Abstract
The present study examined whether metformin treatment prevents isoporterenol-induced cardiac hypertrophy in mice. Chronic subcutaneous infusion of isoproterenol (15 mg/kg/24 h) for 1 week using an osmotic minipump induced cardiac hypertrophy measured by the heart-to-body weight ratio and left ventricular posterior wall thickness. Cardiac hypertrophy was accompanied with increased interleukin-6 (IL-6), transforming growth factor (TGF)-β, atrial natriuretic peptide (ANP), collagen I and III, and matrix metallopeptidase 2 (MMP-2). Coinfusion of metformin (150 mg/kg/24 h) with isoproterenol partially inhibited cardiac hypertrophy that was followed by reduced IL-6, TGF-β, ANP, collagen I and III, and MMP-2. Chronic subcutaneous infusion of metformin did not increase AMP-activated protein kinase (AMPK) activity in heart, although acute intraperitoneal injection of metformin (10 mg/kg) increased AMPK activity. Isoproterenol increased nitrotyrosine levels and mRNA expression of antioxidant enzyme glutathione peroxidase and metformin treatment normalized these changes. These results suggest that metformin inhibits cardiac hypertrophy through attenuating oxidative stress.
Keywords: Metformin, Cardiac hypertrophy, Oxidative stress, AMPK, Isoproterenol
INTRODUCTION
Pathological cardiac hypertrophy is an independent risk factor for heart failure [1]. Although hypertension and loss of myocytes following ischemic damage are the leading causes of pathological cardiac hypertrophy [2], adrenergic overactivation also contributes to hypertrophy. Patients with left ventricular hypertrophy demonstrate increased plasma norepinephrine concentration and enhanced sympathetic nerve activity compared with subjects without hypertrophy [3-5]. Moreover, adrenergic agonists such as isoproterenol can induce cardiac hypertrophy in experimental animals [6-8]. Isoproterenol-induced cardiac hypertrophy is a reliable, reproducible, and well-characterized model of pathological cardiac hypertrophy [9,10].
The biguanide derivative metformin is one of the most commonly used therapeutic agents for type 2 diabetes [11]. Metformin improves glycemic control via suppression of gluconeogenesis and, to a lesser extent, enhances insulin-mediated glucose uptake in fat and muscle tissue [12-14]. In addition to its insulin-sensitizing effect, metformin has also been shown to have cardioprotective effects. Patients who received metformin therapy demonstrate significant improvement all-cause and cardiovascular mortality when compared with patients who received sulphonylurea therapy [15,16]. Metformin treatment also reduces the risk of myocardial infarct in diabetic patients [17]. Recently, metformin was revealed to be an AMP activated protein kinase (AMPK) activator [18] and low doses metformin significantly improves left ventricular function and survival via activation of AMPK [19]. However, the influence of metformin on isoproterenol induced cardiac hypertrophy is unclear. The present study examined whether metformin treatment prevents isoporterenol-induced cardiac hypertrophy.
METHODS
Animals and treatment
Male C57BL/6J mice weighing 20 g were purchased from Samtaco (Seoul, South Korea) and were housed in the animal unit of College of Medicine at Yeungnam University. Mice were housed in a group cage in a room with a 12:12-h light-dark cycle, lights on at 7:00 and off at 19:00. The mice were fed a standard chow diet and given ad libitum access to water. This study was conducted in accordance with the guidelines for the care and use of laboratory animals provided by Yeungnam University. All experimental protocols were approved by the Ethics Committee of Yeungnam University. After intraperitoneal injection of a combination of anesthetics (tiletamine and zolezepam, 25 mg/kg body weight; xylazine, 10 mg/kg body weight), minipumps (Alzet, Cupertino, CA, USA) containing 0.9% saline, metformin (150 mg/kg/24 h), isoproterenol (15 mg/kg/24 h), or metformin with isoproterenol were inserted into skin in the interscapular region. After 1 week, mice were anesthetized and blood samples were collected. After removing blood from hearts, the hearts were weighed. The left ventricles were excised and stored at -80℃ for the measurement of expression of genes and proteins. The chronic effect of metformin on AMPK activation in the heart was measured in mice after inserting minipump (150 mg/kg/day) at 0, 2, 4, 24, and 48 h. The acute effect of metformin on AMPK activation was also measured in mice hearts at 1 h after the intraperitoneal injection of metformin (10 mg/kg). Heart was collected and stored at -80℃ for the measurement of AMPK activity.
Echocardiography
Echocardiograms were conducted on mice anesthetized with intraperitoneal injection of anesthetics after 1 week of saline, isoproterenol, metformin, or isoproterenol with metformin as previously described [6]. Echo imaging was acquired using a Sequoia C512 (Acuson, Mountainview, CA, USA) platform equipped with a 15 MHz linear transducer. Measurements were performed in triplicate using the leading edge convention for myocardial borders, as defined by the American Society of Echocardiography. Posterior wall thickness in diastole was used as an indicator of cardiac hypertrophy.
