Abstract
Pediatric urolithiasis has increased globally in the last few decades. There has been a change in the pattern of stone composition with an increase in the frequency of kidney stones and a decrease in bladder stones. The role of familial predisposition and environmental factors in pediatric urolithiasis is now better understood. Metabolic factors are more common in pediatric urolithiasis than in adult stone disease. This review updates on the epidemiology of pediatric urolithiasis with a focus on the changing trends in the stone disease, current spectrum of stone disease encountered in clinical practice, individual predisposition and the role of environmental factors in stone formation.
Keywords: Epidemiology, pediatric, prevalence, trends, urolithiasis
INTRODUCTION
Pediatric urolithiasis is an important kidney disorder encountered in clinical practice. There has been considerable regional variability in the reported incidences of urolithiasis. Also, there is a growing body of evidence demonstrating that the overall incidence of pediatric urolithiasis is increasing. A better understanding of different risk factors can help with risk stratification in an individual subject and can guide specific measures to prevent stone recurrence. This review focuses on the current state of knowledge on the prevalence of pediatric urolithiasis, temporal trends in stone disease and the status of different risk factors in stone formation. The risk factors for urolithiasis include an individual's susceptibility to form stones, such as genetic predisposition and metabolic abnormalities, and environmental factors that facilitate stone disease, such as dietary practices as well as local climate characteristics.
PREVALENCE OF UROLITHIASIS
Prevalence of urolithiasis varies in different countries. In adults, the prevalence is relatively higher in Western countries than in the Eastern hemisphere. The reported prevalence of urolithiasis increases from 1-5% in Asia, to 5-9% in Europe, 12% in Canada and 13- 15% in the USA, although even some Asian countries, such as Saudi Arabia, have a very high reported prevalence of 20.1%.[1,2] Children represent 2-3% of the total population of stone-formers.[3] Similar to the regional variability seen in adults, the prevalence of pediatric urolithiasis also varies in different parts of the world. In the USA, urolithiasis is said to be responsible for 1 in 7,600 to 1 in 1,000 pediatric hospital admissions.[4] In asymptomatic Turkish primary school children the prevalence of pediatric urolithiasis is reported to be 1%.[5] Urolithiasis contributed to 7% of general outpatient consultations in all children's hospitals in Venezuela during 1998.[6] In a hospital-based study from Ethiopia, 13% of admissions were due to urolithiaisis, and close to half of these admissions were in the age group of 0-19 years.[7] The prevalence might be higher than what hospital-based studies suggest, as subjects with asymptomatic stones may be missed. This point was highlighted by a 3.5% prevalence of X-ray-identified calcifications in the upper urinary tract in a cross-sectional study on 3398 randomly selected asymptomatic Scottish adults.[8]
The etiology of regional variability in urolithiasis is multi-factorial and may depend on local conditions and practices. In a nationwide survey from USA on 1,167,009 adults, the odds of stones among participants residing in Southeast USA were nearly double of those living in the Northwest states.[9] The risk of kidney stones in the USA increases from the West to East and from the North to South.[9] The region of the United States with a higher prevalence of kidney stones has been labeled the “stone belt” [also called the “kidney stone belt”]. The term “stone belt” dates back to at least 1976, and it applies to the region in the Southeast USA that includes Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia and Kentucky [Figure 1]. Similar regional variation was observed in an Italian study with a higher stone incidence in Southern Italy compared to the North of Italy.[10] The Afro-Asian stone belt stretches from Sudan, the Arab Republic of Egypt, Saudi Arabia, the United Arab Emirates, the Islamic Republic of Iran, Pakistan, India, Myanmar, Thailand, Indonesia to Philippines. Within a stone belt, the incidence of urolithiasis varies within the regions due to the local conditions and practices.
Figure 1.
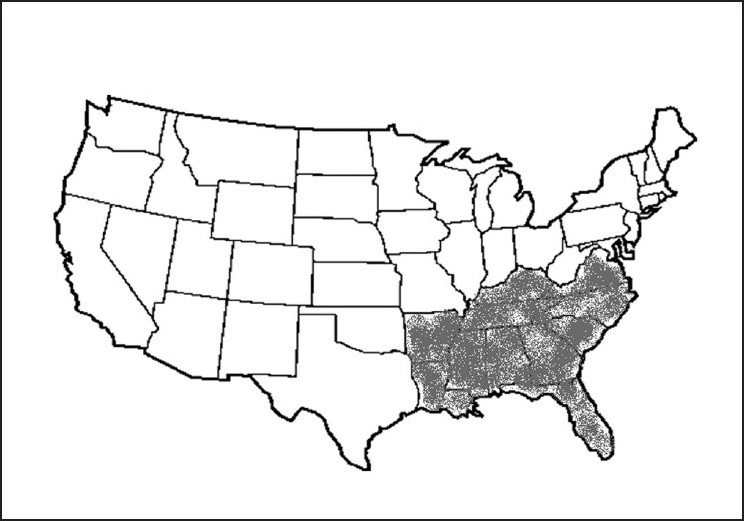
Stone belt in North America
TRENDS IN THE PREVALENCE AND PATTERN OF UROLITHIASIS
The epidemiologic studies have shown a progressive increase in the incidence of pediatric urolithiasis over the last few decades, referred to as a “stone wave”. An earlier study from 1951 did not find a single case of urolithiasis in 21,835 children at the Babies Hospital in New York.[11] In later studies from the 1960s and 1970s, urolithiasis in children increased steadily.[12–14] These studies reported the incidence of pediatric urolithiasis in the range of 1 in 6000, 1 in 7600 and 1 in 1850 hospitalized children.[12–14] This increase in stone incidence has become more pronounced in recent years. VanDervoort et al., reported a fivefold increase in the prevalence of pediatric urolithiasis in North American children in the last decade.[4] Similar trends were also observed in other countries. Annual pediatric referrals for urolithiasis in Turkey showed a fivefold increase in the last decade.[15] It cannot be ruled out that advances in imaging techniques contributed to the reported increase; however, the trend has also paralleled with improved socioeconomic conditions and increased consumption of a protein-rich diet.[16,17]
