Abstract
We used a panel of monoclonal antibodies to H9 hemagglutinin to select 18 escape mutants of mouse-adapted influenza A/Swine/Hong Kong/9/98 (H9N2) virus. Cross-reactions of the mutants with the antibodies and the sequencing of hemagglutinin genes revealed two minimally overlapping epitopes. We mapped the amino acid changes to two areas of the recently reported three-dimensional structure of A/Swine/Hong Kong/9/98 hemagglutinin. The grouping of the antigenically relevant amino acid positions in H9 hemagglutinin differs from the pattern observed in H3 and H5 hemagglutinins. Several positions in site B of H3 hemagglutinin are distributed in two sites of H9 hemagglutinin. Unlike any subtype analyzed so far, H9 hemagglutinin does not contain an antigenic site corresponding to site A in H3 hemagglutinin. Positions 145 and 193 (H3 numbering), which in H3 hemagglutinin belong to sites A and B, respectively, are within one site in H9 hemagglutinin. This finding is consistent with the peculiarity of the three-dimensional structure of the H9 molecule, that is, the absence from H9 hemagglutinin of the lateral loop that forms site A in H3 and the equivalent site in H5 hemagglutinins. The escape mutants analyzed displayed phenotypic variations, including decreased virulence for mice and changes in affinity for sialyl substrates. Our results demonstrate a correlation between intersubtype differences in three-dimensional structure and variations among subtypes in the distribution of antigenic areas. Our findings also suggest that covariation and pleiotropic effects of antibody-selected mutations may be important in the evolution of H9 influenza virus, a possible causative agent of a future pandemic.
Only a few of the 15 antigenic subtypes of influenza A virus hemagglutinin (HA) have been structurally characterized and antigenically mapped. More than two decades ago, in the classic work of Wiley et al. (29), the HA molecule of the H3 subtype was characterized by sequencing the HA of antigenic drift variants and escape mutants, and the antigenic epitopes were mapped on the molecule's three-dimensional structure. Soon after that, in 1982, the antigenic sites of H1 were mapped on the three-dimensional structure of H3 (1). Recently, similar studies were performed for the H2 subtype (25). In 1990, the HA of an avian-pathogenic influenza virus A/Turkey/Ontario/7732/66 (H5N9) was mapped (19), but with limited data; only six amino acid changes were detected in five epitopes, so only the locations of the antigenic sites could be revealed, not their extent and fine structure. In all of these studies on the H1, H2, H3, and H5 subtypes, the antigenic sites were mapped on the three-dimensional structure of H3, the only one available at the time.
After the outbreak of H5N1 infection in humans in Hong Kong in 1997 (2) and the isolation of H9N2 virus from two human cases in 1999 (17), the HAs of H5 and H9 received more attention. Recently, the X-ray crystallographic structures of the H5 and H9 HA molecules were presented and analyzed (8, 9). The H5 strain used for X-ray analysis was closely related to the virus that caused the 1997 Hong Kong outbreak, and the strain of the H9 subtype was a swine isolate, A/Swine/Hong Kong/9/98, that shared some important features, such as the structure of its receptor-binding site, with human H9 isolates (18).
In our previous studies (10), we attempted to elucidate the detailed structure of antigenic sites on H5 HA. We analyzed single, double, and triple escape mutants of A/Mallard/Pennsylvania/10218/84 (H5N2) virus and mapped the amino acid changes on the three-dimensional structure of H5 HA. Thus, the antigenic mapping was performed on the three-dimensional structure of a strain of the same subtype as the strain analyzed, unlike previous studies in which all subtypes were mapped on the H3 structure. The results allowed us to reveal two antigenic sites: one corresponding to site A in H3 HA and the other containing three topographically close areas corresponding, in part, to site B in the H3 structure and partially overlapping site Sa in the H1 HA.
Here we describe the antigenic analysis of H9 HA performed with the use of the selection of escape mutants. We analyzed A/Swine/Hong Kong/9/98, the strain used to determine the three-dimensional structure of H9 HA by X-ray crystallography (8, 9). We used the mouse-adapted variant rather than the original swine virus because the goal of our studies was not limited by the antigenic mapping of HA. It also included the analysis of the phenotypic variations of the escape mutants, especially changes in virulence, and this was much easier to register in a mouse-adapted virus. On the other hand, the changes in HA associated with adaptation to mice are usually minimal (7, 24), and the use of a three-dimensional model of the original strain for the antigenic mapping of a mouse-adapted variant seemed appropriate. The use of the same virus for crystallographic and antigenic studies has been done only once, for H3 HA (29). In the present study, we found that certain peculiar features of the three-dimensional structure of H9 HA are reflected in the relationships between the antigenic areas. We also describe the effect of the amino acid changes in the escape mutants on their phenotypic features, such as virulence in mice and affinity for sialic acid receptors.
MATERIALS AND METHODS
Viruses.
The influenza virus A/Swine/Hong Kong/9/98 (H9N2) (Sw/HK/9/98; the HA sequence has GenBank accession number AF222810) (18), from the virus repository of the Department of Infectious Diseases at St Jude Children's Research Hospital, was adapted to mice by lung-to-lung passage (see Results), and escape mutants were selected for study. The viruses were propagated in 10-day-old embryonated chicken eggs. The virus-containing allantoic fluid was stored at 4°C or at −70°C. For use in enzyme-linked immunosorbent assay (ELISA), virus was concentrated and partially purified by centrifuging the allantoic fluid at low speed, layering it on 20% (wt/wt) sucrose, and pelleting the virus by centrifugation at 23,000 rpm in an SW27.1 rotor at 4°C for 90 min.
MAbs.
We used a panel of 15 monoclonal antibodies (MAbs) to the HA of three H9N2 strains, including two antibodies to A/Quail/Hong Kong/G1/97, MAbs G1-26 and G1-29; three antibodies to A/Chicken/Hong Kong/G9/97, MAbs G9-6, G9-25, and G9-27; and 10 antibodies to A/Duck/Hong Kong/Y280/97, MAbs 19A10, 7B10, 18B1, 18B10, 8C4, 3D11, 2F4, 15F1, 4G3, and 18G4.
Ascites fluids containing the antibodies were prepared by the method described by Kohler and Milstein (11). Briefly, female, 8-week-old BALB/c mice (Jackson Laboratory, Bar Harbor, Maine) were infected intranasally with a 50% egg-infective dose (EID50) of virus of approximately 105.0 to 106.0 per mouse, depending on the virus. These doses caused morbidity but not mortality. One month after infection, the mice were immunized by intraperitoneal injection of 104.0 hemagglutinating units of concentrated and purified virus with incomplete Freund's adjuvant (Gibco-BRL, Life Technologies, Inc., Grand Island, N.Y.), and 2 and 4 weeks later, mice were given booster intravenous injections of the same virus at the same dose. Three days after the second booster injection, the mice were sacrificed and their spleens were removed and disrupted to obtain splenocytes, which were fused 2 days later (on day 5 after the second boost). Hybridoma cells and antibodies were produced and sorted by Rockland Immunochemical, Inc. (Gilbertsville, Pa.).
Serologic methods.
ELISA was performed essentially as described by Philpott et al. (19) with modifications described in our previous paper (10). Hemagglutination inhibition (HI) was performed by a standard method (16).