Real-time polymerase chain reaction (PCR)
Left ventricle of approximately 25 mg was homogenized in TRI reagent (Sigma-Aldrich, St. Louis, MO, USA) using an Ultra-Turrax T25 (Janke & Kunkel, IKA-Labortechnik, Staufel, Germany). RNA was reverse transcribed to cDNA from 1 µg of total RNA using a High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA). Quantitative real-time PCR was performed using the Real-Time PCR 7500 Software system and Power SYBR Green PCR master mix (Applied Biosystems) according to the manufacture's instructions. Expression levels of β-actin were used for sample normalization. The reactions were incubated at 95℃ for 10 min, followed by 45 cycles at 95℃ for 15 s, 55℃ for 20 s, and 72℃ for 35 s for interleukin-6 (IL-6), collagen I, collagen III, glutathione peroxidase 1 (GPx1), matrix metallopeptidase 2 (MMP-2), and MMP-9. The reactions for transforming growth factor-β (TGF-β) and atrial natriuretic peptide (ANP) were used the same condition as with IL-6, except for the annealing temperature, which was 52℃ instead of 55℃. Primers were based on NCBI's nucleotide database and designed using the Primer Express program (Applied Biosystems):β-actin (121 bp: forward, 5'-TGG ACA GTG AGG CAA GGA TAG-3'; reverse, 5'-TAC TGC CCT GGC TCC TAG CA-3'), IL-6 (71 bp: forward, 5'-AAA TGA TGG ATG CTA CCA AAC T-3'; reverse, 5'-CCA GAA GAC CAG AGG AAA TTT T-3'), collagen I (71 bp: forward, 5'-ACA TGC TCA GCT TTG TGG AT -3'; reverse, 5'-ATA TTG GCA TGT TGC TAG GC-3'), collagen III (72 bp: forward, 5'-CGT AGA TGA ATT GGG ATG CA-3'; reverse, 5'-ACA TGG TTC TGG CTT CCA G-3'), GPx1 (71 bp: forward, 5'-GAA GTG CGA AGT GAA TGG TG-3'; reverse, 5'-TGG GTG TTG GCA AGG C-3'), MMP-2 (71 bp: forward, 5'-GGA ACA AGA ACC AGG TCA CA-3'; reverse, 5'-AAG CAT CAT CCA CGG TTT C-3'), MMP-9 (72 bp: forward, 5'-GTG TTC CCA TTC ATC TTT GA-3'; reverse, 5'-CAG CGG TAA CCA TCC GA-3'), TGF-β (72 bp: forward, 5'-CAA CGC CAT CTA TGA GAA AA-3'; reverse, 5'-CGA ATG TCT GAC GTA TTG AAG A-3'), and ANP (71 bp: forward, 5'-CGG TGT CCA ACA CAG ATC-3'; reverse, 5'-TCT TCT ACC GGC ATC TTT C-3').
Western blotting
Left ventricle was used for measurement of protein level of phosphorylated AMPK (Cell Signaling Technologies, Danvers, MA, USA), AMPK (Cell Signaling Technologies), nitrotyrosine (Upstate Biotechnology, Lake Placid, NY, USA), and glyceraldehyde 3-phosphate dehydrogenase (GAPDH; Santa Cruz Biotechnology, Santa Cruz, CA, USA). Tissue approximately 40 mg was homogenized in a lysis buffer (Invitrogen, Carlsbad, CA, USA) containing 1% NP40, 150 mM NaCl, 5 mM MgCl2, 10 mM HEPES buffer, leupeptin, and pepstatin A. Protein concentration was determined by the Bradford method (BioRad, Hercules, CA, USA). A 30 µg sample of the total protein per lane was separated by 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis. The separated proteins were then transferred to a 0.45 µm polyvinylidene fluoride membrane (Gelman Sciences, Ann Arbor, MI, USA). After blocking with a solution containing 5% skim milk, 10 mM Tris-HCl (pH 7.4), 150 mM NaCl, and 0.1% Tween 20, the membrane was incubated overnight at 4℃ with a 1:1,000 dilution of the primary antibody. Specific antibody binding was detected using a 1:2,000 dilution of sheep anti-rabbit IgG horseradish peroxidase (Bio-Rad) for 1 h at room temperature and visualized using an enhanced chemiluminescence detection reagent (Millipore, Billerica, MA, USA).
Statistical analyses
The results are expressed as mean±SE. Differences among the groups were assessed via one-way analysis of variance followed by LSD test. All statistical analyses were conducted using SPSS software (SPSS, Chicago, IL, USA).
