Abstract
Age-Related Macular Degeneration (AMD) is the leading cause of severe vision loss in older adults and impairs the ability to read, drive, and live independently and increases the risk for depression, falls, and earlier mortality. Although new medical treatments have improved AMD’s prognosis, vision-related disability remains a major public health problem. Improving Function in AMD (IF-AMD) is a two-group randomized, parallel design, controlled clinical trial that compares the efficacy of Problem-Solving Therapy (PST) with Supportive Therapy (ST) (an attention control treatment) to improve vision function in 240 patients with AMD. PST and ST therapists deliver 6 one-hour respective treatment sessions to subjects in their homes over 2 months. Outcomes are assessed masked to treatment assignment at 3 months (main trial endpoint) and 6 months (maintenance effects). The primary outcome is targeted vision function (TVF), which refers to specific vision-dependent functional goals that subjects highly value but find difficult to achieve. TVF is an innovative outcome measure in that it is targeted and tailored to individual subjects yet is measured in a standardized way. This paper describes the research methods, theoretical and clinical aspects of the study treatments, and the measures used to evaluate functional and psychiatric outcomes in this population.
Keywords: Vision Function, Age-Related Macular Degeneration, Clinical Trial, Depression
Introduction
Age-Related Macular Degeneration (AMD) is the leading cause of severe vision loss in older adults, with almost 2 million persons in the United States having advanced disease and over 7 million having early signs. [1] Aging of the population will double these numbers by 2020, dramatically increasing the prevalence of older adults who have lost the ability to read, drive, and live independently and who are at risk for depression, falls, and institutionalization. [2–7] Although the anti-vascular endothelial growth factor (anti-VEGF) antibodies ranibizumab and bevacizumab have greatly improved the prognosis of neovascular or “wet” AMD (there are no effective treatments for atrophic or “dry” AMD although certain vitamin preparations slow disease progression), many patients continue to have disabling vision impairment. [8,9] Thus, AMD-related disability remains a major public health problem.
To address that problem, we designed a study entitled, “Improving Function in AMD” (IF-AMD), which is a randomized, controlled clinical trial that compares the efficacy of Problem-Solving Therapy (PST) with Supportive Therapy (ST) to improve vision function in patients with AMD. The study recruits 240 subjects: 120 will be randomized to receive 6 one-hour, in-home PST sessions, and 120 will be randomized to a control group who will receive ST in an identical treatment format. PST is a psychological treatment that teaches patients to identify problems, generate alternative solutions, select the best solution, develop and conduct a plan, and evaluate whether the plan solves the problem. ST is a structured, standardized, psychological treatment that controls for the nonspecific effects of attention. The primary aims of the IF-AMD trial are to test the immediate (3-months) and longer term (6-months) efficacy of PST to improve the primary outcome of vision function.
Vision function refers to vision-related abilities to perform daily living activities (e.g. reading recipes to prepare meals). Our approach to measuring vision function combines both innovative (i.e., Targeted Vision Function) and widely used standard measures (i.e., National Eye Institute Vision Function Questionnaire (NEI VFQ). [9] Targeted vision function (TVF) refers to specific vision-dependent functional goals that subjects highly value but find difficult to achieve. As an outcome measure TVF is innovative and novel, as it recognizes that different people have unique vision function goals. In this way, TVF is targeted and tailored yet measured in a standardized way in all subjects.
The secondary outcomes of the IF-AMD trial are general- and vision-specific quality of life. Quality of life ratings add unique information over and above functional ability assessments and increase our ability to detect broader treatment effects. We also plan to assess PST’s specificity by measuring subjects’ coping strategies, pre- and post-intervention, to determine whether increasing healthy coping strategies mediates PST’s effect on vision function over and above the nonspecific effects of attention. We also plan an exploratory aim to examine whether improvement in vision function is moderated by baseline depression status and type of AMD (wet or dry) given that previous research suggests that these characteristics may differentially affect treatment outcomes.
Study Design
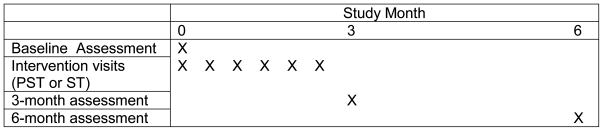
This trial recruits 240 patients with AMD from the retina clinics associated with the Wills Eye Institute (WEI) in Philadelphia, PA and randomizes subjects to PST or ST in a 1:1 allocation ratio. Randomization is stratified based on severity of AMD (visual acuity better vs. worse than 20/100 in the better eye) as treatment response may vary by severity of vision loss. A random numbers table and serially numbered, sealed, opaque envelopes containing the treatment allocations are used to assign subjects to the treatment groups within each stratum. The randomization schedule is based on a permuted random block design to ensure balance between treatment groups on time of subject enrollment. When patients register for their retina clinic visits they have the opportunity to provide written permission to be contacted for possible participation in clinical research. Each week a research assistant reviews the clinical records of patients who provided permission to identify those who met eligibility criteria. We then confirm the AMD diagnosis with each patient’s ophthalmologist, obtain his/her permission to contact the patient, and mail introductory letters to patients signed by the ophthalmologist. We then telephone patients one week later to explain the study, confirm their willingness and eligibility to participate, and schedule an in-home visit within 2 weeks to obtain written informed consent and conduct the baseline assessment. This method of case ascertainment is objective and verifiable, and although subjects self-select for study participation, recruitment avoids relying on ophthalmologists to identify eligible cases and minimizes other selection biases or missed cases. During the informed consent process we state that the study’s purpose is to compare the efficacy of PST and ST, and that both interventions may improve a person’s ability to function with macular degeneration. We indicate that PST emphasizes problem solving skills and that ST emphasizes support and attention to the problems that vision loss causes. We furthermore state that neither PST nor ST will improve vision. Jefferson’s Institutional Review Board approved this approach to contacting and consenting patients for research participation. Following randomization, trained PST and ST therapists deliver 6 one-hour treatment sessions, respectively, to subjects in their homes over 2 months. Outcome assessments masked to treatment assignment occur at 3 and 6 months post-randomization. Figure 1 depicts the schedule of study activities.
