Abstract
Background
Pneumonia and influenza (P&I) is a major cause of morbidity and mortality in the USA, particularly in elderly people. Recent research indicates that P&I may be linked to socioeconomic conditions associated with interactions of children with vulnerable elderly people that may proliferate the spread of disease. This study assessed the associations between four sociodemographic characteristics—median county income, Gini index, youth dependency ratio and proportion of co-residential caregiver grandparents—and P&I on the county level overall and by age group.
Methods
All hospitalisations due to P&I from 1991 to 2004 were abstracted from the Centers for Medicare and Medicaid Services database and categorised by influenza year (July–June) and age category. Using generalised estimating equations, associations between P&I rates and four sociodemographic variables were assessed and models were stratified by income to assess income as a potential effect modifier.
Results
P&I rates were higher in counties with lower median income. In low-income counties, high levels of live-in grandparental caregivers were associated with consistently higher levels of pneumonia and influenza rates. The Gini index was positively associated with disease rates, particularly in younger age groups.
Discussion
These results suggest complex relationships between sociodemographic characteristics and P&I outcomes for elderly people, particularly those related to children. The strength of the relationship between the proportion of grandparental caregivers and disease rates decreases with age, which may caregiving patterns, or may serve as a proxy for related sociodemographic characteristics. These findings merit further research to understand better how area-level factors affect P&I patterns in elderly people.
Keywords: Aged, child care, human, income, infection control, influenza, intergenerational relations, social epidemiology
Influenza-induced morbidity and mortality have increased over the past several decades.1 Each year, pneumonia and influenza (P&I) cause an average of 36 000 deaths in the USA, 90% of which occur in individuals aged 65 years and above.2 The biology,3 epidemiology and transmission pathways4 of influenza and pneumonia are well understood. The prevailing means of preventing influenza is through annual vaccination.5 Given the lack of universal, compulsory vaccination coverage in the USA, determining which population subgroups have the highest risk of contracting influenza, experience the most severe consequences of influenza-associated diseases and would benefit the most from vaccination is an ongoing challenge.6 7 Even accounting for vaccination, unknown factors remain that determine which individuals will contract influenza due to population heterogeneity.8 Although problematical for everyone, influenza is particularly detrimental for elderly people, who experience the highest morbidity and mortality from influenza and related diseases.9
A growing body of evidence suggests that interactions between children and elderly people contribute to the spread of influenza. Vaccinating children against influenza was associated with reduced P&I in the older population,10–12 suggesting herd immunity, or the indirect protection of populations from infections from a portion of the population having immunity from the disease.13 For influenza transmission to occur between children and elderly people, there must be contact between individuals. The greater the number of contacts with infected people one has, the more likely that person is to contract influenza.14 Susceptible individuals, such as adults whose contact network includes more individuals are more vulnerable to infection than those whose contact network is more limited, or than those who have contact with individuals who are less infective. The influenza virus is highly contagious among children largely because of prolific virus shedding in this age group and a short viral replication cycle. Influenza attack rates can be as high as 40% in children during epidemic years.15 Contact rates with other age groups are less frequent, but still important. Up to 13% of all daily contacts of school-aged children are from the age group 51 years and above.16
Grandparental caregiving patterns may facilitate the transmission of influenza virus from children to elderly people. In 2000, nearly 5.8 million grandparents lived with their grandchildren, 43% of whom had primary caregiving responsibilities for their grandchildren who are under 18 years old.17 Caring for grandchildren is believed to affect health in several ways. Direct health effects include increased exertion,18 exposure to infections due to stress19 and loss of sleep.20 Indirect health effects include reducing time for preventive self-care, such as physician visits and exercise,21 and associated changes in overall lifestyle and social relationships.22 Stress from caregiving may be responsible for reductions in immune response, suggesting that caregiving may increase the likelihood of contracting influenza among older adults.23 Caregiving grandparents differ from grandparents who do not caregive in terms of socioeconomic status. Those providing extensive caregiving for their grandchildren were less educated,24 had lower incomes and were more likely to be in poverty than those grandparents who provided occasional care.25 Grandparental caregiving has effects on the individual, household, community and population levels. Research on contextual or proximate determinants of health that show that higher population-level socioeconomic status is associated with better health and well-being, including health achievement26 and seeking preventive health measures.27
Socioeconomic status alone may not fully represent the complete socioeconomic picture of a population, and does not fully explain the health differentials that exist among socioeconomic strata. Income distribution plays an important contextual role in population health, above and beyond the contribution of overall population wealth. Relationships between high income inequality and higher mortality was illustrated on two different geographical levels: the metropolitan area28 and the state.29 The relationship between increased income inequality and morbidity was evident for a variety of health outcomes; in particular, increased infection rates, particularly pneumonia and bronchitis.30
The objective of this study is to assess how the population-level interactions of youth and elderly people influence P&I patterns in older adults and how income and income inequality relate to P&I outcomes and potentially mediate the associations between elderly people and children, and how these relationships vary with age in elderly people.