RESULTS
Heart weight and gene expression
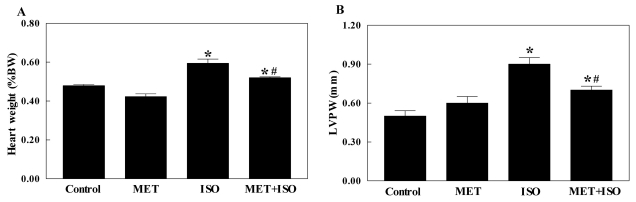
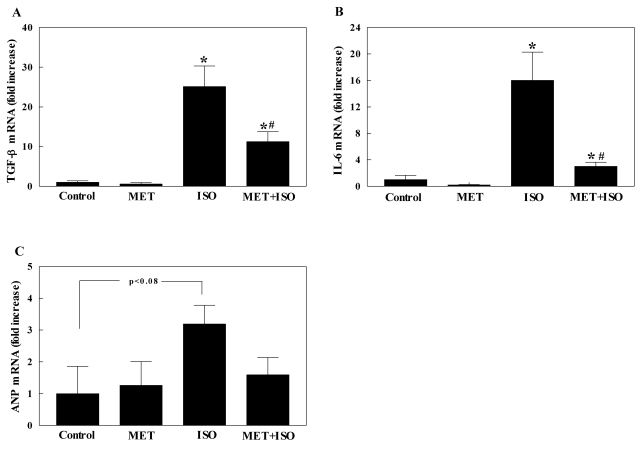
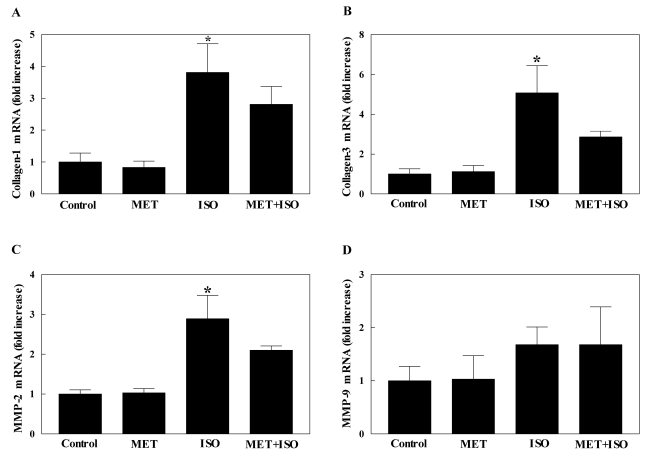
Body weight was not different among the groups (data not shown). Heart weight presented as percentage of heart weight to body weight was increased by isoproterenol infusion that was partially inhibited by coinfusion of isoproterenol with metformin. Metformin alone did not affect heart weight (Fig. 1A). Left ventricular posterior wall thickness also showed same pattern of changes with heart weight (Fig. 1B). Since cardiac hypertrophy is known to be associated with increased gene expression of TGF-β, IL-6, ANP, collagen, and MMPs, the gene expression of these factors were measured in this study for the evaluation of cardiac hypertrophy [20,21]. Isoproterenol infusion increased the mRNA level of TGF-β in heart, which was partially reduced by coinfusion of isoporterenol with metformin (Fig. 2A). The gene expression of IL-6 in heart also showed same pattern of changes with TGF-β; the increased IL-6 mRNA level by isoproterenol was also partially reversed by cotreatment of isoproterenol with metformin (Fig. 2B). The gene expression of ANP showed this same pattern of changes but it was not statistically significant (Fig. 2C). Collagen I and III in heart were significantly increased by isoporterenol infusion compared with saline-infused control mice. However, coinfusion of isoproterenol with metformin did not significantly increase the gene expression of collagen I and III in heart. The gene expression of MMP-2 showed the same pattern of changes with collagen I and III. MMP-9 did not differ among the groups (Fig. 3).
Fig. 1.
Heart weight (A) and left ventricular posterior wall thickness (LVPW) measured using echocardiography (B) in mice. Mice were infused with saline (control), isoproterenol (ISO), metformin (MET) or metformin with isoproterenol (MET+ISO) for I week using osmotic minipumps. Data is expressed as mean±SE. Experimental cases are 6~9. *p<0.05 vs. Control and #p<0.05 vs. ISO.
Fig. 2.
Gene expression of transforming growth factor-β (TFG-β) (A), interleukin-6 (IL-6) (B), and atrial natriuretic peptide (ANP) (C) in the heart of saline (control), isoproterenol (ISO), metformin (MET) or metformin with isoproterenol (MET+ISO) infused mice for 1 week using osmotic minipumps. Data is expressed as mean± SE. Experimental cases are 6~9. *p<0.05 vs. Control and #p<0.05 vs. ISO.
Fig. 3.
Gene expression of collagen-1 (A), collage-3 (B), matrix metallopeptidase 2 (MMP-2) (C), and MMP-9 (D) in the heart of saline (control), isoproterenol (ISO), metformin (MET) or metformin with isoproterenol (MET+ISO) infused mice for 1 week using osmotic minipumps. Data is expressed as mean±SE. Experimental cases are 6~9. *p<0.05 vs. Control.
