Abstract
The objective of this study is to evaluate the psychological responses to caregiving between black and white dementia caregivers measured by self-reports of depressive symptoms evaluating the impact of sub-components of the Center for Epidemiologic Studies Depression Scale (CES-D) and residential arrangements of the caregiving dyad. The method included 87 intergenerational family caregivers enrolled in the Duke Caregiver Study (50 white and 37 black). Total CES-D and the four sub-components were modeled as dependent measures in separate linear regressions. Three models were examined. The first model tested race, living arrangements, and their interaction. The second model adjusted for age, gender, education, income, health status, cultural justification for caregiving, crime concerns, systolic blood pressure, diastolic blood pressure, and glycosylated hemoglobin. A third model added adjustment for caregiver burden. The results showed that there was a significant race by residence interaction for CES-D, somatic symptoms and depressive affect such that when the dyads are living apart – with the care recipient in their own home or in an institutional setting – whites reported more depressive symptoms than blacks. When the dyads lived together, this was reversed, and blacks reported higher depressive symptoms than whites. To conclude, all the parameters such as race, living arrangements, and the components of depression need to be taken into account to understand the impact of caregiving on the emotional health of caregivers.
Keywords: psychological and behavioural symptoms, psychological and social aspects, depression, cultural aspects, caregiving
Introduction
The literature on the impact of caregiving has found that as a group, black caregivers tend to report fewer depressive symptoms during the caregiving experience (Dilworth-Anderson, Williams, & Gibson, 2002; Haley et al., 1995; Pinquart & Sorensen, 2005; Roth, Haley, Owen, Clay, & Goode, 2001). Caregiving is an additional stressor that is added onto ongoing life situations with multiple racial differences (Dilworth-Anderson, 1998; Jackson, Antonucci, & Brown, 2004). The reasons for this are not well understood. In the literature on racial differences in response to stresses of discrimination, African Americans and persons of lower socioeconomic status (SES) have been reported to be less adversely affected than whites and upper SES persons in mental health indicators. This is seen as a paradox as physical health consequences of stress are greater in African Americans (Williams, Yu, Jackson, & Anderson, 1997). In particular, rates of cardiovascular disease (CVD) including hypertension and diabetes are significantly higher in black than in white Americans. Prevalence of total CVD is 45.9% for black males and females compared to 37.8% for white men and 33.3% for white women – a 21.4% increase for black men and a 37.8% increase for black women compared to their white counterparts (American Heart Association Committee on Statistics, 2009).
The most commonly used measure of mental or emotional health in studies of caregivers of Alzheimer’s disease (AD) patients has been depression, as assessed in terms of depressive symptoms using the Center for Epidemiologic Studies Depression Scale (CES-D: Radloff, 1977). Depression, as indexed by the total score on the CES-D, however, may not be an equally good measure of emotional health for all ethnic groups. Roth, Ackerman, Okonkwo, and Burgio (2008) investigated the four-factor model of depression (Shafer, 2006) in 1229 primary caregivers from the Resources for Enhancing Alzheimer’s Caregiver Health (REACH) study comparing African American, white, and Hispanic caregivers. They used latent factors representing depressive affect, well-being, interpersonal problems, and somatic symptoms. Their results indicated black/white differences for depressive affect and well-being such that blacks reported less-depressive affect and better well-being than whites, no ethnic differences for somatic symptoms, and Hispanic/white differences for interpersonal problems. Dilworth-Anderson’s 20-year review of research on race, ethnicity, and culture (Dilworth-Anderson et al., 2002) found that a widely held belief about minority caregivers is that they are generally less distressed than their white counterparts, especially when the index of distress is depression. This is often interpreted as reflecting more resilience (Haley et al., 1995; Roth et al., 2001; Shaffer, Dooley, & Williamson, 2007), but may also be a function of differential cultural meanings attached to caregiving or other differences between caregivers that vary by race and are not controlled for, or other unmeasured factors that were not included in the design of the study. Culture is defined in this study as a way of life shared by members of a population group and includes values that give meaning to experience, and thus goes beyond the concept of race (Dilworth-Anderson, 1998) and has dynamic effects across the lifespan (Jackson et al., 2004).