Selection of escape mutants.
The escape mutants were selected with a two-step protocol, essentially as described in our earlier paper on H5 virus (10). Virus was incubated with an excess of antibody for 1 h at 20°C, and the mixture was inoculated into 10-day-old embryonated chicken eggs. Virus was harvested and cloned in embryonated chicken eggs by the limiting-dilution method. The first-generation mutants (one-step escape mutants) underwent further selection with the antibodies to which each mutant retained sensitivity, and the resistant variants (two-step escape mutants) were cloned.
PCR amplification and sequencing.
Viral RNA was isolated from virus-containing allantoic fluid with the RNeasy Mini kit (Qiagen, Valencia, Calif.) as specified by the manufacturer. Uni-12 primer was used for reverse transcription. PCR was performed with primers specific for the HA gene segment (primer sequences are available on request). PCR products were purified with the QIAquick PCR purification kit (Qiagen). The sequencing reaction was performed by the Hartwell Center for Bioinformatics and Biotechnology at St. Jude Children's Research Hospital. The DNA template was sequenced with rhodamine or dRhodamine dye terminator cycle-sequencing Ready Reaction kits with AmpliTaq DNA polymerase FS (Perkin-Elmer, Applied Biosystems, Inc., Foster City, Calif.) and synthetic oligonucleotides. Samples were analyzed in a Perkin-Elmer Applied Biosystems model 373 or model 377 DNA sequencer. DNA sequences were completed and edited with the Lasergene sequence analysis software package (DNAStar, Madison, Wis.). Multiple-sequence alignments were performed according to the method of Ha et al. (8) with GeneDoc version 2.3 software (available at http://www.psc.edu/biomed/genedoc/gddl.htm).
Assay of virus binding to sialic acid-containing substrates.
The binding of the viruses to fetuin was performed in a direct solid-phase assay with the immobilized virus and horseradish peroxidase-conjugated fetuin (4). The affinity for 3′- and 6′-sialylglycopolymer obtained by conjugation of a 1-N-glycyl derivative of 3′-sialyllactose, 6′-sialyllactose, or 6′-sialyllactosamine with poly(4-phenylacrylate) (6) was evaluated in a competitive assay based on the inhibition of binding of peroxidase-labeled fetuin (14). The sialoglycopolymers were a gift of A. S. Gambaryan of the Institute of Poliomyelitis and Viral Encephalitides, Moscow, Russia.
Infection of mice.
White outbred female mice weighing 6 to 8 g (purchased from the Laboratory Animal Breeding Institution of the Russian Academy of Medical Sciences, Andreevka, Moscow Region, Russia) were lightly anesthetized with ethyl ether and inoculated intranasally. Lung-to-lung passages were used to adapt the virus to mice: infected mice were sacrificed 2 days after inoculation, and a suspension of lung tissue was used for the passage. To assess virulence, the mice were inoculated with 50 μl of serial 10-fold dilutions of virus-containing allantoic fluid (six mice per dilution). Mouse mortality was registered for 10 days after inoculation and expressed as 50% mouse lethal doses (MLD50), calculated by the method of Reed and Muench (21).
Nucleotide sequence accession numbers.
The nucleotide sequences obtained in this study have been deposited in the GenBank database under accession numbers AY428485 to AY428504.
RESULTS
Adaptation of Sw/HK/9/98 virus to mice.
The goals of our studies were not only the elucidation of the antigenic structure of H9 HA, but also the analysis of the effect of the antibody-selected mutations on virus virulence. To increase the precision and ease of performance of our assessment of virulence, we attempted to increase the virulence of Sw/HK/9/98 virus for mice. We presumed that the amino acid changes in HA acquired during adaptation would be few, as occurs in the adaptation of other strains of influenza virus to mice (7, 24), allowing us to map the antigenic sites on the three-dimensional structure of the nonadapted strain. The nonadapted Sw/HK/9/98 virus killed mice if administered intranasally at a low dilution (106.5 EID50 or more per mouse). To increase the virus's virulence, we passaged the virus in mice in two parallel, independent series of lung-to-lung passages, 10 passages in each series. After the 10th passage, the viruses were subjected to limiting-dilution cloning in embryonated chicken eggs. Our assessment of virulence in mice demonstrated that one of the passaged variants (designated Sw/HK/9/98-MA, where MA stands for mouse adapted) acquired an increased ability to kill mice, whereas the other variant (designated Sw/HK/9/98-MP, where MP stands for mouse passaged) retained a low level of virulence, just slightly (albeit statistically significantly) above the virulence of the initial strain. As shown below, Sw/HK/9/98-MP exhibited a change in reaction with several antibodies. Therefore, we analyzed it alongside the escape mutants selected from Sw/HK/9/98-MA.
Selection of escape mutants.
Escape mutants of the virulent mouse-adapted variant Sw/HK/9/98-MA were selected in a two-step protocol with 10 anti-H9 antibodies with HI titers ranging from 1:3,200 to 1:204,800. In the first step, 10 mutants of Sw/HK/9/98-MA were selected, one mutant for each MAb (Table 1). The mutants were characterized by their cross-reaction with the 10 MAbs in the HI assay, and we chose five mutants (mG1-29, m7B10, m3D11, m15F1, and m18G4) for further selection with the antibodies to which each mutant retained sensitivity. Eight escape mutants were selected in the second step, and each mutant was designated by the antibodies sequentially used to select it (Table 1).
TABLE 1.
Sequential selection of escape mutants of mouse-adapted Sw/HK/9/98 (H9N2) influenza virus
| Escape mutants of Sw/HK/9/98 | Acquisition of resistance to indicated MAbs
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Ck/HK/G9/97 G9-27 | Qu/HK/G1/97 G1-29 | Dk/HK/Y280/97
|
||||||||
| 7B10 | 8C4 | 15F1 | 18G4 | 3D11 | 19A10 | 18B10 | 18B1 | |||
| One-step | mG9-27 | mG1-29 | m7B10 | m8C4 | m15F1 | m18G4 | m3D11 | m19A10 | m18B10 | m18B1 |
| Two-step | mG1-29-18G4 | m7B10-18G4, m7B10-18G4′, and 7B10-18B10 | m15F1-3D11 and m15F1-18B10 | m18G4-18B1 | m3D11-18G4 | |||||
Cross-reactions of antibodies with the mouse-adapted viruses and escape mutants of Sw/HK/9/98-MA.
The escape mutants and Sw/HK/9/98-MP were tested in HI and ELISA with all 15 MAbs (Table 2). The results of the HI assay and ELISA coincided in most cases except those for MAbs 19A10 and 7B10, which reacted with mutant m19A10 in the ELISA but not in the HI assay, and those for MAb 8C4, which behaved in this way with four mutants. All four mutants had a common amino acid change (see below).
TABLE 2.
