Abstract
Background:
Large-scale epidemiologic data on stroke in HIV-infected persons are scarce, especially in an era of combination antiretroviral therapies, which have prolonged patient survival, but may boost stroke risk. We assessed trends in the proportion of HIV infection among patients with stroke in the United States.
Methods:
Data were obtained from all states within the United States that contributed to the Nationwide Inpatient Sample. All patients admitted to hospitals between 1997 and 2006 with a primary discharge diagnosis of stroke (identified by the International Classification of Diseases, Ninth Revision procedure codes) were included. Time trends in the proportion of these patients with HIV diagnosis were computed, and independent predictors of comorbid HIV diagnosis evaluated using multivariable logistic regression.
Results:
Of all (ischemic and hemorrhagic) stroke hospitalizations, patients with comorbid HIV infection constituted 0.09% in 1997 vs 0.15% in 2006 (p < 0.0001). Actual numbers of overall US stroke hospitalizations lessened 7% (998,739 to 926,997), while actual numbers of stroke hospitalizations with coexisting HIV infection rose 60% (888 to 1,425). Patients with comorbid HIV infection comprised 0.08% of ischemic strokes in 1997 vs 0.18% in 2006 (p < 0.0001), but their proportion of hemorrhagic strokes did not significantly change. Factors independently associated with higher odds of comorbid HIV diagnosis were Medicaid insurance, urban hospital type, dementia, liver disease, renal disease, and cancer.
Conclusion:
Over the last decade in the United States, there has been a substantial and significant rise in patients hospitalized for stroke with coexisting HIV infection. This has important public health and socioeconomic consequences.
Cerebrovascular disease in HIV-infected patients is generally underrecognized, underreported, and understudied.1 Indeed, there are relatively few epidemiologic data quantifying or qualifying associations of HIV infection with stroke risk.2 Specifically, recent data on stroke trends in HIV-infected persons during a period marked by the advent of effective combination antiretroviral regimens that have reduced morbidity and mortality, but which have also been linked to increased risk of stroke, are lacking. A better understanding of the evolving occurrence of stroke in HIV-infected patients, especially on a nationwide level, could raise awareness and open up avenues for curbing this major neurologic complication of HIV.
The objective of this study was threefold. First, we aimed to assess recent time trends in the proportion of HIV infection among persons hospitalized in the United States with stroke. Second, we set out to examine how these time trends varied by index stroke type. Finally, we evaluated sociodemographic, hospital, and clinical factors independently associated with presence of HIV infection in patients hospitalized for stroke.
METHODS
Data were obtained from the Nationwide Inpatient Sample (NIS), which approximates a stratified 20% sample of all non-Federal, short-term, general, and specialty hospitals serving adults in the United States. Detailed information on the design of the NIS is available at http://www.hcup-us.ahrq.gov. From 1997 to 2006, NIS captured discharge-level information on several million discharges each year. A unique hospital identifier allows for linkage of discharge data to an NIS dataset with hospital characteristics. The Nebraska and Iowa Hospital Associations (Iowa beginning in data year 2001) prohibit release of discharge data on HIV, and so information on these discharges was therefore not included in the NIS.
