Abstract
Objective
To investigate the association between indicators of quality of diabetic management in English family practices and emergency hospital admissions for short-term complications of diabetes.
Study Setting
A total of 8,223 English family practices from 2001/2002 to 2006/2007.
Study Design
Multiple regression analyses of associations between admissions and proportions of practice diabetic patients with good (glycated hemoglobin [HbA1c] ≤7.4 percent) and moderate (7.4 percent <HbA1c ≤10 percent) glycemic control. Covariates included diabetes prevalence, baseline admission rates, socioeconomic, demographic, and geographic characteristics.
Data
Practice quality measures extracted from practice records linked with practice-level hospital admissions data and practice-level covariates data.
Principal Findings
Practices with 1 percent more patients with moderate rather than poor glycemic control on average had 1.9 percent (95 percent CI: 1.1–2.6 percent) lower rates of emergency admissions for acute hyperglycemic complications. Having more patients with good rather than moderate control was not associated with lower admissions. There was no association of moderate or good control with hypoglycemic admissions.
Conclusion
Cross-sectionally, family practices with better quality of diabetes care had fewer emergency admissions for short-term complications of diabetes. Over time, after controlling for national trends in admissions, improvements in quality in a family practice were associated with a reduction in its admissions.
Keywords: Ambulatory care sensitive conditions, primary care, diabetes, quality indicators, hospital admissions
Diabetes is considered to be an ambulatory care sensitive condition where timely and effective management in primary care should reduce emergency hospitalizations (Weissman, Gatsonis, and Epstein 1992; Billings et al. 1993; Bindman et al. 1995; Department of Health [DOH] 2001; Agency for Healthcare Quality and Research [AHQR] 2004; National Institute for Health and Clinical Excellence 2008; Purdy et al. 2009;). Poor diabetic control can result in life-threatening hyperglycemic or hypoglycemic states in the short term, and in vascular complications which are major causes of mortality and morbidity in the long term. Better quality of primary care diabetes management should therefore result in fewer hospitalizations for diabetic complications.
There is, however, little evidence about the relationship between higher quality diabetes management in primary care and emergency hospital admissions for diabetes. In this paper we examine the association, both cross-sectional across practices and over time within practices, between the quality of glycemic control in family practices and their hospital admission rates for emergencies (unplanned admissions) due to short-term diabetic complications.
We use information on the quality of care for all family practices in England extracted automatically from practice electronic records as part of the Quality and Outcomes Framework (QOF) pay-for-performance scheme (Roland 2004). Quality is measured at practice level by a set of clinical indicators with practices awarded points according to the proportion of eligible patients for whom they achieve each indicator. The scheme includes 18 diabetes-related indicators, covering both process measures for secondary prevention (e.g., screening for retinopathy) and intermediate outcome measures, including control of glycated hemoglobin (HbA1c) levels (NHS Employers 2008). We do not attempt to assess the impact of the QOF on admissions because we do not have data on quality before the QOF was introduced. Rather, we use the detailed information produced by the QOF to examine whether higher practice quality is associated with fewer emergency admissions.
Few studies have examined the association between practice diabetes care quality and hospital admissions. Bruni, Nobilio, and Ugolini (2009) found that in the Emilia Romagna region of Italy in 2003 patients registered with family practitioners who received more income from participation in a pay-for-performance program had a significantly lower probability of hyperglycemic emergencies. Saxena et al. (2006) used data from 31 Primary Care Trusts (PCTs—statutory bodies responsible for commissioning care for geographically defined populations) in London for 2000/2001. They found that PCTs with a higher proportion of family practitioners who were offering health promotion clinics for diabetes had lower emergency and elective admission rates for diabetes. This study was based on 1 year's data and relatively few observations and could not allow for potential confounding by socioeconomic factors.
Other studies have used detailed performance indicators available in the QOF incentive scheme. Downing et al. (2007) examined the relationship between the risk of emergency admission for diabetic complications for patients and the QOF points scored by 94 family practices in two PCTs, controlling for socioeconomic and demographic characteristics. Patients in practices with higher scores across all disease areas had lower risks of emergency diabetic admission, but the association was not significant. Bottle et al. (2008) examined all 303 PCTs in England and found that, after allowing for area deprivation and diabetes prevalence, PCTs with higher average QOF scores for diabetes management had significantly lower emergency admission rates for patients aged 60 and older.
We have also used data from the QOF, but we have addressed key limitations of the existing literature based on the QOF. First, the scheme has upper payment thresholds of between 50 percent and 90 percent for quality indicators, so that practices can earn the maximum points on an indicator without necessarily achieving the target for all relevant patients. Practices are also permitted to exclude (“exception report”) patients from specific indicators, for reasons including extreme frailty, intolerance of a particular medication, and patients refusing treatment (DOH 2004). For these reasons, quality is better measured by the proportion of patients for whom a practice achieved a quality indicator, rather than the number of points scored.
Second, the relationships between practices' achievement on diabetes quality indicators and patient outcomes are likely to be complex. Dietary advice, exercise, and appropriate prescribing can reduce HbA1c levels and hence lead to fewer emergency admissions for hyperglycemia. But exercise and insulin can increase the risk of emergency admissions for hypoglycemia (Briscoe and Davis 2006). Improved monitoring of peripheral pulses and neuropathy could lead to increased elective admissions over the short to medium term, as more complications are detected and referred for treatment. In the longer term, they could lead to fewer admissions for retinopathy, neuropathy, cardiovascular disease, and kidney disease. It is, therefore, necessary to relate different types of diabetic admission to the relevant quality indicator.