Figure 1.
Schedule of Study Activities
The study inclusion criteria are: 1) age 65 years or older; 2) bilateral AMD (neovascular and/or dry); 3) visual acuity between 20/70 and 20/400 [inclusive; (best corrected)] in the better-seeing eye, and no lower acuity limit in the fellow eye; and 4) moderate difficulty in at least one valued vision-function goal. The exclusion criteria are: 1) presence of uncontrolled glaucoma, diabetic retinopathy, or planned cataract surgery within 6 months; 2) cognitive impairment on an abbreviated version of the Mini-Mental Status Examination (MMblind) that omits vision-dependent items [10]; 3) presence of life-threatening illness; and 4) residence in a skilled nursing facility.
We chose patients with bilateral disease of this severity because they are more disabled than patients with unilateral AMD or those with less severe vision loss. This is a conservative criterion given West et al’s data showing that binocular visual acuity worse than 20/40 adversely affects vision function and impairs reading in 90% of individuals. [11] We exclude cognitively impaired patients because their cognitive deficits preclude learning new problem-solving skills. Taken together, these eligibility criteria generate a sample of patients with AMD who are at high risk for disability, who are likely to benefit from PST, and who are easily recognizable in clinical practice.
Conceptual Model
The theoretical basis for the IF-AMD Trial is the Disablement Process Model. [12] This is a sociomedical model of disability which describes how medical diseases affect functioning in specific body systems and can lead to disability. Verbrugge et al incorporated psychosocial factors in the model which led to their inclusion in the most recent World Health Organization’s (WHO) International Classification of Functioning, Disability and Health. [13] The WHO model describes function and disability as part of a “complex relationship between health conditions and contextual (i.e. environmental and personal) factors” and explains how two patients with the same disease, of equal severity, can function quite differently from one another. [14]
PST acts on the disablement process model to improve targeted vision function in 3 ways. First, it may reduce the visual demands of a task by helping patients to devise compensatory approaches. Second, PST may reduce depressive symptoms, thereby interrupting the downward spiral of increasingly worsening function and depression that can occur. Third, PST encourages behavioral activation, maintains social engagement, and may result in greater use of low vision devices and services, which may further reduce task difficulty.
Study Treatments
1. Problem-Solving Therapy (PST)
PST is a brief, psychological treatment that teaches problem-solving skills for a variety of conditions (e.g., depression, osteoarthritis, chronic pain, obesity). [15–21] We previously demonstrated the efficacy of PST as a short-term treatment to prevent depression in patients with AMD. [22] Its use in AMD recognizes that vision loss is disabling and that enhancing problem-solving skills may reduce disability. PST also helps patients to recognize the realistic limitations of their visual abilities and to find alternative approaches so that valued activities can still be performed (e.g. using public transportation as an alternative to driving, enabling a patient to continue to travel independently). Thus, PST attempts to reduce task difficulty of valued activities by teaching commonsense, problem-solving skills in a structured way.
The PST therapist and subject begin the treatment process by discussing the subject’s difficulties with specific tasks (e.g., writing checks) that underlie a vision-dependent activity (e.g., managing personal finances). Then, the therapist teaches the problem-solving steps to help the subject devise new ways to reduce task difficulty. The 7 steps are:
clarifying the problems associated with the task
establishing a realistic goal toward improvement of task performance
generating multiple solution alternatives
implementing decision-making guidelines
choosing the preferred solution(s)
implementing the preferred solutions(s) and
evaluating the outcome
The PST therapist discusses the Target Vision Function activities that a subject identified at baseline. The subject selects one vision function activity to address first, and then identifies the problems with performing the tasks that make it difficult to achieve. The goal must be one that can be realistically achieved between sessions and that the subject can exert some control over. This involves breaking down large problems into more manageable parts or reframing the problem so that feasible solutions can be generated. For example, if the activity is meal preparation, the problematic tasks may be measuring ingredients and using the stove. The PST therapist guides the subject through the problem-solving steps to devise compensatory strategies to improve performance of these tasks. In this context, the PST therapist may review a list (printed in large font) of potentially helpful rehabilitative services and devices. Subjects may refer to the list when brainstorming possible solutions to their problems.
