Abstract
Nephrolithiasis in the pediatric population is an important cause of morbidity worldwide. Presenting signs and symptoms are often considerably different from those in adults. Vague abdominal pain, hematuria, and urinary tract infection are more common in children than the classic colicky flank pain. Imaging of suspected cases should be undertaken with careful consideration of diagnostic accuracy and the potentially harmful effects of ionizing radiation. Because children with nephrolithiasis have a high chance of recurrent stone formation, a thorough risk assessment and metabolic evaluation should be performed. This review discusses the presentation, acute evaluation and risk assessment of nephrolithiasis in the pediatric population.
Keywords: Kidney, metabolic, nephrolithiasis, pediatric, renal stone, urolithiasis
INTRODUCTION
Nephrolithiasis is an important cause of morbidity worldwide. While the exact incidence of kidney stone disease in children is unknown, in the United States stones are the reason for 1 out of every 1000-7500 pediatric hospital admissions.[1,2] Consequences of nephrolithiasis include pain, infection, and renal damage that can contribute to renal failure in severe cases. Bladder stones occur in less than 10% of North American children, however they are endemic in other regions as a result of dietary and other factors.[3] Anatomic abnormalities such as ureteropelvic junction (UPJ) obstruction or ureterovesical junction (UVJ) obstruction are found on workup of nephrorolithiasis in 11-24% of children.[4–6] The strong male predominance[6–8] seen in the adult population is less clear in children, with more recent studies suggesting a roughly equal gender distribution,[9,10] or even a female predominance.[11] While nephrolithiasis can occur in any pediatric age group, infants represent roughly 20% of pediatric stone cases and tend to have a distinct history and presentation.[12] We will discuss the acute evaluation of children with suspected nephrolithiasis, as well as the subsequent metabolic workup.
ACUTE EVALUATION
Presentation
The presentation of nephrolithiasis in children differs significantly from that in adults. The classic unilateral colicky flank pain occurs in only about 7% of cases. Instead, abdominal pain is most common, occurring in 53-75% and gross hematuria in 14-33%.[2,6,8,13,14] Urinary tract infection (UTI) is also common, affecting 8-45.9% of children with nephrolithiasis.[4,5,15] In the case of children under five years of age, UTI or incidental radiologic findings most often lead to the diagnosis; UTI occurs in 62% of this age group.[15,16] Furthermore, if one considers only infants, UTI may be the presenting sign up to 75% of the time.[12,16] As in adults, it is particularly important to recognize the combination of an obstructing stone and UTI as this clinical scenario can quickly lead to sepsis.
Laboratory Studies
Urinalysis should be performed in any child in whom nephrolithiasis is suspected. Microhematuria is the most common abnormality, found in 60-95%.[17–19] Pyuria is found in only 20%.[17] Urinary leukocyte esterase and nitrites may be detected if there is an associated UTI, but these have low sensitivity (particularly urinary nitrites). Blood cell counts and urine cultures should be performed if the child presents with fevers, dysuria or other signs of infection.
Imaging
The imaging evaluation of nephrolithiasis in pediatric patients presents several unique issues. Although plain abdominal radiographs may detect stones, the sensitivity is low (30-60%).[20–22] In adults, the gold standard for diagnosis of nephrolithiasis is the non-contrast spiral computed tomography (CT) scan. Multiple studies have verified the optimal sensitivity and specificity of this study as compared to ultrasound (US) or intravenous pyelography (IVP).[23–25] In pediatric patients the superior diagnostic capability of CT has similarly been verified.[26–28] However, the diagnostic advantages of CT must be considered against the substantial dose of radiation, as children are 3 to 10 times more radiosensitive than adults.[29–31] Furthermore, cost and availability may be a limiting factor for CT in some settings.[25] Long-term risks of radiation exposure in children are not completely understood; however, it has been estimated that a single abdominal CT in a one-year-old imparts a 1 in 550 risk of subsequent lethal tumor development.[32] In light of such concerns, and often-ambiguous presentation in pediatric patients, the initial choice of imaging should be made with the goal of accurate diagnosis while minimizing risk of radiation exposure.