Pediatric urolithiasis has also shown a change in the pattern of stone composition and localization. At the beginning of the last century, bladder calculi, composed of ammonium urate were common in Europe; whereas over the past 100 years the pattern has changed to a higher frequency of calculi localized in the upper urinary tract. Moreover, calcium oxalate and calcium phosphate calculi became much more prevalent.[18] This change has been reported from both developed and developing countries.[15,19,20] Struvite stones have decreased in frequency and their occurrence has become limited to children with predisposed conditions such as obstructive uropathy and recurrent urinary tract infections. Bladder stones composed of ammonium urate and calcium still remain prevalent in malnourished children[7,18,21–23] and are more commonly reported in developing countries. Nonetheless, the pattern of pediatric urolithiasis in developing countries is now changing, which is similar to trend that was observed in the Western hemisphere over the last century.[18]
STONE COMPOSITION
Calcium oxalate is the most common stone worldwide, and accounts for 60-90% of pediatric urolithiasis.[4,15,17,19,20,24–28] Sturvite constitutes 1-18% of the stones in developed countries.[15,29] calcium phosphate accounts for 10-20% stones.[30] Uric acid constitutes 5-10%, cystine 1-5% [1 in 15000 live births] and mixed or miscellaneous 4% of the pediatric stones.[30,31] Cystine stones have a higher prevalence in endemic areas and in communities with high consanguinity. The reported prevalence of uncommon stone types could be an underestimation in many developing countries due to the unavailability of required diagnostic tools.[32]
METABOLIC RISK FACTORS
Pediatric urolithiasis requires a comprehensive metabolic evaluation to identify underlying risk factors. Metabolic risk factors increase the risk of stone recurrence.[31,33] The prevalence of metabolic risk factors ranged from less than 20% to greater than 50% in different studies.[15,17,33,34] Hypercalciuria and hypocitraturia are the common metabolic abnormalities, detected in one-third of the stone-formers.[4,15,34] The prevalence of hyperuricosuria and hyperoxaluria has been reported to be approximately 20%.[15,29]
Hypercalciuria
Hypercalciuria is defined as a urinary calcium excretion in excess of 0.1 mmol/kg per 24 h or 4 mg/kg per 24 h.[35] Hypercalciuria can be associated with elevated plasma calcium levels, as in primary hyperparathyroidism, or it can occur with normal serum calcium levels. Hypercalcemia-associated hypercalciuria needs further evaluation of the etiology of hypercalcemia. Normocalcemic hypercalciuria can be an isolated trait, referred to as idiopathic hypercalciuria, or it can have an associated abnormality such as renal tubular acidosis. The term idiopathic hypercalciuria was introduced by Albright and colleagues[36] to describe normocalcemic hypercalciuria without an obvious etiology. The defect in idiopathic hypercalciuria can be impaired renal tubular calcium reabsorption [renal hypercalciuria] or enhanced intestinal calcium absorption [absorptive hypercalciuria]. An overlap of the two mechanisms can also occur, although a differentiation does not change clinical management or prognosis. Calcium balance is negative in almost half the patients with idiopathic hypercalciuria, which can be associated with a reduced bone mineral density.[37,38] The pathogenesis of decreased bone mineral density in this condition is thought to be secondary to a combination of genetic factors, low calcium intake and altered cytokine production.[39] Idiopathic hypercalciuria is treated with a low-salt and high-fluid diet, potassium citrate supplementation and thiazide diuretics.
Hypocitraturia
Urinary citrate inhibits the crystal precipitation and raises the threshold for stone formation through the formation of chelate complexes with calcium. Hypocitraturia can be idiopathic or can be a manifestation of systemic metabolic acidosis, hypokalemia[40,41] or inflammatory bowel disease. Hypocitraturia is treated with potassium citrate supplementation.
Hyperoxaluria
Urinary oxalate is mainly derived from endogenous production of ascorbic acid and glyoxylate metabolism. In normal circumstances, only 10-15% of urinary oxalate originates from dietary intake. Food products with high oxalate content include coffee, tea, vegetables such as beans, canned tomatoes, cocoa and chocolate. The proportion of dietary oxalate increases in gastrointestinal conditions associated with fat malabsorption, inflammatory bowel disease or bowel resection. These conditions aggravate oxalate absorption either due to increased gut permeability or by decreased calcium availability for oxalate binding. Oxalate-rich or pyridoxine-deficient foods can also induce enteric hyperoxaluria. Hyperoxaluria due to an inborn error of metabolism is labeled as primary hyperoxaluria [oxalosis]. Two types of hyperoxaluria are differentiated: Type I and Type II. Type I hyperoxaluria is the more common of the two and it occurs in 1 per 120,000 live births. It is transmitted as an autosomal recessive trait. The genetic mutation leads to the defect in enzyme alanine glyoxylate aminotransferase [AGXT]. This enzyme defect leads to an increase in urinary oxalate, glyoxylic acid and glycolic acid. Type II hyperoxaluria is due to a defect in the D-glycerate dehydrogenase enzyme, and it is associated with an increase in urinary oxalate and L-glycerate levels. Low-oxalate, high-fluid and high-calcium diet, trial of pyridoxine supplementation and potassium citrate administration in the presence of low urinary citrate levels forms the cornerstone of therapy. Severe cases can require combined liver-kidney transplantation. It is important to note that a low-calcium diet can cause secondary hyperoxaluria.