Third, previous studies used a single year of data and were vulnerable to confounding by unobserved factors that affect both practice admission rates and quality as measured by the QOF. We included relevant covariates in our cross-sectional analysis and also examined the longitudinal relationship between practice emergency admissions and quality over 3 years, thereby removing the risk of confounding by unobserved factors which differ across practices but which are constant over time.
METHODS
Our research question was whether better quality of family practice diabetes management was associated with lower practice admission rates for glycemic complications. Although we use data from the QOF incentive scheme for three financial years 2004/2005 to 2006/2007 to measure quality, we do not investigate whether the incentive scheme affected quality.
The quality measures are the proportions of practice-recorded diabetic patients for whom the relevant QOF quality indicators for monitoring and control of HbA1c levels were met. We investigated the association of these indicators with four groups of emergency admissions relating to short-term diabetic complications: (i) all complications due to poor short-term glycemic control, (ii) acute hyperglycemia (ketoacidosis and coma), (iii) nonspecific hyperglycemia, and (iv) hypoglycemia. The all complications group (i) was the sum of groups (ii)–(iv). The unit of analysis was the family practice (groups of family physicians with a mean of four full-time equivalent physicians and a mean registered population of 6,412 patients in 2006/2007).
Outcome Variables
Hospital admissions data were taken from Hospital Episode Statistics for England (Information Centre for Health and Social Care 2009a). For the financial years 2001/2002 to 2006/2007, we extracted all emergency spells for individuals with a primary diagnosis of diabetes. Transfers from one hospital to another were excluded to prevent double counting.
Diagnoses were classified using the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) (World Health Organization 2007). Healthcare Resource Groups (HRG) v3.5 codes (Information Centre for Health and Social Care 2007a, b) were used to assist with classification into acute or nonspecific hyperglycemic and hypoglycemic categories. Our classification was based on preventive quality indicators guidelines published by the U.S. AHQR (see AHQR 2004). The full set of codes is given in Appendix Table SA1. Admissions were aggregated to family practice level for each year to provide a count of the total number of admissions for each family practice.
Diabetes Care Quality Measures
We measured the proportion of recorded diabetic patients in each practice for whom three indicators of diabetic control were met (see the Appendix for further details). We used information on the three quality indicators of glycemic control: whether HbA1c was measured (indicator DM5); whether measured HbA1c was ≤7.4 percent (7.5 percent for 2006/2007) (indicator DM6); and whether measured HbA1c was ≤10 percent (indicator DM7). The categorization of glycemic control is given in Figure 1. For each practice, we constructed three measures of glycemic control—the proportions of all registered diabetic patients for whom:
Figure 1.
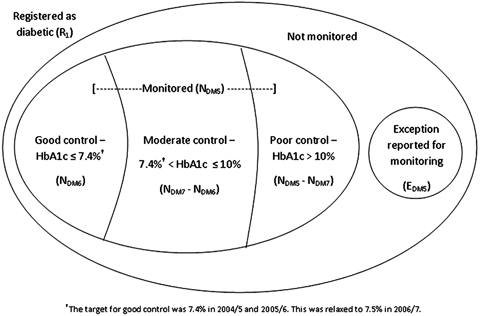
Categorization of Glycemic Control for Patients Registered as Diabetic under the U.K. Quality and Outcomes Framework
HbA1c levels were measured.
HbA1c was measured and was well controlled (HbA1c ≤7.4 percent in 2004/2005 and 2005/2006, and ≤7.5 percent in 2006/2007).
HbA1c was measured and was moderately well controlled (7.4 percent <HbA1c ≤10 percent in 2004/2005 and 2005/2006, 7.5 percent <HbA1c ≤10 percent in 2006/2007).
This method of measuring diabetes quality differs from that used in previous papers based on QOF data in three respects. First, it uses information on specific glycemic control indicators rather than aggregations over all clinical indicators. Second, we measure quality as the proportions of registered diabetic patients for whom good or moderate control has been achieved, rather than as the number of points earned by the practice under the pay-for-performance scheme. As previously noted, a points-based measure will understate the variation in quality in practices because improvements in quality above an upper threshold are not reflected in points earned and because points scores are affected by exception reporting (DOH 2004; Doran et al. 2008a, b; bGravelle, Sutton, and Ma 2010).
Covariates
Practice and patient characteristics were obtained from the DOH's General Medical Services dataset and the Prescription Pricing Division of the Business Services Authority for each year from 2004/2005 to 2006/2007. The variables included the Low Income Scheme Index (Lloyd, Harris, and Clucas 1995), which is the proportion of prescriptions in a practice which are dispensed without charge because the patient has a low income. Measures of access to primary and secondary care, and rurality indicators were obtained from Office of National Statistics and the DOH (DOH 2008). Local population characteristics such as income, education, housing, morbidity, and mortality were derived from the Office of National Statistics Neighbourhood Statistics archive (Office for National Statistics 2008). These data were available for 34,378 Lower Super Output Areas with average populations of 1,500. It was attributed to practices using the Attribution Data Set (Information Centre for Health and Social Care 2009b), which contains information on the number of patients in each family practice resident in each Lower Super Output Area.
To allow for differences in hospital admission policies and treatment quality in secondary care, we included the proportions of a practice's emergency diabetic admissions at each of 298 hospitals in each year. Every family practice is supervised by one of the 303 PCTs in England, which have an average population of 170,000. To allow for unobserved variations in PCT policy, community care, and other geographic characteristics, we included a dummy variable for the practice's supervising PCT. Further details of variable construction are in the Appendix.