All patients with a primary diagnosis of stroke were included whether they were alive or dead at the time of discharge. To analyze percentages of hospital-based stroke diagnoses, all discharges with International Classification of Diseases, Ninth Revision (ICD-9)-CM codes 430.xx–438.xx included in any of the diagnoses were identified. For patients with >1 reported code, only the first reported code was included to avoid double counting patients with multiple reported codes. Total number of stroke hospitalizations was obtained by summing across codes. In a secondary analysis to ensure that all strokes were captured, we included stroke listed as a primary or secondary diagnosis. However, since such an approach could also lead to overascertainment, we utilized an appropriate correction for each code, to account for any potential overascertainment.3 By this procedure, the estimated number of strokes by ICD-9-CM code 430 to 438 was obtained by multiplying the weighted total number of discharges with each ICD-9-CM code by its estimated positive predictive value (PPV) for stroke.3 The PPVs were derived by pooling data from previously published studies.3
We computed the weighted proportion of stroke hospitalizations that occurred in persons who had a comorbid HIV diagnosis across the 10-year study period, by stroke type and overall. Trend p values were computed by including year as a continuous variable in the logistic regression models while adjusting for the NIS survey design. We also plotted the primary stroke hospitalization rates in the general HIV-negative vs HIV-positive population in the United States, and computed the weighted frequency of primary stroke hospitalizations in HIV-positive vs HIV-negative patients in order to obtain the rate numerators. Rate denominators were derived using US census data for the total number of persons with and without HIV in the United States. HIV prevalence data were not available for year 1997, which was therefore excluded from the above plots. Rate comparisons were performed using the Z test.
Univariate logistic regression adjusted for the survey design variables was used to evaluate sociodemographic, hospital-level, and clinical predictors one at a time (unadjusted analysis). To evaluate the independent association of these factors with presence of comorbid HIV diagnosis, we used multivariable logistic regression modeling after adjustment for the survey design variables. In the first multivariable model, sociodemographic (age, race [white, black, other, unknown], primary payer [Medicare, Medicaid, private, other]) and hospital factors (Northeast, Midwest, South, West), bed size (small, medium, large), stroke volume by quartile, and location/teaching status (rural, urban nonteaching, urban teaching) were adjusted for. The second multivariable model adjusted for the variables in model 1 in addition to clinical factors (vascular disease entities including hypertension, myocardial infarction, diabetes, and atrial fibrillation, as well as other chronic general medical conditions including liver disease, renal disease, and chronic pulmonary disease). All data analyses were conducted using SAS (version 9.1; SAS Institute Inc., Cary, NC). To summarize the relation between each of the above factors and the odds of having a comorbid HIV diagnosis, we report the unadjusted and adjusted odds ratios and the corresponding 95% confidence intervals as derived from the above logistic regression models. Statistical hypotheses were tested using p < 0.05 as the level of significance.
Standard protocol approvals, registrations, and patient consents.
Since this was an analysis of a publicly available deidentified administrative online database, formal review by the Institutional Review Board at our institution was not required.
RESULTS
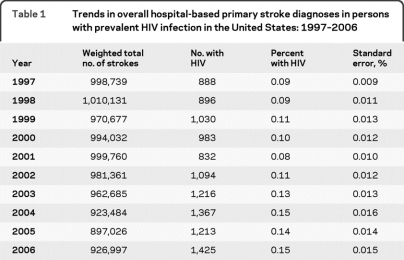
Over the study period, the weighted number of total primary stroke diagnoses in the United States generally declined, with 71,742 fewer incident strokes (7.2% relative drop) in 2006 compared to 1997 (table 1). However, total primary stroke diagnoses among persons with comorbid HIV infection generally rose (table 1), with 537 more incident strokes (60.5% relative rise) in 2006 compared to 1997 (trend for change in proportion: p < 0.0001). Figure e-1 and table e-1 on the Neurology® Web site at www.neurology.org show that in the general HIV-negative population, stroke hospitalization rates decreased from 375 hospitalizations per 100,000 persons in 1998 to 311 hospitalizations per 100,000 persons in 2006 (p < 0.0001), a 17% rate decrease. As seen in figure e-2 and table e-1, the results in the HIV+ population were less pronounced after taking into account population size, since the observed increase in the absolute number of strokes was largely explained by a growing HIV+ US population which increased by close to 40% from 1998 to 2006. However, even after adjustment for population size, following an initial period of decline prior to 2001 there was a roughly 43% increase in the rate of stroke hospitalizations in the HIV+ US population after 2001 from 90 hospitalizations per 100,000 persons in 2001 to 129 hospitalizations per 100,000 persons in 2006 (p = 0.02).
