google Scholar]
- 17.Gonda, M. A., F. Wong-Staal, R. C. Gallo, J. E. Clements, O. Narayan, and R. V. Gilden. 1985. Sequence homology and morphologic similarity of HTLV-III and visna virus, a pathogenic lentivirus. Science 227:173-177. [DOI] [PubMed] [Google Scholar]
- 18.Gram, G. J., A. Hemming, A. Bolmstedt, B. Jansson, S. Olofsson, L. Akerblom, J. O. Nielsen, and J. E. Hansen. 1994. Identification of an N-linked glycan in the V1-loop of HIV-1 gp120 influencing neutralization by anti-V3 antibodies and soluble CD4. Arch. Virol. 139:253-261. [DOI] [PubMed] [Google Scholar]
- 19.Groenink, M., R. A. Fouchier, S. Broersen, C. H. Baker, M. Koot, A. B. van't Wout, H. G. Huisman, F. Miedema, M. Tersmette, and H. Schuitemaker. 1993. Relation of phenotype evolution of HIV-1 to envelope V2 configuration. Science 260:1513-1516. [DOI] [PubMed] [Google Scholar]
- 20.Hammond, A. L., J. Lewis, J. May, J. Albert, P. Balfe, and J. A. McKeating. 2001. Antigenic variation within the CD4 binding site of human immunodeficiency virus type 1 gp120: effects on chemokine receptor utilization. J. Virol. 75:5593-5603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hwang, S. S., T. J. Boyle, H. K. Lyerly, and B. R. Cullen. 1992. Identification of envelope V3 loop as the major determinant of CD4 neutralization sensitivity of HIV-1. Science 257:535-537. [DOI] [PubMed] [Google Scholar]
- 22.Johnson, W. E., J. M. Sauvron, and R. C. Desrosiers. 2001. Conserved, N-linked carbohydrates of human immunodeficiency virus type 1 gp41 are largely dispensable for viral replication. J. Virol. 75:11426-11436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kitrinos, K. M., N. G. Hoffman, J. A. E. Nelson, and R. Swanstrom. 2003. Turnover of env variable region 1 and 2 genotypes in subjects with late-stage human immunodeficiency virus type 1 infection. J. Virol. 77:6811-6822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kohlstaedt, L. A., J. Wang, J. M. Friedman, P. A. Rice, and T. A. Steitz. 1992. Crystal structure at 3.5 A resolution of HIV-1 reverse transcriptase complexed with an inhibitor. Science 256:1783-1790. [DOI] [PubMed] [Google Scholar]
- 25.Koito, A., G. Harrowe, J. A. Levy, and C. Cheng-Mayer. 1994. Functional role of the V1/V2 region of human immunodeficiency virus type 1 envelope glycoprotein gp120 in infection of primary macrophages and soluble CD4 neutralization. J. Virol. 68:2253-2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koito, A., L. Stamatatos, and C. Cheng-Mayer. 1995. Small amino acid sequence changes within the V2 domain can affect the function of a T-cell line-tropic human immunodeficiency virus type 1 envelope gp120. Virol. 206:878-884. [DOI] [PubMed] [Google Scholar]
- 27.Kolchinsky, P., E. Kiprilov, P. Bartley, R. Rubinstein, and J. Sodroski. 2001. Loss of a single N-linked glycan allows CD4-independent human immunodeficiency virus type 1 infection by altering the position of the gp120 V1/V2 variable loops. J. Virol. 75:3435-3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koot, M., I. P. M. Keet, A. H. V. Vos, R. E. Y. de Goede, M. T. L. Roos, R. A. Coutinho, F. Miedema, P. T. A. Schellekens, and M. Tersmette. 1993. Prognostic value of HIV-1 syncytium-inducing phenotype for rate of CD4+ cell depletion and progression of AIDS. Ann. Intern. Med. 118:681-688. [DOI] [PubMed] [Google Scholar]
- 29.Korber, B. T. M., K. MacInnes, R. F. Smith, and G. Myers. 1994. Mutational trends in V3 loop protein sequences observed in different genetic lineages of human immunodeficiency virus type 1. J. Virol. 68:6730-6744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Labrosse, B., C. Treboute, A. Brelot, and M. Alizon. 2001. Cooperation of the V1/V2 and V3 domains of human immunodeficiency virus type 1 gp120 for interaction with the CXCR4 receptor. J. Virol. 75:5457-5464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Land, A., and I. Braakman. 2001. Folding of the human immunodeficiency virus type 1 envelope glycoprotein in the endoplasmic reticulum. Biochimie. 83:783-790. [DOI] [PubMed]