As the epidemiology of dementia of the Alzheimer type (DAT) changes over time, so does the nature of caregiving required. Jalbert, Daiello, and Lapane (2008) review the current state of knowledge on DAT. They report that the median survival time is estimated at 11.8 years and that hours of care required go from 13.1 per week for patients with mild dementia to 46.1 for those with more advanced disease. In addition, as many as 90% of patients with dementia will be institutionalized before death. Thus, caregiving is a process that changes as the disease progresses and the sites of care shift from independent or communal residential living arrangements to institutional care. These changes in site of care are also related to changes in depression for the caregiver. A large multisite demonstration project of over 5000 caregivers (of whom 8% were not white) found that depression was reduced at six months after institutional placement of the care recipient (CR) and stabilized after one year suggesting that the transition to institutional care can be beneficial for caregivers as indexed by reduced caregiver burden and reduced depression (Gaugler, Mittleman, Hepburn, & Newcomer, 2009).
The Duke Caregiver Study was designed to study caregiving as a real-world analogue to our work on studying stress in laboratory settings with an emphasis on understanding the role of genes in the serotonin system and the physical environment (Williams, 1994, 2008). It focused on caregiving for a relative with dementia within the context of stress research with matched controls selected for race, gender, age, neighborhood, and relation to the CR equivalent. This study included a full range of dementia severity in the CR and caregiving dyads in various stages of the caregiving process, including dyads living together, living in separate homes in the community, and with the CR in a long-term care (LTC) facility.
Dilworth-Anderson et al. (2005) reported on the first study of the Cultural Justification for Caregiving Scale (CJCS; Dilworth-Anderson, Goodwin, & Williams, 2004) comparing black or African American and white or European American caregivers. Confirmatory factor analysis indicated that the scale did not differ by racial group in the item loadings, and thus the scale assessed the reasons for caregiving similarly in both black and white caregivers. Compared to white caregivers, African American had higher scores on cultural reasons for giving care. In addition to cultural factors that help to explain psychosocial responses to caregiving, place and context of caregiving are also important. Brummett et al. (2005) reported on neighborhood characteristics that moderated the impact of caregiving on fasting blood glucose (FBG) levels. Neighborhood characteristics were not associated with FBG in controls; but in caregivers, higher levels of crime concerns were associated with higher FBG, controlling for income, education, and race. Thus, multiple sources of stress may be involved in the impact of caregiving on health and include the environmental context of the neighborhood. A recent review of the epidemiology of depression (Kim, 2008) suggests that environmental factors play an important but understudied role. Environmental factors were assessed in two different ways in this study. First, in the residential living arrangements of the caregiver dyad and second by ratings of neighborhood characteristics that were shown to be associated with the levels of FBG.
Thus, the Duke Caregiver Study allows us to evaluate racial differences in subscales of depression as a response to caregiving with particular attention to the possible role of cultural, environmental (including neighborhood characteristics and residential status of the caregiver dyad), and health factors at a single point in time with individuals in different stages of the caregiving process. We expect that race differences in depression will be reduced as covariates reflecting cultural and environmental variables are added to the sequential models. We also expect that there will be race differences on the subscales of the CES-D. We expect that effects of caregiving on that blacks would be more likely in the somatic symptoms subscale of the CES-D given the black versus white differences in the prior research on physical versus mental health responses to stress (Williams et al., 1997), while effects of caregiving on whites would be more likely to be seen in depressive affect component.
Our study was not designed to follow individuals through transitions in living arrangements, but is a cross-sectional snapshot of caregivers where dyads lived together or separately in the community or separately with the CR in institutional care. While we expected the depressive symptom levels in caregivers to be lower (cf. Gaugler et al., 2009) when the CR is institutionalized, we had no a priori predictions that race would moderate the impact of the dyad’s living arrangements on depressive symptoms. We used regression models to examine race, living arrangements, and their potential interaction as predictors of depressive symptoms and its subscales.