Recently, there has been interest in development of low-dose CT techniques for use in the diagnosis of renal stones. By modification of scanner settings, the ionizing radiation dose delivered can be reduced by 50-80% with minimal loss of diagnostic accuracy.[33,34] While these modifications are appropriate for stone diagnosis, they may result in a reduced accuracy for other abdominal pathology. Since CT is often obtained in children with vague presenting signs and symptoms to evaluate for non-urologic conditions (e.g. appendicitis), the ultimate role of low-dose CT in the diagnostic algorithm for urolithiasis remains unclear.
Prior to CT, IVU was the most accurate imaging study for urolithiasis. Its use has fallen off because it has inferior accuracy compared to CT (specificity is comparable, but the sensitivity is significantly lower),[25,34] and also has the disadvantage of requiring intravenous contrast administration.[26,34] However, IVU may detect radiolucent stones missed by conventional abdominal plain films, and remains a reasonable option where CT and US availability is limited.
Given concerns over radiation exposure in children, US is the modality of choice for initial imaging in pediatric patients who present with findings consistent with nephrolithiasis. US boasts a high sensitivity for renal stones (up to 90%), although sensitivity for ureteral stones is lower (44-90%).[23,25,27,35,36] Despite such limitations, US is a useful first test in those children in whom stones are suspected. If stones are not seen on US but suspicion remains high (e.g., hydroureteronephrosis is present), proceeding to CT is reasonable.
When evaluating for urolithiasis in children, practitioners need to be aware of misleading findings on imaging related to prior treatment of vesicoureteral reflux (VUR). Endoscopically injected dextranomer/hyaluronic acid co-polymer (Deflux®,Q-med) has been found to calcify and result in a hyperdense focus on CT in up to 36% of cases.[37,38] These high-density lesions on CT and US examinations have the potential to be misdiagnosed as urolithiasis.[38,39] A history of surgical treatment for VUR should alert the practitioner to the possibility of this finding. If a high-density focus is found, concomitant hydroureteronephrosis may help distinguish true urolithiasis from calcified implants.[37]
RISK EVALUATION
Predisposing factors can be identified in up to 87% of children with urolithiasis and recurrent stone disease occurs in 67% of pediatric patients.[2,40] For these reasons, all children who are found to have nephrolithiasis should have a complete evaluation of potential risk factors. The first step in the evaluation of pediatric patients for their risk of recurrent urolithiasis is a detailed history. Specific attention should be directed towards any family history of stone disease, renal dysfunction, gout, or arthritis. There is a increased risk of recurrent urolithiasis when individuals have first-degree relatives with hypercalciuria and prior kidney stone diagnosis.[41] In addition to familial factors, a careful dietary history is essential, particularly with regard to protein, sodium, calcium, and oxalate intake.[3] Imaging studies should be reviewed to examine for anatomic abnormalities. However, since most patients with anatomic abnormalities do not develop stones, a full metabolic workup is still warranted, even when such abnormalities are encountered.[3] Interestingly, there is evidence to suggest that specific metabolic abnormalities such as hypercalciuria may be independently associated with UPJ obstruction.[42]
METABOLIC EVALUATION
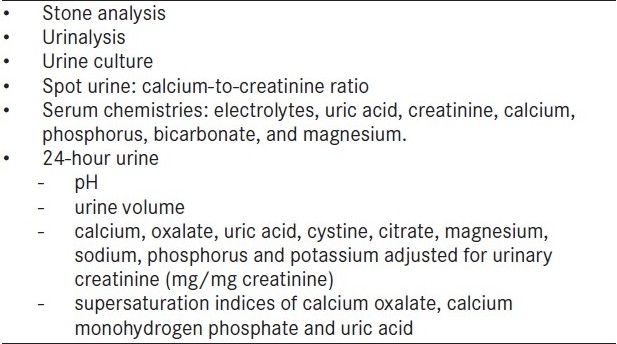
The goals of the metabolic evaluation for urolithiasis are to identify children at increased risk for recurrent stone disease and to diagnose specific treatable metabolic derangements. If stones have been surgically removed or isolated from strained urine during spontaneous passage, compositional analysis is helpful to guide the workup and to determine the underlying pathologic processes. In addition to verifying the major molecular components, compositional analysis can define mixed stone types and the specific forms (e.g., calcium oxalate monohydrate versus calcium oxalate dihydrate). Spot urine and serum testing is combined with 24-h urine analysis to comprehensively assess a child′s metabolic risk for recurrent stone disease. The complete metabolic evaluation for stone disease in the pediatric population is presented in Table 1 and individual components are discussed below.