- 32.Lee, M. K., J. Heaton, and M. W. Cho. 1999. Identification of determinants of interaction between CXCR4 and gp120 of a dual-tropic HIV-1DH12 isolate. Virology 257:290-296. [DOI] [PubMed] [Google Scholar]
- 33.Ly, A., and L. Stamatatos. 2000. V2 loop glycosylation of the human immunodeficiency virus type 1 SF162 envelope facilitates interaction of this protein with CD4 and CCR5 receptors and protects the virus from neutralization by anti-V3 loop and anti-CD4 binding site antibodies. J. Virol. 74:6769-6776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Malenbaum, S. E., D. Yang, L. Cavacini, M. Posner, J. Robinson, and C. Cheng-Mayer. 2000. The N-terminal V3 loop glycan modulates the interaction of clade A and B human immunodeficiency virus type 1 envelopes with CD4 and chemokine receptors. J. Virol. 74:11008-11016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McKnight, A., R. A. Weiss, C. Shotton, Y. Takeuchi, H. Hoshino, and P. R. Clapham. 1995. Change in tropism upon immune escape by human immunodeficiency virus. J. Virol. 69:3167-3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Narayan, O., M. C. Zink, D. Huso, D. Sheffer, S. Crane, S. Kennedy-Stoskopf, P. E. Jolly, and J. E. Clements. 1988. Lentiviruses of animals are biological models of the human immunodeficiency viruses. Microb. Pathog. 5:149-157. [DOI] [PubMed] [Google Scholar]
- 37.Ogert, R. A., M. K. Lee, W. Ross, A. Buckler-White, M. A. Martin, and M. W. Cho. 2001. N-linked glycosylation sites adjacent to and within the V1/V2 and the V3 loops of dualtropic human immunodeficiency virus type 1 isolate DH12 gp120 affect coreceptor usage and cellular tropism. J. Virol. 75:5998-6006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pollakis, G., S. Kang, A. Kliphuis, M. I. Chalaby, J. Goudsmit, and W. A. Paxton. 2001. N-linked glycosylation of the HIV type 1 gp120 envelope glycoprotein as a major determinant of CCR5 and CXCR4 coreceptor utilization. J. Biol. Chem. 276:13433-13441. [DOI] [PubMed] [Google Scholar]
- 39.Purtscher, M., A. Trkola, G. Gruber, A. Buchacher, R. Predl, F. Steindl, C. Tauer, R. Berger, N. Barrett, and A. Jungbauer. 1994. A broadly neutralizing human monoclonal antibody against gp41 of human immunodeficiency virus type 1. AIDS Res. Hum. Retrovir. 10:1651-1658. [DOI] [PubMed] [Google Scholar]
- 40.Roben, P., J. P. Moore, M. Thali, J. Sodroski, C. F. Barbas III, and D. R. Burton. 1994. Recognition properties of a panel of human recombinant Fab fragments to the CD4 binding site of gp120 that show differing abilities to neutralize human immunodeficiency virus type 1. J. Virol. 68:4821-4828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanders, R. W., M. Venturi, L. Schiffner, R. Kalyanaraman, H. Katinger, K. O. Lloyd, P. D. Kwong, and J. P. Moore. 2002. The mannose-dependent epitope for neutralizing antibody 2G12 on human immunodeficiency virus type 1 glycoprotein gp120. J. Virol. 76:7293-7305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sattentau, Q. J., A. G. Dalgleish, R. A. Weiss, and P. C. L. Beverley. 1986. Epitopes of the CD4 antigen and HIV infection. Science 234:1120-1123. [DOI] [PubMed] [Google Scholar]
- 43.Scarlatti, G., E. Tresoldi, A. Bjorndal, R. Fredriksson, C. Colognesi, H. K. Deng, M. S. Malnati, A. Plebani, A. G. Siccardi, D. R. Littman, E. M. Fenyo, and P. Lusso. 1997. In vivo evolution of HIV-1 co-receptor usage and sensitivity to chemokine-mediated suppression. Nat. Med. 3:1259-1265. [DOI] [PubMed] [Google Scholar]
- 44.Schock, H. B., V. M. Garsky, and L. C. Kuo. 1996. Mutational anatomy of an HIV-1 protease variant conferring cross-resistance to protease inhibitors in clinical trials. Compensatory modulations of binding and activity. J. Biol. Chem. 271:31957-31963. [DOI] [PubMed] [Google Scholar]