Methods
Data sources
The unit of analysis in this study is the county. Data for this analysis were abstracted from the Centers for Medicare and Medicaid Services and the US Census Bureau. All claims records of hospitalisations associated with P&I (International Classification of Disease version 9 Clinical Modification codes 480–487)31 were abstracted from the Centers for Medicare and Medicaid Services databases for each of 13 influenza years, defined as 1 July to 30 June of the following year, from 1991–2 to 2003–4, a slight modification of the definition of ‘influenza year’ in previous studies.32 33 Data were aggregated by county for all ages, and by age group: 65–74, 75–84 and 85+ years. This was performed for all years as a whole and for each individual influenza year.
Population counts were estimated using data from the decennial US census. Age-specific population totals were obtained from census 1990 and 2000 and, using linear interpolation, counts by age group were estimated for each single year of analysis, beginning on July 1991. Medicare claims counts were divided by these single-season age-specific population counts to estimate P&I rates for each influenza season, overall and by age category. For the analysis of all years combined, the midpoint population, July 1997, was used as the denominator. Explanatory demographic and socioeconomic variables were obtained from US census 2000 summary file 3. For stability of rates, counties with fewer than 1000 residents aged 65 years and above were combined with adjacent counties to make a total of 2792 counties for analysis.
Statistical analysis
Univariate statistics were obtained for all variables, including means, standard deviations and interquartile ranges. To estimate global spatial autocorrelation, Moran's I statistics were estimated for each explanatory and outcome variable. This measure is similar in interpretation to Pearson's correlation coefficient in which negative values indicate negative spatial correlation and positive values indicate positive spatial correlation. Unlike Pearson's correlation coefficient, however, Moran's I is unbounded, although in practice the statistic generally falls between −1 and 1.34 Maps depicting the spatial distributions of key predictor and outcome variables were also examined. All statistical and spatial analyses were conducted on the county level. An analysis of bivariate Spearman correlations was then performed to examine associations among predictor variables and between predictor and outcome variables. Simple log-linear regression models were then used to assess further the relationships between each predictor and outcome variable pair and to help determine the explanatory variables that were most closely and consistently related to P&I rates.
To model the relationships between socioeconomic and demographic characteristics and P&I rates, multiple log-linear regression models were used. This was done for all ages (65+ years) and for individual age groups 65–74, 75–84 and 85+ years. Seven separate models were examined for each set of outcome variables; the predictors included were based on the results of the preliminary data analysis described above. The first three models had combinations of the two demographic variables: youth dependency ratio (the ratio of the population under age 15 years to the population age 15–64 years) and the proportion of co-residential caregiving grandparents, all of which were abstracted from census 2000 and the American Community Survey. Upon conducting a preliminary analysis using several caregiving-related variables, it was determined that the proportion of co-residential grandparents who were also caregivers for their grandchildren is the best variable to represent the broad social interactions intended to analyse in this study and was adapted based on evidence from earlier literature on the topic of co-residence and caregiving.35 The youth dependency ratio, the ratio of the population under age 15 years to the population age 15–64 years, is an indirect measurement used in public health studies to describe population structure related to the interactions of youth and adults.36 These two predictor variables were analysed separately and together. The second set of models included socioeconomic variables also abstracted from the US Census Bureau bensus 2000 and the American Community Survey: The variable that represented income inequality was the Gini index, a measure of income inequality, which is continuous and can range from 0 to 1, where 0 denotes a county with income distributed perfectly evenly throughout the population and 1 denotes a county with all of the wealth clustered in one individual. Median household income was examined and, using a binary variable, counties were coded as having an average household income above or below the median for the USA. The final model included all four predictor variables from the demographic and socioeconomic models to assess potential confounding (model 7).
A model containing all variables except for income was then stratified by income level to assess possible interactions between the sociodemographic variables and income. To account for variability in the magnitude of P&I over time, each model contained indicator variables representing the influenza season. All multiple log-linear regression models were adjusted for population density and spatial location using the coordinates of the county centroids, given the modest but significant associations between each set of coordinates and disease rates. Models were assessed both giving each county equal weight and weighting by log of population size, although only the results of the unweighted analyses are presented here. Statistical analyses were conducted in SAS version 9, and spatial analyses were performed using ArcMap version 9.1 (Environmental Systems Research Institute).