Table 1.
Metabolic evaluation of pediatric nephrolithiasis
URINALYSIS/CULTURE
A spot urine sample is limited in its ability to evaluate metabolic risk but may provide useful information. The urine pH can suggest the types of crystals that are most likely to form. A low urine pH, for example, may be associated with uric acid stones. A high pH raises the possibility of infection stones, as well as possible renal tubular acidosis. It is important to remember that urine pH varies over the course of the day and a single measurement may only be valid for a specific time point. Microscopic urinalysis may identify distinctive crystal structure, such as the flat hexagonal crystals formed by cystine stones. Urinary leukocytes, nitrites, and leukocyte esterase may suggest the presence of infection. A urine culture should be obtained simultaneously to properly investigate bacterial colonization of the urinary tract. A calcium-to-creatinine ratio can be derived from a single specimen and is often used as an initial screening test for hypercalciuria. If hypercalciuria is suspected based on a random spot sample (ratio >0.2, although infants and toddlers may have higher values normally), this should be confirmed with a 24-h urine collection.[43] If cystiunuria is suspected, a nitroprusside test can verify the presence of cystine.[44]
SERUM TESTING
Serum studies are typically not as informative as urine studies, but may provide useful information and are necessary for interpretation of urine test results. Serum creatinine can identify renal insufficiency and is used to calculate the expected excretion of creatinine in a given urine sample. Bicarbonate and pH levels can help diagnose and classify renal tubular acidosis. Serum calcium, albumin and phosphate levels are used to evaluate for hypercalcemic conditions. If abnormal, specific investigation of parathyroid function (i.e. PTH) should be obtained. Irregularities of serum potassium and magnesium can be associated with abnormalities of urinary stone inhibitors.[44] Elevated serum urate levels are found with abnormalities in the metabolism of purines.
24-H URINALYSIS
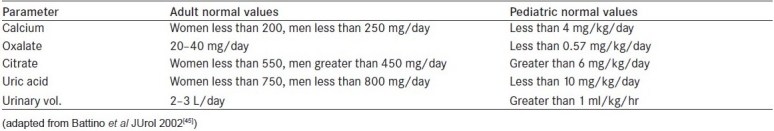
In addition to spot urine and serum tests, a formal 24-h urine collection is essential to the determination of stone-forming risk. Because of variation in diet and fluid intake, results from two separate 24-h urine collections, ideally six weeks after the patient achieves a stone-free status, should be used to guide treatment. To ensure that there is a complete 24-h collection of urine, a total creatinine should be greater than 15-20 mg/kg. When interpreting 24-h urine results, it is important to remember that adult reference values are not necessarily applicable to the pediatric population.[45,46] Borawski et al., measured standard urinary risk factors in 46 healthy children without a history of stones.[46] After adjusting for urinary creatinine and body weight, multiple metabolic parameters including oxalate, uric acid, citrate, magnesium, sodium, phosphorus and potassium significantly decreased with increasing age. Table 2 lists several standard urinary parameters with known pediatric reference ranges.[45] In addition to the concentrations of individual components, the supersaturation indices are especially useful to quantify crystallization potential.[47]
Table 2.