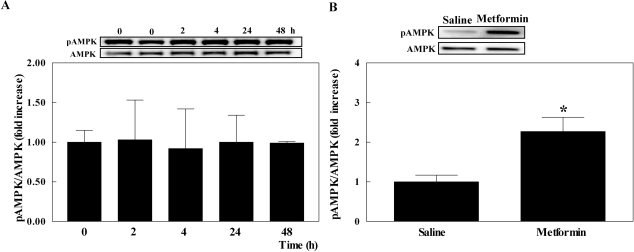
pAMPK levels in heart
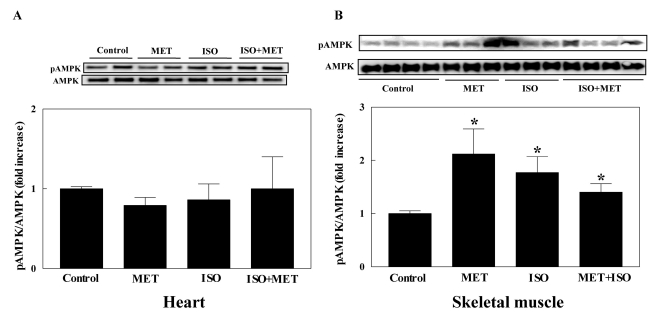
Since metformin is known as an AMPK activator, the pAMPK level was measured in heart to investigate whether the effect of metformin was mediated by AMPK activation. Chronic subcutaneous infusion of metformin for 1 week did not affect the pAMPK level in heart, whereas it increased pAMPK level in skeletal muscle (Fig. 4). Furthermore, subcutaneous infusion of 150 mg/kg/24 h metformin did not increase the pAMPK level at 2, 4, 24 and 48 h in heart (Fig. 5A). The pAMPK level was also determined in heart after the intraperitoneal injection of 10 mg/kg of metformin in mice and pAMPK level was increased by metformin (Fig. 5B). This result suggests that although metformin could function as AMPK activator in mice heart, chronic subcutaneous infusion of 150 mg/kg metformin did not activate AMPK in heart.
Fig. 4.
AMPK activity measured as phosphorylation of AMPK (pAMPK) in heart (A) and skeletal muscle (B) of saline (control), isoproterenol (ISO), metformin (MET) or metformin with isoproterenol (MET+ISO) infused mice for 1 week using osmotic minipumps. Experimental cases are 6~9. *p<0.05 vs. Control.
Fig. 5.
AMPK activity measured as phosphorylation of AMPK (pAMPK) in heart. Metformin (150 mg/kg/24 h) was subcutaneously infused using osmotic minipump for 2, 4, 24, and 48 h (A). Metformin (10 mg/kg) was intraperitoneally injected into mice and pAMPK and AMPK level were measured 1 h after injection (B). Control mice were treated with saline. Experimental cases are 5~7. *p<0.05 vs. Saline.
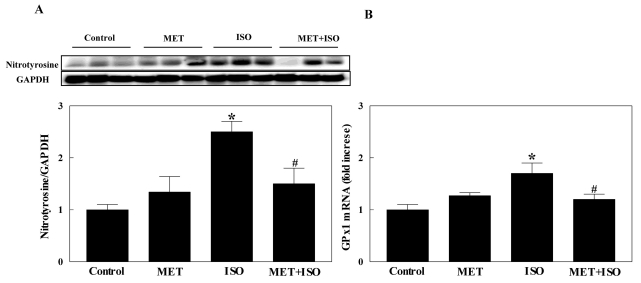
Nitrotyrosine and glutathione peroxidase
To ascertain the mechanism of the inhibitory effect of metformin on isoproterenol-induced cardiac hypertrophy, protein level of nitrotyrosine and gene expression of glutathione peroxidase 1 were measured in heart. The protein level of nitrotyrosine was increased in isoproterenol-infused heart and coinfusion of isoproterenol with metformin reversed nitrotyrosine level. Measurement of glutathione peroxidase 1 mRNA showed the same pattern of changes (Fig. 6). These results suggest that isoproterenol infusion increased oxidative stress and metformin treatment suppressed oxidative stress.
Fig. 6.
Nitrotyrosine level (A) and gene expression of glutathione peroxidase 1 (GPx1) (B) in heart of saline (control), isoproterenol (ISO), metformin (MET) or metformin with isoproterenol (MET+ISO) infused mice for 1 week using osmotic minipumps. Data is expressed as mean±SE. Experimental cases are 6~9. *p<0.05 vs. Control and #p<0.05 vs. ISO.
DISCUSSION
The present study demonstrates that chronic coinfusion of metformin with isoproterenol partially inhibits isoproterenol-induced cardiac hypertrophy that accompanies reduced oxidative stress. Metformin has beneficial effects on heart in human and experimental animals, decreasing cardiovascular mortality and the risk of myocardial infarct in humans and improving left ventricular functions in experimental animals [15-17,19]. Although metformin reduces protein synthesis in cardiac myocyte [22], it is unknown whether metformin inhibits cardiac hypertrophy. Presently metformin partially inhibited isoproterenol-induced cardiac hypertrophy in mice. To our knowledge, this is the first study showing that metformin might also have beneficial effects against cardiac hypertrophy.