A key modification to the brainstorming step of PST was the integration of the Person, Environment, Occupation Model (PEO) of occupational therapy. [23] In the PEO model the term “occupation” refers to “valued activities.” The PEO model suggests three potentially complementary courses of action in response to impaired function. When faced with a participation restriction the individual can: (1) change something about their personal skills and capabilities, (2) change the environment in which the activity is performed, or (3) change the nature of the activity itself. The therapist encourages the subject to think in terms of these themes when generating solutions. However, the PST therapist does not give direct advice; instead the therapist asks subjects to use problem-solving skills to find ways to obtain and/or implement a service or device. Once one activity has been addressed, the subject then addresses additional activities. The number of activities that are ultimately addressed will depend on the subject, his/her success or difficulty implementing solutions, and the complexity of the problem. The aim is to have subjects incorporate the problem-solving method of reasoning as a routine, often recruited approach to solving future as well as current function-related problems.
2. Supportive Therapy (ST)
We are testing PST’s efficacy by comparing it to ST, which is a similarly structured, standardized, control psychological treatment that controls for nonspecific treatment effects. [24–26] ST resembles PST in all ways but for PST’s problem-solving skills training. Both are fully manualized, similar in dose and intensity of attention (i.e. number and duration of sessions), equally credible, and delivered by therapists trained in both treatments to minimize therapist effects. ST is nondirective, supportive, and facilitates personal expression and conveys empathy, respect, and optimism (i.e. a general sense that things can get better). The ST therapist informs a subject that ST’s purpose is to explore the impact of vision loss on his or her life. The goals are to facilitate and deepen knowledge about the subject’s life situation and its relationship to growing older and all of the issues associated with that such as illness, disability, retirement, social isolation and, particularly, vision loss. This portion of therapy is presented as an exploration process that might be helpful for increasing self-confidence. Therapists create an accepting, non-judgmental, empathic environment, by using supportive statements, reflective listening, and empathic communications. In contrast to PST sessions, there is no discussion of vision function goals, problem solving, or low vision rehabilitative strategies. Unlike PST, ST contains no active elements beyond its nonspecific components, has no long-lasting treatment effects, and no theoretical basis to support an effect on vision function. In this way ST is a sham or control treatment. Although ST reduces distress for the time that treatment is delivered, its effects are thought to be transient and not associated with meaningful functional improvement.
Sample Size Calculation
We based the sample size calculation on the following parameters: one primary outcome (i.e., Targeted Vision Function); and treatment effect sizes (ES) observed in other trials of PST and ST. A recent meta-analysis of PST reported ESs ranging from .34 to .83; on this basis we powered the study to detect a medium ES of 0.40. [15] To attain 80% power for a 2-sided alternative hypothesis using a F-test to compare the 2 treatment groups at 3 months, we required 200 subjects (100 per group) to detect an effect size of .4. We over-sampled by 20% to account for attrition, bringing the total sample size to 240.
Masking
Psychotherapy trials differ from most other clinical trials in medicine in that double-blind administration of treatments is impossible: therapists are aware of what treatment they deliver as are the subjects. Recognizing this, procedures have been developed to ensure structural equivalence of treatments and to assess and maintain treatment fidelity and differentiability. A research nurse who is masked to treatment assignment obtains all outcome data during in-home interviews. The nurse instructs subjects to reveal nothing about the treatments they may have received. Despite careful precaution, breaches in masking occur that may introduce treatment-related biases. [27, 28] We require that central data collection, measurement, and data entry procedures are made by persons masked to treatment assignment; only the project director, statistician, and therapists are aware of treatment assignment. Prior to all outcome assessments, the purpose and importance of masked treatment assignment are discussed with subjects.
Fidelity, Supervision, and Adherence
The therapists for this study are trained to deliver both PST and ST. Having each therapist deliver both forms of treatment (rather than having separate therapists for each treatment) reduces variance due to therapist effects. In this regard, it is critically important to have both therapists closely follow the PST and ST treatment manuals. To maintain their objectivity, we did not inform them of the study hypotheses or the nature of the outcome measures.
Both PST and ST are manual driven treatments; thus training concentrates on properly adhering to the principles and activities outlined in the manual. The training program consists of workshops, review and discussion of the relevant treatment manuals, and supervision of 5 training cases. Therapists must meet satisfactory levels of competence before starting the treatment trial. All treatment sessions are audio-taped during the study and 30% of subjects are randomly selected for treatment fidelity ratings to control for treatment “drift.” To assess subjects’ adherence to PST, the therapists rate whether PST subjects understand and apply PST principles; whether subjects comply with homework; and whether requisite problem-solving tasks are accomplished.