Reactions of anti-HA MAbs with escape mutants of Sw/HK/9/98-MA in the HI assay and ELISA
| MAb | Reactiona with escape mutant:
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| m15F1 | Sw/HK/9/98-MP | mG9-27 | m18G4 | mG1-29 | m19A10 | m18B1 | m7B10 | m3D11 | m8C4 | m18B10 | m7B10-18G4 | m7B10-18G4′ | m18G4-18B1 | mG1-29-18G4 | m15F1-3D11 | m3D11-18G4 | m15F1-18B10 | m7B10-18B10 | |
| 15F1 | − | + | + | + | + | + | + | + | + | − | − | + | + | + | + | − | + | − | + |
| G9-27 | − | − | − | − | − | + | + | + | + | + | + | − | − | − | − | − | − | − | + |
| G9-6 | − | − | − | − | − | + | + | + | + | + | + | − | − | − | − | − | − | − | + |
| G1-26 | − | − | − | − | − | + | + | + | + | + | + | − | − | − | − | − | − | − | + |
| 18G4 | + | − | − | − | + | + | + | + | + | + | + | − | − | − | − | + | − | + | + |
| G9-25 | + | − | − | − | − | + | + | + | + | + | + | + | + | − | − | + | − | + | + |
| G1-29 | + | − | − | − | − | + | + | + | + | + | + | − | − | − | − | + | − | − | − |
| 19A10 | + | + | + | + | + | −* | − | + | + | + | + | + | + | − | + | + | + | + | + |
| 18B1 | + | + | + | + | + | − | − | − | − | + | + | − | − | − | + | − | − | − | − |
| 2F4 | + | + | + | + | + | − | − | − | − | + | + | − | − | − | + | − | − | − | − |
| 7B10 | + | + | + | + | + | −* | − | − | − | + | + | − | − | − | + | + | + | − | − |
| 3D11 | + | − | − | − | + | − | + | − | − | + | + | − | − | − | − | − | − | − | − |
| 4G3 | + | − | − | − | + | − | − | − | − | + | + | − | − | − | − | − | − | − | − |
| 8C4 | + | + | + | + | + | + | + | −* | −* | − | − | −* | −* | + | − | + | + | − | − |
| 18B10 | + | + | + | + | + | + | + | + | + | − | − | + | + | + | + | + | + | − | − |
+, HI titer similar to that obtained with wild-type virus (≤8-fold difference) and antibody-virus binding in ELISA >75%; −, HI titer at least 16 times less than that obtained with wild-type virus and binding in ELISA <25%; −*, HI titer at least 16 times less than that obtained with wild-type virus, but binding in ELISA >50%. Percent binding in ELISA was calculated from the equation A = 100 × (Bxv/Bpv), where A is the amount of antibody bound as a percentage of that binding to wild-type virus (100%), Bxv is binding of the MAb to the test virus, and Bpv is binding of pooled MAbs to the test virus.
The reactions of the antibodies and mutants revealed an array of epitopes partially overlapping one another in a complex pattern. The two-step mutants m18G4-18B1 and mG1-29-18G4 had an additive pattern. For example, m18G4-18B1 was resistant to antibodies that did not react with m18G4 and to those that did not react with m18B1. However, several two-step mutants exhibited a pattern of resistance deviating from additivity: m15F1-18B10 was resistant to several antibodies that bound mutants m15F1 and m18B10, and m7B10-18B10 was resistant to several antibodies that bound mutants m7B10 and m18B10. These discrepancies suggest that the amino acid changes selected by MAb 18B10 in the one-step mutants differed from the mutations selected by this MAb from m15F1 and m7B10 at the second selection step. This interpretation was confirmed by the sequencing data. Because most of the two-step mutants deviated from the additive pattern, we did not attempt to design an operational map with the cross-reaction data alone. Instead, such mapping was performed with the sequencing data on amino acid changes in the escape mutants.
Sequence analysis of the escape mutants.
We sequenced the HA genes of Sw/HK/9/98-MA, Sw/HK/9/98-MP, and the escape mutants and compared the encoded amino acid sequences (Table 3) with that of the initial Sw/HK/9/98 strain (GenBank accession number AF222810) (18). The low-virulence Sw/HK/9/98-MP, the virulent mouse-adapted Sw/HK/9/98-MA, and all the escape mutants derived from Sw/HK/9/98-MA differed from the initial strain by one amino acid change (P15S) in HA2. This substitution is far from the antigenically relevant areas, justifying our use of the three-dimensional structure of the original strain for the antigenic mapping of the mouse-adapted variant. The low-virulence variant Sw/HK/9/98-MP also had another substitution in HA1, S127N (S133N in H3 numbering), leading to the formation of a new glycosylation site. This substitution was also present in two one-step escape mutants, mG27 and m18G4. These three viruses exhibited the same pattern of reactions with the antibodies (see Table 2). This result suggests that the S127N change induces resistance to the eight antibodies G1-26, G1-29, G9-6, G9-25, G9-27, 3D11, 4G3, and 18G4. How this substitution was selected in Sw/HK/9/98-MP is not obvious, because lung-to-lung passage at 2-day intervals is unlikely to result in immune selection.
TABLE 3.
Amino acid substitutions in the HA of H9 escape mutants
| Virus | Substitution at positiona:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HA1
|
HA2, 15 (15) | |||||||||||
| 116 (109) | 133 (127) | 135 (129) | 145 (135) | 147 (137) | 157 (147) | 162 (152) | 189 (179) | 193 (183) | 198 (188) | 226 (216) | ||
| Sw/HK/9/98 (GenBank) | S | S | T | D | F | K | P | T | N | T | L | P |
| Sw/HK/9/98-MA | S | |||||||||||
| Sw/HK/9/98-MP | N | S | ||||||||||
| mG9-27 | N | S | ||||||||||
| m18G4 | N | S | ||||||||||
| mG1-29 | T | S | ||||||||||
| m3D11 | D | S | ||||||||||
| m7B10 | D | S | ||||||||||
| m18B1 | E | S | ||||||||||
| m18B10 | N | S | ||||||||||
| m8C4 | N | S | ||||||||||
| m19a10 | Q | S | ||||||||||
| m15F1 | L | S | ||||||||||
| m7B10-18G4 | I | K | D | S | ||||||||
| m7B10-18G4′ | K | D | S | |||||||||
| m18G4-18B1 | N | Q | S | |||||||||
| m7B10-18B10 | A | D | S | |||||||||
| m15F1-18B10 | L | T | S | |||||||||
| m15F1-3D11 | A | L | L | S | ||||||||
| m3D11-18G4 | N | D | S | |||||||||
| mG1-29-18G4 | N | T | S | |||||||||
Position numbers are for the H3 HA, with those for H9 HA in parentheses.
Another substitution creating a new glycosylation site, T188N (T198N in H3 numbering), was registered in one-step mutants m18B10 and m8C4. Notably, the substitutions selected by MAb 18B10 in the two-step mutants m7B10-18B10 and m15F1-18B10 occurred in positions other than 188. In m7B10-18B10, the position of the amino acid change selected by MAb 18B10 occurred at position 179 (189 in H3 numbering), whereas in m15F1-18B10 it occurred at the same position as in the one-step mutants selected by two other MAbs, m3D11 and m7B10. The substitution, however, was not the same; it was a conservative change, N183T (N193T in H3 numbering) rather than the nonconservative change (N183D) seen in m3D11 and m7B10.