Cardiac hypertrophy is associated with increases of cytokines including IL-6, TGF-β, and ANP. Isoproterenol increases IL-6 expression in the heart of rodents [6,23] and IL-6 transgenic mice display increased left ventricular wall thickness [24]. TGF-β is increased in an animal model of pressure overload hypertrophy [25] and in the hearts of patients with cardiomyopathy [26]. Hypertrophic stimulus also increases ANP expression [27]. Consistent with these previous reports, isoproterenol presently increased the expression of IL-6, TGF-β, and ANP, and metformin partially normalized the increments of these cytokines in heart. Together with reduction of heart weight, attenuated expression of these cytokines in heart supports the therapeutic effect of metformin in cardiac hypertrophy. Furthermore, the increased expression of collagen I and III and MMP-2 by isoproterenol was suppressed by metformin. Since collagen and MMP are involved in cardiac fibrosis and are increased by catecholamine [28,29], reduced expression of these genes by metformin also support the beneficial effect of metformin in cardiac hypertrophy.
One possible mechanism involved in the inhibitory effect of metformin on cardiac hypertrophy may be the attenuation of oxidative stress. This notion is supported by the fact that metformin presently reduced isoproterenol-induced increased nitrotyrosine level. Isoproterenol increases inducible nitric oxide synthase (iNOS), leading greater amounts of nitric oxide (NO) compared to other types of NOS, and is induced under various pathologic conditions [30,31]. NO can be transformed in a reaction with superoxide free radical (O2-) to form peroxynitrite (ONOO-) [32]. Peroxynitrite can nitrate proteins, which can lead to protein dysfunction [32]. One of the few identified nitrated protein is nitrotyrosine, which is a marker of peroxynitrite production and nitrosative stress [33]. In agreement with our result, hypertrophied heart shows increased nitrotyrosine levels and treatment of cardiac hypertrophy is accompanied with reduced oxidative stress including an attenuated nitrotyrosine level [34,35]. Moreover, isoproterenol presently increased antioxidant enzyme glutathione peroxidase 1, which was normalized by metformin. We speculated that the antioxidant enzyme is increased to protect the heart from hypertrophy and that metformin treatment reduces hypertrophy, which leads to normalization of the antioxidant enzyme.
A variety of effects of metformin are mediated by activation of AMPK. Metformin activates AMPK in hepatocytes which leads to increased lipid oxidation, reduced lipid synthesis and inhibited glucose production [36]. Activation of AMPK by metformin in cardiovascular tissues also mediates a protective effect. Metformin attenuates increased expression of adhesion molecules and apoptosis by high glucose through activation of AMPK in endothelial cells [18]. AMPK activation by metformin also prevents myocardial infarction and reperfusion injury in experimental animal [37,38]. The antioxidant effect of metformin is also mediated by AMPK activation. Treatment with metformin protects cultured cardiomyocytes from cell death during exposure to hydrogen peroxide via AMPK activation [37]. Metformin reduces intracellular reactive oxygen species induced by palmitate that is mediated by AMPK activation [39]. Presently acute intraperitoneal injection of 10 mg/kg metformin increases AMPK phosphorylation suggesting that metformin can activate AMPK phosphorylation in mice hearts. However, chronic subcutaneous infusion of 150 mg/kg/24 h metformin did not activate AMPK phosphorylation in heart. In agreement with our study, an AMPK-independent effect of metformin was recently reported, in which the administration of 2 mM metformin did not alter AMPK activity in the heart of Sprague-Dawley rats and H9C2 cells although metformin altered fatty acid oxidation and glucose utilization [40]. Metformin also does not increase AMPK activity in mice liver, while it reduces alcohol-induced hepatic lipid accumulation [41]. Whereas metformin alone does not increase AMPK activity, it enhances the activation effect of dehydroepiandrosterone (DHEA) on AMPK activity in mice ovaries [42]. The mechanism of the differential effect of metformin on AMPK activation remains unclear. It is possible that the dose of metformin and the methods of administration are involved. Further studies are needed to clear it.
Overall, metformin partially inhibits isoproterenol-induced cardiac hypertrophy that may be contributed by reduced oxidative stress. This study provides more supportive data concerning the beneficial effect of metformin in terms of the cardiac protective effect on heart.
ACKNOWLEDGEMENTS
This work was supported by the Korea Science and Engineering Foundation (KOSEF) grant funded by the Korea government (2009-0076238 and 2010-0007389).