Primary Outcome Measure
1. Vision Function
There is no single, universally accepted measure or methodology to measure vision function. Although instruments such as the National Eye Institute Vision Function Questionnaire (NEI-VFQ), the Activities Inventory (AI), and the Veterans Affairs Low Vision Visual Functioning Questionnaire (VA LV VFQ-48) measure multiple aspects of vision function, few studies have evaluated their sensitivity to psychosocial interventions. [9, 29–31] Because these instruments measure several diverse dimensions of vision loss (i.e., the NEI-VFQ assesses difficulty with daily activities, social functioning, general health and vision, and quality of life), they may be unable to detect specific intervention effects. This may be especially true when the most important outcome is an improvement in a personally valued goal. Improvement on just one goal may enhance life quality tremendously but may not be reflected as a statistically significant change on a multi-dimensional rating scale. Furthermore, because vision goals and vision deficits vary from person to person, change in total scale scores may be less informative than change in a more targeted outcome.
To address this issue, we are using a targeted outcome measurement approach, which employs a standardized method to identify and quantify specific problems for outcome assessment. [30] A number of studies have demonstrated this approach’s reliability, validity and practicality, showing that it can be more sensitive to treatment effects than multi-dimensional, multi-symptom measures. [32–34] Using such an approach, we devised a measure, Targeted Vision Function (TVF), to serve as the primary outcome of the IF-AMD trial. As an outcome measure, TVF pinpoints and evaluates change in the vision-function goals that subjects consider most important and has the face validity, clinical relevance and flexibility to convey meaningful change in response to rehabilitative interventions. To derive the TVF measure, at the baseline assessment, prior to randomization, subjects complete the Activities Inventory and identify up to 4 vision function goals that they highly value ( rated as “important” or “very important”) but find difficult to achieve. They then rate the difficulty of each goal on a scale from 0 to 4 (not difficult, to impossible). The average TVF score is the sum of the difficulty ratings of the (up to) 4 goals divided by the number of goals (from 1 to 4). Higher average scores indicate greater disability. At each outcome assessment (efficacy at 3 months; long-term benefit at 6 months), subjects again rate the difficulty of the same targeted goals and the average TVF score is calculated. For example, at baseline a subject may rate the goal of cooking as moderately difficult (score = 2) and rates paying bills as very difficult (score = 3). The subject’s average TVF score at baseline is then = 2.5. At 3 months, PST may have reduced the difficulty of both goals by one level (2 to 1 for cooking, and 3 to 2 for paying bills) such that the average TVF score is 1.5. Thus, possible average TVF scores at 3 months can range from 0 (no difficulty on any goal) to 4 (severe difficulty on 4 goals). While this may seem like a narrow range, actual scores are likely to be decimals, such that the variability of scores is considerably larger.
At the study endpoints, the mean differences from baseline in the average TVF scores in the two treatment groups are compared after adjusting for baseline scores. This approach allows that subjects may vary in the number of TVF goals they selected at baseline. The primary treatment hypothesis is that PST-subjects will report less difficulty with TVF goals at 3 months compared to ST-controls; this will be reflected in lower average TVF scores in between-group and within-group comparisons.
Secondary Outcome Measures
1. Activities Inventory (AI)
The AI is a structured vision function questionnaire that asks patients to rate the value and difficulty of 48 vision function goals (e.g., daily meal preparation) and the tasks (e.g., seeing stove settings) that are required to achieve them. [30,31] The goals are nested under 3 main Objectives (e.g., Independent Daily Living, Social Interactions, and Recreation). If a goal is important (range not important “0” to very important “4”), the subject rates its “difficulty” [on a scale of 0 (not difficult) to 4 (impossible)]. The AI provides the standardized method necessary to identify the TVF goals described above in clear, specific, and operational terms, and guides subjects through a process of inquiries to identify their goals. This works especially well in AMD because the universe of possible vision function goals, although theoretically unlimited, in practice is finite and definable using the AI. Also, the AI’s extensive development and validation in large populations of older visually impaired people avoids the possibility that subjects may define a problem that cannot be addressed in treatment.
2. NEI VFQ-25 plus Supplement
The NEI VFQ-25 consists of 25 items and a supplement of 14 additional items, derived from the original 52-item NEI VFQ. [9] This instrument measures both self-reported vision function and vision-related quality of life (QoL). Of the 39 items, 6 ask patients to grade their general health and vision, 20 rate difficulties with activities, and 13 assess the severity of problems associated with vision loss (and include the QoL questions). The items on activity difficulties are rated from 1 to 6, with responses indicating increasing levels of difficulty. The QoL questions assess vision-specific social functioning, vision-specific mental health, vision-specific role difficulties, and dependency due to vision. The instrument creates 11 subscale scores and an overall score. The NEI VFQ-25 can be accessed at http://www.rand.org/health/surveys_tools/vfq/.