Results
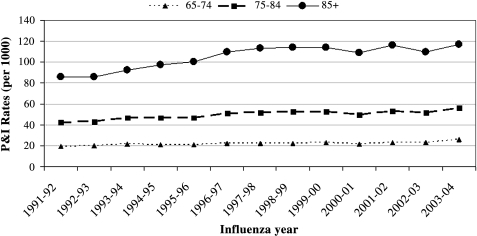
Summary statistics are displayed in table 1, and suggest somewhat right-skewed distributions for population density and, to a lesser extent, for P&I rates in each age category. More specific, annual differences in P&I hospitalisation rates by age category are displayed in figure 1. P&I rates increased over time (p<0.001 for each age group), particularly in the 85+ years group, and then levelled off in the late 1990s. From the 1992–3 to the 1998–9 seasons, average county P&I rates increased 13.8% for 65–74-yearolds, 21.0% for 75–84-year olds and 32.2% for those age 85 years and above. Spatial autocorrelations, as assessed through global Moran's indices, were small but statistically significant (p<0.05) for all exposure and outcome variables. Moran's I was lower for P&I rates (I=0.03–0.04) than for the socioeconomic and demographic predictor variables (I=0.07–0.13).
Table 1.
Summary statistics for P&I rates and key demographic and socioeconomic explanatory variables
| Percentiles | ||||||
| No of counties | Mean (SD) | 25th | 50th | 75th | Moran's I | |
| P&I rates | ||||||
| Overall | 2785 | 47.3 (27.5) | 33.9 | 43.1 | 55.1 | 0.03 |
| 65–74 years | 2791 | 24.9 (15.1) | 17.5 | 22.5 | 29.1 | 0.04 |
| 75–84 years | 2792 | 55.2 (32.4) | 40.4 | 50.8 | 63.9 | 0.03 |
| 85+ years | 2786 | 119.1 (73.4) | 85.0 | 106.8 | 138.4 | 0.03 |
| Demographic variables | ||||||
| Population density (per square mile) | 2792 | 103.1 (701.7) | 8.8 | 19.0 | 45.8 | 0.07 |
| Percentage of co-residential grandparents in the grandparent population | 2792 | 2.7 (1.5) | 1.7 | 2.4 | 3.5 | 0.07 |
| Percentage of co-residential grandparents who care for their grandchildren | 2792 | 57.5 (12.0) | 49.8 | 57.5 | 65.1 | 0.07 |
| Youth dependency ratio | 2792 | 33.1 (4.6) | 30.5 | 33.0 | 35.4 | 0.09 |
| Socioeconomic variables | ||||||
| Gini index | 2792 | 0.417 (0.033) | 0.394 | 0.416 | 0.439 | 0.13 |
| Median income | 2792 | 35 670 (8914) | 29 973 | 34 097 | 39 741 | 0.10 |
P&I, pneumonia and influenza.
Figure 1.
Distributions of county-level pneumonia and influenza (P&I) hospitalisation rates by influenza year (July–June) for three age groups: 65–74, 75–84 and 85+ years. Symbols depict medians.
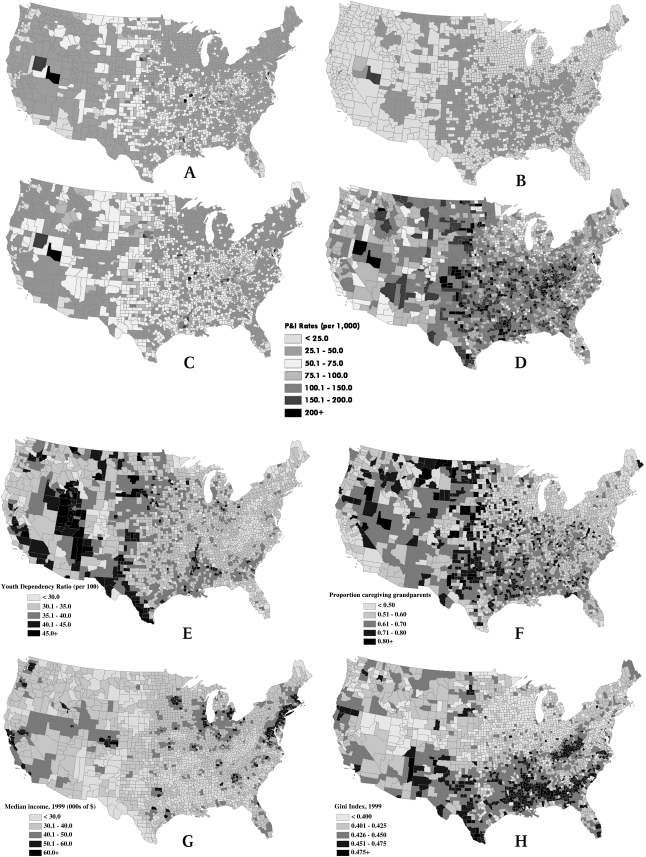
The spatial distributions of P&I rates over the entire period of study are shown in figure 2. These maps demonstrate that P&I rates follow distinct geographical patterns and generally increase with age over the age categories examined. Regions with the highest P&I rates include the western Appalachians to the Midwest, the High Plains region and several counties in Nevada. Spatial distributions of the four key explanatory variables are also shown in figure 2. Youth dependency ratios were highest in the northern Great Plains, the lower Mississippi valley, western Texas, Utah and northeastern Arizona. The proportion of co-residential caregiving grandparents was highest in the Great Plains, the South and the Rocky Mountains. Median household income was highest near major cities, whereas the counties with the lowest incomes were found predominantly in the Deep South and western Appalachians. Gini indices were highest in the South, Southwest and scattered throughout the High Plains.