A similar pattern of selection, that is, selection of different substitutions at the second selection step compared to the substitution in the one-step mutant, was observed for several MAbs. For example, MAb 18G4 selected the first-generation mutant m18G4 and the two-step mutants m3D11-18G4 and mG1-29-18G4, which had the glycosylation site-forming mutation S127N (S133N in H3 numbering). However, in m7B10-18G4 and m7B10-18G4′, MAb 18G4 selected a different mutation, T129K (T135K in H3 numbering), situated close to position 127 (133 in H3 numbering) but not forming a glycosylation site. MAb 3D11, which selected the amino acid change N183D (N193D in H3 numbering) in one-step mutant m3D11, selected other mutations, T129A and F137L (T135A and F147L in H3 numbering), in the two-step mutant m15F1-3D11. This mutant acquired resistance to four antibodies (MAbs 18B1, 2F4, 4G3, and 3D11) to which the one-step mutant m15F1 was sensitive.
One cannot unambiguously conclude which of the two mutations, T129A and F137L, is responsible for the additional range of resistance in the two-step mutant. MAb 18G4 reacted with mutant m15F1-3D11 but failed to react with another mutant carrying a mutation at position 129, m7B10-18G4. However, the substitution in m7B10-18G4, T129K (T135K in H3 numbering), was nonconservative, unlike mutation T129A in m15F1-3D11. Since it is not possible to make a conclusive choice between the amino acid changes T135A and F147L (H3 numbering) as the cause of resistance to MAbs acquired by m15F1-3D11 after the second selection step, we did not include the amino acid changes T135A and F147L in the antigenic map presented in Table 4 and Fig. 2. The two-step mutant m7B10-18G4 acquired two amino acid changes at the second selection step, S116I and T135K (H3 numbering). The substitution S116I is probably incidental because it is not present in mutant m7B10-18G4′, which reacts with the same antibodies as does m7B10-18G4 (Table 2).
TABLE 4.
Map of epitopes revealed by grouping amino acid changes recognized by individual antibodies in H9 escape mutantsa
| Epitope | MAb | Amino acid change(s) preventing HA-MAb interaction
|
||
|---|---|---|---|---|
| Site I | Overlapping area | Site II | ||
| I | 15F1 | P162L | T198N | |
| G9-27 | P162L, K157T, T135K | S133N | ||
| G9-6 | P162L, K157T, T135K | S133N | ||
| G1-26 | P162L, K157T, T135K | S133N | ||
| G1-29 | K157T, T135K | T189A, S133N | N193T | |
| G9-25 | K157T, T135K | S133N | ||
| 18G4 | T135K | S133N | ||
| II | 19A10 | L226Q, D145E | ||
| 18B1 | L226Q, N193D, D145E N193T | |||
| 2F4 | L226Q, N193D, D145E | |||
| 4G3 | S133N | L226Q, N193D, D145E N193T | ||
| 7B10 | L226Q, N193D, D145E N193T | |||
| 3D11 | S133N | L226Q, N193D N193T | ||
| 8C4 | T198N | N193D N193T | ||
| 18B10 | T198N, T189A | N193T | ||
Positions of amino acid substitutions are numbered according to H3 subtype of HA.
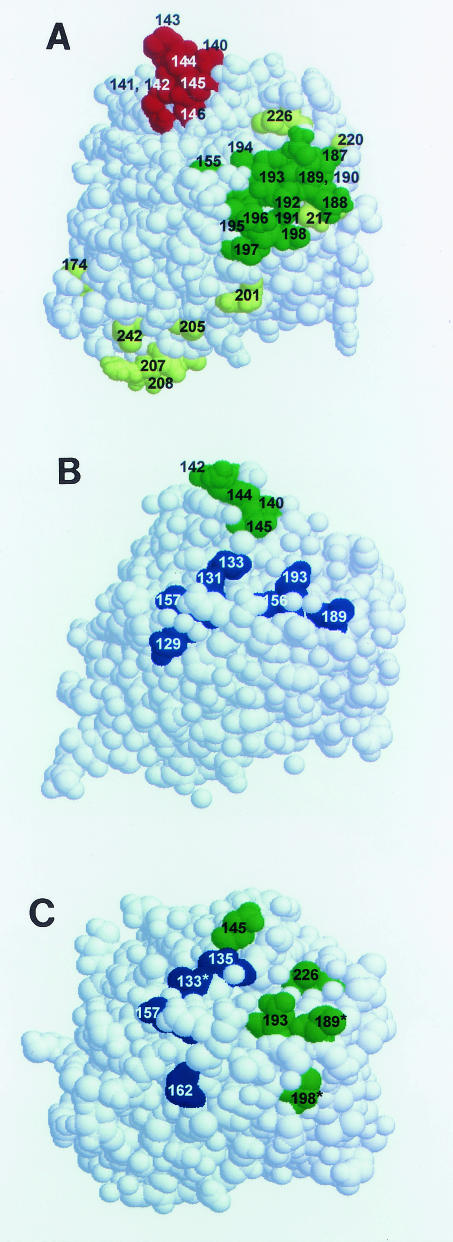
FIG. 2.
Antigenic sites on the globular head of HA of the H3 (A), H5 (B), and H9 (C) subtypes mapped on the three-dimensional structure of the molecule (top view). Images were created with RasMol 2.6, and HA structures are from the Protein Data Bank (PDB accession numbers 1HGF, 1JSM, and 1JSD, respectively). Antigenic sites in H3 (A) are marked in red, green, and yellow, corresponding to sites A, B,and D, respectively, described by Skehel and Wiley (23). Antigenic sites at the top of the H5 HA (B) and H9 HA (C) are shown in blue and green. Residue numbering corresponds to the HA of subtype H3. Residues in H9 contributing to the overlap of epitopes are marked by asterisks. H5 antigenic sites correspond to those given in our previous paper (10).
The positions of amino acid changes in the escape mutants were generally consistent with the immunologic relations revealed by the cross-reactions of the mutants with the antibodies (Table 2). If two MAbs used in a sequential way to obtain a two-step mutant selected two mutations identical to those selected by them in one-step mutants, the pattern of resistance to the MAbs was additive, whereas the pattern was not additive if the selection with a specific MAb produced different substitutions in a one-step mutant and in a two-step mutant. The relationships between the amino acid substitutions in escape mutants and the resistance of the mutants to the antibodies are presented in Table 4. We use the H3 numbering in Table 4 as well as in Tables 5 and 6 in order to facilitate the comparison of the antigenic maps of different subtypes.
TABLE 5.
Effect of amino acid changes in the HA of Sw/HK/9/98-MA virus on virulence in mice
| Virulence | Virus (amino acid change) | Virulencea (EID50/MLD50 ratio ± SE) |
|---|---|---|
| High | Sw/HK/9/98-MA | 4.01 ± 0.48 |
| m7B10 (N193D) | 3.64 ± 0.38 | |
| m18G4-18B1 (S133N, L226Q) | 3.73 ± 0.53 | |
| mG9-27 (S133N) | 3.96 ± 0.43 | |
| m3D11 (N193D) | 4.16 ± 0.08 | |
| m7B10-18G4′ (T135K, N193D) | 4.16 ± 0.44 | |
| m15F1-18B10 (N193T, P162L) | 4.28 ± 0.46 | |
| m18B1 (D145E) | 4.35 ± 0.16 | |
| m18G4 (S133N) | 4.36 ± 0.37 | |
| m15F1 (P162L) | 4.4 ± 0.47 | |
| m19A10 (L226Q) | 4.50 ± 0.25 | |
| m7B10-18G4 (S116I, T135K, N193D) | 4.57 ± 0.41 | |
| mG1-29 (K157T) | 4.58 ± 0.34 | |
| Moderate | mG1-29-18G4 (S133N, K157T) | 5.87 ± 0.29 |
| m3D11-18G4 (S133N, N193D) | 5.74 ± 0.44 | |
| Sw/HK/9/98-MP (S133N) | 5.64 ± 0.38 | |
| m15F1-3D11 (T135A, F147L, P162L) | 5.06 ± 0.59 | |
| m7B10-18B10 (N193D, T189A) | 4.95 ± 0.41 | |
| Low | m18B10 (T198N) | 7.06 ± 0.26 |
| m8C4 (T198N) | 7.20 ± 0.43 | |
| Sw/HK/9/98 | 6.74 ± 0.43 |
Expressed as log10 EID50/MLD50 ± standard error × tα,n−2, where tα is Student's coefficient with probability α (α = 0.95). Amino acids are numbered according to the HA of the H3 subtype.
