Abstract
Objective
To test the efficacy of a prevention intervention to reduce sexual risk behavior among Latino adolescents.
Design
Randomized controlled trial from April 2000 through March 2003, with data collection before and after intervention and at 3, 6, and 12 months.
Setting
Northeast Philadelphia schools.
Participants
Latinos aged 13 through 18 years (249 males and 304 females); 81.6% retained at 12-month follow-up.
Interventions
The HIV and health-promotion control interventions consisted of six 50-minute modules delivered by adult facilitators to small, mixed-gender groups in English or Spanish.
Main Outcome Measure
Self-reported sexual behavior.
Results
Analyses using generalized estimation equations over the follow-up period revealed that adolescents in the HIV intervention were less likely to report sexual intercourse (odds ratio, 0.66; 95% confidence interval [CI], 0.46-0.96), multiple partners (odds ratio, 0.53; 95% CI, 0.31-0.90), and days of unprotected intercourse (relative risk, 0.47; 95% CI, 0.26-0.84) and more likely to report using condoms consistently (odds ratio, 1.91; 95% CI, 1.24-2.93). Baseline sexual experience and language use moderated intervention efficacy. Adolescents assigned to the HIV intervention who were sexually inexperienced at baseline reported fewer days of unprotected sex (relative risk, 0.22; 95% CI, 0.08-0.63); Spanish speakers were more likely to have used a condom at last intercourse (odds ratio, 4.73; 95% CI, 1.72-12.97) and had a greater proportion of protected sex (mean difference,0.35; P<.01) compared with similar adolescents in the health-promotion intervention.
Conclusion
Results provide evidence for the efficacy of HIV intervention in decreasing sexual activity and increasing condom use among Latino adolescents.
Human immunodeficiency virus (HIV) and AIDS disproportionately affect Latino adolescents. The incidence of AIDS for adult and adolescent Latinos in 2001 was more than 3 times higher than that among their non-Hispanic white counterparts.1,2 Heterosexual contact is the major mode of HIV transmission among Latino adolescents.3 Data from the national Youth Risk Behavior Surveillance System show that the incidence of sexual intercourse before the age of 13 years, as well as multiple (>4) sexual partnerships, is higher among Latino youth than among non-Hispanic whites.4 Furthermore, studies have consistently documented lower condom use by Latino adolescents than by African American or white adolescents.4-6
Despite the high risk of sexually transmitted HIV infection among Latino adolescents, few controlled intervention studies have been conducted in this population. In an electronic literature search, we identified only 5 intervention studies from 1994 through 2004 with sexual behavior outcomes that had sizable proportions (25% or more of the sample) of Latino adolescents.7-11
In 3 studies,7-9 Latinos were included in tests of HIV risk-reduction curricula; however, the reported intervention effects on behavior were not consistent. Results from 1 study9 indicated that an HIV risk-reduction intervention had no effect on sexual behavior among students in 6 Los Angeles middle schools. Conversely, a test of a 2-year comprehensive school-based HIV/sexually transmitted disease and pregnancy-prevention program indicated significant sexual behavior outcomes for Latino adolescents.7 Latino adolescents in the intervention schools were significantly more likely to delay the initiation of sex, use condoms at last sex, and report fewer incidences of unprotected sex than those in the control schools. Because there was only 1 measure obtained 7 months after intervention, the long-term effects of the intervention are unknown.
Latino adolescents were targeted in only 2 studies.10,11 One study11 included Spanish-speaking Latino adolescents but was not a randomized controlled trial, and only one10 indicated that the intervention was culturally tailored for Latino adolescents. Sellers et al11 reported mixed results from a community AIDS prevention program. The intervention did not significantly affect frequency of sex, the onset of sexual activity for girls, or number of partners among boys compared with those factors in a control group. However, in the intervention city, boys were less likely to initiate their first sexual intercourse, whereas girls were less likely to have multiple partners.