Figure 2.
Average annual pneumonia and influenza (P&I) hospitalisation rates by county for age 65 years and above (panel A), age 65–74 years (panel B), age 75–84 years (panel C) and age 85 years and above (panel D), and distributions of county-level predictor variables: youth dependency ratio (panel E), proportion of live-in grandparents who provide care for grandchildren (panel F), median household income (panel G) and Gini index (panel H).
There were strong correlations between the socioeconomic and demographic predictor variables. All covariates were significantly associated with each other covariate at the p<0.001 level, although the magnitude of these associations varied among variable pairs. The strongest negative association was found between the Gini index and median income (r=−0.673, p<0.001). Income and the log of population density were strongly and positively correlated (r=0.516, p<0.001). The proportion of co-residential caregiving grandparents was also negatively correlated with income level (r=−0.407, p<0.001). We also examined related, potentially influential variables, including the average number of people households, but found only weak associations between this variable and P&I rates overall and for each age category (r between −0.023 and −0.090).
Parameter estimates from the seven Poisson regression models examined are displayed in table 2. Model 1 showed no significant relationships between the youth dependency ratio and P&I rates across all age categories. However, there was a consistent positive relationship between the proportion of live-in grandparents who have primary caregiving responsibilities for their grandchildren and P&I rates across all age categories, although the magnitude of the relationship became slightly smaller as age increased (models 2 and 3). Associations were observed for the Gini index in model 5, in which there was a significant positive association between the P&I rate and Gini index for the population overall and for those aged 65–74 years. The risk of P&I was between approximately 11% and 28% higher in counties whose median household incomes were below the national median, compared with those above the national median (model 4, all counties), respectively, and these associations remained when the Gini index was included (model 6). This relationship between median county income and P&I rates was present across all three age groups. All socioeconomic and demographic variables were included in model 7, and the relationships observed in the individual models remained, including a consistent positive relationship between P&I and the percentage of co-residential caregiving grandparents, except in the oldest age category. Moran's I for these models were modest (I=0.03–0.04), but statistically significant, suggesting some slight residual spatial autocorrelation, even after accounting for spatial and socioeconomic attributes. All models controlled for the log of population density, spatial location and seasonal variability.
Table 2.
Estimates of relative risks and 95% CI from Poisson regression modelling of P&I rates overall and by age categories for demographic (models 1–3), socioeconomic (models 4–6) and for all variables combined (model 7)
| Children–elderly person interactions | Socioeconomic status | ||||
| Youth dependencyratio | Proportion of live-in grandparents who care for their grandchildren | Below US median income county | Gini index | ||
| Model 1 | All | 0.84 (0.48, 1.48) | |||
| 65–74 years | 1.04 (0.58, 1.86) | ||||
| 75–84 years | 0.81 (0.46, 1.28) | ||||
| 85+ years | 0.66 (0.90, 1.17) | ||||
| Model 2 | All | 1.62 (1.25, 2.12)*** | |||
| 65–74 years | 1.67 (1.27, 2.21)*** | ||||
| 75–84 years | 1.50 (1.14, 1.97)** | ||||
| 85+ years | 1.41 (1.06, 1.88)* | ||||
| Model 3 | All | 0.93 (0.54, 1.60) | 1.62 (1.25, 2.11)*** | ||
| 65–74 years | 1.16 (0.66, 2.03) | 1.68 (1.28, 2.20)*** | |||
| 75–84 years | 0.88 (0.51, 1.52) | 1.49 (1.14, 1.96)** | |||
| 85+ years | 0.70 (0.40, 1.22) | 1.40 (1.06, 1.84)* | |||
| Model 4 | All | 1.19 (1.11, 1.28)*** | |||
| 65–74 years | 1.23 (1.14, 1.32)*** | ||||
| 75–84 years | 1.16 (1.08, 1.25)*** | ||||
| 85+ years | 1.13 (1.05, 1.23)** | ||||
| Model 5 | All | 1.14 (1.03, 1.26)** | |||
| 65–74 years | 1.21 (1.08, 1.35)*** | ||||
| 75–84 years | 1.10 (0.99, 1.23) | ||||
| 85+ years | 1.08 (0.97, 1.20) | ||||
| Model 6 | All | 1.20 (1.09, 1.31)*** | 0.98 (0.87, 1.11) | ||
| 65–74 years | 1.21 (1.11, 1.32)*** | 1.03 (0.90, 1.18) | |||
| 75–84 years | 1.18 (1.08, 1.29)*** | 0.96 (0.84, 1.09) | |||
| 85+ years | 1.15 (1.05, 1.27)** | 0.96 (0.84, 1.10) | |||
| Model 7 | All | 1.04 (0.61, 1.77) | 1.48 (1.11, 1.96)** | 1.18 (1.08, 1.30)*** | 0.97 (0.86, 1.09) |
| 65–74 years | 1.36 (0.79, 2.36) | 1.48 (1.16, 1.98)** | 1.20 (1.09, 1.32)*** | 1.02 (0.90, 1.16) | |
| 75–84 years | 0.95 (0.55, 1.62) | 1.38 (1.03, 1.85)* | 1.17 (1.07, 1.28)** | 0.95 (0.84, 1.07) | |
| 85+ years | 0.74 (0.43, 1.28) | 1.31 (0.97, 1.78) | 1.14 (1.03, 1.26)* | 0.95 (0.83, 1.07) | |
* p<0.05; **p<0.01; ***p<0.001.