Table 1.
Trends in overall hospital-based primary stroke diagnoses in persons with prevalent HIV infection in the United States: 1997–2006
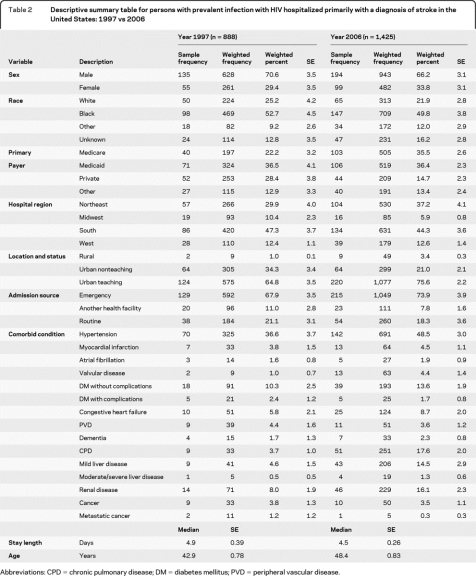
Table 2 displays descriptive summary statistics (for simplicity, only results for 1997 and 2006 are shown) for patients hospitalized with primary stroke who had comorbid HIV infection. These results were broadly comparable across several variables. There was an approximately 6-year rise in median patient age by 2006. Of note, there were also changes of greater than 10% points across the decade in the following variables: increase in Medicare patients and decrease in privately insured patients; rise in patients encountered at urban teaching hospitals and decrease in those seen at nonurban teaching facilities; greater prevalence of hypertension, chronic pulmonary disease, and mild liver disease. The median duration of hospitalization of HIV-infected patients with stroke remained constant (4.9 vs 4.5 days).
Table 2.
Descriptive summary table for persons with prevalent infection with HIV hospitalized primarily with a diagnosis of stroke in the United States: 1997 vs 2006
Abbreviations: CPD = chronic pulmonary disease; DM = diabetes mellitus; PVD = peripheral vascular disease.
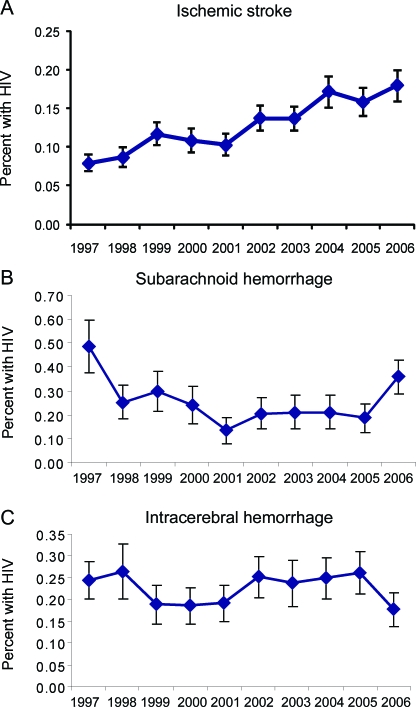
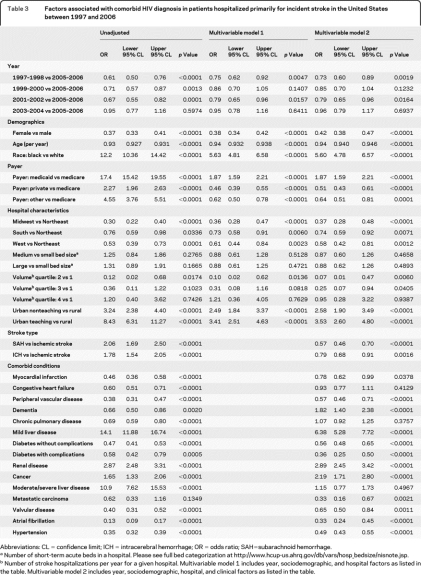
Figure 1 and table e-2 show the percentage of coexistent HIV infection among primary stroke diagnoses stratified by type in the United States from 1997 to 2006. As shown, the proportion of ischemic strokes that occurred in patients with a comorbid HIV diagnosis more than doubled from 1997 to 2006 (trend: p < 0.0001). Conversely, the proportion of incident subarachnoid hemorrhage (SAH) (trend: p = 0.27) or incident intracerebral hemorrhage (ICH) (trend: p = 0.88) that occurred in patients with a comorbid HIV diagnosis did not follow a significant linear trend across time. Results of the secondary analysis including both primary and secondary stroke diagnoses were similar to those of primary strokes alone (figure e-3): there was an increase in the proportion of HIV+ diagnoses among patients who had a diagnosis of ischemic stroke (trend: p < 0.0001), but not among patients who had SAH (trend: p = 0.56) or ICH (trend: p = 0.77). Table 3 displays results for the relation between various factors and the odds of comorbid HIV diagnosis in patients primarily hospitalized with stroke. In unadjusted analysis, increasing age, female sex, and non-Northeast hospital region were associated with significantly lesser odds of comorbid HIV diagnosis, while nonwhite race, non-Medicare insurance, nonrural hospital type, and index hemorrhagic strokes were associated with significantly greater odds of comorbid HIV diagnosis. Medical conditions associated with greater odds of comorbid HIV diagnosis were mild liver disease, moderate/severe liver disease, renal disease, and cancer.