Urinary tract infection
Urinary tract infection from urease-producing organisms can predispose to infection stones by splitting urea to ammonia and CO2. Ammonia preconditions to the formation of struvite and carbonate apatite stones in the presence of concomitant alkaline urine.[21] The association of pediatric urolithiasis with urinary tract infections is approximately 25%.[32] In pediatric urolithiasis, the prevalence of genitourinary anatomical abnormalities such as ureteropelvic junction obstruction and vesicoureteric reflux can range at 14- 30%.[17,31]
FAMILIAL AND INHERITED PREDISPOSITION
First-degree relatives of stone-formers have a 2-16 times higher risk of developing renal stones when compared with the general population.[42,43] In a stone-former, the probability of having a relative with stones may be as high as 35-65% as compared with a 5-20% probability in a non-stone-former.[43] It is important to understand that familial recurrence does not necessarily imply an inherited genetic cause. Shared environmental factors and common dietary habits can contribute to familial predisposition. After controlling for dietary pattern, genetic factors have also been recognized to play a significant role in urolithiasis.[44] The mode of inheritance for the genetic factors is largely considered to be polygenic.[45] Monogenic inheritance has been identified for relatively less common etiologies such as cystinuria, primary hyperoxaluria, and for selected etiologies of hypercalciuria such as Dent's disease [the association of low molecular weight proteinuria and hypercalciuria], Bartter syndrome Type V, autosomal dominant hypocalcemic hypercalciuria, familial hypomagnesemia with hypercalciuria and hypercalciuric nephrolithiasis with hypophosphatemia.[46]
Idiopathic hypercalciuria can have a familial predisposition or can occur in a sporadic form. Family history could be positive in up to 65% of patients with hypercalciuric nephrolithiaisis.[47] In familial forms, the pattern of transmission is found to be consistent with autosomal dominant inheritance.[48] Familial pattern has been reported for both absorptive hypercalciuria[48] and renal hypercalciuria.[49] In pedigree analyses, genetic defect was mapped to Chromosome 1q23.3-23.4[50] for human soluble adenylate cyclase gene;[51] Chromosome 12q12-q14 for vitamin D receptor [VDR] gene;[52] and to Chromosome 9q33.2-q34.2, from which an appropriate candidate gene remains to be identified.[53]
The role of genetic factors in oxalate handling has been the focus of a few studies. Recurrent idiopathic stone-formers have been reported to have a higher prevalence of anomalous erythrocyte transmembrane oxalate flux. In the affected families, the transmission pattern suggested an autosomal monogenetic trait, with complete penetration and a variable expressivity.[54] Hydrochlorothiazide and amiloride have been shown to restore the oxalate flux to normal.[54] The significance of oxalate flux in the clinical management of nephrolithiasis needs further evaluation.
ETHNICITY AND GENDER
Idiopathic stone disease has been reported to be more frequent in white Caucasians than in African-Americans from both adult and pediatric studies.[55] These differences are difficult to explain based simply on ethnicity. Decrease in ethnic disparity in the stone prevalence with the change in dietary pattern in African-Americans suggests a predominant role of environmental factors in the observed discrepancy.
With regard to gender distribution, males were found to be more susceptible for stones in some pediatric studies,[19] an observation not seen in other studies.[31]
DIETARY HABITS
Epidemiologic studies indicate a major role of diet in the pathogenesis of urolithiasis.
Both malnutrition and obesity increase the risk of urolithiasis.[10] The increase in the stone disease with malnutrition is associated with ammonium-urate stones in the bladder, whereas obesity predisposes to calcium-containing stones localized in the upper urinary tract. In obesity, insulin resistance has been associated with an increase in urinary calcium and decrease in renal tubular acid excretion.[56] Impaired renal tubular acid excretion lowers urinary citrate level and enhances the risk of stone precipitation.
Evidence supports a link between higher dietary animal protein and increase in stone incidence.[57] Protein consumption in children in Europe and North America is three to five times higher than the recommended intake.[58] The increase in dietary protein has been associated with an increase in calcium oxalate stones and higher localization of stones in the kidneys.[10,16,17] Diet low in animal protein but high in cereal shifts the spectrum towards a higher predominance of bladder stones composed of ammonium and urate ions, more commonly seen with malnutrition.[19,22]
The lithogenic potential of dietary protein is believed to be through different mechanisms. It results from a combination of a higher renal load of lithogenic substances, and a tendency towards their increased precipitation in the kidneys. Animal proteins are rich in sulfur-containing amino acids such as cystine and methionine. Oxidation of sulfur to sulfate generates acid load that aggravates calcium mobilization from bones.[59] High purine content in animal protein increases the uric acid burden. Urine oxalate level also increases with high protein intake.[60] High protein load increases glomerular filtration and facilitates a higher delivery of these substances to the urinary tract. Calcium forms soluble complex with sulfate generated from the oxidation of sulfur in proteins. Acid load increases calcium mobilization from the bones, and causes hypercalciuria and low urine citrate levels.[61]
Dietary sodium increases the risk of urolithiasis. Salt intake expands intravascular volume, which can increase urinary calcium level, likely by decreasing renal tubular calcium reabsorption.[62] Increase in salt intake can induce mild systemic metabolic acidosis, which can lower urinary citrate levels, and increases the risk of calcium precipitation in kidneys.[62]
On the contrary, potassium-rich foods lower stone formation through a decrease in urinary calcium excretion.[63] High urinary potassium is believed to increase renal tubular phosphate absorption and consequently inhibit 1, 25-dihydroxyvitamin synthesis.[64] Decrease in 1, 25-dihydroxy vitamin slows intestinal calcium absorption. Potassium-rich foods offer the additional advantage of high citrate content thus decreasing the precipitation of urinary calcium.[26]
Considering the key role of calcium in the pathogenesis of urolithiasis, the interaction between dietary calcium and the risk of urolithiasis has been controversial. High calcium concentration in calcium oxalate and calcium phosphate stones makes it sound intuitive that high dietary calcium will increase urinary calcium levels and the risk of calcium stones. On the other hand, a low-calcium diet can increase intestinal oxalate absorption and enhance the risk of calcium oxalate stones. This important question was addressed in a prospective study on 45,619 men, aged 40 to 75 years, with no history of kidney stones.[65] The risk of urolithiasis was found to be inversely related to dietary calcium intake.[65] With this evidence, dietary calcium restriction is no longer recommended. The implication of dietary calcium becomes even more significant in children, due to the importance of adequate calcium intake for growth and bone metabolism in the pediatric age group.