All models controlled for log of population density, spatial location and seasonal variability.
P&I, pneumonia and influenza.
Parameter estimates from the full model, except for the income indicator variable, stratified by county income level are shown in table 3. The youth dependency ratio was again not significantly associated with P&I rates in any of the models. The Gini index was positively associated with P&I rates in the low-income counties for the 65–74 years age group. The proportion of caregiving, co-residential grandparents was significantly associated with increased P&I rates in low-income counties for all age groups examined, the magnitude of which decreased slightly with increasing age; this association was not evident in high-income counties.
Table 3.
Relative risks from full model by county median income (above or below national median)
| Youth dependency ratio | Proportion of live-in grandparents who care for their grandchildren | Gini index | ||
| Overall | High-income counties | 1.00 (0.34, 2.92) | 1.27 (0.66, 2.46) | 0.83 (0.67, 1.02) |
| Low-income counties | 0.95 (0.63, 1.43) | 1.62 (1.34, 1.95)*** | 1.10 (1.00, 1.22) | |
| 65–74 years | High-income counties | 1.75 (0.62, 4.95) | 1.32 (0.69, 2.52) | 0.85 (0.66, 1.09) |
| Low-income counties | 1.12 (0.72, 1.73) | 1.57 (1.29, 1.92)*** | 1.20 (1.08, 1.32)*** | |
| 75–84 years | High-income counties | 0.84 (0.29, 2.48) | 1.15 (0.59, 2.27) | 0.79 (0.63, 0.99)* |
| Low-income counties | 0.90 (0.60, 1.35) | 1.55 (1.29, 1.87)*** | 1.10 (1.00, 1.21) | |
| 85+ years | High-income counties | 0.58 (0.20, 1.70) | 1.07 (0.53, 2.15) | 0.81 (0.64, 1.02) |
| Low-income counties | 0.74 (0.49, 1.13) | 1.48 (1.21, 1.80)*** | 1.07 (0.96, 1.19) |
*p<0.05; **p<0.01; ***p<0.001.
All models controlled for log of population density, spatial location and seasonal variability.
Discussion
Interpretation of findings
This study is among the first to examine the potential for co-residential caregiving grandparents to have an increased risk of P&I in the older population. Caregiving responsibilities in co-residential grandparents may serve as a contextual proxy for related socioeconomic conditions that may actually be related to the spread of P&I between children and elderly people or among elderly people themselves.37 Alternatively, this finding could reflect the true nature of influenza transmission between children and grandparental caregivers—namely increased contact between the generations in areas with high grandparental caregiving levels16 perhaps contributing to decreased immune response in older adults.23 The magnitude of the positive relationship between the proportion of co-residential caregiving grandparents and P&I decreased with age, which may indicate lower levels of primary caregiving for grandchildren at the oldest ages, consistent with earlier research.25 The percentage of co-residential caregiving grandparents was consistently and positively associated with P&I rates in the poorest counties, particularly in the younger age groups, which supports the notion that the association of increased grandparental caregiving and higher P&I rates may be more problematical in poor socioeconomic populations. The precise mechanisms of this remain not fully understood, but these observations could be due to differences in the type of care provided by grandparents in lower income areas, such as crowdedness, which may lead to increased physical proximity, or perhaps from older, decaying infrastructure, such as poor ventilation or a propensity to live in public housing. On a broader scope, grandparents living in poorer areas may also have a limited access to health care, particularly because of income for care payment, more difficult access to a physician, or even less possibility to consult a physician with children at home for whom they provide care.