TABLE 6.
Affinity of H9 escape mutants for sialyl substratesa
| Virus (amino acid change) |
Kd for substrate:
|
|||
|---|---|---|---|---|
| Fetuin | p3′SL | p6′SL | p6′SLN | |
| Sw/HK/9/98 | 2.43 ± 0.18 | >20 | 0.16 ± 0.03 | 0.18 ± 0.04 |
| Sw/HK/9/98-MA | 2.51 ± 0.12 | >20 | 0.19 ± 0.03 | 0.19 ± 0.03 |
| Sw/HK/9/98-MP (S133N) | 2.38 ± 0.12 | >20 | 0.19 ± 0.03 | 0.19 ± 0.01 |
| mG9-27 (S133N) | 2.47 ± 0.28 | >20 | 0.18 ± 0.02 | 0.19 ± 0.02 |
| m18G4 (S133N) | 2.35 ± 0.20 | >20 | 0.19 ± 0.03 | 0.23 ± 0.02 |
| mG1-29 (K157T) | 2.43 ± 0.16 | >20 | 0.23 ± 0.05 | 0.21 ± 0.03 |
| m18B1 (D145E) | 2.38 ± 0.35 | >20 | 0.19 ± 0.02 | 0.18 ± 0.01 |
| m7B10 (N193D) | 2.34 ± 0.30 | >20 | 0.63 ± 0.07 | 0.18 ± 0.02 |
| m3D11 (N193D) | 2.29 ± 0.15 | >20 | 0.65 ± 0.02 | 0.19 ± 0.02 |
| m15F1 (P162L) | 2.43 ± 0.19 | >20 | 0.51 ± 0.06 | 0.46 ± 0.06 |
| m19A10 (L226Q) | 2.58 ± 0.41 | 1.60 ± 0.22 | 0.86 ± 0.08 | 0.81 ± 0.06 |
| m18B10 (T198N) | 5.56 ± 0.13 | >20 | 2.09 ± 0.33 | 2.49 ± 0.27 |
| m8C4 (T198N) | 5.74 ± 0.52 | >20 | 1.90 ± 0.29 | 2.60 ± 0.32 |
| m18G4-18B1 (S133N, L226Q) | 2.31 ± 0.21 | 1.75 ± 0.14 | 0.87 ± 0.11 | 0.84 ± 0.07 |
| m7B10-18G4 (S116I, T135K, N193D) | 2.42 ± 0.24 | >20 | 0.68 ± 0.03 | 0.22 ± 0.05 |
| m7B10-18G4′ (T135K, N193D) | 2.55 ± 0.17 | >20 | 0.65 ± 0.07 | 0.22 ± 0.04 |
| m7B10-18B10 (N193D, T189A) | 2.50 ± 0.44 | >20 | 2.46 ± 0.34 | 2.87 ± 0.46 |
| m15F1-3D11 (P162L, F147L, T135A) | 2.23 ± 0.43 | >20 | 1.37 ± 0.22 | 1.16 ± 0.11 |
| m15F1-18B10 (P162L, N193T) | 2.22 ± 0.30 | >20 | 0.25 ± 0.04 | 0.25 ± 0.04 |
| mG1-29-18G4 (S133N, K157T) | 2.40 ± 0.26 | >20 | 0.45 ± 0.04 | 0.29 ± 0.02 |
| m3D11-18G4 (S133N, N193D) | 5.31 ± 0.53 | >20 | 1.15 ± 0.10 | 0.56 ± 0.05 |
In each case, Kd = mean ± SE × tα,n−1, where tα is Student's coefficient with probability α (α = 0.90) (micromolar sialic acid). Kd was calculated from results obtained in four independent experiments. p3′SL, 3′-sialyllactose on a polyacrylic carrier; p6′SL, 6′-sialyllactose on a polyacrylic carrier; p6′SLN, 6′-sialyllactosamine on a polyacrylic carrier. Amino acids are numbered according to the HA of the H3 subtype.
The pattern of resistance revealed the presence of two minimally overlapping epitopes, I and II, each consisting of several amino acid positions. The antibodies recognized either a whole epitope (e.g., MAbs G9-6 and 18B1) or a part of an epitope (e.g., MAbs 18G4 and 19A10). However, some antibodies (e.g., MAb G1-29) interacted with parts of both antigenic areas. The amino acid changes leading to the formation of glycosylation sites were recognized by the MAbs reacting with different epitopes: mutants mG9-27, m18G4, m18B10, and m8C4 failed to react with some antibodies recognizing epitope I and some antibodies recognizing epitope II. A likely explanation for such overlapping patterns of antibody binding is that the presence of an oligosaccharide chain may hinder the interaction of an antibody with the antigen some distance from the glycosylated amino acid, thus affecting the reaction of the antibody with distantly located parts of both epitopes (22).
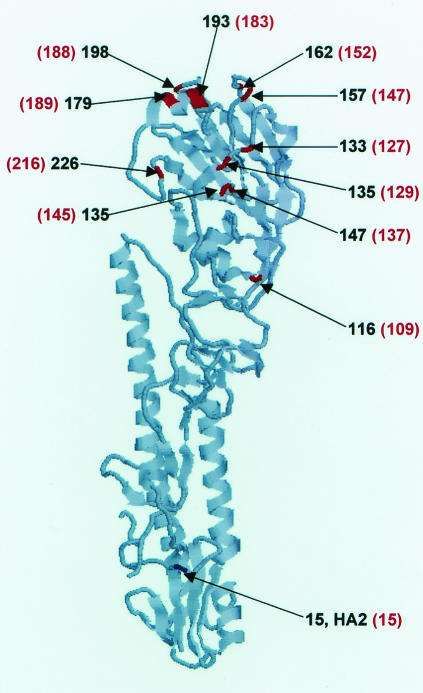
The mapping of the amino acid changes on the three-dimensional structure (8, 9) revealed the locations of the antigenically relevant amino acid changes in the upper part of the HA molecule (Fig. 1). A view from the top of the molecule (Fig. 2C) allowed us to visualize the areas interacting with different groups of monoclonal antibodies. The positions of the amino acid changes are consistent with the epitope map presented in Table 4, one area containing positions 129, 147, and 152 (135, 157, and 162 in H3 numbering), and the other containing positions 135, 183, and 216 (145, 193, and 226 in H3 numbering). The binding of MAb G1-29 to part of both epitopes I and II (see Table 4) is consistent with the location of these substitutions on the three-dimensional structure. The grouping of the amino acid changes in H9 HA is different from the pattern of antigenic sites in the H3 and H5 subtypes, as shown in the comparative top views of the H3, H5, and H9 HA molecules (Fig. 2A, B, and C).