A carbohydrate-rich diet has been associated with an increase in urolithiasis in predisposed subjects. Glucose load can induce hypercalciuria, which is ascribed to decreased distal tubular calcium absorption and augmented intestinal calcium uptake.[66] High glucose can also increase the risk of urolithiasis through an increase in urinary oxalate levels.[67]
Climate and season
Parry and Lister were the first to propose that exposure to sunlight might influence stone formation after they observed an increase in urinary calcium among soldiers during summer but not in winter months.[36] In a large voluntary reported survey on 1,185,124 adults aged 30 years or older, ambient temperature and sunlight exposure was positively associated with stone prevalence after adjusting for other relevant variables.[9] Incidence of urinary stones tends to be higher in countries with warm or hot climates. Even within North America, the prevalence of stones becomes higher with an increase in average annual temperature [5.2°C in North Dakota to 22° in Florida] and sunlight index [14.6 in Washington state to 39.7 in Florida].[9] In a similar observation from Italy, the highest frequency of urolithiasis was found in Southern Italy and the lowest in Northern Italy.[10] Corresponding to high temperatures, stone recurrence becomes higher in summer and fall than in winter and spring.[17] The peak incidence of stone formation occurs in July, August, and September[9,25–33] in the Northern hemisphere.
The relationship between urolithiasis and high ambient temperature can be explained by intravascular volume contraction resulting from a combination of dehydration and inadequate fluid intake. Volume contraction increases urine concentration and promotes stone formation.[34,35] Higher sunlight exposure can also increase the production of 25-hydroxycholecalciferol in the skin, leading to an increase in 1, 25 dihydroxyvitamin D levels which augments intestinal calcium absorption. Elevated levels of circulating 1, 25 dihydroxyvitamin D have been found in patients with hypercalciuria.[37]
LOCAL FACTORS AFFECTING STONE FORMATION
Local factors have been reported to affect the regional distribution of pediatric urolithiasis.
Intestinal colonization of Oxalobacter formigenes [O. formigenes]
Deficient intestinal colonization of Oxalobacter formigenes [O. formigenes] in the North Indian population has been associated with a higher frequency of urolithiasis in the local population[68] O. formigenes is a Gram-negative, anaerobic bacterium that metabolizes oxalate in the intestinal tract and has a prevalence of 46-77% in different populations.[69] Deficient intestinal colonization of O. formigenes has been associated with increased risk of absorptive hyperoxaluria and calcium oxalate stones.[68]
The reasons for lower colonization of O. formigenes in certain populations are not well understood. Recent antibiotic administration and local practices of antibiotic use can affect O. formigenes colonization.[70] A study in Ukrainian children provided early insight into the natural history of O. formigenes.[69] O. formigenes was not detected in children younger than one year, had a prevalence of 100% [by polymerase chain reaction ; approximately 80% by culture] between ages six and eight, and dropped to approximately 75% at age 12.[69] Long-term pattern of O. formigenes colonization, loss and reacquisition of the bacterium over the course needs evaluation.
The use of O. formigenes as a probiotic is at an early stage of investigation. A preliminary trial on 16 patients showed a reduction in urinary or plasma oxalate in 11 patients with no adverse effects; however, none of the patients seemed to be permanently colonized during follow-up.[71]
Endemic prevalence of distal renal tubular acidosis
Higher prevalence of renal stones in Northeast Thailand has been attributed to the local endemicity of distal renal tubular acidosis [RTA].[66] Distal RTA induces systemic metabolic acidosis and increases the risk of urolithiasis by inducing hypercalciuria and hypocitraturia. Even in the absence of overt metabolic acidosis, intermittent and mild acidosis from incomplete distal RTA is capable of causing hypercalciuria and renal calculi.[61,72] In the presence of metabolic acidosis, hypercalciuria results from calcium mobilization from bones during acid buffering. Renal tubular acidification defects can also lower urinary citrate levels. Low urinary citrate concentration facilitates calcium precipitation in the kidneys. Correction of acidosis offers a therapeutic benefit in both complete and incomplete distal RTA.[73]
Exogenous substances
Melamine contamination in milk has been recently associated with nephrolithiasis in infants. After initial reports of nephrolithiasis among Chinese infants, attributed to milk-based formula surfaced in the summer of 2008, a systematic search by the Chinese Administration of Quality Supervision, Inspection, and Quarantine [AQSIQ] revealed 22 commercial brands of milk powder with detectable levels of melamine.[74] Melamine 1,3,5-triazine-2,4,6-triamine, or C3H6N6], a synthetic chemical developed in the 1830s, is used in a variety of inedible commercial products including cleaning supplies, dry erase boards, and other plastics and has widespread legitimate uses.[29] Melamine can increase non-protein nitrogen content and manufacturers added it to milk to meet quality control tests for protein-based nitrogen content.