3. Quality of Life (QoL)
We will investigate whether PST influences quality of life using the vision-related quality of life (QoL) items of the NEI-VFQ-25 plus Supplement. [9] A number of research reports indicate that disease-specific measures perform better than generic measures of QoL. For example, Scott et al showed that vision-targeted questionnaires better demonstrate associations between vision and QoL and are more sensitive than general health-related QoL questionnaires to score changes in response to low vision services. [35] Nevertheless, we believe it is important to include a general QoL measure to compare our outcomes with other non-ophthalmologic patient populations. Thus, we will also measure general QoL at baseline and at months 3 and 6 using the 6-item Medical Outcome Study (MOS-6) survey, which assesses physical, role, social, and psychological functioning, as well as current health perceptions and physical pain. [36] Although we hypothesize that PST will improve vision-related QoL, we anticipate benefits in other areas of life as well.
Other Measures
Personal Characteristics
These include age, sex, race, marital status, living arrangements, education, and income.
Vision Status
We have devised a standardized battery of vision tests which we administer in subjects’ homes at baseline and months 3 and 6. This approach standardizes vision assessments by setting and examiner and includes the assessment of distance and near visual acuity, contrast sensitivity, and the size and location of central scotomas.
Physical Health Status
To assess physical status we obtain the Chronic Disease Score, which provides an objective measure of medical comorbidity based on a weighted sum of medications taken for chronic illness, and the Multilevel Assessment Inventory Health Conditions Check List, which lists specific acute and chronic conditions. [37, 38]
Depression
We will use the Patient Health Questionnaire-9, which is a diagnostic instrument that generates criteria-based diagnoses of depression and a continuous measure of depression severity. [39]
Behavior Activation for Depression Scale (BADS)
Subjects in both treatment groups complete the BAS at baseline and at months 3 and 6 to assess change in healthy versus unhealthy coping strategies. The BADS, which consists of 26 items rated on a 7-point scale, yields 4 subscale scores: 1) the Activation scale measures adherence to goal directed planned activities (e.g., following through on a plan to try audio books to circumvent reading difficulties); 2) Avoidance/Rumination assesses avoidance of negative states and the tendency to think about problems but not problem solve solutions (e.g., continual thinking about vision loss but unwillingness to try magnifiers); 3) Work/School Impairment refers to an unwillingness to fulfill necessary responsibilities and obligations (e.g., not paying bills because it is too difficult); and 4) Social Impairment measures social isolation (e.g., avoiding social situations because it is hard to see faces). [40] Together these subscales provide a quantifiable process measure to link treatment assignment to outcomes and increase our ability to detect specific treatment effects.
Data Analyses
The observations to be used for primary and secondary outcome measures take the form of ordinal rating scales or dichotomous indicator scores. The items to be scored in the TVF are subject-generated; the other instruments require that the same fixed set of items be rated by all subjects. Summary scores are generated for the instruments with fixed sets of items by rescaling averages of response rank scores across items in the set. These summary scores necessarily have a ceiling and a floor, which limit the sensitivity and interpretability of change scores to treatment effects. To correct for ceiling and floor effects, we will linearize rating scale summary scores using a logit transform. [41]
The TVF consists of activity goals drawn from the AI. The subject’s rating of goal importance serves as a filter to determine whether the goal will be included in the subject’s personal set. The subject’s rating of goal difficulty serves two functions: 1) it acts as a filter to determine which goals that pass the importance test will be included in the subject’s personal set and, 2) it provides an ordinal magnitude estimate of the latent variable that is the outcome measure. Each activity goal in the AI requires a minimum level of visual ability to be achieved with a criterion level of ease. The minimum required visual ability for each goal has been estimated from difficulty ratings by a large sample of the low vision population. [42, 43] Theoretically, the difficulty rating corresponds to the subject’s estimate of the magnitude of the difference between that subject’s visual ability and the visual ability required by the goal, i.e., functional reserve. A positive outcome means that PST increases functional reserve for one or more of the subject’s goals. Thus, we expect to see an increase in average functional reserve across goals if PST is effective. However, the intervals between difficulty response categories are not necessarily equal; therefore, we cannot simply use averages of the response rank scores. Based on Rasch analysis of AI goal difficulty ratings for a large sample of the low vision population, we have estimates of average functional reserve for each difficulty response category, which is a linear interval-scaled measure. [42, 43] We will transform individual TVF goal difficulty ratings to low vision population-based functional reserve values and average across each subject’s goals. The change in average functional reserve from baseline to post-treatment is the primary outcome measure.
To test the efficacy of PST to improve TVF functional reserve measures at 3 months, we will use an ANCOVA in which group differences (PST vs. ST) in 3-month average TVF scores will be examined, adjusting for baseline TVF measures. The stratification variable [visual acuity between 20/70 and 20/100 (inclusive) vs. worse than 20/100 in the better eye)] will also be a covariate, as will any demographic or clinical characteristics that are significantly different between the two study groups. We will also conduct subsidiary analyses that will examine treatment group effects on total AI measures and the NEI-VFQ vision function difficulty measures at 3 months estimated from Rasch analysis. 44] To evaluate the long-term effects of PST at 6-months, we will use the same strategy as above except that the dependent variable will be TVF, AI, or NEI VFQ measures, respectively at 6-months.