Exclusions
A total of 8,606 practices had complete diabetes registers for at least 1 year between 2004/2005 and 2006/2007. Practices were excluded from the study if they had fewer than 1,000 registered patients in a year; missing baseline admission rates; incomplete socioeconomic or practice data; or no recorded prevalence. Our main results are based on data from 8,158 practices in 2004/2005, 7,921 in 2005/2006, and 7,956 in 2006/2007.
Estimation
For each of the four categories of emergency admissions, we tested for an association between practice diabetes management quality and emergency admission rates in two ways. First, we examined the cross-sectional association across practices between quality and admissions to see whether practices with better quality in a year had lower admission rates in that year. We estimated random effects multiple regression count data models with a large set of socioeconomic and practice covariates to reduce the risk of confounding. The covariates included the average admissions for a practice over the 3-year period 2001/2002 to 2003/2004. This presample admission rate will pick up unobserved practice confounding characteristics that do not vary over time (Blundell, Griffith, and Windmeijer 2002) (see the Appendix for full details). We also included year dummy variables in the regressions to allow for national time trends in admissions affecting all practices. Thus, the estimated coefficients on the quality variables in the cross-sectional regressions show the association between quality and admissions across practices in any given year.
Second, we examined the longitudinal association at practice level between quality and admissions to see whether practices that improved their quality over time experienced a reduction in admissions. We used fixed-effects count data multiple regressions and included year dummies so that the coefficients on the quality variables estimate the association between changes in practice quality and changes in admission rates after allowing for national trends and for potentially confounding covariates that changed over time. By looking at the association of the changes over time in admissions within practices and changes over time in quality within practices, we removed the effects of unobserved practice characteristics that did not change over time and that might affect admissions and be correlated with quality.
Effect on Costs of Diabetes-Related Admissions
We used the estimated coefficient on the moderate control variable to calculate the reduction in hospital costs per practice from having 5 percent more patients with moderate rather than poor glycemic control in an average practice.
RESULTS
National Trends in Emergency Admissions
The overall rate of short-term diabetic emergency admissions in England increased from 6.35 per 10,000 person years in 2004/2005 to 6.79 per 10,000 person years in 2006/2007 (Table 1). Hyperglycemic admissions were on average 3.5 times more frequent than hypoglycemic admissions, and 25 percent of practices had no hypoglycemic admissions during the first 3 years of the pay-for-performance scheme.
Table 1.
Descriptive Statistics for Emergency Admissions for Short-Term Complications and for Glycemic Control Indicators for English General Practices, 2004/2005 to 2006/2007
| Variable | Mean | Standard Deviation | Minimum | Maximum | Variable | Mean | Standard Deviation | Minimum | Maximum |
|---|---|---|---|---|---|---|---|---|---|
| 2004/2005 (n=8,158) | |||||||||
| All short-term admissions* | 6.35 | 5.38 | 0.00 | 96.69 | Diabetes prevalence | 3.48 | 1.01 | 0.21 | 16.56 |
| Acute hyperglycemic | 2.78 | 3.66 | 0.00 | 60.78 | Glycated hemoglobin (HbA1c) measured | 91.17 | 7.69 | 0.26 | 100.00 |
| Nonspecific hyperglycemic | 2.71 | 3.00 | 0.00 | 35.91 | HbA1c ≤7.4† | 51.39 | 10.78 | 0.00 | 97.78 |
| Hypoglycemic | 0.86 | 1.41 | 0.00 | 14.79 | 7.4<HbA1c ≤10† | 31.92 | 7.21 | 0.00 | 66.67 |
| Excepted for HbA1c measurement | 3.01 | 3.05 | 0.00 | 76.30 | |||||
| 2005/2006 (n=7,921) | |||||||||
| All short-term admissions | 6.75 | 5.71 | 0.00 | 61.92 | Diabetes prevalence | 3.68 | 1.03 | 0.20 | 14.51 |
| Acute hyperglycemic | 3.07 | 3.96 | 0.00 | 45.84 | HbA1c measured | 93.15 | 5.35 | 20.53 | 100.00 |
| Nonspecific hyperglycemic | 2.77 | 3.05 | 0.00 | 51.60 | HbA1c ≤7.4† | 53.97 | 9.70 | 8.59 | 99.03 |
| Hypoglycemic | 0.91 | 1.47 | 0.00 | 18.44 | 7.4<HbA1c ≤10† | 31.47 | 6.72 | 0.00 | 55.32 |
| Excepted for HbA1c measurement | 3.29 | 2.72 | 0.00 | 42.86 | |||||
| 2006/2007 (n=7,956) | |||||||||
| All short-term admissions | 6.79 | 5.64 | 0.00 | 91.07 | Diabetes prevalence | 3.77 | 1.07 | 0.13 | 10.64 |
| Acute hyperglycemic | 3.29 | 4.13 | 0.00 | 86.01 | HbA1c measured | 93.92 | 4.44 | 12.20 | 100.00 |
| Nonspecific hyperglycemic | 2.60 | 2.85 | 0.00 | 31.50 | HbA1c ≤7.5† | 59.26 | 9.45 | 0.00 | 94.41 |
| Hypoglycemic | 0.90 | 1.44 | 0.00 | 14.22 | 7.5<HbA1c ≤10† | 27.43 | 6.47 | 0.00 | 66.67 |
| Excepted for HbA1c measurement | 3.06 | 2.54 | 0.00 | 24.58 | |||||
Per 10,000 patients on practice list.
Percentage of registered diabetic patients whose most recent HbA1c level was in the stated range.