Adult and pediatric reference values for 24-hour urinalysis
Recent investigations into stone-forming risk have resulted in the Bonn risk index (BRI) which may better predict recurrent calcium oxalate stone formation.[48,49] The BRI is the ratio of ionized urinary calcium to the amount of ammonium oxalate required to induce calcium oxalate crystallization in 200 ml of urine. This ratio remains relatively stable in children across age and sex. BRI values in children with renal stones are 15-fold higher when compared to healthy children. Future research on the BRI is required to define its potential as a predictor of stone formation in asymptomatic children.
Perhaps the single most significant finding on a 24-h urine collection is the total volume. Pediatric stone-formers tend to have vastly insufficient oral fluid intake, and this may be the single most important factor in stone formation and recurrence. Low volumes documented on a 24-h urine (<1 mL/kg/hour) may serve as evidence of poor intake and may facilitate a discussion with families of the need to aggressively increase fluid intake throughout the day.
SPECIFIC METABOLIC FINDINGS
Hypercalciuria
Hypercalciuria is the most common cause of stones in children, representing up to 50% of the metabolic risk factors identified during evaluation.[50,51] Defined as a urinary calcium excretion of more than 4 mg/kg/day, it is found in as many as 4% of healthy children.[52] DeFoor et al., compared 24-h urine parameters children, and found that recurrent stone-formers have significantly higher calcium levels than first-time stone patients.[53] Most of the causes of hypercalciuria are idiopathic, both sporadic or familial.[54] Elevated vitamin D has been implicated in some cases of hypercalciuria; however, up to half of patients with idiopathic hypercalciuria have normal levels.[55] Alternatively, an increased number of vitamin D receptors may be responsible for hypercalciuria in certain patients. Other causes of hypercalciuria include distal renal tubular acidosis, medullary sponge kidney, and the use of medications such as adrenocorticotropic hormone (ACTH), loop diuretics, theophylline, and corticosteroids.
Most children with hypercalciuria have a normal serum calcium.[18] However, in those with hypercalcemia, specific conditions should be considered: primary hyperparathyroidism, immobilization, hypo- or hyperthyroidism, adrenocorticosteroid excess (endogenous or exogenous), adrenal insufficiency, osteolytic metastases, idiopathic hypercalcemia of infancy, sarcoidosis, hypervitaminosis D, milk alkali syndrome, Williams syndrome, and, rarely, mutations of the calcium-sensing receptor.
Hyperoxaluria
Hyperoxaluria, seen in up to 20% of children with nephrolithiasis, is most commonly caused by idiopathic hyperoxaluria with mild elevations of urinary oxalate levels.[3] Foods high in oxalate include beet and turnip greens, rhubarb, strawberries, star fruit, sweet potatoes, wheat bran, tea, cocoa, pepper, chocolate, parsley, beets, spinach, dill, nuts and citrus juices. Fat malabsorption can increase dietary oxalate via colonic hyperabsorption. The malabsorbed fatty acids displace luminal calcium from oxalate allowing increased absorption. More rarely, Type 1 primary hyperoxaluria (an autosomal recessive disease) causes a severe phenotype characterized by recurrent calcium oxalate urolithiasis, nephrocalcinosis and extrarenal tissue oxalate deposition.[3]
Hyperuricosuria
Hyperuricosuria has been found in 2-10% of children who are metabolically predisposed to kidney stone formation.[54] Most patients with hyperuricosuria also have hypercalciuria; calcium oxalate urolithiasis may be coexistent. Children with the familial or idiopathic form of the disease tend to have normal serum uric acid concentrations. Overproduction of uric acid may also occur secondary to inborn errors of metabolism, myeloproliferative disorders or a ketogenic diet. Overall, however, uric acid stones are uncommon in the pediatric population.
Cystinuria
Cystine stones comprise approximately 6% of the stones in the pediatric population. Stones result from elevated urinary excretion of cystine (cystinuria) caused by an autosomal recessive disorder of renal tubular transport, occurring in 1 in 15,000 live births.[3] It is characterized by failure of the renal tubules to reabsorb four basic amino acids: cystine, ornithine, lysine and arginine. Cystine is poorly soluble at acidic pH, and at urine pH of less than 7.0 cystine will precipitate and form stones. Patients with cystinuria are characteristically lifelong stone-formers.