Figure 1. Trends in stroke hospitalization by type among persons with a diagnosis of HIV in the United States population 1997–2006.
(A) Ischemic stroke: trend p value < 0.0001. (B) Subarachnoid hemorrhage: trend p value = 0.27. (C) Intracerebral hemorrhage: trend p value = 0.88.
Table 3.
Factors associated with comorbid HIV diagnosis in patients hospitalized primarily for incident stroke in the United States between 1997 and 2006
Abbreviations: CL = confidence limit; ICH = intracerebral hemorrhage; OR = odds ratio; SAH=subarachnoid hemorrhage.
Number of short-term acute beds in a hospital. Please see full bed categorization at http://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp.
Number of stroke hospitalizations per year for a given hospital. Multivariable model 1 includes year, sociodemographic, and hospital factors as listed in the table. Multivariable model 2 includes year, sociodemographic, hospital, and clinical factors as listed in the table.
Both multivariable models produced similar OR estimates, and were consistent with the directions of the unadjusted analysis except for a few noteworthy differences (table 3). Unlike the unadjusted analysis, multivariable model results indicated that compared to Medicare patients those with private or “other” insurance actually had lesser odds of comorbid HIV diagnosis. Another important deviation from the unadjusted analysis was that in the multivariable analyses hemorrhagic strokes were associated with a decrease (not an increase) in the odds of comorbid HIV diagnosis when compared to patients with ischemic stroke, the unadjusted result likely mainly confounded by age, since younger patients were much more likely to have comorbid HIV diagnosis and hemorrhagic stroke (the positive association of SAH and ICH stroke types with comorbid HIV diagnosis all but disappeared with adjustment for age alone).
DISCUSSION
We found that over the last decade, there was a significant rise of approximately 67% in the proportion of patients hospitalized for stroke who had prevalent HIV infection in the United States. The rise occurred in the setting of a 7% decrease in actual numbers of overall stroke hospitalizations in 2006 (vs 1997), and a 60% increase in actual numbers of stroke hospitalizations with coexisting HIV infection in 2006 (vs 1997), indicating that the boost in proportion of patients hospitalized for stroke with prevalent HIV infection was not driven by recently recognized reductions in stroke incidence due to traditional vascular risk factor control, but possibly by evolving circumstances unique to HIV-infected patients. Although the absolute numbers of stroke hospitalizations with HIV infection are relatively small, reflecting the fact that stroke is generally an infrequent manifestation of HIV infection, this steep rise over a short period of time may be of major public health concern. This is coupled with an increase in patients on Medicaid and a decrease in those on private insurance, which has important socioeconomic consequences.
