Abstract
Objective
We examined the frequency and significance of extracoronary findings in a sample of asymptomatic of Multiethnic Study of Atherosclerosis participants who had coronary magnetic resonance angiography (MRA).
Subjects and Methods
The Multiethnic Study of Atherosclerosis is a cohort study that, at baseline, included 6814 participants 45 to 84 years old, and free of clinical cardiovascular disease. A random subset of 254 participants underwent coronary MRA. Two experienced readers evaluated all images, and a consensus reading was performed. The findings were classified based on their clinical significance.
Results
Extracoronary findings were detected in 101 (39.8%) of the 254 participants. Additional imaging or clinical referral was need for 15 (5.9%) of the 254 participants. None of the participants required emergency referral. Signal loss in a pulmonary artery branch due to navigator beam saturation occurred in 59 (23%) of the 254 participants simulating a pulmonary embolus.
Conclusions
The prevalence of reportable extracoronary findings on coronary MRA is high. Familiarity with noncardiac magnetic resonance imaging interpretation may help in avoiding unnecessary testing resulting from inconclusive identification of extracoronary abnormalities detected incidentally on coronary MRA.
Keywords: coronary MRA, extracardiac findings, MR artifacts, MESA
The frequency and clinical significance of extracardiac abnormalities associated with coronary computed tomography (CT) angiography have been described,1 but extracardiac findings associated with coronary magnetic resonance angiography (MRA) have not been reported. Similar to cardiac multidetector CT, magnetic resonance imaging (MRI) examinations of the chest also include portions of the lung parenchyma, spine, and upper abdominal organs. Portions of the field of view beyond the myocardium may reveal important pathologic findings. Correct identification of these incidentally discovered abnormalities may help in detecting clinically silent or early disease. Improper diagnosis, however, may result in increased health care costs due to unnecessary workup of insignificant findings.
The purpose of this study was to describe the frequency and significance of extracardiac findings in subjects undergoing coronary MRA in the Multiethnic Study of Atherosclerosis (MESA), a multicenter cohort study of cardiovascular disease.
MATERIAL AND METHODS
The MESA study included at baseline 6814 subjects without prevalent clinical cardiovascular disease at the time of entry into the study in 2000 to 2002. This study is based on the data from 2 of the 6 communities (Baltimore and Chicago) where MRA was being performed. Magnetic resonance angiography results were available for 254 participants randomly selected from the study samples in these 2 centers.
The first 11 subjects were evaluated using a 1.5 T whole-body MRI system (Signa CVi, General Electric Medical Systems, Waukesha, WI). Subsequently, 243 subjects were imaged on a 1.5 T whole-body clinical scanner (Avanto, Siemens Medical Solutions, Erlangen, Germany). Three plane scout images/ localizing images and steady state free precession coronary MRA images were acquired using either breath-hold technique (n = 23) or 3-dimensional steady-state free precession (SSFP) navigator assisted free breathing whole heart technique (n = 231).2 Imaging parameters for the SSFP whole heart technique were TR 200 ms/TE1.5 ms, field of view 34 × 24 cm, 420 × 420 mm matrix, slice thickness 0.8 mm.
MR Image Analysis
Two experienced board certified dedicated MR radiologists (D.A.B. and J.V.C.) evaluated all images (including scout images), and a consensus reading was performed when differences occurred. The findings were classified based on their clinical significance: (1) no participant follow up or referral, but reportable to the referring physician in an imaging interpretation report, (2) follow-up MRI examination to ensure stability of finding (6–12 months), (3) additional nonemergent imaging test and/or clinical referral needed to evaluate the abnormality (<6 months), (4) immediate emergency clinical referral or emergent additional imaging test recommended. Imaging features that potentially mimicked pathologic findings were also recorded at the time of interpretation.
RESULTS
Mean age was 60.5 years (±9.1 SD; age range, 45–89 years). Participants’ ethnic background, age, and gender distributions are shown in Table 1. The sample had a predominance of caucacian (63%) and relatively few participants in the age group 75 to 84 years. Men and women were almost equally distributed.