The mechanism of melamine nephrotoxicity is not completely understood, although animal studies have provided some insight. Melamine can precipitate in distal renal tubules and forms intratubular green radial crystals which are distinct from calcium oxalate or calcium phosphate crystals.[75] Renal injury is believed to be secondary to an increase in intrarenal pressure resulting from crystal deposition in distal tubule leading to intratubular obstruction and distal tubular necrosis. Melamine stones are composed of melamine and its metabolite cyanuric acid with uric acid, protein and phosphate.[74] These stones are not fully radiopaque.
CONCLUSION
The incidence of urolithiasis in children has increased globally over the last few decades. The pattern of stone disease has also changed, with an increase in kidney stones secondary to calcium oxalate or calcium phosphate in the kidneys and a decrease in bladder stones composed of ammonium and urate. Evidence favors a significant role of dietary practices in the increase in pediatric urolithiasis. There are marked regional variations in the stone prevalence that has led to the recognition of ‘stone belts’. Local climatic conditions play an important role in the stone pathogenesis. Stone occurrence increases in warmer and sunnier regions. The individual risk of stone disease is modified by familial predisposition and genetic susceptibility. Metabolic workup is indicated in all children with a stone disease. Adequate water intake and maintaining a balanced diet are important to reduce the risk of kidney stones. At-risk subjects identified by metabolic workup can benefit by an intervention directed to the specific defect.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ramello A, Vitale C, Marangella M. Epidemiology of nephrolithiasis. J Nephrol. 2000;13:S45–50. [PubMed] [Google Scholar]
- 2.Lopez M, Hoppe B. History, epidemiology and regional diversities of urolithiasis. Pediatr Nephrol. 2010;25:49–59. doi: 10.1007/s00467-008-0960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwarz RD, Dwyer NT. Pediatric kidney stones: Long-term outcomes. Urology. 2006;67:812–16. doi: 10.1016/j.urology.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 4.VanDervoort K, Wiesen J, Frank R, Vento S, Crosby V, Chandra M, et al. Urolithiasis in pediatric patients: A single center study of incidence, clinical presentation and outcome. J Urol. 2007;177:2300–5. doi: 10.1016/j.juro.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Remzi D, Cakmak F, Erkan I. A study on the urolithiasis incidence in Turkish school-age children. J Urol. 1980;123:608. doi: 10.1016/s0022-5347(17)56063-2. [DOI] [PubMed] [Google Scholar]
- 6.Orta-Sibu N, Lopez M, Moriyon JC, Chavez JB. Renal diseases in children in Venezuela, South America. Pediatr Nephrol. 2002;17:566–9. doi: 10.1007/s00467-002-0892-4. [DOI] [PubMed] [Google Scholar]
- 7.Alemu MH. Pattern of urinary tract stone diseases in Mekelle, Ethiopia. Ethiop Med J. 2008;46:237–41. [PubMed] [Google Scholar]
- 8.Scott R. Prevalence of calcified upper urinary tract stone disease in a random population survey.Report of a combined study of general practitioners and hospital staff. Br J Urol. 1987;59:111–7. doi: 10.1111/j.1464-410x.1987.tb04799.x. [DOI] [PubMed] [Google Scholar]
- 9.Soucie JM, Coates RJ, McClellan W, Austin H, Thun M. Relation between geographic variability in kidney stones prevalence and risk factors for stones. Am J Epidemiol. 1996;143:487–95. doi: 10.1093/oxfordjournals.aje.a008769. [DOI] [PubMed] [Google Scholar]
- 10.Serio A, Fraioli A. Epidemiology of nephrolithiasis. Nephron. 1999;81:26–30. doi: 10.1159/000046295. [DOI] [PubMed] [Google Scholar]
- 11.Lattimer JK, Hubbard M. Pediatric urologic admissions. J Urol. 1951;66:289–93. doi: 10.1016/s0022-5347(17)74341-8. [DOI] [PubMed] [Google Scholar]
- 12.Bass HN, Emanuel B. Nephrolithiasis in childhood. J Urol. 1966;95:749–53. doi: 10.1016/S0022-5347(17)63533-X. [DOI] [PubMed] [Google Scholar]
- 13.Troup CW, Lawnicki CC, Bourne RB, Hodgson NB. Renal calculus in children. J Urol. 1972;107:306–7. doi: 10.1016/s0022-5347(17)61011-5. [DOI] [PubMed] [Google Scholar]
- 14.Malek RS, Kelalis PP. Pediatric nephrolithiasis. J Urol. 1975;113:545–51. doi: 10.1016/s0022-5347(17)59521-x. [DOI] [PubMed] [Google Scholar]
- 15.Alpay H, Ozen A, Gokce I, Biyikli N. Clinical and metabolic features of urolithiasis and microlithiasis in children. Pediatr Nephrol. 2009;24:2203–9. doi: 10.1007/s00467-009-1231-9. [DOI] [PubMed] [Google Scholar]