CONCLUSIONS
The evaluation of nephrolithiasis in children differs from that of adults. The non-classical and often vague presentation requires a high level of clinical suspicion. Imaging must be undertaken with care to identify stones while avoiding excess radiation exposure. Because of the prevalence of metabolic risk factors and the significant risk of recurrence in this population, all children require a complete evaluation with metabolic workup.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Walther PC, Lamm D, Kaplan GW. Pediatric urolithiases: a ten-year review. Pediatrics. 1980;65:1068–72. [PubMed] [Google Scholar]
- 2.Milliner DS, Murphy ME. Urolithiasis in pediatric patients. Mayo Clin Proc. 1993;68:241–8. doi: 10.1016/s0025-6196(12)60043-3. [DOI] [PubMed] [Google Scholar]
- 3.Nicoletta JA, Lande MB. Medical evaluation and treatment of urolithiasis. Pediatr Clin North Am. 2006;53:479–91. doi: 10.1016/j.pcl.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Dursun I, Poyrazoglu HM, Dusunsel R, Gunduz Z, Gurgoze MK, Demirci D, et al. Pediatric urolithiasis: an 8-year experience of single centre. Int Urol Nephrol. 2008;40:3–9. doi: 10.1007/s11255-007-9234-6. [DOI] [PubMed] [Google Scholar]
- 5.Sternberg K, Greenfield SP, Williot P, Wan J. Pediatric stone disease: an evolving experience. J Urol. 2005;174:1711–4. doi: 10.1097/01.ju.0000179537.36472.59. [DOI] [PubMed] [Google Scholar]
- 6.Tekin A, Tekgul S, Atsu N, Sahin A, Ozen H, Bakkaloglu M. A study of the etiology of idiopathic calcium urolithiasis in children: hypocitruria is the most important risk factor. J Urol. 2000;164:162–5. [PubMed] [Google Scholar]
- 7.Ozokutan BH, Küçükaydin M, Gündüz Z, Kabaklioğlu M, Okur H, Turan C. Urolithiasis in childhood. Pediatr Surg Int. 2000;16:60–3. doi: 10.1007/s003830050016. [DOI] [PubMed] [Google Scholar]
- 8.Smith SL, Somers JM, Broderick N, Halliday K. The role of the plain radiograph and renal tract ultrasound in the management of children with renal tract calculi. Clin Radiol. 2000;55:708–10. doi: 10.1053/crad.2000.0501. [DOI] [PubMed] [Google Scholar]
- 9.Reisiger K, Vardi I, Yan Y, Don S, Coplen D, Austin P, et al. Pediatric nephrolithiasis: does treatment affect renal growth? Urology. 2007;69:1190–4. doi: 10.1016/j.urology.2007.01.072. [DOI] [PubMed] [Google Scholar]
- 10.Pietrow PK, Pope JC, 4th, Adams MC, Shyr Y, Brock JW., 3rd Clinical outcome of pediatric stone disease. J Urol. 2002;167:670–3. doi: 10.1016/S0022-5347(01)69121-3. [DOI] [PubMed] [Google Scholar]
- 11.Novak TE, Lakshmanan Y, Trock BJ, Gearhart JP, Matlaga BR. Sex prevalence of pediatric kidney stone disease in the United States: an epidemiologic investigation. Urology. 2009;74:104–7. doi: 10.1016/j.urology.2008.12.079. [DOI] [PubMed] [Google Scholar]
- 12.Mohamed J, Riadh M, Abdellatif N. Urolithiasis in infants. Pediatr Surg Int. 2007;23:295–9. doi: 10.1007/s00383-007-1889-7. [DOI] [PubMed] [Google Scholar]
- 13.Van Savage JG, Palanca LG, Andersen RD, Rao GS, Slaughenhoupt BL. Treatment of distal ureteral stones in children: similarities to the american urological association guidelines in adults. J Urol. 2000;164:89–93. doi: 10.1097/00005392-200009020-00043. [DOI] [PubMed] [Google Scholar]