The age-associated relationships observed between income inequality and P&I rates were consistent with the findings of a similar study demonstrating that higher income inequality was associated with poor health conditions across the US population, but the magnitude of this relationship decreased as age increased.38 Few studies have examined the potential for the relationship between income inequality and health to vary by age, although several studies examine the relationships between income inequality and health and age and health independently.39 40 This study explores the possibility that income inequality and health are related, even after accounting for the relationship between income and health.
Limitations
Several important limitations should be taken into consideration regarding the statistical modelling procedures and variable construction used in this analysis. This analysis employs the county Gini index as the exposure variable, but several studies have suggested that other measures, such as the Robin Hood index and the Atkinson index,41 and other measures, including simple poverty measures, have the potential to capture other aspects of income distribution and inequality that the Gini index cannot.42 A related issue to this is the question of how income inequality affects health outcomes; little is known about the specific pathways through which income inequality influences health, but researchers have speculated several possibilities. One potential mechanism is the breakdown of social cohesion that occurs in areas with high socioeconomic inequality. In economically homogeneous societies and local areas, increased social cohesion, solidarity and life expectancies have been observed, even after accounting for the overall level of wealth.43 44 Another possibility is that areas of high socioeconomic disparities lead to worse provision of public goods and services,45 including the public health infrastructure, which could lead to more detrimental health outcomes, such as P&I. Alternatively, in areas of high income inequality, being of comparatively low social status relative to others could affect patterns of violence, disrespect, poor social relations and depression, and may interact with other health-related factors such as social support.46 More research is needed to elucidate these relationships and specify those exact pathways through which the relationship between income inequality and health outcomes occurs, as well as understanding the differences in how income inequality, distinct from income itself, affects population health.
An assessment of contact rates between children and elderly people is difficult to estimate on the population level. The two primary variables of interest—the proportion of co-residential, caregiving grandparents and the youth dependency ratio—provide meaningful information, but may not tell the complete picture about contact rates. Average household size, contact networks, and other related variables may shed additional light on this complex issue and can be addressed in future studies. The way in which caregiving itself was measured—the proportion of co-residential grandparents who provide care for their grandchildren—omits non-co-residential caregiving grandparents and may be skewed by a small denominator: the co-residential grandparent population. However, this variable was selected to quantify the size of the older population who potentially have the greatest contact with children, as opposed to co-residential grandparents who do not provide care, or non-co-residential grandparents who provide care occasionally.
Ecological studies are often criticised because the findings of an ecological study apply only on the population level and cannot be extended to the individual level,47 an example of the ‘ecological fallacy’.48 Despite the inherent drawbacks of the ecological design, it is both necessary and appropriate to use an ecological design in this type of analysis. In addition, this research does not purport to extend the relationships observed at the county level to the individual level. This study is concerned with population rates, not an individual's susceptibility to P&I based on individual risk factors, such as caregiving, personal income and individual contact networks. Furthermore, some variables—measures of income inequality and dependency ratios—cannot be defined on the individual level.49 50 Future research can expand on those individual-level factors that cannot be addressed in ecological studies, but are crucial to the understanding of the transmission of influenza from children to elderly people. Another issue ecological analyses raise is the choice of geographical level on which to aggregate. Relationships observed on the county level do not necessarily reflect the nature of the relationships on other geographical levels.51
Policy implications and future research
Despite these limitations, the findings of this study contribute to the small, but growing body of evidence suggesting that certain sociodemographic factors, particularly those pertaining to the dynamics between children and co-residential elderly people, may influence P&I rates in elderly people. Future research is necessary to help explain the observed relationships between co-residential grandparents providing care to their grandchildren, income inequality and P&I outcomes in elderly people. Although this research is preliminary, these findings have potential significance for policies and programmes for grandparental caregivers. Targeted social distancing may be effective at reducing the spread of influenza from particularly vulnerable populations—elderly people—from those that are often most infective—children. This does not mean keeping children and elderly people separated from one another, but rather to direct resources to reduce the spread of influenza from children to elderly people, such as the vaccination of children against influenza and related diseases.
What is already known on this subject.
Influenza causes substantial morbidity and mortality for the vulnerable population of US elderly people.
Children play an integral role in the spread of influenza, yet little is known about how children transmit influenza to elderly people on the population level.
Income inequality also affects population health and has negative effects on many chronic and infectious diseases. Therefore, we examined the associations between four key sociodemographic factors related to child–senior interactions and socioeconomic status and influenza outcomes using a comprehensive database of hospitalisations in US elderly people for 13 influenza years.
What this study adds.
This study demonstrated that areas of high income inequality and low overall income had higher levels of influenza-associated disease in elderly people, and there were consistent associations between grandparental caregiving and influenza-associated diseases in elderly people, even after controlling for socioeconomic status. These findings indicate that population-level sociodemographic factors, particularly the potential for increased intergenerational contact for co-residential grandparents, may influence influenza dynamics.