Table 1.
Study Population
| N (254) | % | ||
|---|---|---|---|
| Race | Caucacian | 161 | 63.4 |
| African American | 93 | 36.6 | |
| Age | 45–54 | 82 | 32.3 |
| 55–64 | 77 | 30.3 | |
| 65–74 | 81 | 31.9 | |
| 75–84 | 14 | 5.5 | |
| Mean ± SD | 60.5 ± 9.1 | ||
| Range | 45–84 | ||
| Gender | Female | 130 | 51.2 |
| Male | 124 | 48.8 |
Number and percent distributions of the MESA subset undergoing coronary MRA, according to ethnic background, age, and gender.
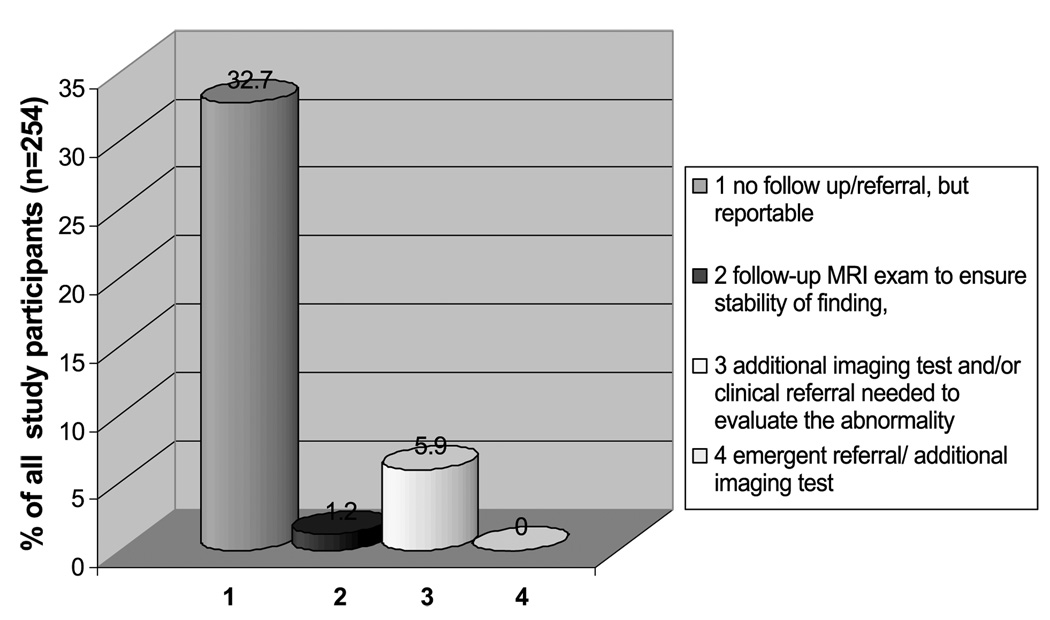
A total of 60.2% (153/254) of MRI examinations had no reportable extracoronary findings. Extracoronary findings were detected in 101 (about 39.8%) of the 254 participants (Figs. 1 and 2). Sixteen participants had 2, 3 subjects had 3, and 1 participant had 4 extracoronary findings.
Figure 1.
Frequency of noncoronary findings on coronary MRA in a sample of participants of the MESA.