To determine PST’s impact on vision-related quality-of-life at 3 months, we will use a MANCOVA in which the dependent variables will be the following 4 NEI-VFQ logit-transformedsubscales assessed at 3 months: 1) vision-specific mental health; 2) vision-specific role functioning; 3) dependency due to vision loss; and 4) vision-specific social functioning. We will conduct a parallel analysis using total MOS scores to examine the impact on general quality of life. We will conduct parallel analyses using 6 month data. To determine whether the mechanism linking PST to improved TVF involves changes in coping strategies, we will use Baron and Kenny’s 3-step approach to test for mediation effects. [45]
Conclusion
Severe vision loss and disability are frequent consequences of AMD. Although anti-VEGF treatments can improve and/or stabilize vision, many patients continue to have high levels of disability and depression. [46] In fact, many patients experience vision loss, depression, and disability as a single syndrome, with each element amplifying and perpetuating the adverse effects of the others. Thus, a brief, easy to understand, behavioral intervention that improves vision function may also reduce the risk of depression.
To improve vision function, we are using PST, which teaches patients new skills to solve vision function problems and thereby to preserve their ability to pursue valued activities. AMD provides an ideal model to test the problem solving approach because it is common, affects men and women equally, is quantifiable in terms of severity, has no overlap of symptoms with depression (which confounds assessments of disability in osteoarthritis, stroke, and cancer) and produces disability within a short time period, making it an efficient disease model. If the trial is successful, its results may well generalize to other chronic, disabling disorders, especially those that impair vision (e.g. diabetic retinopathy, glaucoma). The clinical and public health significance of the IF-AMD trial are clear: the disability of AMD will become more prevalent, costly, and burdensome to patients, families, and ophthalmologists as the population ages. [2, 3] This makes devising and testing practical interventions to improve vision function a national priority.
Acknowledgments
This work was supported by NEI grant U01 EY 015839 and the Farber Institute for Neurosciences of Thomas Jefferson University.
Footnotes
Additional Contributions: The Wills Eye AMD Study Group provided assistance with recruitment of the sample and data collection. Members of this group include William E. Benson, MD, Gary C. Brown, MD, Jay L. Federman, MD, Mitchell S. Fineman, MD, David H. Fischer, MD, Sunir J. Garg, MD, Allen C. Ho, MD, Jason Hsu, MD, Richard S. Kaiser, MD, Alfred C. Lucier, MD, Joseph I. Maguire, MD, J. Arch McNamara, MD, Carl H. Park, MD, Carl D. Regillo, MD, Lov K. Sarin, MD, Arunan Sivalingam, MD, Marc J. Spirn, MD, and James F. Vander, MD.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Barry W. Rovner, Email: barry.rovner@jefferson.edu.
Robin J. Casten, Email: robin.casten@jefferson.edu.
Mark T. Hegel, Email: Mark.T.Hegel@Dartmouth.edu.
Robert W. Massof, Email: rmassof@lions.med.jhu.edu.
Benjamin E. Leiby, Email: bleiby@mail.jci.tju.edu.
William S. Tasman, Email: wst1@ureach.com.
Literature Cited
- 1.Fine SL, Berger JW, Maguire MG, et al. Age-related macular degeneration. N Eng J Med. 2000;342:483–492. doi: 10.1056/NEJM200002173420707. [DOI] [PubMed] [Google Scholar]
- 2.The Eye Diseases Prevalence Research Group. Prevalence of Age-Related Macular Degeneration in the United States. Arch Ophthalmol. 2004;122:564–572. doi: 10.1001/archopht.122.4.564. [DOI] [PubMed] [Google Scholar]
- 3.Rein DR, Wittenborn JS, Zhang X, Honeycutt AA, Lesesne SB, Saaddine J for the Vision Health Cost-Effectiveness Study Group. Forecasting Age-Related Macular Degeneration Through the Year 2050: The Potential Impact of New Treatments. Arch Ophthalmol. 2009;127:533–540. doi: 10.1001/archophthalmol.2009.58. [DOI] [PubMed] [Google Scholar]
- 4.Slakter JS, Stur M. Quality of life in patients with age-related macular degeneration: impact of the condition and benefits of treatment. Surv Ophthalmol. 2005;50:263–273. doi: 10.1016/j.survophthal.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 5.Szabo SM, Janssen PA, Khan K, Potter MJ, MD, Lord SR. Older Women with Age-Related Macular Degeneration Have a Greater Risk of Falls: A Physiological Profile Assessment Study. J Am Geriatr Soc. 2008;56:800–807. doi: 10.1111/j.1532-5415.2008.01666.x. [DOI] [PubMed] [Google Scholar]