Mixed results also were reported in a test of a behavioral intervention conducted with a majority sample (78%) of pregnant adolescent Latina mothers (mean age,16.7 years).10 At 6 months post intervention, adolescents who participated in the HIV prevention program were significantly more likely than those in the control group to decrease the number of sex partners. However, there were no significant intervention effects on behavior at 12-month follow-up.
In summary, data about the efficacy of behavioral interventions to reduce sexual risk behavior among Latino adolescents are sparse. Moreover, no randomized controlled intervention trials have been conducted with Latino adolescents who are monolingual Spanish speakers. An important recommendation by Flores et al12 and others13 supports the need to address language and cultural barriers in interventions for Latino youth. Therefore, the purpose of this study was to test the efficacy of a culture- and theory-based intervention designed to reduce HIV sexual risk behavior among Latino adolescents.
METHODS
PARTICIPANTS
A total of 684 adolescents were eligible to participate; data analyzed for this study included 553 self-identified Latino adolescents (249 males and 304 females). Most participants were Puerto Rican (472 [85.4%]) with nearly half (249 [45.0%]) born outside the mainland United States. Participants had a mean (SD) age of 14.9 (1.49) years and a median of ninth grade in school, with 86.9% of the students in grades 8 through 11. About 235 (42.5%) reported ever having sexual intercourse, and the mean (SD) age of first intercourse was 13.5 (1.81) years.
PROCEDURES
The study was a randomized controlled trial with data collection at preintervention; immediately after completion of the 2-day intervention; and at 3, 6, and 12 months after intervention. The human subjects committees of the University of Pennsylvania and the University of Michigan approved the study.
Latino students were recruited from 3 northeast Philadelphia high schools and community-based organizations within these neighborhoods. Students were invited to participate in “¡Cuídate! (Take Care of Yourself) The Latino Youth Health Promotion Program,” an 8-hour program conducted over 2 consecutive Saturdays. The study was implemented with a pilot group, and 5 subsequent groups enrolled sequentially across 5 months. Youth were eligible to participate if they self-reported as being Latino, were aged 13 through 18 years, and provided assent and parental consent. Non-Latino students (n=103) were not excluded from participation in the intervention but were excluded from the analysis. Students were asked their language preference and subsequently received the English or Spanish version of the questionnaires. The English versions were received by 412 adolescents and the Spanish versions by 141 adolescents.
Using a stratified permuted block randomization, we stratified adolescents according to gender, primary language, ethnicity (Latino and non-Latino), and age. On the basis of computer-generated random number sequences, adolescents were randomly assigned to the HIV risk-reduction intervention or the health-promotion intervention. Students received a T-shirt with the study logo for participating. In addition, they were compensated as much as $110 for participation: $40 after completion of the 2-session intervention, $20 for the 3- and 6-month follow-ups, and $30 for the12-month follow-up.
INTERVENTION
The process of developing ¡Cuídate! and details regarding the content of the curriculum have been previously described.14 The HIV risk-reduction and health-promotion interventions were similar in organization, format, length, and delivery mode. Both interventions involved small-group discussions, videos, interactive exercises, and skill-building activities. Functionally equivalent versions of the HIV risk-reduction and health-promotion curriculum in English and Spanish were developed and pilot tested.
The HIV risk-reduction curriculum tested in this study was an adaptation of Be Proud! Be Responsible!15 and similarly was based on social cognitive theory16 and the theories of reasoned action and planned behavior.17,18 ¡Cuídate! also incorporated salient aspects of Latino culture, specifically familialism, or the importance of family, and gender-role expectations. Abstinence and condom use were presented as culturally accepted and effective ways to prevent sexually transmitted diseases, including HIV.
The health-promotion intervention focused on behaviors related to significant health issues affecting Latinos. These behaviors included diet; exercise and physical activity; and cigarette, alcohol, and drug use. Latino cultural values were presented as an important context that supported positive health behaviors.