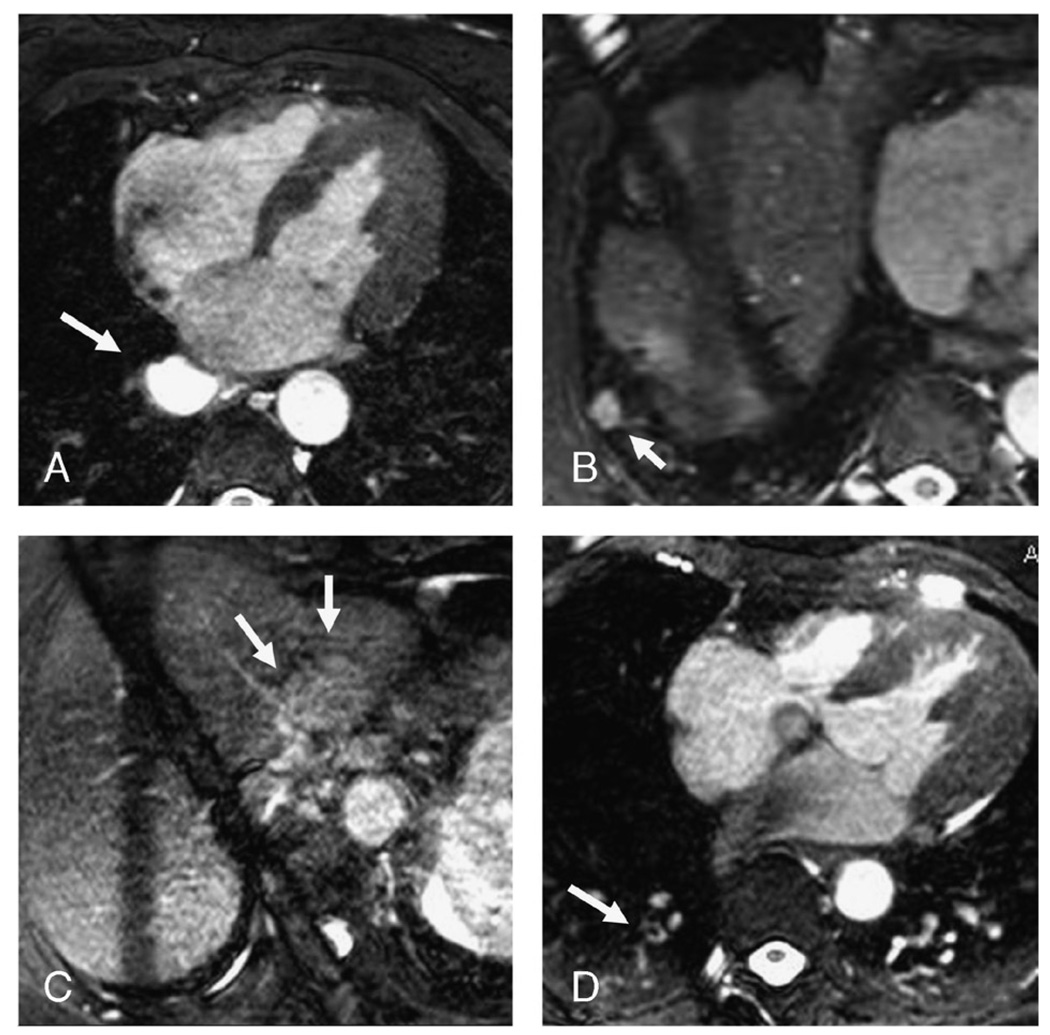
Figure 2.
Examples of noncoronary findings (A and B) and MR image artifacts (C and D) mimicking pathology on SSFP coronary MRA exams in the MESA cohort. A, Esophageal duplication cyst (1, no follow up/referral, but reportable). B, 2 cm lung mass right lower lobe (3, additional imaging test and/or clinical referral needed to evaluate the abnormality). C, Pseudomass in liver due to z-axis rap-around artifact from ascending aorta (0, no extracardiac findings). D, Pseudo-pulmonary embolus right lower lobe due to saturation artifact from diaphragmatic navigator (0, no extra cardiac findings).
None of the participants required emergency (grade 4) referral/additional imaging test. Fifteen of 254 (5.9%) had grade 3 findings with additional imaging test suggested for follow-up. Examples of grade 3 findings included enlargement of main pulmonary artery, lung nodule, renal hydronephrosis (Table 2). Grade 2 findings were present in 3 (1.2%) of the 254 participants and required follow-up MRA examination in 12 months to ensure stability of a finding (eg, ascending aortic dilatation >4 cm).