ABBREVIATIONS
- AMPK
AMP-activated protein kinase
- ANP
atrial natriuretic peptide
- GPx1
glutathione peroxidase 1
- IL-6
interleukin-6
- MMP-2
matrix metallopeptidase 2
- MMP-9
matrix metallopeptidase 9
- TGF-β
transforming growth factor-β
References
- 1.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322:1561–1566. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 2.Barry SP, Davidson SM, Townsend PA. Molecular regulation of cardiac hypertrophy. Int J Biochem Cell Biol. 2008;40:2023–2039. doi: 10.1016/j.biocel.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 3.Corea L, Bentivoglio M, Verdecchia P. Echocardiographic left ventricular hypertrophy as related to arterial pressure and plasma norepinephrine concentration in arterial hypertension. Reversal by atenolol treatment. Hypertension. 1983;5:837–843. doi: 10.1161/01.hyp.5.6.837. [DOI] [PubMed] [Google Scholar]
- 4.Greenwood JP, Scott EM, Stoker JB, Mary DA. Hypertensive left ventricular hypertrophy: relation to peripheral sympathetic drive. J Am Coll Cardiol. 2001;38:1711–1717. doi: 10.1016/s0735-1097(01)01600-x. [DOI] [PubMed] [Google Scholar]
- 5.Schlaich MP, Kaye DM, Lambert E, Sommerville M, Socratous F, Esler MD. Relation between cardiac sympathetic activity and hypertensive left ventricular hypertrophy. Circulation. 2003;108:560–565. doi: 10.1161/01.CIR.0000081775.72651.B6. [DOI] [PubMed] [Google Scholar]
- 6.Cha HN, Hong GR, Kim YW, Kim JY, Dan JM, Park SY. Deficiency of iNOS Does Not Prevent Isoproterenol-induced Cardiac Hypertrophy in Mice. Korean J Physiol Pharmacol. 2009;13:153–159. doi: 10.4196/kjpp.2009.13.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shantz LM, Feith DJ, Pegg AE. Targeted overexpression of ornithine decarboxylase enhances beta-adrenergic agonist-induced cardiac hypertrophy. Biochem J. 2001;358:25–32. doi: 10.1042/0264-6021:3580025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osadchii OE. Cardiac hypertrophy induced by sustained beta-adrenoreceptor activation: pathophysiological aspects. Heart Fail Rev. 2007;12:66–86. doi: 10.1007/s10741-007-9007-4. [DOI] [PubMed] [Google Scholar]
- 9.Krenek P, Kmecova J, Kucerova D, Bajuszova Z, Musil P, Gazova A, Ochodnicky P, Klimas J, Kyselovic J. Isoproterenol-induced heart failure in the rat is associated with nitric oxide-dependent functional alterations of cardiac function. Eur J Heart Fail. 2009;11:140–146. doi: 10.1093/eurjhf/hfn026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Szabo J, Csaky L, Szegi J. Experimental cardiac hypertrophy induced by isoproterenol in the rat. Acta Physiol Acad Sci Hung. 1975;46:281–285. [PubMed] [Google Scholar]
- 11.Abbasi F, Chu JW, McLaughlin T, Lamendola C, Leary ET, Reaven GM. Effect of metformin treatment on multiple cardiovascular disease risk factors in patients with type 2 diabetes mellitus. Metabolism. 2004;53:159–164. doi: 10.1016/j.metabol.2003.07.020. [DOI] [PubMed] [Google Scholar]
- 12.Rossetti L, DeFronzo RA, Gherzi R, Stein P, Andraghetti G, Falzetti G, Shulman GI, Klein-Robbenhaar E, Cordera R. Effect of metformin treatment on insulin action in diabetic rats: in vivo and in vitro correlations. Metabolism. 1990;39:425–435. doi: 10.1016/0026-0495(90)90259-f. [DOI] [PubMed] [Google Scholar]
- 13.Stafford JM, Elasy T. Treatment update: thiazolidinediones in combination with metformin for the treatment of type 2 diabetes. Vasc Health Risk Manag. 2007;3:503–510. [PMC free article] [PubMed] [Google Scholar]
- 14.Perriello G, Misericordia P, Volpi E, Santucci A, Santucci C, Ferrannini E, Ventura MM, Santeusanio F, Brunetti P, Bolli GB. Acute antihyperglycemic mechanisms of metformin in NIDDM. Evidence for suppression of lipid oxidation and hepatic glucose production. Diabetes. 1994;43:920–928. doi: 10.2337/diab.43.7.920. [DOI] [PubMed] [Google Scholar]
- 15.Johnson JA, Majumdar SR, Simpson SH, Toth EL. Decreased mortality associated with the use of metformin compared with sulfonylurea monotherapy in type 2 diabetes. Diabetes Care. 2002;25:2244–2248. doi: 10.2337/diacare.25.12.2244. [DOI] [PubMed] [Google Scholar]