Methods
Participants
The 87 participants in this report are a subsample from The Duke Caregiver Study. The Duke Caregiver Study included data from 344 persons of whom 175 were family caregivers matched to 169 non-caregiving controls. Because the focus of this article is on race, emotional health, and the residential environment, only non-spouse caregivers are included in the analyses reported here. This is due to the differential distributions of the variables of interest in the analyses between spouse and adult child caregivers. Only 12% of spouse caregivers were black and none of the spouse dyads lived apart in the community. In our spouse caregivers, 73% lived together in the community with 52 couples in their own homes and nine couples in a shared dwelling located in a life-care community. Of the 27% of the couples living apart with the CR in LTC, 14 of the spouses remained in their own homes and nine spouses lived in a separate dwelling that was a part of the same life-care community. The 87 intergenerational family caregivers (50 white and 37 black) included in this report joined the study between June 2002 and May 2004. The majority were adult children (49 of 50 whites and 35 of 37 blacks) with one white and two black grandchildren caregivers. All participants lived within the driving distance of Duke Hospital. CRs lived with the respondent in the same home (n= 26), or lived separately in a two separate homes (n= 23), or lived separately with the CR in a LTC facility (n= 38). All respondents were primary caregivers. This resulted in a wide range of dementia severity from a diagnosis of mild cognitive impairment (MCI) to terminal dementia. Four respondents who met the criteria for this report were dropped from the analysis due to missing data (one did not report income, one did not report education, and two did not give sufficient blood to be assayed for glycosylated hemoglobin) resulting in 87/91 or 95.6% of eligible respondents included in this report.
The final sample used in this article had 12 black and 11 white dyads who lived apart in the community; 11 black and 27 white dyads where the CR lived in a LTC facility, and 14 black and 12 white dyads who lived together in the community. The race by residence distribution was not statistically significant (χ2= 5.10, p= 0.07); but it was interesting. Descriptively, for blacks 32% lived apart in the community, 30% with the CR in LTC, while 38% lived together; for whites the distribution was 22% living apart in the community, 50% in LTC, and 24% living together.
Parent study population
Caregivers were recruited using flyers, advertisements in the local media, and community outreach efforts conducted in collaboration with the Duke Caregiver Support Program. Caregivers nominated controls who were matched by location, age, race, and relationship to the CR (see Brummett et al., 2005 and Dilworth-Anderson et al., 2005 for additional information on the parent study). The parent study included an additional 84 spouse caregivers and 169 controls. Preliminary analysis of the full parent study population indicated that living arrangements for the caregiving dyads were important and these empirical findings led to the design of this study.
Study procedures
Study procedures were identical to the parent study. Data were collected at the respondent’s home and in the laboratory. Individuals received a home visit to profile their physical environment, leave questionnaires to be filled out, and instruct persons on the collection of physiological samples for analyses. A visit to the Duke Clinical Research Center was scheduled within the week where subjects returned their questionnaires which could be checked for missing data, had blood drawn and a medical history taken by the study nurse, and were interviewed about their caregiving situation.
Study participants were paid $250 for their participation and received a report of their medical findings and any needed referrals from the Duke Caregiver Support Group. This study was approved by the Duke University Medical Center Institutional Review Board.
Measures
Depressive symptoms were assessed using the CES-D and the four subscales. Subscales were calculated from the items assigned to scales in Table 3 in Roth et al. (2008). Sample items and α values were as follows for the subscales: somatic (bothered by things, appetite was poor and trouble concentrating) α= 0.77, depressive affect (cannot shake the blues, felt depressed, and sad) α= 0.78, well-being (hopeful about the future and happy) α= 0.74, and interpersonal (people disliked me and people were unfriendly) α= 0.86.
Residential arrangements of the caregiving dyad were assessed during scheduling so that arrangements for the CR could be made (funds for sitters were provided – or the CR could accompany the caregiver to the laboratory) and appropriate control matches could be recruited. Residential arrangements were categorized as living together in the same residence or living apart in the community. Living apart was further divided into situations where the CR lived in a separate home and where the CR lived in a LTC facility. Caregivers who lived in life-care communities were matched to controls from the same life-care communities.