Table 2.
Extracoronary MRI Findings
| Grade 1 (reportable finding, no follow-up required) | Liver cyst(s)/hemangioma | 30 |
| Small pleural effusion | 11 | |
| Lung atelectasis | 9 | |
| Small hiatal hernia | 7 | |
| Kidney cyst | 7 | |
| Vertebral body hemangioma | 5 | |
| Breast cyst(s) | 5 | |
| Gallstones | 5 | |
| Lung scarring | 4 | |
| Moderate hiatal hernia | 3 | |
| Duplication cyst | 3 | |
| Sternal wires | 3 | |
| Colonic diverticula | 2 | |
| Vertebral body compression fracture | 2 | |
| Small pericardial effusion | 2 | |
| Moderate elevation right hemidiaphragm | 2 | |
| Bulla lung | 1 | |
| Central venous catheter | 1 | |
| Interstitial thickening/fibrosis | 1 | |
| Moderate degenerative disc disease | 1 | |
| Esophageal achalasia | 1 | |
| Moderate thoracic spine kyphosis | 1 | |
| Splenic cyst | 1 | |
| Subcutaneous sebaceous cyst | 1 | |
| Grade 2 (follow-up MRI examination to ensure stability of finding) | Ascending aortic dilatation >4 cm | 3 |
| Grade 3 (additional imaging test and/or clinical referral needed) | Lung consolidation | 3 |
| Aortic regurgitation | 3 | |
| Aortic stenosis | 2 | |
| Lung mass/nodule | 2 | |
| Hydronephrosis | 1 | |
| Moderately enlarged main pulmonary artery/suspected pulmonary hypertension | 1 | |
| Hypertrophic cardiomyopathy | 1 | |
| Indeterminate liver lesion | 1 | |
| Moderate pericardial effusion | 1 |
Extracoronary MRI findings in a subset of the MESA participants. The total number of findings listed above was 126 in the 101 participants, because some MESA participants had more than 1 finding. Sixteen participants had 2, 3 subjects had 3 and 1 participant had 4 extracoronary findings.
Of all participants and of participants with extracoronary findings, 83/254 (37.7%) and 83/101 (82.2%), respectively, had grade 1 findings, which did not require follow up imaging or clinical referral (eg, gallstones in normal gallbladder, liver cysts, kidney cysts, pericardial cyst, small pleural/pericardial effusion, moderately elevated hemi-diaphragm, breast cysts, hiatal hernia).
Every MRI study was noted by reviewers to have some type of image artifact, such as wrap around and pulsation artifacts (Fig. 2C). Signal loss in a pulmonary artery branch due to navigator beam saturation occurred in 59 (23%) of the 254 participants; 5 participants had 2 of these defects (Fig. 2D). This artifact simulated a pulmonary embolus (PE) and predominantly occurred in the right lower lobe pulmonary artery branches, although 4 participants had this artifact in the right upper lobe and 1 in the right middle lobe pulmonary artery. Features which distinguished this from PE included (a) appearance only in the right lung (corresponding to the side of the navigator beam), (b) central location within the vessel, (c) similar in-plane position to the navigator echo on more inferior imaging slices.
Reader consensus for noncoronary findings was very good. Four findings merited additional discussion by readers for a final consensus read: (1 “pseudo” PE due to the navigator beam, 1 pericardial cyst, and 2 liver lesions classified as liver cysts/hemangiomas).
DISCUSSION
In our study, noncoronary abnormalities were identified by coronary MRA in about 40% of participants. Correct interpretation of benign, clinically insignificant findings, or MRI artifacts is crucial to avoid unnecessary referrals or additional imaging tests that otherwise would increase health care cost without benefit for an individual. Incorrect interpretation of the significance or type of extracoronary finding(s) may also cause unnecessary participant anxiety and/or unnecessary and often expensive additional testing.