- 16.Johnson JA, Simpson SH, Toth EL, Majumdar SR. Reduced cardiovascular morbidity and mortality associated with metformin use in subjects with Type 2 diabetes. Diabet Med. 2005;22:497–502. doi: 10.1111/j.1464-5491.2005.01448.x. [DOI] [PubMed] [Google Scholar]
- 17.Kao J, Tobis J, McClelland RL, Heaton MR, Davis BR, Holmes DR, Jr, Currier JW. Relation of metformin treatment to clinical events in diabetic patients undergoing percutaneous intervention. Am J Cardiol. 2004;93:1347–1350. A1345. doi: 10.1016/j.amjcard.2004.02.028. [DOI] [PubMed] [Google Scholar]
- 18.Davis BJ, Xie Z, Viollet B, Zou MH. Activation of the AMP-activated kinase by antidiabetes drug metformin stimulates nitric oxide synthesis in vivo by promoting the association of heat shock protein 90 and endothelial nitric oxide synthase. Diabetes. 2006;55:496–505. doi: 10.2337/diabetes.55.02.06.db05-1064. [DOI] [PubMed] [Google Scholar]
- 19.Gundewar S, Calvert JW, Jha S, Toedt-Pingel I, Ji SY, Nunez D, Ramachandran A, Anaya-Cisneros M, Tian R, Lefer DJ. Activation of AMP-activated protein kinase by metformin improves left ventricular function and survival in heart failure. Circ Res. 2009;104:403–411. doi: 10.1161/CIRCRESAHA.108.190918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Masson S, Arosio B, Luvara G, Gagliano N, Fiordaliso F, Santambrogio D, Vergani C, Latini R, Annoni G. Remodelling of cardiac extracellular matrix during beta-adrenergic stimulation: upregulation of SPARC in the myocardium of adult rats. J Mol Cell Cardiol. 1998;30:1505–1514. doi: 10.1006/jmcc.1998.0714. [DOI] [PubMed] [Google Scholar]
- 21.Hori Y, Kunihiro S, Sato S, Yoshioka K, Hara Y, Kanai K, Hoshi F, Itoh N, Higuchi S. Doxycycline attenuates isoproterenol-induced myocardial fibrosis and matrix metalloproteinase activity in rats. Biol Pharm Bull. 2009;32:1678–1682. doi: 10.1248/bpb.32.1678. [DOI] [PubMed] [Google Scholar]
- 22.Chan AY, Soltys CL, Young ME, Proud CG, Dyck JR. Activation of AMP-activated protein kinase inhibits protein synthesis associated with hypertrophy in the cardiac myocyte. J Biol Chem. 2004;279:32771–32779. doi: 10.1074/jbc.M403528200. [DOI] [PubMed] [Google Scholar]
- 23.Mikaelian I, Coluccio D, Morgan KT, Johnson T, Ryan AL, Rasmussen E, Nicklaus R, Kanwal C, Hilton H, Frank K, Fritzky L, Wheeldon EB. Temporal gene expression profiling indicates early up-regulation of interleukin-6 in isoproterenol-induced myocardial necrosis in rat. Toxicol Pathol. 2008;36:256–264. doi: 10.1177/0192623307312696. [DOI] [PubMed] [Google Scholar]
- 24.Tanaka T, Kanda T, Itoh T, Tsugawa H, Takekoshi N, Yamakawa J, Kurimoto M, Kurabayashi M. Increased cardiac weight in interleukin-6 transgenic mice with viral infection accompanies impaired expression of natriuretic peptide genes. Res Commun Mol Pathol Pharmacol. 2001;110:275–283. [PubMed] [Google Scholar]
- 25.Villarreal FJ, Dillmann WH. Cardiac hypertrophy-induced changes in mRNA levels for TGF-beta 1, fibronectin, and collagen. Am J Physiol. 1992;262:H1861–H1866. doi: 10.1152/ajpheart.1992.262.6.H1861. [DOI] [PubMed] [Google Scholar]
- 26.Li RK, Li G, Mickle DA, Weisel RD, Merante F, Luss H, Rao V, Christakis GT, Williams WG. Overexpression of transforming growth factor-beta1 and insulin-like growth factor-I in patients with idiopathic hypertrophic cardiomyopathy. Circulation. 1997;96:874–881. doi: 10.1161/01.cir.96.3.874. [DOI] [PubMed] [Google Scholar]
- 27.Schmechel A, Grimm M, El-Armouche A, Hoppner G, Schwoerer AP, Ehmke H, Eschenhagen T. Treatment with atorvastatin partially protects the rat heart from harmful catecholamine effects. Cardiovasc Res. 2009;82:100–106. doi: 10.1093/cvr/cvp005. [DOI] [PubMed] [Google Scholar]
- 28.Briest W, Rassler B, Deten A, Zimmer HG. Norepinephrine-induced cardiac hypertrophy and fibrosis are not due to mast cell degranulation. Mol Cell Biochem. 2003;252:229–237. doi: 10.1023/a:1025596404975. [DOI] [PubMed] [Google Scholar]