FIG. 1.
Locations of the amino acid changes in the HA of H9 escape mutants mapped on the three-dimensional map of A/Swine/Hong Kong/9/98 HA (8). Amino acids were mapped on the three-dimensional structure with the RasMol 2.6 program (available at http://www.umass.edu/microbio/rasmol/getras.htm). Positions of amino acid changes detected by the binding of MAbs are shown in red, and the position of the change resulting from mouse adaptation is shown in blue. Numbering corresponds to the HA of subtype H3. H9 numbering (8) is presented in red in parentheses.
Virulence of H9 escape mutants in mice.
The virulence (EID50/MLD50 ratio) of the H9 escape mutants with the mutation T188N (T198N in H3 numbering) was similar to that of the nonadapted strain Sw/HK/9/98 (Table 5). The substitution T188N created a new glycosylation site. Previous studies have shown that the emergence of a new glycosylation site is associated with loss of virulence of an H5 virus (10) and with a decrease in receptor binding and cell fusion activity in H2 virus (26). In the present study, several double mutants had a moderate, although statistically significant, loss of virulence. The amino acid changes present in these moderately attenuated mutants did not significantly influence virulence when they were present as single mutations (i.e., in the one-step mutants), or, at least, the effect was too low to be revealed as statistically significant. Unlike the loss of virulence associated with the change T188N, which was registered in two independently selected escape mutants, the decrease in virulence of the double mutants cannot be unequivocally ascribed to the mutations recognized by the antibodies, because one cannot exclude a covariation effect produced by a change in a gene other than the HA gene. However, data on the affinity of the viruses to sialic acid substrates (see below) suggest that the decrease in virulence is connected to the changes in the HA. In contrast, the low virulence of Sw/HK/9/98-MP probably does not result from mutations in the HA of this virus. Both escape mutants carrying the mutation S127N were virulent, and the change P15S in HA2 was present in the virulent Sw/HK/9/98-MA and all its escape mutants.
Affinity of H9 escape mutants for sialic acid substrates.
One of the mechanisms by which a mutation in HA may affect virus virulence is by decreasing the affinity of HA for cell receptors. Previous reports have described a correlation between the decrease in affinity for sialic receptors and the loss of virulence (20), as well as changes in receptor binding in escape mutants (3). We surmised that the decrease in virulence of at least some H9 escape mutants resulted from their low affinity for sialic receptors. Moreover, two escape mutants, m19A10 and m18G4-18B1, had the amino acid substitution L216Q (L226Q in H3 numbering), which usually correlates with a shift in the affinity of HA from the human-type sialic receptors to the avian-type sialic receptors, that is, from a preference for a 2′-6′ link to a 2′-3′ link between the sialic acid residue and galactose.
We measured the affinity of the H9 escape mutants for high-molecular-weight sialic substrates, both natural (fetuin) and synthetic (3′- and 6′-sialyllactose and 6′-sialyllactosamine attached to a polyacrylic carrier). The affinity for the 3′ substrate was negligible in the wild-type virus and in all escape mutants except those carrying the L216Q (L226 in H3 numbering) change (Table 6). The latter exhibited an expressed affinity for the 3′-sialyllactose-acrylic polymer. Several escape mutants showed decreased affinity for polymer substrates containing 6′-sialyllactose or 6′-sialyllactosamine. The low-virulence mutants carrying the mutation T188N (T198N in H3 numbering), leading to the formation of a new glycosylation site (mutants m18B10 and m8C4), exhibited a sharp decrease in affinity for both synthetic 6′ substrates and fetuin. Several two-step mutants carrying two or three amino acid changes had a decreased affinity either for fetuin and the 6′-sialyllactose-containing polymer (m3D11-18G4) or for both synthetic 6′-polymer substrates (m7B10-18B10 and m15F1-3D11). These mutants had a moderately reduced virulence for mice (Table 5). Only one mutant with decreased virulence, mG1-29-18G4, had affinity values close to those observed for the wild-type virus.
DISCUSSION
Our analysis of the antigenic structure of H9 HA with escape mutants revealed a pattern of antigenically relevant areas that is distinctly different from those of the subtypes analyzed so far. The difference is not in the positions of the substitutions in the polypeptide chain of HA but rather in the grouping of the amino acid changes into antigenic sites, as revealed by immunologic analysis, and this grouping reflects the peculiar features of the three-dimensional structure of H9 HA (9). The unusual features of the antigenic map of H9 are especially evident in comparison with earlier findings on the antigenic structure of influenza A virus HAs of different subtypes. HA of subtypes H1 (1) and H2 (25) mapped on the three-dimensional structure of the H3 molecule show a pattern similar to that of H3 (29). Four antigenic sites in H1 HA correspond to sites in H3 HA, although no equivalent of site C in H3 HA could be found in H1 (1). H2 HA contained an additional site but had a pattern that was otherwise similar to the H3 HA pattern (25).
In our previous studies (10), we analyzed H5 HA with the three-dimensional structure of HA of a strain of this subtype (8). In an earlier work, the H5 molecule was studied to a limited extent with the use of the three-dimensional structure of H3 (19). In both studies, the epitopes revealed in H5 HA generally corresponded to the antigenic sites of H3 HA: four of five sites in H5 HA detected by Philpott et al. (19) corresponded to the sites of the H3 subtype, and two sites analyzed in detail in our earlier research (10) corresponded to sites A and B of the H3 molecule. The site in H5 HA corresponding to site B in H3 HA was more complex than site B in H3: it contained a part not involved in the H3 site B and partially overlapping site Sa in H1. However, the equivalence of site Sa in H1 to site B in H3 suggests that the H5 site described as group 1 by Philpott et al. (19) and as epitope I in our studies (10) is the equivalent of site B in H3 HA. The site designated epitope II in our studies (10) and group 5 by Philpott et al. (19) is obviously an exact equivalent of site A of H3 HA; that is, it comprises the loop at the lateral side of the HA globule (29).
In H9 the situation is entirely different. There are two partially overlapping antigenic sites at the top of the HA molecule (Fig. 2C). Site I in H9 HA contains positions that, in H3, belong to site A (position 135 in H3 numbering) and to site B (positions 157 and 162 in H3 numbering) (Fig. 2A). Site II in H9 HA contains, in H3 numbering, positions 145 (site A in H3), 193 (site B in H3), and 226 (site D in H3). This distribution of mutations in antigenic epitopes corresponds to the locations of the amino acid changes in the three-dimensional structure of Sw/HK/9/98 HA (Fig. 2C). The peculiarities in the allocation of amino acid positions to antigenic areas of the H9 molecule correspond to its conformational features (9): unlike H3 or H5 HA, the molecule of H9 HA does not have the lateral loop forming antigenic site A in H3 and the equivalent site in H5. Accordingly, the amino acid residues forming site A in H3 HA or the equivalent site in H5 (and, presumably, in H1 and H2) do not form a discrete antigenic area in H9: they belong to two different epitopes (Fig. 2).