Acknowledgments
The authors wish to thank Drs Thomas Louis, Ann Klassen and Michelle Hindin of the Johns Hopkins Bloomberg School of Public Health, Drs Kenneth Chui, Jyotsna Jagai, Janet Forrester, Sioban Mor and Ms Julia Wenger of Tufts University and Ms Sara Parisi of the Children's Hospital of Pittsburgh for their assistance with this research project.
Footnotes
Funding: This research was funded by the following grants: NIH-NIAID U19 AI62627 and HHSN266200500032C.
Competing interests: None.
Ethics approval: This study was conducted with the approval of the Tufts Medical Center and the Johns Hopkins Bloomberg School of Public Health.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA 2004;292:1333–40 [DOI] [PubMed] [Google Scholar]
- 2.Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA 2003;289:179–86 [DOI] [PubMed] [Google Scholar]
- 3.Nicholson KG, Wood JM, Zambon M. Influenza. Lancet 2003;362:1733–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zambon MC. Epidemiology and pathogenesis of influenza. J Antimicrob Chemother 1999;44(Suppl B):3–9 [DOI] [PubMed] [Google Scholar]
- 5.Ompad DC, Galea S, Vlahov D. Distribution of influenza vaccine to high-risk groups. Epidemiol Rev 2006;28:54–70 [DOI] [PubMed] [Google Scholar]
- 6.Iton AB. Rationing influenza vaccine: legal strategies and considerations for local health officials. J Public Health Manag Pract 2006;12:349–55 [DOI] [PubMed] [Google Scholar]
- 7.Harper SA, Fukuda K, Uyeki TM, et al. Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2005;54:1–40 [PubMed] [Google Scholar]
- 8.Halloran ME, Haber M, Longini IM., Jr Interpretation and estimation of vaccine efficacy under heterogeneity. Am J Epidemiol 1992;136:328–43 [DOI] [PubMed] [Google Scholar]
- 9.Sprenger MJ, Mulder PG, Beyer WE, et al. Impact of influenza on mortality in relation to age and underlying disease, 1967–1989. Int J Epidemiol 1993;22:334–40 [DOI] [PubMed] [Google Scholar]
- 10.Monto AS, Davenport FM, Napier JA, et al. Modification of an outbreak of influenza in Tecumseh, Michigan by vaccination of schoolchildren. J Infect Dis 1970;122:16–25 [DOI] [PubMed] [Google Scholar]
- 11.Reichert TA, Sugaya N, Fedson DS, et al. The Japanese experience with vaccinating schoolchildren against influenza. N Engl J Med 2001;344:889–96 [DOI] [PubMed] [Google Scholar]
- 12.Ghendon YZ, Kaira AN, Elshina GA. The effect of mass influenza immunization in children on the morbidity of the unvaccinated elderly. Epidemiol Infect 2006;134:71–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fine PE. Herd immunity: history, theory, practice. Epidemiol Rev 1993;15:265–302 [DOI] [PubMed] [Google Scholar]
- 14.Ferrari MJ, Bansal S, Meyers LA, et al. Network frailty and the geometry of herd immunity. Proc Biol Sci 2006;273:2743–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramet J, Weil-Olivier C, Sedlak W. Influenza vaccination: the paediatric perspective. Vaccine 2007;25:780–7 [DOI] [PubMed] [Google Scholar]
- 16.Mikolajczyk RT, Akmatov MK, Rastin S, et al. Social contacts of school children and the transmission of respiratory-spread pathogens. Epidemiol Infect 2008;136:813–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simmons T, Dye JL. Grandparents living with grandchildren: 2000. Census 2000 Brief. http://www.census.gov/prod/2003pubs/c2kbr-31.pdf (accessed 2 Dec 2008).