- 14.Gearhart JP, Herzberg GZ, Jeffs RD. Childhood urolithiasis: experiences and advances. Pediatrics. 1991;87:445–50. [PubMed] [Google Scholar]
- 15.Alpay H, Ozen A, Gokce I, Biyikli N. Clinical and metabolic features of urolithiasis and microlithiasis in children. Pediatr Nephrol. 2009;24:2203–9. doi: 10.1007/s00467-009-1231-9. [DOI] [PubMed] [Google Scholar]
- 16.Biocić M, Saraga M, Kuzmić AC, Bahtijarević Z, Budimir D, Todorić J, et al. Pediatric urolithiasis in Croatia. Coll Antropol. 2003;27:745–52. [PubMed] [Google Scholar]
- 17.Kobayashi T, Nishizawa K, Watanabe J, Ogura K. Clinical characteristics of ureteral calculi detected by nonenhanced computerized tomography after unclear results of plain radiography and ultrasonography. J Urol. 2003;170:799–802. doi: 10.1097/01.ju.0000081424.44254.45. [DOI] [PubMed] [Google Scholar]
- 18.Gillespie RS, Stapleton FB. Nephrolithiasis in children. Pediatr Rev. 2004;25:131–9. doi: 10.1542/pir.25-4-131. [DOI] [PubMed] [Google Scholar]
- 19.Bove P, Kaplan D, Dalrymple N, Rosenfield AT, Verga M, Anderson K, et al. Reexamining the value of hematuria testing in patients with acute flank pain. J Urol. 1999;162:685–7. doi: 10.1097/00005392-199909010-00013. [DOI] [PubMed] [Google Scholar]
- 20.Goldwasser B, Cohan RH, Dunnick NR, Andriani RT, Carson CC, 3rd, Weinerth JL. Role of linear tomography in evaluation of patients with nephrolithiasis. Urology. 1989;33:253–6. doi: 10.1016/0090-4295(89)90406-8. [DOI] [PubMed] [Google Scholar]
- 21.Diament MJ, Malekzadeh M. Ultrasound and the diagnosis of renal and ureteral calculi. J Pediatr. 1986;109:980–3. doi: 10.1016/s0022-3476(86)80280-3. [DOI] [PubMed] [Google Scholar]
- 22.Johnston R, Lin A, Du J, Mark S. Comparison of kidney-ureter-bladder abdominal radiography and computed tomography scout films for identifying renal calculi. BJU Int. 2009;4:670–3. doi: 10.1111/j.1464-410X.2009.08542.x. [DOI] [PubMed] [Google Scholar]
- 23.Fowler KA, Locken JA, Duchesne JH, Williamson MR. US for detecting renal calculi with nonenhanced CT as a reference standard. Radiology. 2002;222:109–13. doi: 10.1148/radiol.2221010453. [DOI] [PubMed] [Google Scholar]
- 24.Hamm M, Wawroschek F, Weckermann D, Knöpfle E, Häckel T, Häuser H, et al. Unenhanced helical computed tomography in the evaluation of acute flank pain. Eur Urol. 2001;39:460–5. doi: 10.1159/000052486. [DOI] [PubMed] [Google Scholar]
- 25.Yilmaz S, Sindel T, Arslan G, Ozkaynak C, Karaali K, Kabaalioğlu A, et al. Renal colic: comparison of spiral CT, US and IVU in the detection of ureteral calculi. Eur Radiol. 1998;8:212–7. doi: 10.1007/s003300050364. [DOI] [PubMed] [Google Scholar]
- 26.Strouse PJ, Bates DG, Bloom DA, Goodsitt MM. Non-contrast thin-section helical CT of urinary tract calculi in children. Pediatr Radiol. 2002;32:326–32. doi: 10.1007/s00247-001-0655-6. [DOI] [PubMed] [Google Scholar]
- 27.Palmer JS, Donaher ER, O'Riordan MA, Dell KM. Diagnosis of pediatric urolithiasis: role of ultrasound and computerized tomography. J Urol. 2005;174:413–6. doi: 10.1097/01.ju.0000173133.79174.c8. [DOI] [PubMed] [Google Scholar]