- 16.Yoshida O, Terai A, Ohkawa T, Okada Y. National trend of the incidence of urolithiasis in Japan from 1965 to 1995. Kidney Int. 1999;56:1899–904. doi: 10.1046/j.1523-1755.1999.00754.x. [DOI] [PubMed] [Google Scholar]
- 17.Sternberg K, Greenfield SP, Williot P, Wan J. Pediatric stone disease: An evolving experience. J Urol. 2005;174:1711–4. doi: 10.1097/01.ju.0000179537.36472.59. [DOI] [PubMed] [Google Scholar]
- 18.Trinchieri A. Epidemiology of urolithiasis. Arch Ital Urol Androl. 1996;68:203–49. [PubMed] [Google Scholar]
- 19.Rizvi SA, Naqvi SA, Hussain Z, Hashmi A, Hussain M, Zafar MN, et al. Pediatric urolithiasis: Developing nation perspectives. J Urol. 2002;168:1522–5. doi: 10.1016/S0022-5347(05)64509-0. [DOI] [PubMed] [Google Scholar]
- 20.Sarkissian A, Babloyan A, Arikyants N, Hesse A, Blau N, Leumann E. Pediatric urolithiasis in Armenia: A study of 198 patients observed from 1991 to 1999. Pediatr Nephrol. 2001;16:728–32. doi: 10.1007/s004670100647. [DOI] [PubMed] [Google Scholar]
- 21.Bichler KH, Eipper E, Naber K, Braun V, Zimmermann R, Lahme S. Urinary infection stones. Int J Antimicrob Agents. 2002;19:488–98. doi: 10.1016/s0924-8579(02)00088-2. [DOI] [PubMed] [Google Scholar]
- 22.Bakane BC, Nagtilak SB, Patil B. Urolithiasis: A tribal scenario. Indian J Pediatr. 1999;66:863–5. doi: 10.1007/BF02723855. [DOI] [PubMed] [Google Scholar]
- 23.Hassan I, Mabogunje OA. Urinary stones in children in Zaria. Ann Trop Paediatr. 1993;13:269–71. doi: 10.1080/02724936.1993.11747657. [DOI] [PubMed] [Google Scholar]
- 24.Biocic M, Saraga M, Kuzmic AC, Bahtijarevic Z, Budimir D, Todoric J, et al. Pediatric urolithiasis in Croatia. Coll Antropol. 2003;27:745–52. [PubMed] [Google Scholar]
- 25.Al-Eisa AA, Al-Hunayyan A, Gupta R. Pediatric urolithiasis in Kuwait. Int Urol Nephrol. 2002;33:3–6. doi: 10.1023/a:1014419830292. [DOI] [PubMed] [Google Scholar]
- 26.Srivastava T, Alon US. Urolithiasis in adolescent children. Adolesc Med Clin. 2005;16:87–109. doi: 10.1016/j.admecli.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 27.Coward RJ, Peters CJ, Duffy PG, Corry D, Kellett MJ, Choong S, et al. Epidemiology of paediatric renal stone disease in the UK. Arch Dis Child. 2003;88:962–5. doi: 10.1136/adc.88.11.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shah AM, Kalmunkar S, Punekar SV, Billimoria FR, Bapat SD, Deshmukh SS. Spectrum of pediatric urolithiasis in western India. Indian J Pediatr. 1991;58:543–9. doi: 10.1007/BF02750939. [DOI] [PubMed] [Google Scholar]
- 29.Milliner DS, Murphy ME. Urolithiasis in pediatric patients. Mayo Clin Proc. 1993;68:241–8. doi: 10.1016/s0025-6196(12)60043-3. [DOI] [PubMed] [Google Scholar]
- 30.Minevich E. Pediatric urolithiasis. Pediatr Clin North Am. 2001;48:1571–85. doi: 10.1016/s0031-3955(05)70392-8. [DOI] [PubMed] [Google Scholar]
- 31.Kit LC, Filler G, Pike J, Leonard MP. Pediatric urolithiasis: Experience at a tertiary care pediatric hospital. Can Urol Assoc J. 2008;2:381–6. doi: 10.5489/cuaj.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Petrarulo M, Vitale C, Facchini P, Marangella M. Biochemical approach to diagnosis and differentiation of primary hyperoxalurias: An update. J Nephrol. 1998;11:23–8. [PubMed] [Google Scholar]
- 33.Pietrow PK, Pope JCt, Adams MC, Shyr Y, Brock JW., 3rd Clinical outcome of pediatric stone disease. J Urol. 2002;167:670–3. doi: 10.1016/S0022-5347(01)69121-3. [DOI] [PubMed] [Google Scholar]
- 34.Nicoletta JA, Lande MB. Medical evaluation and treatment of urolithiasis. Pediatr Clin North Am. 2006;53:479–91. doi: 10.1016/j.pcl.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Curhan GC, Willett WC, Speizer FE, Stampfer MJ. Twenty-four-hour urine chemistries and the risk of kidney stones among women and men. Kidney Int. 2001;59:2290–8. doi: 10.1046/j.1523-1755.2001.00746.x. [DOI] [PubMed] [Google Scholar]
- 36.Albright F, Henneman P, Benedict PH, Forbes AP. Idiopathic hypercalciuria: A preliminary report. Proc R Soc Med. 1953;46:1077–81. [PMC free article] [PubMed] [Google Scholar]
- 37.Garcia-Nieto V, Ferrandez C, Monge M, de Sequera M, Rodrigo MD. Bone mineral density in pediatric patients with idiopathic hypercalciuria. Pediatr Nephrol. 1997;11:578–83. doi: 10.1007/s004670050341. [DOI] [PubMed] [Google Scholar]