- 18.Grinstead LN, Leder S, Jensen S, et al. Review of research on the health of caregiving grandparents. J Adv Nurs 2003;44:318–26 [DOI] [PubMed] [Google Scholar]
- 19.Minkler M, Fuller-Thomson E, Miller D, et al. Depression in grandparents raising grandchildren: results of a national longitudinal study. Arch Fam Med 1997;6:445–52 [DOI] [PubMed] [Google Scholar]
- 20.Jendrek MP. Grandparents who parent their grandchildren: circumstances and decisions. Gerontologist 1994;34:206–16 [DOI] [PubMed] [Google Scholar]
- 21.Roe KM, Minkler M, Saunders F, et al. Health of grandmothers raising children of the crack cocaine epidemic. Med Care 1996;34:1072–84 [DOI] [PubMed] [Google Scholar]
- 22.Szinovacz ME, DeViney S, Atkinson MP. Effects of surrogate parenting on grandparents' well-being. J Gerontol B Psychol Sci Soc Sci 1999;54:S376–88 [DOI] [PubMed] [Google Scholar]
- 23.Kiecolt-Glaser JK, Glaser R, Gravenstein S, et al. Chronic stress alters the immune response to influenza virus vaccine in older adults. Proc Natl Acad Sci U S A 1996;93:3043–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pittman LD. Grandmothers' involvement among young adolescents growing up in poverty. J Res Adolesc 2007;17:89–115 [Google Scholar]
- 25.Fuller-Thomson E, Minkler M. American grandparents providing extensive child care to their grandchildren: prevalence and profile. Gerontologist 2001;41:201–9 [DOI] [PubMed] [Google Scholar]
- 26.Xu KT. State-level variations in income-related inequality in health and health achievement in the US. Soc Sci Med 2006;63:457–64 [DOI] [PubMed] [Google Scholar]
- 27.Pill R, Peters TJ, Robling MR. Social-class and preventive health behavior—a British example. J Epidemiol Community Health 1995;49:28–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lynch JW, Kaplan GA, Pamuk ER, et al. Income inequality and mortality in metropolitan areas of the United States. Am J Public Health 1998;88:1074–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ross NA, Wolfson MC. Income inequality and mortality in Canada and the United States. An analysis of provinces/states. Ann N Y Acad Sci 1999;896:338–40 [DOI] [PubMed] [Google Scholar]
- 30.Kennedy BP, Kawachi I, Prothrow-Stith D. Income distribution and mortality: cross sectional ecological study of the Robin Hood index in the United States. BMJ 1996;312:1004–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Viboud C, Bjornstad ON, Smith DL, et al. Synchrony, waves, and spatial hierarchies in the spread of influenza. Science 2006;312:447–51 [DOI] [PubMed] [Google Scholar]
- 32.Viboud C, Boëlle PY, Pakdaman K, et al. Influenza epidemics in the United States, France, and Australia, 1972–1997. Emerg Infect Dis 2004;10:32–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Serfling RE. Methods for current statistical analysis of excess pneumonia-influenza deaths. Public Health Rep 1963;78:494–506 [PMC free article] [PubMed] [Google Scholar]
- 34.Crighton EJ, Elliott SJ, Moineddin R, et al. An exploratory spatial analysis of pneumonia and influenza hospitalizations in Ontario by age and gender. Epidemiol Infect 2007;135:253–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hughes ME, Waite LJ, LaPierre TA, et al. All in the family: the impact of caring for grandchildren on grandparents' health. J Gerontol B Psychol Sci Soc Sci 2007;62:S108–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guyer B, Freedman MA, Strobino DM, et al. Annual summary of vital statistics: trends in the health of Americans during the 20th century. Pediatrics 2000;106:1307–17 [DOI] [PubMed] [Google Scholar]
- 37.Le C, Chongsuvivatwong V, Geater A. Contextual socioeconomic determinants of cardiovascular risk factors in rural south-west China: a multilevel analysis. BMC Public Health 2007;7:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.LeClere FB, Soobader MJ. The effect of income inequality on the health of selected US demographic groups. Am J Public Health 2000;90:1892–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lopez R. Income inequality and self-rated health in US metropolitan areas: a multi-level analysis. Soc Sci Med 2004;59:2409–19 [DOI] [PubMed] [Google Scholar]
- 40.Robert SA, Lee KY. Explaining race differences in health among older adults—the contribution of community socioeconomic context. Res Aging 2002;24:654–83 [Google Scholar]
- 41.Atkinson AB. Measurement of inequality. J Econ Theory 1970;2:244–63 [Google Scholar]
- 42.Kawachi I, Kennedy BP. The relationship of income inequality to mortality: does the choice of indicator matter? Soc Sci Med 1997;45:1121–7 [DOI] [PubMed] [Google Scholar]
- 43.House JS, Landis KR, Umberson D. Social relationships and health. Science 1988;241:540–5 [DOI] [PubMed] [Google Scholar]
- 44.Kawachi I, Kennedy BP. Health and social cohesion: why care about income inequality? BMJ 1997;314:1037–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Marmot M. The influence of income on health: views of an epidemiologist. Health Affairs 2002;21:31–46 [DOI] [PubMed] [Google Scholar]
- 46.Wilkinson RG. Health, hierarchy, and social anxiety. Ann N Y Acad Sci 1999;896:48–63 [DOI] [PubMed] [Google Scholar]
- 47.Kaplan GA, Pamuk ER, Lynch JW, et al. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. BMJ 1996;312:999–1003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Robinson W. Ecological correlations and the behavior of individuals. Am Sociol Rev 1950;50:331–7 [Google Scholar]
- 49.Susser M. The logic in ecological: I. The logic of analysis. Am J Public Health 1994;84:825–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schwartz S. The fallacy of the ecological fallacy: the potential misuse of a concept and the consequences. Am J Public Health 1994;84:819–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Krieger N, Chen JT, Waterman PD, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. Am J Epidemiol 2002;156:471–82 [DOI] [PubMed] [Google Scholar]