FACILITATORS AND FACILITATOR TRAINING
Facilitator recruitment, characteristics, and training have been described previously.14 The bilingual facilitators (n=41; 8 men and 33 women) had a mean (SD) age of 33.7 (10.23) years; and 34 (82.9%) self-identified as Puerto Rican. Facilitators were stratified according to age, gender, and ethnicity and were assigned according to computer-generated random number sequences to implement either the HIV risk-reduction intervention or the health-promotion intervention. This process ensured that there were no significant differences (P>.05) between facilitators in the interventions according to age, gender, or ethnicity. All facilitators received 2½ days of training designed to provide information and skills related to their specific intervention, to encourage and ensure implementation fidelity, and to generate high motivation and enthusiasm among all facilitators irrespective of their assigned intervention.
QUALITY ASSURANCE
We took several measures to ensure the fidelity of intervention implementation. Project staff unobtrusively monitored facilitators and gave them cues to ensure fidelity to the time allotted for each activity. Facilitators completed a debriefing questionnaire to assess issues with implementation and their degree of fidelity to activities as written in the curriculum. Facilitators in both interventions reported a high degree of fidelity, implementing all activities in each module 87.8% (36/41) of the time. There were no significant differences among facilitators in relation to the number of modules completed.
OUTCOME MEASURES
We used several self-report measures of sexual activity and condom use. Participants were asked if they ever had sexual intercourse (“your penis in a girl’s vagina” or “boy’s penis in your vagina”) and whether they had done so in the past 3 months (yes or no). Given the past 3 months as a reference point, adolescents also were asked the number of days in which they had intercourse, the number of times they had sex, the number of days of sex without using a condom, and the number of sexual partners. For condom use, adolescents indicated on a 5-point Likert scale how often they used a condom (1=never to 5=always). Binary variables were created for consistent condom use (always used a condom; 0=no; 1=yes), and number of partners (0=1 or no partner; 1=2 or more partners). We also calculated the proportion of days of protected sex (1–number of days of sex without a condom/number of days of sex). We previously reported the procedures for the Spanish translation and pilot testing of these measures.19
We used several measures that had been used previously to increase the validity of self-reported sexual behavior.20 First, we had trained project assistants, who were not involved in the delivery of the intervention, administer questionnaires. We stressed the confidentiality of participants’ responses and used only code numbers on questionnaires. To facilitate the recall of sexual behaviors, we used a relatively brief follow-up (eg, 3 months) and provided calendars to mark the 3-month intervals. To minimize overreporting or underreporting of sexual behaviors, we stressed the importance of providing honest responses. Participants also signed a survey agreement form in which they pledged to answer questions honestly. Finally, we included a standard measure of social desirability bias,21 which was used to examine statistically whether such bias could explain apparent intervention effects.
STATISTICAL ANALYSES
We conducted a series of χ2 tests, Poisson and negative binomial regression analyses, and independent sample t tests to identify significant differences between intervention groups in sociodemographic variables and preintervention measures of sexual behavior. In addition, we performed discrete time survival analysis22 to model the likelihood of attrition and identify baseline factors influencing the likelihood of attrition.
Hypotheses regarding the effects of the HIV intervention on sexual behavior and condom use outcomes were tested in generalized linear model analyses. The models included the following covariates: intervention group (HIV risk reduction or health promotion), time (3-, 6-, and 12-month follow-up), sexual experience (ie, ever had intercourse) at baseline, baseline values for outcome variables, language (English or Spanish), and gender. Baseline values were not used as covariates for hypotheses regarding condom use because of the small number of participants who reported sexual intercourse at baseline.
In all analyses, generalized estimation equation methodology23 was used to fit the generalized linear models to the type of longitudinal outcome data (continuous, count, or categorical measures). This method accounts for the likely correlations of repeated outcome measures for each participant. To determine potential moderators of intervention effects, we tested interactions between intervention and covariates hierarchically in the generalized linear models. Analyses were conducted by using an intention-to-treat approach in which participants were analyzed in their original randomized groups regardless of the number of intervention sessions they attended.
RESULTS
PREINTERVENTION COMPARABILITY OF CONDITIONS
There were no significant differences between adolescent intervention groups at baseline in gender, language use, or age. As seen in the Table, there were no significant differences in sexual behavior outcomes between the HIV risk-reduction group and the health-promotion group.