It is noteworthy that the observed increase in patients hospitalized for stroke with coexisting HIV infection seemed compelled by a rise in ischemic stroke and not hemorrhagic stroke hospitalizations. If anything, the proportions of patients hospitalized for SAH and ICH with prevalent HIV infection were lower in 2006 compared to 1997, albeit nonsignificantly. Conversely, the proportion of patients hospitalized for ischemic stroke with comorbid HIV infection more than doubled by 2006, and it appears that the first major uptick began about midyear of 2001.
The precise reasons for the rise in patients hospitalized for stroke with coexisting HIV infection are not immediately clear and are beyond the scope of this administrative dataset to decipher. However, there are some speculations that could be made based partly on these results as well as prior knowledge. The median age for stroke in this population was the fifth decade, which is much lower than that of the non-HIV-infected population. This indicates that HIV infection or its treatment is directly related to the stroke pathophysiology in this population. HIV infection can cause stroke via several mechanisms including HIV-stimulated endothelial activation (predisposing to accelerated atherosclerosis), opportunistic infections, neoplasia, HIV-induced cardiac disease, HIV-associated cerebral vasculopathy, HIV-induced systemic vasculitis, prothrombosis, and metabolic derangements.4–8 So for instance, the observed increase in several metabolic factors over time may have predisposed these patients to greater risk for developing strokes. It is also possible that recently there has been greatly increased action by the virus in facilitating these mechanisms to the extent that ischemic stroke incidence in particular is much higher, but this would seem unlikely without any supportive evidence.
A more plausible explanation could be that these trends reflect consequences of broad use of combination antiretroviral therapies in HIV-infected patients. First, combination antiretroviral therapy increases life expectancy and as such inadvertently boosts the risk of ischemic stroke, a condition that is highly age-correlated and occurs with greater length of time exposure to conventional vascular risk factors.1 In fact, the increase in stroke also coincides with the introduction of combination antiretroviral drugs in the mid-1990s and increased usage of these drugs in subsequent years. Also supporting this notion is the change in the demographics over time, with older, male, and African American subjects encountered later in the study period. Each of these demographic factors could independently increase the rate of stroke alone and account for some of the observed differences. Similarly, longer exposure to HIV, even at low viral load levels, may allow for the direct effects of the virus to increase stroke risk. Second, combination antiretroviral therapy directly causes immune activation and metabolic and endothelial dysfunction that can accelerate atherosclerosis9–11 and lead to symptomatic ischemic vascular events.12,13 Third, hepatotoxicity is a known complication of combination antiretroviral drug treatment,14 and in our multivariable analyses among factors independently linked to coexistent HIV infection with stroke hospitalization, mild liver disease had by far the strongest association. It is possible that the hepato-renal dysfunction may contribute to the metabolic syndrome leading to accelerated vascular disease.
This study has limitations. We cannot exclude possible inaccurate reporting of ICD codes, we lacked information on the rate of nonhospital strokes in the country, and did not count stroke as a secondary hospital diagnosis. Furthermore, we were unable to evaluate use or duration of antiretroviral therapy prior to the index stroke hospitalization, or at discharge. The study benefited from its nationwide scope and clinician-diagnosed incidence data.
Supplementary Material
ACKNOWLEDGMENT
The authors thank Daniela Markovic, MS, and Jeffrey Gornbein, DrPh, of the UCLA School of Medicine for statistical consultation.
- ICD-9
- International Classification of Diseases, Ninth Revision
- ICH
- intracerebral hemorrhage
- NIS
- Nationwide Inpatient Sample
- PPV
- positive predictive value
- SAH
- subarachnoid hemorrhage
Supplemental data at www.neurology.org.