- 6.Cruess A, Zlateva G, Xu X, Rochon S. Burden of illness of neovascular age- related macular degeneration in Canada. Can J Ophthalmal. 2007;42:836–843. doi: 10.3129/i07-153. [DOI] [PubMed] [Google Scholar]
- 7.Evans JR, Smeeth L, Fletcher AE. Risk of Admission to a Nursing Home Among Older People with Visual Impairment in Great Britain. Arch Ophthalmol. 2008;126:1428–1433. doi: 10.1001/archopht.126.10.1428. [DOI] [PubMed] [Google Scholar]
- 8.Rosenfeld P, Rich R, Lalwani G. Ranibizumab: phase III clinical trial results. Ophthalmol Clin N Am. 2006;19:361–372. doi: 10.1016/j.ohc.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 9.Age-Related Eye Disease Study Research Group. A Randomized, Placebo Controlled, Clinical Trial of High-Dose Supplementation with Vitamins C and E, Beta Carotene, and Zinc for Age-Related Macular Degeneration and Vision Loss. AREDS Report No. 8. Arch Ophthalmol. 2001;119:1417–1436. doi: 10.1001/archopht.119.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mangione CM, Lee PP, Gutierrez P, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute visual function questionnaire (VFQ-25) Arch Ophthal. 2001;119:1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 11.Reischies FM, Geiselmann B. Age-related cognitive and vision impairment affecting the detection of dementia symdrome in old age. Br J Psychiatry. 1997;171:449–451. doi: 10.1192/bjp.171.5.449. [DOI] [PubMed] [Google Scholar]
- 12.West SK, Rubin GS, Broman AT, Munoz B, et al. How Does Visual Impairment Affect Performance on Tasks of Every Day Life? Arch Ophthalmol. 2002;120:774–780. doi: 10.1001/archopht.120.6.774. [DOI] [PubMed] [Google Scholar]
- 12.Verbrugge LM, Jette AM. The Disablement Process. Soc Sci Med. 1994;38:114–128. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 13.Verbrugge LM, Lepkowski JM, Imanaka Y. Comorbidity and its impact on disability. Milbank Q. 1989;67:450–484. [PubMed] [Google Scholar]
- 14.World Health Organization. ICF: Introduction. 2001 December; Retrieved 12/20/01, from http://www.who.int/icf/icfthemplate.cfm.
- 15.Cuijpers P, van Straten A, Warmerdam L. Problem solving therapies for depression: A meta-analysis. European Psychiatry. 2007:9–15. doi: 10.1016/j.eurpsy.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Mynors-Wallis LM, Gath DH, Lloyd-Thomas AR, Tomlinson D. Randomized Control Trial Comparing Problem-Solving Treatment With Amitriptyline and Placebo for Major Depression in Primary Care. Br Med J. 1995;310:441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeVellis BN, Blalock SJ, Hahn PM, DeVellis RF, Hochbaum GN. Evaluation of a problem-solving intervention for patients with arthritis. Patient Education and Counseling. 1988;11:29–42. [Google Scholar]
- 18.Ahles PA, Seville J, Wasson J, Johnson D, Callahan E, Stukel TA. Panel-based pain management in primary care: A pilot study. J Pain Symptom Manage. 2001;22:584–590. doi: 10.1016/s0885-3924(01)00301-3. [DOI] [PubMed] [Google Scholar]
- 19.Perri MG, Nazu AN, McKelvey WF, Shermar RL, Renjilian DA, Viegener BJ. Relapse prevention training and problem-solving therapy in the long-term management of obesity. J Consult and Clin Psychology. 2001;69:722–726. [PubMed] [Google Scholar]
- 20.Mynors-Wallis L, Davies I, Gray A, Barbour F, Gath D. A randomized Control Trial and Cost Analysis of Problem-Solving Treatment for Emotional Disorders Given By Community Nurses in Primary Care. Br J Psych. 1997;170:113–119. doi: 10.1192/bjp.170.2.113. [DOI] [PubMed] [Google Scholar]
- 21.Williams JW, Jr, Barrett J, Oxman T, et al. Treatment of dysthymia and minor depression in primary care: A randomized controlled trial in older adults. JAMA. 2000;284:1519–1526. doi: 10.1001/jama.284.12.1519. [DOI] [PubMed] [Google Scholar]
- 22.Rovner BW, Casten RJ, Hegel MT, Lieby BE, Tasman WS. Preventing Depression in Age-Related Macular Degeneration. Archives of General Psychiatry. 2007;64:886–892. doi: 10.1001/archpsyc.64.8.886. [DOI] [PubMed] [Google Scholar]
- 23.Law M, Cooper B, Strong S, Stewart D, Rigby P, Letts L. The person-environment-occupation model: A transactive approach to occupational performance. Canadian Journal of Occupational Therapy. 1996;63:9–23. doi: 10.1177/000841749906600304. [DOI] [PubMed] [Google Scholar]
- 24.Borkovec T, Newman M, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. J Consulting Clin Psych. 2002;70:288–298. [PubMed] [Google Scholar]
- 25.Alexopoulos G, Raue P, Arean P, Lytle R. Problem-solving therapy vs. supportive therapy in geriatric major depression with executive dysfunction. Am J Geriatr Psychiatry. 2003;11:46–52. [PubMed] [Google Scholar]