Table.
Self-Reported Sexual Behavior According to Intervention Group at Baseline*
| Sexual Behavior | Intervention Group |
|
|---|---|---|
| HIV Risk Reduction, % (n = 263) |
Health Promotion, % (n = 287) |
|
| Ever had sex | 40.9 | 44.7 |
| Sexual intercourse in the past 3 mo | 26.0 | 29.0 |
| Mean (SD) proportion of days of protected intercourse† |
0.67 (0.41) | 0.68 (0.39) |
| Multiple partners (≥2) | 21.0 | 15.6 |
| Consistent condom use† | 46.8 | 34.8 |
| Condom use at last intercourse† | 58.0 | 50.4 |
Abbreviation: HIV, human immunodeficiency virus.
For all values, P >.10. The P values for percentages are from χ2 tests; all others are from t tests. Combined sample numbers vary because of missing data for baseline sexual experience.
For the participants who were sexually active at baseline, 106 were in the HIV risk-reduction group and 127 were in the health-promotion group.
ATTRITION
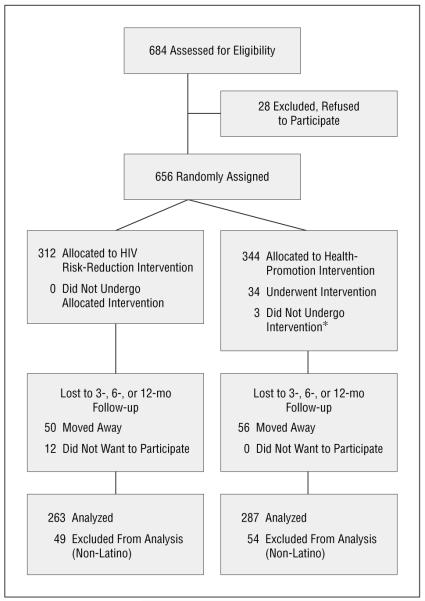
As shown in Figure 1, there was little attrition. Discrete time survival analyses22 indicated there were no significant differences in attrition between the interventions. Among age, gender, primary language, and baseline sexual activity, the only significant predictor of attrition was primary language. English speakers were 90% more likely to attend a follow-up session than Spanish speakers (odds ratio [OR] = 1.91; 95% confidence interval [CI],1.30-2.78).
Figure 1.
Progress of participants through the trial. Asterisk indicates reason unknown; HIV, human immunodeficiency virus.
EFFECTS OF THE HIV RISK-REDUCTION INTERVENTION ON SEXUAL BEHAVIOR
The intervention had significant effects on sexual intercourse and multiple partners in the past 3 months. In Figures 2, 3, and 4, we provide a graphic representation of intervention results by showing the unadjusted means in each intervention group across time. Results of generalized estimation equation analyses indicate that adolescents in the HIV risk-reduction group were less likely to report having had sexual intercourse in the past 3 months during follow-up (OR, 0.66; 95% CI, 0.46-0.96) than were those in the health-promotion intervention. Similarly, adolescents in the HIV risk-reduction intervention were less likely to report having multiple partners across follow-up compared with adolescents in the health-promotion intervention (OR, 0.53; 95% CI, 0.31-0.90).
Figure 2.