Quality of Care
Prevalence of diabetes, as recorded by the practices, increased from 3.5 percent in 2004/2005 to 3.8 percent in 2006/2007. As Table 1 shows, practice scores on the quality indicators have generally been high. On average, in 2004/2005 practices measured the HbA1c levels of 91.2 percent of diabetic patients, increasing to 94.0 percent by 2006/2007. Over this period, the percentage of registered diabetics achieving good glycemic control increased from 51.4 percent to 59.3 percent—although the target was relaxed slightly in 2006/2007—and the percentage with poor control fell from 16.7 percent to 13.3 percent.
Cross-Sectional Association of Quality of Care and Emergency Admissions across Practices
Table 2 has estimates of the cross-sectional association of quality of care and admissions. The reported coefficients δ are incident rate ratios, so that a unit increase in an explanatory variable is associated with 100(δ–1) percent higher admission rates. Thus, higher proportions of diabetic patients with good or moderate measured glycemic control were significantly associated with lower admission rates for all emergency admissions, and for acute and nonspecific hyperglycemic emergency admissions. There was no significant association with hypoglycemic admissions.
Table 2.
Multiple Regression Models of Cross-Sectional Associations between Practice Quality and Practice Emergency Admission Rates for All Short-Term, Hyperglycemic, and Hypoglycemic Emergency Admissions
| All Short Term | Acute Hyperglycemic | Nonspecific Hyperglycemic | Hypoglycemic | |||||
|---|---|---|---|---|---|---|---|---|
| Coefficient† | Z-Statistic | Coefficient | Z-Statistic | Coefficient | Z-Statistic | Coefficient | Z-Statistic | |
| Cross-sectional model† | ||||||||
| Glycated hemoglobin (HbA1c) ≤7.4/7.5 | 0.985 | −8.33** | 0.981 | −6.92** | 0.986 | −6.21** | 0.996 | −1.40 |
| 7.4/7.5<HbA1c ≤10 | 0.987 | −6.32** | 0.981 | −5.64** | 0.988 | −4.35** | 0.997 | −0.67 |
| HbA1c monitored | 1.011 | 5.10** | 1.015 | 4.20** | 1.010 | 3.64** | 1.005 | 1.33 |
| Excluded from HbA1c monitoring | 1.000 | 0.15 | 1.001 | 0.29 | 1.000 | 0.04 | 0.997 | −0.69 |
| Year: 2005/2006‡ | 1.057 | 5.67** | 1.097 | 5.77** | 1.018 | 1.32 | 1.050 | 2.30* |
| Year: 2006/2007‡ | 1.074 | 5.80** | 1.182 | 8.46** | 0.975 | −1.53 | 1.048 | 1.94 |
| Diabetes prevalence | 1.073 | 7.83** | 1.089 | 5.98** | 1.067 | 5.44** | 1.062 | 3.93** |
| Baseline admission rate§ | 1.163 | 23.12** | 1.202 | 20.55** | 1.112 | 13.68** | 1.054 | 5.48** |
| Efron's R2¶ | 0.206 | 0.147 | 0.124 | 0.083 | ||||
Statistically significant at 5% level.
Statistically significant at 1% level.
Coefficients reported as incident rate ratios. Quality indicators measured as percentages. Prevalence and baseline admission rate measured in standard deviation units. The percentage change in the admission rate associated with a 1 unit change in a continuous explanatory variable, holding all other variables constant, can be calculated as (coefficient—1)100%. The coefficients on the year dummy variables show the difference in admissions in the year compared with 2004/2005, holding all other factors constant.
Compared with baseline year (2004/2005).
Baseline admission rate for short-term diabetic complications of same type as dependent variable, averaged over to 2001/2002 to 2003/2004.
Obtained from the R2 from a regression of actual admission rates on predicted admission rates.
+ All models also include a full set of covariates, including Primary Care Trust dummies and the proportions of the practice admissions at each hospital trust. Full results in Appendix Table SA3. The number of observations in each model is 24,035.
The coefficients in Table 2 on the good control quality variable (HbA1c ≤7.4 percent or 7.5 percent) are estimates of partial associations, holding constant the proportions of diabetic patients with measured HbA1c levels and with measured HbA1c with moderate control. They show that practices with a higher proportion of patients with good measured control (and hence a smaller proportion with poor measured control) have lower rates of admission. Similarly, the coefficient on the moderate control measure shows that practices with a higher proportion of patients with measured moderate control (and a lower proportion with poor measured control) also have lower rates of admission.
The quality measures are measured as percentages so that a 1 percent higher proportion of recorded diabetic patients with moderate glycemic control rather than poor control was associated with a 1.3 percent (95 percent CI: 0.92–1.73 percent) lower rate of all emergency admissions for all short-term complications. This equates to 0.058 (95 percent CI: 0.040–0.076) fewer admissions per year for an average practice. A 1 percent higher proportion of patients with moderate rather than poor control was associated with 1.9 percent (95 percent CI: 1.2–2.6 percent) fewer admissions for acute hyperglycemic complications.
The difference between the coefficients on good and moderate control was not significant for any of the admission types. Thus, practices with similar proportions of patients with good or moderate control had similar admission rates, irrespective of the relative size of the proportions with good and moderate control.
There was a significant positive association of monitoring with admission rates in the combined and hyperglycemic models. Because the proportions of monitored patients with good and moderate control and the proportion of diabetic patients exception reported are held constant, a higher rate of monitoring implies that a higher proportion of monitored patients have poor control and that there is a lower proportion of unmonitored, but not exception reported patients (see Figure 1). This suggests that unmonitored patients were at less risk of admission than monitored patients in poor control and were probably a mix of patients with good, moderate, and poor control.