- 29.Yamada T, Nagata K, Cheng XW, Obata K, Saka M, Miyachi M, Naruse K, Nishizawa T, Noda A, Izawa H, Kuzuya M, Okumura K, Murohara T, Yokota M. Long-term administration of nifedipine attenuates cardiac remodeling and diastolic heart failure in hypertensive rats. Eur J Pharmacol. 2009;615:163–170. doi: 10.1016/j.ejphar.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 30.Lin Y, Wang LN, Xi YH, Li HZ, Xiao FG, Zhao YJ, Tian Y, Yang BF, Xu CQ. L-arginine inhibits isoproterenol-induced cardiac hypertrophy through nitric oxide and polyamine pathways. Basic Clin Pharmacol Toxicol. 2008;103:124–130. doi: 10.1111/j.1742-7843.2008.00261.x. [DOI] [PubMed] [Google Scholar]
- 31.Kelly RA, Balligand JL, Smith TW. Nitric oxide and cardiac function. Circ Res. 1996;79:363–380. doi: 10.1161/01.res.79.3.363. [DOI] [PubMed] [Google Scholar]
- 32.Torres SH, De Sanctis JB, de L Briceño M, Hernandez N, Finol HJ. Inflammation and nitric oxide production in skeletal muscle of type 2 diabetic patients. J Endocrinol. 2004;181:419–427. doi: 10.1677/joe.0.1810419. [DOI] [PubMed] [Google Scholar]
- 33.Beckman JS, Koppenol WH. Nitric oxide, superoxide, and peroxynitrite: the good, the bad, and ugly. Am J Physiol. 1996;271:C1424–C1437. doi: 10.1152/ajpcell.1996.271.5.C1424. [DOI] [PubMed] [Google Scholar]
- 34.Nadruz W, Jr, Lagosta VJ, Moreno H, Jr, Coelho OR, Franchini KG. Simvastatin prevents load-induced protein tyrosine nitration in overloaded hearts. Hypertension. 2004;43:1060–1066. doi: 10.1161/01.HYP.0000124252.43470.2c. [DOI] [PubMed] [Google Scholar]
- 35.Balta N, Stoian I, Petec C, Petec G. Decreased SOD activity and increased nitrates level in rat heart with left ventricular hypertrophy induced by isoproterenol. Rom J Physiol. 1999;36:175–182. [PubMed] [Google Scholar]
- 36.Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, Musi N, Hirshman MF, Goodyear LJ, Moller DE. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest. 2001;108:1167–1174. doi: 10.1172/JCI13505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sasaki H, Asanuma H, Fujita M, Takahama H, Wakeno M, Ito S, Ogai A, Asakura M, Kim J, Minamino T, Takashima S, Sanada S, Sugimachi M, Komamura K, Mochizuki N, Kitakaze M. Metformin prevents progression of heart failure in dogs: role of AMP-activated protein kinase. Circulation. 2009;119:2568–2577. doi: 10.1161/CIRCULATIONAHA.108.798561. [DOI] [PubMed] [Google Scholar]
- 38.Solskov L, Lofgren B, Kristiansen SB, Jessen N, Pold R, Nielsen TT, Botker HE, Schmitz O, Lund S. Metformin induces cardioprotection against ischaemia/reperfusion injury in the rat heart 24 hours after administration. Basic Clin Pharmacol Toxicol. 2008;103:82–87. doi: 10.1111/j.1742-7843.2008.00234.x. [DOI] [PubMed] [Google Scholar]
- 39.Hou X, Song J, Li XN, Zhang L, Wang X, Chen L, Shen YH. Metformin reduces intracellular reactive oxygen species levels by upregulating expression of the antioxidant thioredoxin via the AMPK-FOXO3 pathway. Biochem Biophys Res Commun. 2010;396:199–205. doi: 10.1016/j.bbrc.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 40.Saeedi R, Parsons HL, Wambolt RB, Paulson K, Sharma V, Dyck JR, Brownsey RW, Allard MF. Metabolic actions of metformin in the heart can occur by AMPK-independent mechanisms. Am J Physiol Heart Circ Physiol. 2008;294:H2497–H2506. doi: 10.1152/ajpheart.00873.2007. [DOI] [PubMed] [Google Scholar]
- 41.Bergheim I, Guo L, Davis MA, Lambert JC, Beier JI, Duveau I, Luyendyk JP, Roth RA, Arteel GE. Metformin prevents alcohol-induced liver injury in the mouse: Critical role of plasminogen activator inhibitor-1. Gastroenterology. 2006;130:2099–2112. doi: 10.1053/j.gastro.2006.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Elia E, Sander V, Luchetti CG, Solano ME, Di Girolamo G, Gonzalez C, Motta AB. The mechanisms involved in the action of metformin in regulating ovarian function in hyperandrogenized mice. Mol Hum Reprod. 2006;12:475–481. doi: 10.1093/molehr/gal057. [DOI] [PubMed] [Google Scholar]