- 28.Eshed I, Witzling M. The role of unenhanced helical CT in the evaluation of suspected renal colic and atypical abdominal pain in children. Pediatr Radiol. 2002;32:205–8. doi: 10.1007/s00247-001-0610-6. [DOI] [PubMed] [Google Scholar]
- 29.Brody AS, Frush DP, Huda W. Brent RL Radiation risk to children from computed temography. Pediatrics. 2007;120:677–82. doi: 10.1542/peds.2007-1910. [DOI] [PubMed] [Google Scholar]
- 30.International Commission on Radiological Protection. Ann ICRP. 1990;21:201. Recommendations of the International Commission on Radiological Protection. [PubMed] [Google Scholar]
- 31.Charles M. UNSCEAR report 2000. J Radiol Prot. 2001;21:83–6. doi: 10.1088/0952-4746/21/1/609. sources and effects of ionizing radiation.United Nations Scientific Comittee on the Effects of Atomic Radiation. [DOI] [PubMed] [Google Scholar]
- 32.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289–96. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 33.Kim BS, Hwang IK, Choi YW, Namkung S, Kim HC, Hwang WC, et al. Low-dose and standard-dose unenhanced helical computed tomography for the assessment of acute renal colic: prospective comparative study. Acta Radiol. 2005;46:756–63. doi: 10.1080/02841850500216004. [DOI] [PubMed] [Google Scholar]
- 34.Meagher T, Sukumar VP, Collingwood J, Crawley T, Schofield D, Henson J. Low dose computed tomography in suspected acute renal colic. Clin Radiol. 2001;56:873, 6. doi: 10.1053/crad.2001.0842. [DOI] [PubMed] [Google Scholar]
- 35.Passerotti C, Chow JS, Silva A, Schoettler CL, Rosoklija I, Perez-Rossello J, et al. Ultrasound versus computerized tomography for evaluating urolithiasis. J Urol. 2009;182:1829–34. doi: 10.1016/j.juro.2009.03.072. [DOI] [PubMed] [Google Scholar]
- 36.Oner S, Oto A, Tekgul S, Koroglu M, Hascicek M, Sahin A, et al. Comparison of spiral CT and US in the evaluation of pediatric urolithiasis. JBR-BTR. 2004;87:219–23. [PubMed] [Google Scholar]
- 37.Cerwinka WH, Qian J, Easley KA, Scherz HC, Kirsch AJ. Appearance of dextranomer/hyaluronic Acid copolymer implants on computerized tomography after endoscopic treatment of vesicoureteral reflux in children. J Urol. 2009;81:1324–8. doi: 10.1016/j.juro.2008.11.036. [DOI] [PubMed] [Google Scholar]
- 38.Nelson CP, Chow JS. Dextranomer/hyaluronic acid copolymer (Deflux) implants mimicking distal ureteral calculi on CT. Pediatr Radiol. 2008;38:104–6. doi: 10.1007/s00247-007-0613-z. [DOI] [PubMed] [Google Scholar]
- 39.Clark AT, Guerra L, Leonard M. Dextranomer/Hyaluronic Acid Copolymer Implant Calcification Mimicking Distal Ureteral Calculi on Ultrasound. Urology. 2010;75:1178. doi: 10.1016/j.urology.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 40.Kalorin CM, Zabinski A, Okpareke I, White M, Kogan BA. Pediatric urinary stone disease--does age matter? J Urol. 2009;181:2267–71. doi: 10.1016/j.juro.2009.01.050. [DOI] [PubMed] [Google Scholar]
- 41.Stapleton FB. Making a “dent” in hereditary hypercalciuric nephrolithiasis. J Pediatr. 1998;132:764–5. doi: 10.1016/s0022-3476(98)70300-2. [DOI] [PubMed] [Google Scholar]