The baseline admission rate was highly significant in predicting subsequent admissions in all models, indicating the importance of controlling for persistent unobservable practice and patient characteristics that affect admissions. The coefficients on the year dummies show that after allowing for changes in quality of diabetes care, in diabetes and other disease prevalence, in demographic characteristics of the patient populations and changes in practice size and composition over time, admission rates increased significantly year on year by 6 percent (95 percent CI: 3–8 percent) in 2005/2006 and by 7 percent (95 percent CI: 3–11 percent) in 2006/2007 relative to 2004/2005.
Holding diabetes care quality constant, other characteristics of the practice and its population had statistically significant associations with emergency hospital admission (see Appendix Table SA3). Lower admission rates were associated with higher proportions of patients resident in community care establishments and education-deprived areas (for nonspecific hyperglycemic admissions).
Higher admission rates were associated with the following: higher recorded levels of other morbidities (including mental health problems and chronic obstructive pulmonary disease [COPD]); higher mortality rates; higher prevalence of risk factors such as smoking and obesity; and demographic characteristics including the proportion of female patients aged 15–44 and over 75, and the proportion of the population that was nonwhite.
Longitudinal Association of Diabetes Care Quality and Admissions within Practices
Table 3 reports results from multiple regression models of the association of changes in practice quality and practice admission rates (full results are available from the authors). In all cases, an increase in the proportions of diabetic patients in good and moderate glycemic control was significantly associated with lower admissions, with larger reductions for acute than for nonspecific hyperglycemic admissions. The differences in the coefficients on the good and moderate control indicators were again not significant. Results (available on request) from other longitudinal models were very similar in magnitude, except that the associations for moderate control with acute and nonspecific admissions were insignificant in the fixed-effects model. All models had small and nonsignificant associations of better control on hypoglycemic admissions.
Table 3.
Multiple Regression Models of Longitudinal Associations between Practice Quality and Practice Emergency Admission Rates for All Short-Term, Hyperglycemic, and Hypoglycemic Emergency Admissions
| All Short Term | Acute Hyperglycemic | Nonspecific Hyperglycemic | Hypoglycemic | |||||
|---|---|---|---|---|---|---|---|---|
| Coefficient† | Z-Statistic | Coefficient | Z-Statistic | Coefficient | Z-Statistic | Coefficient | Z-Statistic | |
| Longitudinal model‡ | ||||||||
| Glycated hemoglobin (HbA1c) ≤7.4/7.5 | 0.991 | −3.74** | 0.989 | −2.92** | 0.991 | −2.78** | 0.999 | −0.20 |
| 7.4/7.5<HbA1c ≤10 | 0.992 | −3.08** | 0.990 | −2.30* | 0.991 | −2.45** | 0.998 | −0.37 |
| HbA1c monitored | 1.008 | 2.9** | 1.006 | 1.40 | 1.011 | 2.97** | 1.002 | 0.27 |
| HbA1c excluded | 0.999 | −0.39 | 0.999 | −0.14 | 0.999 | −0.3 | 0.994 | −0.920 |
| Year: 2005§ | 1.058 | 4.52** | 1.126 | 6.15** | 0.996 | −0.01 | 1.060 | 2.39* |
| Year: 2006§ | 1.066 | 3.30** | 1.237 | 7.31** | 0.931 | −2.43** | 1.041 | 0.253 |
| Diabetes prevalence | 1.074 | 4.52** | 1.087 | 2.94** | 1.104 | 3.13** | 1.001 | 0.04 |
| Efron's R2¶ | 0.359 | 0.315 | 0.204 | 0.086 | ||||
Statistically significant at 5% level.
Statistically significant at 1% level.
Coefficients reported as incident rate ratios. Quality indicators measured as percentages. Prevalence and baseline admission rate measure in standard deviation units. The percentage change in the admission rate associated with a 1 unit change in a continuous explanatory variable, holding all other variables constant, can be calculated as (coefficient−1)100%. The coefficients on the year binary variables show the difference in admissions in the year compared with 2004/2005 holding all other factors constant.
The longitudinal models include the same time-varying explanatory variables as the cross-sectional models.
Compared with baseline year (2004/2005).
Obtained from the R2 from a regression of actual admission rates on predicted admission rates.
Financial Implications
Under the QOF incentive scheme the financial reward for the moderate control indicator (DM7) increased linearly with the ratio of diabetics with at least moderate control to those declared eligible, between a lower threshold of 0.4 and an upper threshold of 0.9. Further increases in the ratio did not yield additional reward. Achieving the upper threshold in 2006/2007 would have earned the average practice £1,375 (U.S.$2,063). For the indicator of good control (DM6) the lower and upper thresholds were 0.40 and 0.50 and an average practice would have received £2,125 (U.S.$3,188) for achieving the upper threshold.
In 2006/2007, the average family practice in England had 32 (13.3 percent) of its reported diabetic patients with recorded poor control. In 2006/2007 a practice with 5 percent more patients with moderate rather than poor control would have had hospital admission costs for short-term diabetic complications that were lower by £771 (95 percent CI: £533–£1,012) (U.S.$1,157 [95 percent CI: U.S.$799–U.S.$1,518]). Such a practice would have earned £146 (U.S.$219) more from the incentive scheme if it was between the lower and upper limits for the moderate control indicator. However, in 2006/2007, 96 percent of practices were above the upper threshold for at least moderate control (DM7) (and 79 percent above the upper threshold for good control [DM6]) and so would have received no additional direct financial reward for such an improvement in diabetes control.