- 38.Freundlich M, Alonzo E, Bellorin-Font E, Weisinger JR. Reduced bone mass in children with idiopathic hypercalciuria and in their asymptomatic mothers. Nephrol Dial Transplant. 2002;17:1396–401. doi: 10.1093/ndt/17.8.1396. [DOI] [PubMed] [Google Scholar]
- 39.Zerwekh JE. Bone disease and hypercalciuria in children. Pediatr Nephrol. 2010;25:395–401. doi: 10.1007/s00467-009-1338-z. [DOI] [PubMed] [Google Scholar]
- 40.Sharma RK, Sharma AP, Kapoor R, Gupta A. Prognostic significance of distal renal tubular acidosis in posterior urethral valve. Pediatr Nephrol. 2001;16:581–5. doi: 10.1007/s004670100590. [DOI] [PubMed] [Google Scholar]
- 41.Sharma RK, Sharma AP, Kapoor R, Pandey CM, Gupta A. Prognostic factors for persistent distal renal tubular acidosis after surgery for posterior urethral valve. Am J Kidney Dis. 2001;38:488–93. doi: 10.1053/ajkd.2001.26832. [DOI] [PubMed] [Google Scholar]
- 42.Trinchieri A, Mandressi A, Luongo P, Coppi F, Pisani E. Familial aggregation of renal calcium stone disease. J Urol. 1988;139:478–81. doi: 10.1016/s0022-5347(17)42497-9. [DOI] [PubMed] [Google Scholar]
- 43.Resnick M, Pridgen DB, Goodman HO. Genetic predisposition to formation of calcium oxalate renal calculi. N Engl J Med. 1968;278:1313–38. doi: 10.1056/NEJM196806132782403. [DOI] [PubMed] [Google Scholar]
- 44.Goldfarb DS, Fischer ME, Keich Y, Goldberg J. A twin study of genetic and dietary influences on nephrolithiasis: A report from the Vietnam Era Twin [VET] Registry. Kidney Int. 2005;67:1053–61. doi: 10.1111/j.1523-1755.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 45.Griffin DG. A review of the heritability of idiopathic nephrolithiasis. J Clin Pathol. 2004;57:793–6. doi: 10.1136/jcp.2003.014886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stechman MJ, Loh NY, Thakker RV. Genetic causes of hypercalciuric nephrolithiasis. Pediatr Nephrol. 2009;24:2321–32. doi: 10.1007/s00467-008-0807-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frick KK, Bushinsky DA. Molecular mechanisms of primary hypercalciuria. J Am Soc Nephrol. 2003;14:1082–95. doi: 10.1097/01.asn.0000062960.26868.17. [DOI] [PubMed] [Google Scholar]
- 48.Nicolaidou P, Themeli S, Karpathios T, Georgouli H, Athanassaki K, Xaidara A, et al. Family pattern of idiopathic hypercalciuria and its subtypes. J Urol. 1996;155:1042–4. [PubMed] [Google Scholar]
- 49.Harangi F, Mehes K. Family investigations in idiopathic hypercalciuria. Eur J Pediatr. 1993;152:64–8. doi: 10.1007/BF02072519. [DOI] [PubMed] [Google Scholar]
- 50.Reed BY, Heller HJ, Gitomer WL, Pak CY. Mapping a gene defect in absorptive hypercalciuria to chromosome 1q23.3-q24. J Clin Endocrinol Metab. 1999;84:3907–13. doi: 10.1210/jcem.84.11.6155. [DOI] [PubMed] [Google Scholar]
- 51.Reed BY, Gitomer WL, Heller HJ, Hsu MC, Lemke M, Padalino P, et al. Identification and characterization of a gene with base substitutions associated with the absorptive hypercalciuria phenotype and low spinal bone density. J Clin Endocrinol Metab. 2002;87:1476–85. doi: 10.1210/jcem.87.4.8300. [DOI] [PubMed] [Google Scholar]
- 52.Scott P, Ouimet D, Valiquette L, Guay G, Proulx Y, Trouve ML, et al. Suggestive evidence for a susceptibility gene near the vitamin D receptor locus in idiopathic calcium stone formation. J Am Soc Nephrol. 1999;10:1007–13. doi: 10.1681/ASN.V1051007. [DOI] [PubMed] [Google Scholar]
- 53.Wolf MT, Zalewski I, Martin FC, Ruf R, Muller D, Hennies HC, et al. Mapping a new suggestive gene locus for autosomal dominant nephrolithiasis to chromosome 9q33.2-q34.2 by total genome search for linkage. Nephrol Dial Transplant. 2005;20:909–14. doi: 10.1093/ndt/gfh754. [DOI] [PubMed] [Google Scholar]
- 54.Baggio B, Gambaro G, Marchini F, Cicerello E, Tenconi R, Clementi M, et al. An inheritable anomaly of red-cell oxalate transport in “primary” calcium nephrolithiasis correctable with diuretics. N Engl J Med. 1986;314:599–604. doi: 10.1056/NEJM198603063141002. [DOI] [PubMed] [Google Scholar]
- 55.Michaels EK, Nakagawa Y, Miura N, Pursell S, Ito H. Racial variation in gender frequency of calcium urolithiasis. J Urol. 1994;152:2228–31. doi: 10.1016/s0022-5347(17)31648-8. [DOI] [PubMed] [Google Scholar]
- 56.Abate N, Chandalia M, Cabo-Chan AV, Jr, Moe OW, Sakhaee K. The metabolic syndrome and uric acid nephrolithiasis: Novel features of renal manifestation of insulin resistance. Kidney Int. 2004;65:386–92. doi: 10.1111/j.1523-1755.2004.00386.x. [DOI] [PubMed] [Google Scholar]