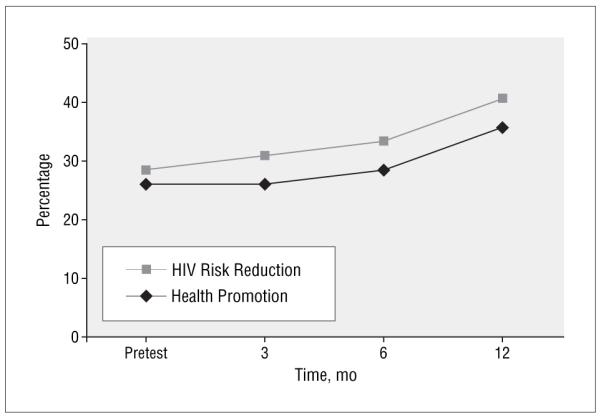
Self-report of sexual intercourse in the past 3 months. This graph does not represent results of generalized estimation equation analyses. The percentage (SE) was calculated for the outcome variable; unadjusted scores are presented for each time period. Values for the human immunodeficiency virus (HIV) risk-reduction group are as follows: pretest, 25.9% (0.44%); 3 mo, 26.0% (0.44%); 6 mo, 28.4% (0.45%); and 12 mo, 35.7% (0.48%). Values for the health-promotion group are as follows: pretest, 28.4% (0.45%); 3 mo, 31.0% (0.46%); 6 mo, 33.3% (0.47%); and 12 mo, 40.7% (0.49%).
Figure 3.
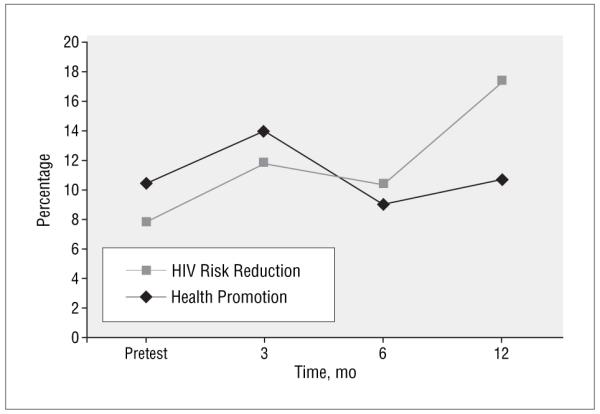
Self-report of multiple partners in the past 3 months. This graph does not represent results of generalized estimation equation analyses. The percentage (SE) was calculated for the outcome variable; unadjusted scores are presented for each time period. Values for the human immunodeficiency virus (HIV) risk-reduction group are as follows: pretest, 10.4% (0.31%); 3 mo, 14.0% (0.35%); 6 mo, 9.0% (0.29%); and 12 mo, 10.7% (0.31%). Values for the health-promotion group are as follows: pretest, 7.8% (0.27%); 3 mo, 11.7% (.0.32%); 6 mo, 10.3% (0.30%); and 12 mo, 17.3% (0.38%).
Figure 4.
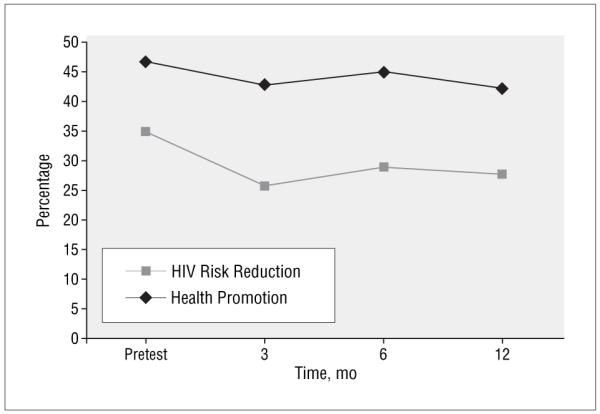
Consistent condom use in the past 3 months. This graph does not represent results of generalized estimation equation analyses. The percentage (SE) was calculated for the outcome variable; unadjusted scores are presented for each time period. Scores were calculated only for participants who were sexually active at baseline (human immunodeficiency virus [HIV] risk-reduction group [n = 106], health-promotion group [n = 127]). Values for the HIV risk-reduction group are as follows: pretest, 46.8% (0.50%); 3 mo, 42.6% (0.50%); 6 mo, 44.8% (0.50%); and 12 mo, 42.2% (0.50%). Values for the health-promotion group are as follows: pretest, 34.8% (0.48%); 3 mo, 25.7% (0.44%); 6 mo, 28.8% (0.46%); and 12 mo, 27.6% (0.45%).