DISCUSSION
Potential Limitations
Our study was ecological, measuring quality of care at the practice level. We therefore could not relate an individual's risk of admission for short-term diabetic complications to his or her quality of care. This may lead to biased estimates of the association if the relationship is nonlinear or if important covariates were omitted in aggregating to practice level. We did, however, include a rich set of covariates measured at practice level.
The prevalence of diabetes recorded by family practices in our study—3.7 percent in 2006/2007—was about a quarter less than prevalence estimates from the Health Survey for England (Massó González et al. 2009). In addition to including reported practice prevalence in our models, we allow for under-recording of prevalence by including practice population demographic and socioeconomic characteristics that will be correlated with prevalence.
The negative association between practice glycemic control and practice admissions does not prove that better control causes lower admissions. The association may be due to confounding by unobserved factors that increased admissions and were negatively correlated with recorded glycemic control. For example, there might be a negative association—even if control has no effect on admissions—if practices with more deprived populations have higher diabetes prevalence (and hence more admissions) and also find it harder to reduce patients' HbA1c levels. However, in our cross-sectional analysis we included a rich set of important practice and patient population covariates, including baseline admission rates. Our longitudinal analysis compared changes in practices' admissions over time with changes in quality, thereby removing spurious correlations arising from unobserved factors that do not change over time.
It is possible that practices with better glycemic control also provided better access for diabetic patients to the practice, with longer opening times and more nurses, so that patients would be more likely to use the practice rather than the hospital when experiencing complications. This interpretation of the results would not change the basic message of the paper—practices with better overall diabetes management tend to have lower emergency admission rates for short-term diabetic complications.
There is a long-term upward trend in emergency diabetes admissions (Appendix Figure SA1), partly because of an underlying trend increase in the prevalence of diagnosed diabetes, especially in Type 2 diabetes (Information Centre for Health and Social Care 2006; Massó González et al. 2009;). This trend continued between 2004/2005 and 2007/2008 despite the improvements in practice recorded glycemic control. However, our cross-sectional analysis of the association between control and admissions across practices allowed for the growth in admissions over time. Moreover, our longitudinal analysis showed that, although admissions generally increased, the increase was less for practices with greater improvements in quality.
We believe that the observed association suggests that better management of diabetes in family practice reduces admissions for hyperglycemic complications without increasing admissions for hypoglycemic complications.
Implications of Results
Our study has shown that family practices with a higher proportion of recorded diabetic patients with moderate rather than poor glycemic control had significantly lower rates of emergency hospital hyperglycemic admissions. There was no significant association of practice diabetic control with hypoglycemic admissions. We also found that what mattered was moving patients from poor to moderate control: Having more patients with good rather than moderate control was associated with much smaller and statistically insignificant reduction in admissions.
The reductions in emergency admission for all short-term diabetic complications associated with improvements in glycemic control were modest for individual practices—a 5 percent higher proportion of patients with moderate diabetic control rather than poor control was associated with 0.3 fewer emergency admissions per year for the average practice. Reproduced nationally, however, this would imply 2,300 fewer emergency admissions each year in England.
The study also has implications for the design of pay-for-performance schemes in primary care. The main aim of such schemes is to improve patient outcomes by modifying the behavior of the medical professionals responsible for their care. However, the lag times involved with most chronic diseases make it difficult to attribute an outcome to the activity of a particular physician or medical group, or to adjust for external factors beyond the physician's control (Doran 2008). Most pay-for-performance initiatives do not, therefore, tie payments directly to outcomes, but to process activities and intermediate outcomes over which physicians have more direct control and for which there is evidence or a professional consensus for long-term benefit (Bruni et al. 2009; Scott et al. 2009; Lee et al. 2010;). This was the approach taken during the development of the U.K. QOF (Roland 2004).
We did not test whether the QOF improved quality because we did not have data on quality before the scheme was introduced. There is evidence from tracker studies of samples of practices that the QOF incentive scheme accelerated an already upward trend in quality of diabetic care processes and glycemic control (Campbell et al. 2007; Ashworth, Medina, and Morgan 2008; Doran et al. 2008a; Calvert et al. 2009; Alshamsan et al. 2010;). Coupled with our findings that better quality is associated with fewer emergency admissions, this implies that the incentive scheme is likely to have improved outcomes for diabetic patients.
Our study suggests that the basic assumption of the incentive scheme—that improving intermediate outcomes in primary care will result directly or indirectly in improved outcomes for patients and reduced hospital costs—appears to be justified in the case of glycemic control. Other studies have suggested mechanisms by which improved intermediate outcomes were achieved (Maisey et al. 2008). Practice record keeping improved under the QOF. Installation of electronic record systems was required for participation in the incentive scheme. New software became available to assist practices in increasing their quality scores. Such improved record keeping has been shown to improve diabetic care (Peterson et al. 2008). Practices also employed more staff under the incentive scheme: The number of family practitioners increased by 15 percent, and the number of practice nurses increased by 21 percent, between 2002 and 2006 (Information Centre for Health and Social Care 2009c). Ashworth and Armstrong (2006) and Griffiths et al. (2010) report that practices with more family practitioners and practice nurses, respectively, had higher QOF quality points scores.
By 2006/2007 the vast majority of practices were performing above the standards required for maximum remuneration under the incentive scheme, despite potential for improvements in poor glycemic control in their populations, but would have received no additional financial reward for improvements to their patients' glycemic control. This suggests that the financial incentives in the QOF were misaligned with the outcomes they were intended to achieve.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The National Primary Care Research and Development Centre receives core funding from the DOH. The views expressed are those of the authors and not necessarily those of the DOH. We are grateful to the National Health Service Information Centre for providing access to Hospital Episode Statistics. We would like to thank three anonymous reviewers, Stephen Morris, and participants at the Health Econometrics and Data Group seminar series in York for helpful comments.