- 45.Schuitemaker, H., M. Koot, N. A. Kootstra, M. W. Dercksen, R. E. Y. de Goede, R. P. van Steenwijk, J. M. A. Lange, J. K. M. Eeftinck Schattenkerk, F. Miedema, and M. Tersmette. 1992. Biological phenotype of human immunodeficiency virus type 1 clones at different stages of infection: progression of disease is associated with a shift from monocytotropic to T-cell-tropic virus populations. J. Virol. 66:1354-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schuitemaker, H., N. A. Kootstra, R. E. Y. de Goede, F. de Wolf, F. Miedema, and M. Tersmette. 1991. Monocytotropic human immunodeficiency virus type 1 (HIV-1) variants detectable in all stages of HIV-1 infection lack T-cell line tropism and syncytium-inducing ability in primary T-cell culture. J. Virol. 65:356-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shioda, T., S. Oka, S. M. Xin, H. Liu, R. Harukuni, A. Kurotani, M. Fukushima, M. K. Hasan, T. Shino, Y. Takebe, A. Iwamoto, and Y. Nagai. 1997. In vivo sequence variability of human immunodeficiency virus type 1 envelope gp120: association of V2 extension with slow disease progression. J. Virol. 71:4871-4881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spijkerman, I. J. B., M. Koot, M. Prins, I. P. M. Keet, A. J. A. R. van den Hoek, F. Miedema, and R. A. Coutinho. 1995. Lower prevalence and incidence of HIV-1 syncytium-inducing phenotype among injecting drug users compared with homosexual men. AIDS 9:1085-1092. [DOI] [PubMed] [Google Scholar]
- 49.Tersmette, M., J. M. A. Lange, R. E. Y. de Goede, F. de Wolf, J. K. M. Eeftinck Schattenkerk, P. T. A. Schellekens, R. A. Coutinho, J. G. Huisman, J. Goudsmit, and F. Miedema. 1989. Association between biological properties of human immunodeficiency virus variants and risk for AIDS and AIDS mortality. Lancet i:983-985. [DOI] [PubMed] [Google Scholar]
- 50.Trkola, A., W. A. Paxton, S. P. Monard, J. A. Hoxie, M. A. Siani, D. A. Thompson, L. Wu, C. R. Mackay, R. Horuk, and J. P. Moore. 1998. Genetic subtype-independent inhibition of human immunodeficiency virus type 1 replication by CC and CXC chemokines. J. Virol. 72:396-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Trkola, A., M. Purtscher, T. Muster, C. Ballaun, A. Buchacher, N. Sullivan, K. Srinivasan, J. Sodroski, J. P. Moore, and H. Katinger. 1996. Human monoclonal antibody 2G12 defines a distinctive neutralization epitope on the gp120 glycoprotein of human immunodeficiency virus type 1. J. Virol. 70:1100-1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tscherning, C., A. Alaeus, R. Fredriksson, A. Bjorndal, H. Deng, D. R. Littman, E. M. Fenyo, and J. Albert. 1998. Differences in chemokine coreceptor usage between genetic subtypes of HIV-1. Virology 241:181-188. [DOI] [PubMed] [Google Scholar]
- 53.Van Rij, R. P., and H. Schuitemaker. 2002. Host genetic factors in the clinical course of HIV-1 infection: chemokines and chemokine receptors. Community Genet. 5:88-101. [DOI] [PubMed] [Google Scholar]
- 54.Watkins, B. A., R. Crowley, A. E. Davis, A. T. Louie, and M. S. Reitz, Jr. 1997. Syncytium formation induced by human immunodeficiency virus type 1 isolates correlates with affinity for CD4. J. Gen. Virol. 78(Pt. 10):2513-2522. [DOI] [PubMed] [Google Scholar]
- 55.Wei, X., J. M. Decker, S. Wang, H. Hui, J. C. Kappes, X. Wu, J. F. Salazar-Gonzalez, M. G. Salazar, J. M. Kilby, M. S. Saag, N. L. Komarova, M. A. Nowak, B. H. Hahn, P. D. Kwong, and G. M. Shaw. 2003. Antibody neutralization and escape by HIV-1. Nature 422:307-312. [DOI] [PubMed] [Google Scholar]
- 56.Xiang, S. H., P. D. Kwong, R. Gupta, C. D. Rizzuto, D. J. Casper, R. Wyatt, L. Wang, W. A. Hendrickson, M. L. Doyle, and J. Sodroski. 2002. Mutagenic stabilization and/or disruption of a CD4-bound state reveals distinct conformations of the human immunodeficiency virus type 1 gp120 envelope glycoprotein. J. Virol. 76:9888-9899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang, Y. J., and J. P. Moore. 1999. Will multiple coreceptors need to be targeted by inhibitors of human immunodeficiency virus type 1 entry? J. Virol. 73:3443-3448. [DOI] [PMC free article] [PubMed] [Google Scholar]