The intervention also had significant effects related to consistent condom use and frequency of unprotected sex. Adolescents in the HIV risk-reduction group were more likely to report using condoms consistently (OR, 1.91; 95% CI, 1.24-2.93) and less likely to report days of unprotected sex (relative risk, 0.47; 95% CI, 0.26-0.84) than were adolescents in the health-promotion intervention. There were no significant effects for the outcomes of condom use at last sex (OR, 1.45; 95% CI, 0.97-2.15) and proportion of days of protected sex (B, 0.02; 95% CI, −0.07 to 0.12).
MODERATORS OF THE INTERVENTION
Gender and social desirability did not moderate effects of the intervention. Sexual experience and primary language, however, had significant interactions with the intervention on selected outcomes. Additional analyses revealed that among adolescents who were sexually inexperienced at baseline, those assigned to the HIV risk-reduction intervention were more likely to have fewer days of unprotected sex compared with adolescents in the health-promotion intervention (relative risk, 0.22; 95% CI, 0.08-0.63). In relation to primary language, among Spanish speakers, the odds of having used a condom at last sexual intercourse were nearly 5 times higher for adolescents in the HIV risk-reduction intervention than in the health-promotion intervention (OR, 4.73; 95% CI, 1.72-12.97). There were no significant differences between intervention groups among English speakers (OR, 1.11; 95% CI, 0.72-1.71). Similarly, Spanish speakers in the HIV risk-reduction group had a higher proportion of protected sex than did Spanish speakers who participated in the health-promotion control intervention (mean difference,0.35; P<.01). Conversely, there were no significant differences between intervention groups among English speakers (mean difference, −0.03; P>.5).
COMMENT
Results of this randomized controlled trial provide evidence of the efficacy of a culture- and theory-based intervention on HIV sexual risk behavior. Specifically, participation in the HIV risk-reduction intervention resulted in fewer reports of sexual intercourse and number of sexual partners compared with participation in the health-promotion control intervention. In addition, the HIV risk-reduction intervention caused an increase in consistent condom use and frequency of condom use compared with the control intervention.
Results of this study are important for several reasons. First, to our knowledge, this study is the first randomized controlled trial of an HIV risk-reduction curriculum developed specifically for Latino adolescents to demonstrate long-term (12-month) effects on frequency of sexual intercourse and condom use. Other intervention studies that have included Latino adolescents either have been ineffective or have examined only short-term effects.7-9,11
Second, to our knowledge, this study is the first randomized controlled trial to demonstrate efficacy with Spanish-speaking Latino adolescents. The intervention used in this study was tailored to Latino culture, and we found that it had greater effects among Spanish-speaking adolescents on several outcomes. Specifically, Spanish speakers who participated in the HIV risk-reduction intervention had a higher proportion of days of protected sex and more frequent condom use at last sexual intercourse. To our knowledge, this is the first randomized controlled trial to demonstrate greater efficacy of a culturally tailored HIV risk-reduction intervention among people who speak the language of the culture for which it was tailored.
Third, results of this study demonstrate the efficacy of a safer sex intervention in decreasing sexual intercourse and increasing condom use. In addition, Latino adolescents who were sexually inexperienced before the intervention and who were assigned to the HIV risk-reduction intervention reported fewer days of unprotected sex in the past 3 months than did adolescents in the control group. Results of this study demonstrate that addressing abstinence and condom use within a curriculum can affect both behaviors. In addition, the increased efficacy of the intervention on some outcomes for Latino adolescents who were Spanish-language dominant and sexually inexperienced provides support for tailoring intervention approaches. Furthermore, additional strategies may be needed for English-dominant Latino adolescents, as well as those who are sexually experienced, to enhance the efficacy of the intervention with these groups.
Finally, results of this study support the growing body of research that indicates that interventions based on behavioral theories and tailored to the culture of adolescents are effective.24-26 The HIV risk-reduction curriculum used in this study was based on an existing curriculum15 and integrated culturally relevant concepts and approaches.19
Results of this study should be considered in light of several limitations. First, most participants were of Puerto Rican descent, attending school, and living in northeast Philadelphia, and they were self-selected. Further research is needed to determine the extent to which findings are generalizable to other Latino adolescents. Second, the outcome measures used in this study were based on self-report. We did, however, include several procedures to increase the validity of self-reports. Furthermore, our measure of social desirability21 did not interact with intervention results to affect self-reported outcomes, suggesting that adolescents’ responses were not motivated by the desire to please others.