Perceptions of neighborhood conditions were indexed by a measure of crime concerns. This was derived from a factor analysis of respondents’ descriptions of their physical environment using 21 items from a questionnaire designed to measure the participant’s ratings of specific problems. This score moderated the impact of environment on glucose metabolism in a prior study by our group (Brummett et al., 2005). The factor scores are standard scores with a mean of 0 and a standard deviation (SD) of 1, and positive numbers reflect a better environment.
Health status indicators were systolic blood pressure (SBP) and diastolic blood pressure (DBP), and glycosylated hemoglobin concentration (HbA1c%). SBPs >140 mmHg, DBPs >90 mmHg, and HbA1c >6% are indicative of disease. HbA1c gives an estimate of the average plasma glucose over the previous three months; a level of 6% corresponds to a fasting glucose level of 126 mg/dL indicating diabetes. In the overall study, race was unrelated to fasting glucose levels, but blacks were more likely to have elevated levels of HbA1c. More detailed information about these measurements, findings, and the overall study design can be found in Brummett et al. (2005).
Age was measured in years, gender was modeled as a numeric variable with 1= male and 0= female, education was measured in years, and income was measured in categories from under $10,000 to over $100,000 per year in $5000 increments.
Reasons for giving care that reflect cultural values were indexed by the CJCS (Dilworth-Anderson et al., 2004). This 10-item scale has a Cronbach α= 0.86.
Objective caregiver burden was indexed with the Clinical Dementia Rating (CDR; Morris, McKeel, Fulling, Torack, & Berg, 1988) and the number of years of caregiving assessed by the study nurse in an interview with the caregiver. The range of dementia in the CR group was large with CDR 0 (no dementia but with a diagnosis of MCI, n= 1), CDR 0.5 (diagnosis pending with n= 8), CDR 1 (mild with n= 18), CDR 2 (moderate with n= 30), CDR 3 (severe with n= 25), CDR 4 (profound with n= 7), and CDR 5 (terminal dementia with n= 2). Length of time of caregiving ranged from 1 to 20 years. The CR was not evaluated independently.
Statistical analyses
The focus of this study was to examine differences in the residence of the caregiver dyad as a potential moderator of race differences in the symptoms of depression. Total CES-D and its four subscales were modeled as dependent measures in separate linear regression analyses using PROC GLM (SAS, version 9.1, 2002–2003). When a model did not have a significant race by residence interaction, it was re-run to check the parameters after the interaction term was removed. The analyses were conducted in three related steps with each step testing a more inclusive model. In the preliminary model we tested race, living arrangements, and their interaction as predictors of the total CES-D score and its four subscales. The next model adjusted for variables in our study that have been associated in the caregiving literature with race, with depression, or with both factors. This set of covariates included age, gender, education, income, CJCS, crime concerns, SBP, DBP, and HbA1c. The final model added adjustment for the objective burden imposed by the degree of dementia in the CR and the number of years as a caregiver. This analytic strategy tested our emerging hypothesis that race differences in depressive symptoms that were moderated by residential location could be accounted for by adjusting for socioeconomic, demographic, and health indicators in the intermediate model, adding adjustment for caregiver burden in the final model. The adjustment for caregiver burden in the final model was prompted by the observation that when the CR was in LTC, the mean CDR was 2.6 for both black and white caregivers, when living in two homes in the community that average CDR was 1.5 for blacks and 1.2 for whites; however, when the dyads lived together, the CDR was 2.6 for blacks, the same level of impairment as for the LTC groups for care for both black and white caregivers, but only 1.8 for whites.
Results
The descriptive data are shown in Table 1 organized by our study design. The first section of the table shows the total CES-D scale and its subscales, the second section of the table shows the nine covariates used in the intermediate model as adjustment factors from the traditional caregiving literature, and the third section of the table shows the two measures of caregiver burden as distributed in our sample for the final model. For each variable, the mean and SD is given for residential groups and race as tested in a regression analysis with no interactions.