Disclosures: Professor Roland reports serving as an academic adviser to the Government and British Medical Association negotiating teams during the development of the U.K. pay-for-performance scheme in 2001 and 2002. There are no other disclosures.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Table SA1: Classification of Emergency Short-Term Diabetes Admissions.
Table SA2: Definitions of ICD-10 and HRG Codes.
Table SA3: Multiple Regression Models of Practice Emergency Admission Rates for All Short-Term, Hyperglycemic, and Hypoglycemic Emergency Admissions: Incident Rate Ratios fromNegative Binomial Regressions.
Figure SA1: Emergency Diabetes Admission Rates per 10,000 Person Years 1997/1998 to 2006/2007.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Agency for Healthcare Quality and Research (AHQR) AHRQ Quality Indicators—Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Rockville, MD: 2004. Agency for Health Care Quality and Research, publication No. 02-R0203 [accessed on January 2007]. Available at: http://www.qualityindicators.ahrq.gov/pqi_download.htm. [Google Scholar]
- Alshamsan R, Millett C, Majeed A, Khunti K. Has Pay for Performance Improved the Management of Diabetes in the United Kingdom? Primary Care Diabetes. 2010;4(2):73–8. doi: 10.1016/j.pcd.2010.02.003. [DOI] [PubMed] [Google Scholar]
- Ashworth M, Armstrong D. The Relationship between General Practice Characteristics and Quality of Care: A National Survey of Quality Indicators Used in the UK Quality and Outcomes Framework, 2004–5. BMC Family Practice. 2006;7:68. doi: 10.1186/1471-2296-7-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashworth M, Medina J, Morgan M. Blood Pressure Monitoring and Control in England: A Comparison between Least and Most Deprived Areas Based on Data from the ‘Quality and Outcomes Framework.’. British Medical Journal. 2008;337:a2030. doi: 10.1136/bmj.a2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of Socioeconomic Status on Hospital Use in New York City. Health Affairs (Millwood) 1993;12:162–73. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- Bindman A, Grumbach K, Osmond D, Komaromy A, Vranizan K, Lurie N. Preventable Hospitalizations and Access to Health Care. Journal of the American Medical Association. 1995;274:305–11. [PubMed] [Google Scholar]
- Blundell R, Griffith R, Windmeijer F. Individual Effects and Dynamics in Count Data Models. Journal of Econometrics. 2002;108:113–31. [Google Scholar]
- Bottle A, Millett C, Xie Y, Saxena S, Wachter R, Majeed A. Quality of Primary Care and Hospital Admissions for Diabetes Mellitus in England. Journal of Ambulatory Care Management. 2008;31:226–38. doi: 10.1097/01.JAC.0000324668.83530.6d. [DOI] [PubMed] [Google Scholar]
- Briscoe V, Davis S. Hypoglycemia in Type 1 and Type 2 Diabetes: Physiology, Pathophysiology, and Management. Clinical Diabetes. 2006;24:115–21. [Google Scholar]
- Bruni M, Nobilio L, Ugolini C. Economic Incentives in General Practice: The Impact of Pay-for-Participation and Pay-for-Compliance Programs on Diabetic Care. Health Policy. 2009;90:140–8. doi: 10.1016/j.healthpol.2008.09.008. [DOI] [PubMed] [Google Scholar]
- Calvert M, Shankar A, McManus R, Lester H, Freemantle N. Effect of the Quality and Outcomes Framework on Diabetes Care in the United Kingdom: Retrospective Cohort Study. British Medical Journal. 2009;380:1366–70. doi: 10.1136/bmj.b1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell S, Reeves D, Kontopantelis E, Sibbald B, Roland M. Improvements in Clinical Quality in English Primary Care before and after the Introduction of a Pay for Performance Scheme: Longitudinal Cohort Study. New England Journal of Medicine. 2007;351:181–90. doi: 10.1056/NEJMsr065990. [DOI] [PubMed] [Google Scholar]
- Department of Health (DOH) National Service Framework for Diabetes. London: Department of Health; 2001. [Google Scholar]
- Department of Health (DOH) QOF Guidance. London: Department of Health; 2004. [accessed on February 2008]. Available at: http://www.dh.gov.uk/en/Policyandguidance/Organisationpolicy/Primarycare/Primarycarecontracting/QOF/DH_4125653. [Google Scholar]
- Department of Health (DOH) Resource Allocation Weighted Capitation Formula. 6th Edition. Leeds: Department of Health; 2008. [accessed on May 2009]. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_091849. [Google Scholar]
- Doran T. Lessons from Early Experience with Pay for Performance. Disease Management and Health Outcomes. 2008;16:69–77. [Google Scholar]
- Doran T, Fullwood C, Gravelle H, Reeves D, Roland M. Exclusion of Patients from Pay-for-Performance Targets by English Physicians. New England Journal of Medicine. 2008a;359:274–84. doi: 10.1056/NEJMsa0800310. [DOI] [PubMed] [Google Scholar]
- Doran T, Fullwood C, Kontopantelis E, Reeves D. The Effect of Financial Incentives on Inequalities in the Delivery of Primary Care in England. Lancet. 2008b;372:728–36. doi: 10.1016/S0140-6736(08)61123-X. [DOI] [PubMed] [Google Scholar]