Among the amino acid substitutions in H9 HA, the change L216Q (L226Q in H3 numbering) is of special interest. This position plays a prominent role in the receptor binding specificity of HA. The presence of glutamine in this position is characteristic of avian strains, whereas leucine is usual in human and swine influenza viruses (28). Although the selection of escape mutants with a substitution in position 226 and a changed receptor affinity has been described for the H3 subtype (3), the selection of H9 escape mutants with altered receptor-binding specificity may have special importance. Among H9 isolates, the swine and human strains invariably contain leucine in position 216 (226 in H3 numbering), whereas the avian viruses, including those circulating at present, contain either glutamine or leucine in this position (13, 15). The presence of leucine 226 (H3 numbering) in the H9 strains isolated from waterfowl was considered to favor the infection of humans (12).
The measurement of the affinity of H9 escape mutants for sialic acid-containing substrates confirmed the shift in receptor specificity of the escape mutant carrying mutation L216Q (L226Q in H3 numbering) to an avian-type receptor specificity (Table 6). The mutants with a reduced affinity for 6′-sialyl substrates, except those carrying the mutation N183D (N193D in H3 numbering), did not distinguish 6′-sialyllactose from 6′-sialyllactosamine. All the mutants with the N183D substitution had a reduced affinity for 6′-sialyllactose but not for 6′-sialyllactosamine, which is considered more similar to the human receptor than is 6′-sialyllactose (5). Therefore, the residue in position 183 may also be involved in the specificity of host cell recognition by H9 HA. These observations suggest that under natural conditions, immune selection can result in variants with altered host specificity, which may be important in the natural evolution of the H9 subtype, a plausible candidate for the agent likely to cause a future pandemic (27).
Several H9 escape mutants showed decreased virulence for mice. Generally, differences in virulence may result from mutations in genes other than HA. This is illustrated by the fact that the nonvirulent variant Sw/HK/9/98-MP has exactly the same HA amino acid sequence as the virulent escape mutants mG9-27 and m18G4 (Table 3). However, a single mutation in HA can affect virulence (10, 19). Among the H9 escape mutants characterized in the present paper, the greatest loss of virulence was associated with the substitution T188N (T198 in H3 numbering), resulting in the acquisition of a potential glycosylation site. The effect of the loss or acquisition of glycosylation sites on virulence has been described for HA of the H3 subtype (20) and H1 subtype (7), and the decrease in virulence for mice associated with the appearance of a new glycosylation site in escape mutants was described in our earlier studies of HA of H5 subtype (10). In addition, the acquisition of glycosylation sites in escape mutants of an H2 virus has been shown to be associated with a decrease in the cell fusion and receptor-binding activities of HA (26).
This abundance of data on the effect of glycosylation on virulence and related properties, as well as our current findings that two independently selected mutants lost virulence to the same extent, suggest that mutation T188N (T198N in H3 numbering), and not a mutation in another gene, is the cause of the loss of virulence. The situation is less clear for the double mutants exhibiting a moderate decrease in virulence (Table 5). One should keep in mind that a decrease in virulence in an antibody-selected mutant may result from random coselection of an attenuating mutation in a gene other than HA. However, our results show a connection between the decrease in virulence and the reduced affinity for sialic acid-containing substrates (Tables 5 and 6). We cannot claim that there is a strict quantitative correlation between virulence and the affinity for a definite sialyl substrate. However, mutants carrying the substitution T198N (H3 numbering) both had sharply decreased virulence and a lowered affinity for fetuin and the synthetic sialoglycopolymers, whereas three of the four mutants of intermediate virulence had a moderately decreased affinity either for both synthetic substrates or for fetuin and one of the synthetic sialyl substrates. Therefore, the decrease in virulence in most, if not in all, escape mutants is likely to be, at least in part, a result of the amino acid changes causing the decreased affinity of HA for cell receptors. Notably, however, the same amino acid changes, when present as single mutations, affect neither virulence nor the affinity for sialyl substrates. It seems that the combined amino acid substitutions in the double or triple mutants have a synergistic effect.
The differences in antigenic architecture between H9 HA and the other HA subtypes mapped so far suggest that the pathways of the antigenic drift of the H9 subtype, if it ever appears in the human population as a circulating agent, may differ from those of the known human influenza virus subtypes. One cannot predict whether the natural antigenic drift of the H9 subtype would involve amino acid changes in the same positions as those observed in the escape mutants. Interestingly, positions 133, 145, and 198 (H3 numbering) in H9 escape mutants (Table 3) coincide with the differences between A/Sw/HK/9/98 and a human H9 isolate (13). The significance of this coincidence, however, should not be overestimated, since these strains have differences at as many as 32 positions. The limitations imposed by the multiple effects of pleiomorphic mutations, such as loss of virulence or changes in the binding of cell receptors, should be as important in H9 as in other subtypes.
The present paper and, to a certain extent, our previous paper on HA of the H5 subtype (10) provide information that can be used to establish a correlation between intersubtype structural differences and variations in the location of antigenic areas among subtypes. This information could not have been obtained from earlier studies with the three-dimensional structure of H3 to obtain an antigenic map of any subtype.
At present, because only three subtypes (H3, H5, and H9) have been antigenically mapped on their own three-dimensional models, conclusions about a correlation between the structure of the HA molecule and its antigenicity are necessarily limited and await the availability of crystallographic data and antigenic maps of the HAs of other subtypes. Nevertheless, the present paper and, to a certain extent, our previous paper on H5 HA (10) provide new information that can be used to establish a correlation between intersubtype structural differences and variations in antigenic distribution.
Acknowledgments
These studies were supported by grant AI95357 from the National Institute of Allergy and Infectious Diseases, by Cancer Center Support (CORE) grant CA-21765 from the National Institutes of Health, by NATO Collaborative Linkage grant 979155, by grants 00-04-48017, 03-04-06212, and 03-04-48353 from the Russian Foundation for Basic Research (RFBR), and by the American-Lebanese-Syrian Associated Charities (ALSAC).
We thank Patrick Seiler for excellent technical assistance, Aleksandra S. Gambaryan for the gift of sialic polymer substrates and useful discussion, Richard J. Webby for critical comments, and Janet R. Davies for editorial assistance.