Table 1.
Description of study variables.
| Variable | Live apart | CR LTC | Together | F (3, 83) | Black | White | F (3, 83) |
|---|---|---|---|---|---|---|---|
| Number of S ’s | 23 | 38 | 26 | 37 | 50 | ||
| Measures of depressive symptoms | |||||||
| CES-D | 13.3 (11.9) | 10.9 (10.2) | 12.9 (10.9) | 0.70 | 10.9 (10.4) | 13.1 (11.2) | 1.41 |
| Somatic | 5.1 (4.7) | 4.6 (3.5) | 5.3 (4.3) | 0.41 | 4.4 (4.2) | 5.3 (3.9) | 1.13 |
| Depressive affect | 3.7 (4.6) | 3.2 (4.3) | 3.4 (4.5) | 0.21 | 2.9 (4.4) | 3.7 (4.4) | 0.81 |
| Well-being | 4.2 (3.5) | 2.8 (3.2) | 3.7 (3.3) | 1.77 | 3.0 (2.8) | 3.7 (3.6) | 1.76 |
| Interpersonal | 0.43 (0.90) | 0.36 (0.99) | 0.57 (1.17) | 0.35 | 0.4 (0.9) | 0.5 (1.1) | 0.08 |
| Adjustment variables in intermediate model | |||||||
| Age | 51.1 (9.7) | 53.7 (10.4) | 50.85 (10.0) | 0.61 | 51.2 (10.3) | 52.9 (10.0) | 0.25 |
| Gender (%) | 4.3 (20.8) | 15.7 (37.0) | 23.0 (43.0) | 1.7 | 16.2 (37.3) | 14.0 (35.0) | 0.10 |
| Education | 15.2 (2.4) | 16.0 (2.8) | 15.8 (2.7) | 0.75 | 15.8 (2.6) | 15.7 (2.7) | 0.20 |
| Income | 53.7 (30.7) | 68.8 (30.7) | 57.3 (34.7) | 1.21 | 53.6 (30.2) | 67.2 (32.8) | 2.44 |
| CJCS | 32.2 (7.7) | 34.4 (4.9) | 33.3 (5.6) | 1.98 | 35.0 (6.0) | 32.4 (5.7) | 6.11* |
| Crime concerns | 0.5 (1.2) | −0.2 (0.9) | −0.22 (0.58) | 4.3* | 0.06 (0.84) | −0.01 (1.0) | 0.15 |
| SBP | 111.4 (11.1) | 119.9 (16) | 124.4 (16.7) | 5.2** | 122.7 (14.9) | 116.2 (15.9) | 4.64* |
| DBP | 64.1 (5.7) | 67.0 (9.0) | 73.4 (8.7) | 8.2*** | 70.5 (9.5) | 66.4 (8.0) | 4.59* |
| HbA1c% | 5.9 (0.80) | 5.6 (0.56) | 5.8 (0.99) | 0.54 | 6.0 (0.74) | 5.6 (0.72) | 6.48** |
| Adjustment variables in final model | |||||||
| CDR | 1.35 (0.89) | 2.59 (1.03) | 2.21 (0.85) | 13.8*** | 2.2 (1.2) | 2.1 (0.98) | 2.30 |
| Years caregiver | 5.4 (2.4) | 5.9 (4.4) | 5.9 (4.0) | 0.54 | 6.9 (4.3) | 5.0 (3.1) | 6.50** |
Notes: % represents % male; CJCS, Cultural Justification for Caregiving Scale; SBP, systolic blood pressure; DBP, diastolic blood pressure, HbA1c, glycosylated hemoglobin; CDR, Clinical Dementia Rating; and years is total of years a caregiver.
p<0.05,
p<0.01,
p<0.001.
There were no differences for either race or residential status for age, gender, education, income, total CES-D, or any of the subscales. There were residence differences for crime concerns – lower concerns for those who lived apart by reporting a better neighborhood, blood pressure which was higher for those who lived together, and the CDR which was highest when the CR was in LTC. There were race differences for cultural justification which was higher in blacks, the three health indicators indicating worse health status in blacks, and length of time being a caregiver which was longer for blacks.