- 26.Barrowclough C, King P, Colville J, et al. A Randomized Trial of the Effectiveness of Cognitive-Behavioral Therapy and Supportive Counseling for Anxiety Symptoms in Older Adults. J Consulting Clin Psych. 2001;69:756–762. doi: 10.1037//0022-006x.69.5.756. [DOI] [PubMed] [Google Scholar]
- 27.Perlis RH, Ostacher M, Fava M, Nierenberg AA, Sachs GS, Rosenbaum JF. Assuring that double-blind is blind. Am J Psych. 2001;167:250–251. doi: 10.1176/appi.ajp.2009.09060820. [DOI] [PubMed] [Google Scholar]
- 28.Carroll KM, Rounsaville BJ, Nich C. Blind Man’s Bluff: Effectiveness and Significance of Psychotherapy and Pharmacotherapy Blinding Procedures in a Clinical Trial. J Consulting Clinical Psych. 1994;62:276–280. doi: 10.1037//0022-006x.62.2.276. [DOI] [PubMed] [Google Scholar]
- 29.Stelmack JA, Szlyk JP, Stelmack TR, et al. Measuring outcomes of low vision rehabilitation with the Veterans Affairs Low Vision Visual Functioning Questionnaire (VA LV VFQ-48) Invest Ophthalmol Vis Sci. 2006;47:3253–3261. doi: 10.1167/iovs.05-1319. [DOI] [PubMed] [Google Scholar]
- 30.Massof RW. A systems model for low vision rehabilitation. I. Basic concepts. Optom Vis Sci. 1995;72:725–736. doi: 10.1097/00006324-199510000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Massof RW, Rubin GS. Vision Function Questionnaires. Surv Ophthalmol. 2001;45:531–548. doi: 10.1016/s0039-6257(01)00194-1. [DOI] [PubMed] [Google Scholar]
- 32.Bilsbury CD, Richman A. A Staging Approach to Measuring Patient-Centered Subjective Outcomes. Acta Psychiatr Scand. 2002;106 (suppl 414):5–40. doi: 10.1046/j.0001-690x.2002.00052.x. [DOI] [PubMed] [Google Scholar]
- 33.Arnold LE, Vitiello V, McDougle C, et al. Parent-Defined Target Symptoms Respond to Risperidone in RUPP Autism Study: Customer Approach to Clinical Trials. J Am Acad Child Adolesc Psych. 2003;42:1443–1450. doi: 10.1097/00004583-200312000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Mulsant B, Mazumdar S, Pollock B, et al. Methodological Issues in Characterizing Treatment Response in Demented Patients with Behavioral Disturbances. Int J Geriatr Psychiatry. 1997;12:537–547. [PubMed] [Google Scholar]
- 35.Scott IU, Schein OD, West S, et al. Functional status and quality of life measurement among ophthalmic patients. Arch Ophthalmol. 1994;112:329–335. doi: 10.1001/archopht.1994.01090150059023. [DOI] [PubMed] [Google Scholar]
- 36.Ware JE, Nelson EC, Sherbourne CD, Stewart AL. Preliminary tests of a 6-item general health survey: A patient application. In: Stewart Anita, Ware John., editors. Measuring Functioning and Well- Being: The Medical Outcomes Study Approach. Duke University Press; Durham: 1992. [Google Scholar]
- 37.Von Korff M, Wagner EH, Saunders K. A Chornic Disease Score From Automated Pharmacy Data. J Clin Epidemiol. 1992;45:197–203. doi: 10.1016/0895-4356(92)90016-g. [DOI] [PubMed] [Google Scholar]
- 38.Lawton MP, Moss M, Fulcomere MC, Kleban MH. A Research and Science Oriented Multi-Level Assessment Instrument. J Geront. 1982;37:91–99. doi: 10.1093/geronj/37.1.91. [DOI] [PubMed] [Google Scholar]
- 39.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kanter JW, Mulick PS, Busch AM, Berlin KS, Martell CR. The Behavioral Activation for Depression Scale (BADS): Psychometric Properties and Factor Structure. J Psychopathol Behav Assess. 2007;29:191–202. [Google Scholar]
- 41.Massof RW. Application of stochastic measurement models to visual function rating scale questionnaires. Ophthal Epidemiol. 2005;12:103–124. doi: 10.1080/09286580590932789. [DOI] [PubMed] [Google Scholar]
- 42.Massof RW, et al. Visual disability variables. I. The importance and difficulty of activity goals for a sample of low vision patients. Arch Phys Med Rehabil. 2005;86:946–953. doi: 10.1016/j.apmr.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 43.Massof RW, et al. The Activity Inventory: An adaptive visual function questionnaire. Optom Vis Sci. 2007;84:763–774. doi: 10.1097/OPX.0b013e3181339efd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Massof RW. An interval-scaled scoring algorithm for visual function questionnaires. Optom Vis Sci. 2007;84:690–705. doi: 10.1097/OPX.0b013e31812f5f35. [DOI] [PubMed] [Google Scholar]
- 45.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Personality Social Psych. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 46.Casten R, Rovner B, Lieby B, Tasman W. Depression Despite Anti Vascular Endothelial Growth Factor Treatment of Age-Related Macular Degeneration. Arch Ophthalmol. 2010;128:506–507. doi: 10.1001/archophthalmol.2010.24. [DOI] [PubMed] [Google Scholar]