- 57.Curhan GC. Dietary calcium, dietary protein, and kidney stone formation. Miner Electrolyte Metab. 1997;23:261–4. [PubMed] [Google Scholar]
- 58.Prentice A, Branca F, Decsi T, Michaelsen KF, Fletcher RJ, Guesry P, et al. Energy and nutrient dietary reference values for children in Europe: Methodological approaches and current nutritional recommendations. Br J Nutr. 2004;92:S83–146. doi: 10.1079/bjn20041159. [DOI] [PubMed] [Google Scholar]
- 59.Arnett TR. Extracellular pH regulates bone cell function. J Nutr. 2008;138:415S–8. doi: 10.1093/jn/138.2.415S. [DOI] [PubMed] [Google Scholar]
- 60.Holmes RP, Goodman HO, Hart LJ, Assimos DG. Relationship of protein intake to urinary oxalate and glycolate excretion. Kidney Int. 1993;44:366–72. doi: 10.1038/ki.1993.253. [DOI] [PubMed] [Google Scholar]
- 61.Sharma AP, Sharma RK, Kapoor R, Kornecki A, Sural S, Filler G. Incomplete distal renal tubular acidosis affects growth in children. Nephrol Dial Transplant. 2007;22:2879–85. doi: 10.1093/ndt/gfm307. [DOI] [PubMed] [Google Scholar]
- 62.Sakhaee K, Harvey JA, Padalino PK, Whitson P, Pak CY. The potential role of salt abuse on the risk for kidney stone formation. J Urol. 1993;150:310–2. doi: 10.1016/s0022-5347(17)35468-x. [DOI] [PubMed] [Google Scholar]
- 63.Osorio AV, Alon US. The relationship between urinary calcium, sodium, and potassium excretion and the role of potassium in treating idiopathic hypercalciuria. Pediatrics. 1997;100:675–81. doi: 10.1542/peds.100.4.675. [DOI] [PubMed] [Google Scholar]
- 64.Jaeger P, Bonjour JP, Karlmark B, Stanton B, Kirk RG, Duplinsky T, et al. Influence of acute potassium loading on renal phosphate transport in the rat kidney. Am J Physiol. 1983;245:F601–5. doi: 10.1152/ajprenal.1983.245.5.F601. [DOI] [PubMed] [Google Scholar]
- 65.Curhan GC, Willett WC, Rimm EB, Stampfer MJ. A prospective study of dietary calcium and other nutrients and the risk of symptomatic kidney stones. N Engl J Med. 1993;328:833–8. doi: 10.1056/NEJM199303253281203. [DOI] [PubMed] [Google Scholar]
- 66.Vasuvattakul S, Nimmannit S, Chaovakul V, Susaengrat W, Shayakul C, Malasit P, et al. The spectrum of endemic renal tubular acidosis in the northeast of Thailand. Nephron. 1996;74:541–7. doi: 10.1159/000189449. [DOI] [PubMed] [Google Scholar]
- 67.Schwille PO, Hanisch E, Scholz D. Postprandial hyperoxaluria and intestinal oxalate absorption in idiopathic renal stone disease. J Urol. 1984;132:650–5. doi: 10.1016/s0022-5347(17)49808-9. [DOI] [PubMed] [Google Scholar]
- 68.Kumar R, Mukherjee M, Bhandari M, Kumar A, Sidhu H, Mittal RD. Role of Oxalobacter formigenes in calcium oxalate stone disease: A study from North India. Eur Urol. 2002;41:318–22. doi: 10.1016/s0302-2838(02)00040-4. [DOI] [PubMed] [Google Scholar]
- 69.Sidhu H, Enatska L, Ogden S, Williams WN, Allison MJ, Peck AB. Evaluating Children in the Ukraine for Colonization With the Intestinal Bacterium Oxalobacter formigenes, Using a Polymerase Chain Reaction-based Detection System. Mol Diagn. 1997;2:89–97. doi: 10.1054/MODI00200089. [DOI] [PubMed] [Google Scholar]
- 70.Duncan SH, Richardson AJ, Kaul P, Holmes RP, Allison MJ, Stewart CS. Oxalobacter formigenes and its potential role in human health. Appl Environ Microbiol. 2002;68:3841–7. doi: 10.1128/AEM.68.8.3841-3847.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hoppe B, Beck B, Gatter N, von Unruh G, Tischer A, Hesse A, et al. Oxalobacter formigenes: A potential tool for the treatment of primary hyperoxaluria type 1. Kidney Int. 2006;70:1305–11. doi: 10.1038/sj.ki.5001707. [DOI] [PubMed] [Google Scholar]
- 72.Konnak JW, Kogan BA, Lau K. Renal calculi associated with incomplete distal renal tubular acidosis. J Urol. 1982;128:900–2. doi: 10.1016/s0022-5347(17)53268-1. [DOI] [PubMed] [Google Scholar]
- 73.Sharma AP, Singh RN, Yang C, Sharma RK, Kapoor R, Filler G. Bicarbonate therapy improves growth in children with incomplete distal renal tubular acidosis. Pediatr Nephrol. 2009;24:1509–16. doi: 10.1007/s00467-009-1169-y. [DOI] [PubMed] [Google Scholar]
- 74.Ingelfinger JR. Melamine and the global implications of food contamination. N Engl J Med. 2008;359:2745–8. doi: 10.1056/NEJMp0808410. [DOI] [PubMed] [Google Scholar]
- 75.Brown CA, Jeong KS, Poppenga RH, Puschner B, Miller DM, Ellis AE, et al. Outbreaks of renal failure associated with melamine and cyanuric acid in dogs and cats in 2004 and 2007. J Vet Diagn Invest. 2007;19:525–31. doi: 10.1177/104063870701900510. [DOI] [PubMed] [Google Scholar]