Despite these limitations, this study is an important contribution in assisting Latino adolescents to decrease HIV sexual risk behavior. It is an important effort in providing practitioners an evidence base from which to guide and support adolescents in sexual decision making. Much more research is needed with Latino adolescents to address the health disparity in HIV and AIDS.
Announcement.
Submissions. The Editors welcome contributions to Picture of the Month. Submissions should describe common problems presenting uncommonly, rather than total zebras. Cases should be of interest to practicing pediatricians, highlighting problems that they are likely to at least occasionally encounter in the office or hospital setting. High-quality clinical images (in either 35-mm slide or electronic format) along with parent or patient permission to use these images must accompany the submission. The entire discussion should comprise no more than 750 words. Articles and photographs accepted for publication will bear the contributor’s name. There is no charge for reproduction and printing of color illustrations. For details regarding electronic submission, please see: http://archpedi.ama-assn.org.
Acknowledgment
The authors gratefully acknowledge the support and contributions of staff, facilitators, project assistants, adolescents, and community members in the development and implementation of this project. In particular, we acknowledge the contributions of Margarita Bleier, MSW, Project Director, and Monique Howard, MS, PhD(c), HIV Curriculum Specialist. The authors also would like to acknowledge the contributions of Brady West, MA, BS, for his statistical consultation regarding the manuscript and Brenda L. Eakin, MS, in the preparation and editing of this article.
Funding/Support: The project described was supported by grant NR04855 from the National Institute of Nursing Research (Dr Villarruel). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health.
Footnotes
Author Contributions: Dr Villarruel had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Villarruel, J. B. Jemmott, and L. S. Jemmott. Acquisition of data: Villarruel and L. S. Jemmott. Analysis and interpretation of data: Villarruel and J. B. Jemmott. Drafting of the manuscript: Villarruel. Critical revision of the manuscript for important intellectual content: Villarruel, J. B. Jemmott, and L. S. Jemmott. Statistical analysis: Villarruel and J. B. Jemmott. Obtained funding: Villarruel, J. B. Jemmott, and L. S. Jemmott. Administrative, technical, and material support: Villarruel and L. S. Jemmott. Study supervision: Villarruel.
Financial Disclosure: None reported.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) Diagnosis of HIV/AIDS—32 states, 2000-2003. MMWR Morb Mortal Wkly Rep. 2004;53:1106–1110. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. National Center for HIV, STD and TB Prevention, Divisions of HIV/AIDS Prevention [Accessed February 10, 2005];HIV/AIDS among Hispanics. http://www.cdc.gov/hiv/pubs/facts/hispanic.htm.