DISCLOSURE
Dr. Ovbiagele serves on a scientific advisory board for Avanir Pharmaceuticals and serves as an Assistant Editor of Stroke, an Associate Editor of Journal Watch Neurology and BMC Public Health, and on the editorial boards of the Journal of Stroke and Cerebrovascular Diseases and Stroke Research and Treatment. Dr. Nath serves on scientific advisory boards for Biogen Idec and DioGenix, Inc.; serves as an Associate Editor for the Journal of Neurovirology; may accrue revenue on patents re: Tat as an immunogen; Diosgenin for treatment of neurodegenerative diseases; Role of Kv channels in neuroregeneration and protection; Role of Lominoid compounds as neuroprotective agents; and Tat ELISA; has served as a consultant for Nerveda Inc. and Elan Corporation; receives research support from the NIH; and has provided expert advice in medico-legal cases.
REFERENCES
- 1. Rabinstein AA. Stroke in HIV-infected patients: a clinical perspective. Cerebrovasc Dis 2003;15:37–44 [DOI] [PubMed] [Google Scholar]
- 2. Cole JW, Pinto AN, Hebel JR, et al. Acquired immunodeficiency syndrome and the risk of stroke. Stroke 2004;35:51–56 [DOI] [PubMed] [Google Scholar]
- 3. Williams GR, Jiang JG, Matchar DB, Samsa GP. Incidence and occurrence of total (first-ever and recurrent) stroke. Stroke 1999;30:2523–2528 [DOI] [PubMed] [Google Scholar]
- 4. Ortiz G, Koch S, Romano JG, Forteza AM, Rabinstein AA. Mechanisms of ischemic stroke in HIV-infected patients. Neurology 2007;68:1257–1261 [DOI] [PubMed] [Google Scholar]
- 5. Brilla R, Nabavi DG, Schulte-Altedorneburg G, et al. Cerebral vasculopathy in HIV infection revealed by transcranial Doppler: a pilot study. Stroke 1999;30:811–813 [DOI] [PubMed] [Google Scholar]
- 6. Connor MD, Lammie GA, Bell JE, Warlow CP, Simmonds P, Brettle RD. Cerebral infarction in adult AIDS patients: observations from the Edinburgh HIV Autopsy Cohort. Stroke 2000;31:2117–2126 [DOI] [PubMed] [Google Scholar]
- 7. Ances BM, Bhatt A, Vaida F, et al. Role of metabolic syndrome components in human immunodeficiency virus-associated stroke. J Neurovirol 2009;15:249–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Qureshi AI, Janssen RS, Karon JM, et al. Human immunodeficiency virus infection and stroke in young patients. Arch Neurol 1997;54:1150–1153 [DOI] [PubMed] [Google Scholar]
- 9. Depairon M, Chessex S, Sudre P, et al. Premature atherosclerosis in HIV-infected individuals–focus on protease inhibitor therapy. AIDS 2001;15:329–334 [DOI] [PubMed] [Google Scholar]
- 10. Jerico C, Knobel H, Calvo N, et al. Subclinical carotid atherosclerosis in HIV-infected patients: role of combination antiretroviral therapy. Stroke 2006;37:812–817 [DOI] [PubMed] [Google Scholar]
- 11. Maggi P, Serio G, Epifani G, et al. Premature lesions of the carotid vessels in HIV-1-infected patients treated with protease inhibitors. AIDS 2000;14:F123–F128 [DOI] [PubMed] [Google Scholar]
- 12. d'Arminio A, Sabin CA, Phillips AN, et al. Cardio- and cerebrovascular events in HIV-infected persons. AIDS 2004;18:1811–1817 [DOI] [PubMed] [Google Scholar]
- 13. Friis-Moller N, Sabin CA, Weber R, et al. Combination antiretroviral therapy and the risk of myocardial infarction. N Engl J Med 2003;349:1993–2003 [DOI] [PubMed] [Google Scholar]
- 14. Cooper CL. HIV antiretroviral medications and hepatotoxicity. Curr Opin HIV AIDS 2007;2:466–473 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.