Extracardiac findings have previously been shown to be very common with cardiac CT, and their prevalence has ranged from 25% to 61%; of these incidental CT findings, 5% to 10% have been considered as major.1,3–5 Notwithstanding the fact that ours was an asymptomatic study population undergoing MRA, it is interesting that our results are within the range of these previous CT studies, as 40% of our participants had extracoronary abnormalities.
Only 5.9% of the participants in this study needed routine referral/additional imaging tests, which is similar to the rate of major findings in multi-detector computed tomography (MDCT) studies. In a MDCT study by Haller et al,4 abnormalities with immediate impact on patient management, treatment, or both, such as pulmonary embolism, pneumonia, or bronchial carcinoma, were identified in 4.8% of the participants. Probably because our sample did not include individuals with prevalent cardiovascular disease, we did not observe serious abnormalities requiring emergency care, such as a PE. Haller reported a 0.6% incidence of pulmonary embolism (1/166 patients) in individuals undergoing angiography, who had been referred because of chest pain.
In a prior study by Waltering et al6 that used cardiac MRI (but not MR coronary angiography) for detection of myocardial ischemia, cardiac masses or thrombi and assessment of myocarditis or cardiomyopathies, clinically relevant findings were detected in 8.7% of patients compared with 7.1% of participants in categories 2 and 3 in the present study (Fig. 1). In that study, 5.7% (vs 5.9% in category 3 in the present study [Fig. 1]) of the patients were referred for additional diagnostic procedures. Although those authors included vascular variants and benign findings, their data are otherwise quite similar to those of the present study.
Magnetic resonance imaging artifacts were common but were distinguished from pathologic findings by trained cardiovascular MRI observers. One unique artifact on coronary MRA, not previously described, was due to blood saturation from the navigator beam used for coronary MRA. This artifact was common in the right lower lobe and could mimic a PE. The artifact is on the side of the navigator beam and produces an apparent central filling defect in the pulmonary artery.
In summary, the prevalence of clinically relevant extracoronary findings observed by cardiac MRI is similar to that of previous reports using coronary MDCT. Familiarity with noncardiac MRI interpretation may help in avoiding unnecessary testing resulting from inconclusive identification of extracoronary abnormalities detected incidentally on coronary MRA.
ACKNOWLEDGMENTS
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org. J.V.C. was supported by the Radiological Society of North America Research and Education Foundation.
REFERENCES
- 1.Sosnouski D, Bonsall RP, Mayer FB, et al. Extracardiac findings at cardiac CT: a practical approach. J Thorac Imaging. 2007;22:77–85. doi: 10.1097/RTI.0b013e3180317a5b. [DOI] [PubMed] [Google Scholar]
- 2.Weber OM, Martin AJ, Higgins CB. Whole-heart steady-state free precession coronary artery magnetic resonance angiography. Magn Reson Med. 2003;50:1223–1228. doi: 10.1002/mrm.10653. [DOI] [PubMed] [Google Scholar]
- 3.Kirsch J, Araoz PA, Steinberg FB, et al. Prevalence and significance of incidental extracardiac findings at 64-multidetector coronary CTA. J Thorac Imaging. 2007;22:330–334. doi: 10.1097/RTI.0b013e31813434a9. [DOI] [PubMed] [Google Scholar]
- 4.Haller S, Kaiser C, Buser P, et al. Coronary artery imaging with contrast-enhanced MDCT: extracardiac findings. Am J Roentgenol. 2006;187:105–110. doi: 10.2214/AJR.04.1988. [DOI] [PubMed] [Google Scholar]
- 5.Horton KM, Post WS, Blumenthal RS, et al. Prevalence of significant noncardiac findings on electron-beam computed tomography coronary artery calcium screening examinations. Circulation. 2002;106:532–534. doi: 10.1161/01.cir.0000027136.56615.de. [DOI] [PubMed] [Google Scholar]
- 6.Waltering K, Schlosser T, Bruder O, et al. RSNA meeting. Chicago, IL, USA: 2005. Prevalence of Accidental Non-Cardiac Findings in Cardiac MRI. abstract. [Google Scholar]