- 3.Rosenberg PS, Biggar RJ. Trends in HIV incidence among young adults in the United States. JAMA. 1998;279:1894–1899. doi: 10.1001/jama.279.23.1894. [DOI] [PubMed] [Google Scholar]
- 4.Grunbaum JA, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2003. MMWR Surveill Summ. 2004;53:1–96. published corrections appear in MMWR Morb Mortal Wkly Rep. 2004;53:536; MMWR Morb Mortal Wkly Rep. 2005;54:608. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Trends in sexual risk behaviors among high school students—United States, 1991-2001. MMWR Morb Mortal Wkly Rep. 2002;51:856–859. [PubMed] [Google Scholar]
- 6.Kann L, Kinchen SA, Williams BI, et al. Youth risk behavior surveillance—United States, 1999. MMWR CDC Surveill Summ. 2000;49:1–32. [PubMed] [Google Scholar]
- 7.Kirby DB, Baumler E, Coyle KK, et al. The “Safer Choices” intervention: its impact on the sexual behaviors of different subgroups of high school students. J Adolesc Health. 2004;35:442–452. doi: 10.1016/j.jadohealth.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy MG, Mizuno Y, Hoffman R, et al. The effect of tailoring a model HIV prevention program for local adolescent target audiences. AIDS Educ Prev. 2000;12:225–238. [PubMed] [Google Scholar]
- 9.Kirby D, Korpi M, Adivi C, Weissman J. An impact evaluation of project SNAPP: an AIDS and pregnancy prevention middle school program. AIDS Educ Prev. 1997;9(1 suppl):44–61. [PubMed] [Google Scholar]
- 10.Koniak-Griffin D, Lesser J, Nyamathi A, et al. Project CHARM: an HIV prevention program for adolescent mothers. Fam Community Health. 2003;26:94–107. doi: 10.1097/00003727-200304000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Sellers DE, McGraw SA, McKinlay J. Does the promotion and distribution of condoms increase teen sexual activity? evidence from an HIV prevention program for Latino youth. Am J Public Health. 1994;84:1952–1959. doi: 10.2105/ajph.84.12.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flores G, Fuentes-Afflick E, Barbot O, et al. The health of Latino children: urgent priorities, unanswered questions, and a research agenda. JAMA. 2002;288:82–90. doi: 10.1001/jama.288.1.82. [DOI] [PubMed] [Google Scholar]
- 13.National Institutes of Health (NIH) NIH Consensus Development Statement-Interventions to Prevent HIV Risk Behaviors. NIH; Bethesda, Md: 1997. [PubMed] [Google Scholar]
- 14.Villarruel AM, Jemmott LS, Jemmott JB., III Designing a culturally based intervention to reduce HIV sexual risk for Latino adolescents. J Assoc Nurses AIDS Care. 2005;16:23–31. doi: 10.1016/j.jana.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Jemmott LS, Jemmott JB, III, McCaffree K. Be Proud! Be Responsible! Strategies to Empower Youth to Reduce Their Risk for AIDS. Select Media Publications; New York, NY: 1995. [Google Scholar]
- 16.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 17.Ajzen I, Madden T. Prediction of goal-directed behavior: attitudes, intentions, and perceived behavioral control. J Exp Soc Psychol. 1986;22:453–474. [Google Scholar]
- 18.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 19.Villarruel AM, Jemmott JB, III, Jemmott LS, Ronis DL. Predictors of sexual intercourse and condom use intentions among Spanish-dominant Latino youth: a test of the planned behavior theory. Nurs Res. 2004;53:172–181. doi: 10.1097/00006199-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Jemmott JB, III, Jemmott LS, Fong GT. A randomized controlled trial of abstinence and safer sex HIV risk-reduction interventions for young African American adolescents. JAMA. 1998;279:1529–1536. doi: 10.1001/jama.279.19.1529. [DOI] [PubMed] [Google Scholar]
- 21.Crowne D, Marlowe D. The Approval Motive. John Wiley & Sons; New York, NY: 1964. [Google Scholar]
- 22.Allison P. Survival Analysis Using the SAS System: A Practical Guide. SAS Institute Inc; Cary, NC: 1995. [Google Scholar]
- 23.Diggle PJ, Heagerty P, Liang KY, Zeger SL. The Analysis of Longitudinal Data. 2nd ed. Oxford University Press; Oxford, England: 2002. [Google Scholar]
- 24.Jemmott JB, III, Jones JM. Social psychology and AIDS among ethnic minority individuals: risk behaviors and strategies for changing them. In: Pryor J, Reeder G, editors. Social Psychology of HIV Infection. Lawrence Erlbaum Associates; Hillsdale, NJ: 1993. pp. 183–224. [Google Scholar]
- 25.Marín BV. Analysis of AIDS Prevention Among African Americans and Latinos in the United States. Office of Technology Assessment; Washington, DC: 1995. [Google Scholar]
- 26.Wingood GM, DiClemente RJ. HIV sexual risk reduction for women: a review. Am J Prev Med. 1996;12:209–217. [PubMed] [Google Scholar]