- 42.García-Nieto V, Navarro JF, Luis-Yanes MI, López-Méndez M, García-Rodríguez V. Hypercalciuria in pediatric patients with ureteropelvic junction obstruction is of genetic origin. Scand J Urol Nephrol. 2007;41:144–8. doi: 10.1080/00365590600991201. [DOI] [PubMed] [Google Scholar]
- 43.Koyun M, Güven AG, Filiz S, Akman S, Akbas H, Baysal YE, Dedeoglu N. Screening for hypercalciuria in schoolchildren: what should be the criteria for diagnosis? Pediatr Nephrol. 2007;22:1297–301. doi: 10.1007/s00467-007-0528-9. [DOI] [PubMed] [Google Scholar]
- 44.Tiselius HG. Medical evaluation of nephrolithiasis. Endocrinol Metab Clin North Am. 2002;31:1031–50. doi: 10.1016/s0889-8529(02)00027-0. [DOI] [PubMed] [Google Scholar]
- 45.Battino BS, DeFOOR W, Coe F, Tackett L, Erhard M, Wacksman J, et al. Metabolic evaluation of children with urolithiasis: are adult references for supersaturation appropriate? J Urol. 2002;168:2568–71. doi: 10.1016/S0022-5347(05)64217-6. [DOI] [PubMed] [Google Scholar]
- 46.Borawski KM, Sur RL, Preminger GM. Renal calculi presenting as hyperhidrosis in patient with spinal cord injury. Urology. 2006;67:1084. doi: 10.1016/j.urology.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 47.Goldfarb DS. In the clinic.Nephrolithiasis. Ann Intern Med. 2009;151:2. doi: 10.7326/0003-4819-151-3-200908040-01002. [DOI] [PubMed] [Google Scholar]
- 48.Porowski T, Zoch-Zwierz W, Wasilewska A, Spotyk A, Konstantynowicz J. Normative data on the Bonn Risk Index for calcium oxalate crystallization in healthy children. Pediatr Nephrol. 2007;22:514–20. doi: 10.1007/s00467-006-0383-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Porowski T, Zoch-Zwierz W, Konstantynowicz J, Taranta-Janusz K. A new approach to the diagnosis of children′s urolithiasis based on the Bonn Risk Index. Pediatr Nephrol. 2008;23:1123–8. doi: 10.1007/s00467-008-0786-1. [DOI] [PubMed] [Google Scholar]
- 50.Minevich E. Pediatric urolithiasis. Pediatr Clin North Am. 2001;48:1571–85. doi: 10.1016/s0031-3955(05)70392-8. [DOI] [PubMed] [Google Scholar]
- 51.Tanaka ST, Pope JCT. Pediatric stone disease. Curr Urol Rep. 2009;10:138–43. doi: 10.1007/s11934-009-0025-8. [DOI] [PubMed] [Google Scholar]
- 52.Kruse K, Kracht U, Kruse U. Reference values for urinary calcium excretion and screening for hypercalciuria in children and adolescents. Eur J Pediatr. 1984;143:25–31. doi: 10.1007/BF00442743. [DOI] [PubMed] [Google Scholar]
- 53.DeFoor W, Minevich E, Jackson E, Reddy P, Clark C, Sheldon C, et al. Urinary metabolic evaluations in solitary and recurrent stone forming children. J Urol. 2008;179:2369–72. doi: 10.1016/j.juro.2008.01.151. [DOI] [PubMed] [Google Scholar]
- 54.Avner ED, Harmon W, Niaudet P, Yoshikawa N. Pediatric nephrology.Philadelphia: Lippincott Williams and Wilkins. 2009:1411–1412. [Google Scholar]
- 55.Favus MJ, Karnauskas AJ, Parks JH, Coe FL. Peripheral blood monocyte vitamin D receptor levels are elevated in patients with idiopathic hypercalciuria. J Clin Endocrinol Metab. 2004;89:4937–43. doi: 10.1210/jc.2004-0412. [DOI] [PubMed] [Google Scholar]