- Downing A, Rudge G, Cheng Y, Tu Y, Keen J, Gilthorpe M. Do the UK Government's New Quality and Outcomes Framework (QOF) Scores Adequately Measure Primary Care Performance? A Cross-Sectional Survey of Routine Healthcare Data. BMC Health Services Research. 2007;7:166. doi: 10.1186/1472-6963-7-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravelle H, Sutton M, Ma A. Doctor Behaviour under a Pay for Performance Contract: Treating, Cheating and Case Finding? Economic Journal. 2010;120:F129–56. [Google Scholar]
- Griffiths P, Murrells T, Maben J, Jones S, Ashworth M. Nurse Staffing and Quality of Care in UK General Practices. British Journal of General Practice. 2010;60:e36–48. doi: 10.3399/bjgp10X482086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Information Centre for Health and Social Care. Health Survey for England 2006. Leeds, England: The Information Centre; 2006. [Google Scholar]
- Information Centre for Health and Social Care. HRG Definitions Manual. Leeds, England: The Information Centre for Health and Social Care; 2007a. [accessed on May 1, 2009]. Available at: http://www.ic.nhs.uk/services/the-casemix-service/using-thisservice/reference/archive/hrg-v35-toolkit/ [Google Scholar]
- Information Centre for Health and Social Care. 2007b. Online GP Practice Results Database [accessed on October 1, 2007]. Available at: http://www.qof.ic.nhs.uk/
- Information Centre for Health and Social Care. Hospital Episode Statistics. Leeds: The Information Centre for Health and Social Care; 2009a. [accessed on May 1, 2009]. Available at: http://www.hesonline.org.uk/ [Google Scholar]
- Information Centre for Health and Social Care. Attribution Data Set. Leeds: The Information Centre for Health and Social Care; 2009b. [accessed on May 1, 2009]. Available at: http://www.ic.nhs.uk/statistics-and-data-collections/population-and-geography. [Google Scholar]
- Information Centre for Health and Social Care. General and Personal Medical Services England 1998–2008. Leeds, England: The Information Centre; 2009c. [Google Scholar]
- Lee T, Cheng S, Chen C, Lai M. A Pay-for-Performance Program for Diabetes Care in Taiwan: A Preliminary Assessment. American Journal of Managed Care. 2010;16:65–9. [PubMed] [Google Scholar]
- Lloyd DC, Harris CM, Clucas DW. Low Income Scheme Index: A New Deprivation Scale Based on Prescribing in General Practice. British Medical Journal. 1995;310:165–9. doi: 10.1136/bmj.310.6973.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisey S, Steel N, Marsh R, Gillam S, Fleetcroft R, Howe A. Effects of Payment for Performance in Primary Care: Qualitative Interview Study. Journal of Health Services Research and Policy. 2008;13:133–29. doi: 10.1258/jhsrp.2008.007118. [DOI] [PubMed] [Google Scholar]
- Massó González E, Johansson S, Wallander M, García Rodríguez L. Trends in the Prevalence and Incidence of Diabetes in the UK: 1996–2005. Journal of Epidemiology and Community Health. 2009;63:332–6. doi: 10.1136/jech.2008.080382. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. NICE Clinical Guideline 66: The Management of Type 2 Diabetes. London: National Institute for Health and Clinical Excellence; 2008. [Google Scholar]
- NHS Employers. Quality and Outcomes Framework Guidance for GMS Contract 2008/09. London: NHS Confederation; 2008. [Google Scholar]
- Office for National Statistics. 2008. Neighbourhood Statistics [accessed on December 1, 2008]. Available at: http://www.neighbourhood.statistics.gov.uk/dissemination/
- Peterson K, Arneson T, Radosevich D, Corbett V, O'Connor P, Weinhandl J, Nyman J, Lange C, Prineas R, Hannan P, Smith S. Improving Diabetes Care in Practice: Findings from the TRANSLATE Trial. Diabetes Care. 2008;31:2238–43. doi: 10.2337/dc08-2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purdy S, Griffin T, Salisbury C, Sharp D. Ambulatory Care Sensitive Conditions: Terminology and Disease Coding Need to Be More Specific to Aid Policy Makers and Clinicians. Public Health. 2009;123:169–73. doi: 10.1016/j.puhe.2008.11.001. [DOI] [PubMed] [Google Scholar]
- Roland M. Linking Physician Pay to Quality of Care: A Major Experiment in the UK. New England Journal of Medicine. 2004;351:1448–54. doi: 10.1056/NEJMhpr041294. [DOI] [PubMed] [Google Scholar]
- Saxena S, George J, Barber J, Fitzpatrick J, Majeed A. Association of Population and Practice Factors with Potentially Avoidable Admission Rates for Chronic Diseases in London: Cross Sectional Analysis. Journal of the Royal Society of Medicine. 2006;99:81–9. doi: 10.1258/jrsm.99.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott A, Schurer S, Jensen PH, Sivey P. The Effects of an Incentive Program on Quality of Care in Diabetes Management. Health Economics. 2009;18:1091–108. doi: 10.1002/hec.1536. [DOI] [PubMed] [Google Scholar]
- Weissman J, Gatsonis C, Epstein A. Rates of Avoidable Hospitalization by Insurance Status in Massachusetts and Maryland. Journal of the American Medical Association. 1992;268:2388–94. [PubMed] [Google Scholar]
- World Health Organization. 2007. International Statistical Classification of Diseases and Related Health Problems 10th Revision [accessed on October 1, 2008]. Available at: http://www.who.int/classifications/apps/icd/icd10online/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