REFERENCES
- 1.Caton, A. J., G. G. Brownlee, J. M. Yewdell, and W. Gerhard. 1982. The antigenic structure of the influenza virus A/PR/8/34 hemagglutinin (H3 subtype). Cell 31:417-427. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 1998. Update: isolation of avian influenza viruses from humans—Hong Kong, 1997-1998. Morb. Mortal. Weekly Rep. 46:1245-1247. [PubMed] [Google Scholar]
- 3.Daniels, R. S., S. Jeffries, P. Yates, G. C. Schild, G. N. Rodgers, J. C. Paulson, S. A. Wharton, A. R. Douglas, J. J. Skehel, and D. C. Wiley. 1987. The receptor binding and membrane fusion properties of influenza virus variants selected with anti-haemagglutinin monoclonal antibodies. EMBO J. 6:1459-1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gambaryan, A. S., and M. N. Matrosovich. 1992. A solid-phase enzyme-linked assay for influenza virus receptor-binding activity. J. Virol. Methods 39:111-123. [DOI] [PubMed] [Google Scholar]
- 5.Gambaryan, A. S., J. S. Robertson, and M. N. Matrosovich. 1999. Effects of egg adaptation on the receptor-binding properties of human influenza A and B viruses. Virology 258:232-239. [DOI] [PubMed] [Google Scholar]
- 6.Gambaryan, A. S., A. B. Tuzikov, V. E. Piskarev, S. S. Yamnikova, D. K. Lvov, J. S. Robertson, N. V. Bovin, and M. N. Matrosovich. 1997. Specification of receptor-binding phenotypes of influenza virus isolates from different hosts with synthetic sialoglycopolymers: non egg-adapted human H1 and H3 influenza A and influenza B viruses share a common high binding affinity for 6′-sialyl(N-acetyllactosamine). Virology 232:345-350. [DOI] [PubMed] [Google Scholar]
- 7.Gitelman, A. K., N. V. Kaverin, I. G. Kharitonenkov, I. A. Rudneva, E. I. Sklyanskaya, V. M. Zhdanov. 1986. Dissociation of the haemagglutinin inhibition and the infectivity neutralization in the reactions of influenza A/USSR/90/97 virus variants with monoclonal antibodies. J. Gen. Virol. 67:2247-2251. [DOI] [PubMed] [Google Scholar]
- 8.Ha, Y., D. J. Stevens, J. J. Skehel, and D. C. Wiley. 2001. X-ray structures of H5 avian and H9 swine influenza virus hemagglutinins bound to avian and human receptor analogs. Proc. Natl. Acad. Sci. USA 98:11181-11186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ha, Y., D. J. Stevens, J. J. Skehel, and D. C. Wiley. 2002. H5 avian and H9 swine influenza virus hemagglutinin structures: possible origin of influenza subtypes. EMBO J. 21:865-875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaverin, N. V., I. A. Rudneva, N. A. Ilyushina, N. L. Varich, A. S. Lipatov, Y. A. Smirnov, E. A. Govorkova, A. S. Gitelman, D. K. Lvov, and R. G. Webster. 2002. Structure of antigenic sites on the haemagglutinin molecule of H5 influenza virus and phenotypic variation of escape mutants. J. Gen. Virol. 83:2497-2505. [DOI] [PubMed] [Google Scholar]
- 11.Kohler, G., and C. Milstein. 1976. Derivation of specific antibody-producing tissue culture and tumor lines by cell fusion. Eur. J. Immunol. 6:511-519. [DOI] [PubMed] [Google Scholar]
- 12.Li, K. S., K. M. Xu, J. S. M. Peiris, L. M. L. Poon, K. Z. Yu, K. Y. Yen, K. F. Shortridge, R. G. Webster, and Y. Guan. 2003. Characterization of H9 subtype influenza viruses from the ducks of southern China: a candidate for the next influenza pandemic in humans? J. Virol. 77:6988-6994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin, Y. P., M. Shaw, V. Gregory, K. Cameron, W. Lim, A. Klimov, K. Subarrao, Y. Guan, S. Krauss, K. Shortridge, R. Webster, N. Cox, and A. Hay. 2000. Avian-to-human transmission of H9N2 subtype influenza A viruses: relationship between H9N2 and H5N1 human isolates. Proc. Natl. Acad. Sci. USA 97:9654-9658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matrosovich, M. N., A. S. Gambaryan, A. B. Tuzikov, N. A. Byramova, L. V. Mochalova, A. A. Golbraikh, M. D. Shenderovich, J. Finne, and N. V. Bovin. 1993. Probing of the receptor-binding sites of the H1 and H3 influenza virus hemagglutinins by synthetic and natural sialosides. Virology 196:111-123. [DOI] [PubMed] [Google Scholar]
- 15.Matrosovich, M. N., S. Krauss, and R. G. Webster. 2001. H9N2 influenza A viruses from poultry in Asia have human virus-like receptor specificity. Virology 281:156-162. [DOI] [PubMed] [Google Scholar]
- 16.Palmer, D. F., W. R. Dowdle, M. T. Coleman, and G. C. Schild. 1975. Advanced laboratory techniques for influenza diagnosis. U.S. Department of Health, Education and Welfare Immunology Series, no. 6. Centers for Disease Control, Atlanta, Ga.
- 17.Peiris, M., K. Y. Yuen, C. W. Leung, K. H. Chan, P. L. Ip, R. W. Lai, W. K. Orr, and K. F. Shortridge. 1999. Human infection with influenza H9N2. Lancet 354:916-917. [DOI] [PubMed] [Google Scholar]
- 18.Peiris, J. S. M., Y. Guan, D. Markwell, P. Ghose, R. G. Webster, and K. F. Shortridge. 2001. Cocirculation of avian H9N2 influenza A viruses in pigs in southeastern China: potential for genetic reassortment? J. Virol. 75:9679-9686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Philpott, M., C. Hioe, M. Sheerar, and V. Hinshaw. 1990. Hemagglutinin mutations related to attenuation altered cell tropism of a virulent avian influenza A virus. J. Virol. 64:2941-2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reading, P. C., L. S. Morey, I. C. Crouch, and M. E. Anders. 1997. Collectin-mediated antiviral host defense of the lung: evidence from influenza virus infection of mice. J. Virol. 71:8204-8212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reed, L. J., and H. Muench. 1938. A simple method for estimating 50% endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 22.Schulze, I. T. 1997. Effect of glycosylation on the properties and functions of influenza virus hemagglutinin. J. Infect. Dis. 176:S24-S28. [DOI] [PubMed] [Google Scholar]
- 23.Skehel, J. J., and D. C. Wiley. 2001. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 69:531-569. [DOI] [PubMed] [Google Scholar]
- 24.Smirnov, Y. A., A. S. Lipatov, R. van Beek, A. K. Gitelman, A. D. M. E. Osterhaus, and E. C. J. Claas. 2000. Characterization of adaptation of an avian influenza A (H5N2) virus to a mammalian host. Acta Virol. 44:1-8. [PubMed] [Google Scholar]
- 25.Tsuchiya, E., K. Sugawara, S. Hongo, Y. Matsuzaki, Y. Muraki, Z.-N. Li, and K. Nakamura. 2001. Antigenic structure of the haemagglutinin of human influenza A/H2N2 virus. J. Gen. Virol. 82:2475-2484. [DOI] [PubMed] [Google Scholar]
- 26.Tsuchiya, E., K. Sugawara, S. Hongo, Y. Matsuzaki, Y. Muraki, Z.-N. Li, and K. Nakamura. 2002. Effect of addition of new oligosaccharide chains to the globular head of influenza A/H2N2 virus haemagglutinin on the intracellular transport and biological activities of the molecule. J. Gen. Virol. 83:1137-1146. [DOI] [PubMed] [Google Scholar]
- 27.Webby, R. G., and R. G. Webster. 2001. Emergence of influenza A viruses. Philos. Trans. R. Soc. London B 356:1818-1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Webster, R. G., W. J. Bean, O. T. Gorman, T. M. Chambers, and Y. Kawaoka. 1992. Evolution and ecology of influenza A viruses. Microbiol. Mol. Biol. Rev. 56:152-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wiley, D. C., I. A. Wilson, and J. J. Skehel. 1981. Structural identification of the antibody-binding sites of Hong Kong influenza hemagglutinin and their involvement in antigenic variation. Nature (London) 289:373-378. [DOI] [PubMed] [Google Scholar]