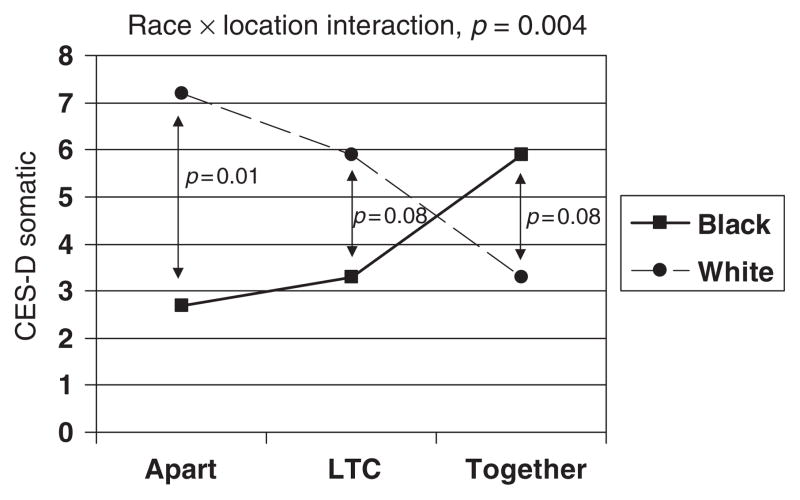
The initial preliminary model tested for an interaction of race and residence for total CES-D and its subscales. This interaction between residential status and race was found for the total CES-D (F= 3.4, p<0.05) and the somatic subscale (F= 5.4, p<0 01), with a marginally significant interaction for the depressive affect component (F= 2.8, p= 0.06). Results for the interaction in the well-being and interpersonal subscales were not significant (F= 0.88, p= 0.41 for well-being and F= 1.38, p= 0.257), and these two subscales are not studied further. In the intermediate model adjusted for the nine covariates, the race by residence interaction remained significant for the total CES-D (F= 4.4, p<0.05) and the somatic subscale (F= 6.1, p<0.001), and was significant for the depressive affect subscale (F= 3.3, p<0.05). In the final model, adding objective burden indicators, the race by residence interaction remained significant for the total CES-D (F= 4.0, p<0.05); the somatic subscale (F= 5.6, p<0.01); and the depressive affect subscale was no longer statistically significant (F= 2.6, p<0.10).
With regard to covariates from our intermediate model, the following were statistically significant: when predicting CES-D, income (p= 0.003) and education (p= 0.02) were significant; for somatic symptoms, income (p= 0.01), education (p= 0.02), SBP (p= 0.02), and DBP (p= 0.05); and for depressive affect, only income (p= 0.006). The race by residence interactions for the CES-D, somatic, and depressive affect subscales are shown in Figures 1–3. Note the similar patterns in the three figures.
Figure 1.
Total CES-D scores by race and residential location of the dyad.
Figure 3.
Depressive affect subscale scores by race and residential location of the dyad.
When we compare blacks and whites living apart – in either the community or with CR in LTC – depression is lower in blacks as compared to whites. In the situation where blacks and whites are living together, however, we see a cross over such that there is a trend for blacks to have higher levels of depressive symptoms than whites.
Because the mean level of depressive symptoms on the CES-D for the whites living apart is near the clinically significant level for the scale defined as 16 or higher, we also evaluated the proportion of each group in this range by race. The difference for the groups living apart was marginally significant with 54% of whites and 16% blacks in this range (χ2= 3.63, p= 0.056). When the CR was in LTC, 30% of whites versus none of the blacks was significant (χ2= 4.12, p= 0.042). There was no difference for those living together where 33% of the whites and 36% of the blacks scored in that range (χ2= 0.01, p= 0.899).
Discussion
This article started with a simple purpose, to increase our understanding of the basis for racial differences that have consistently found that black caregivers are less distressed than white caregivers. We looked at subscales of the CES-D scale and environmental measures that were well characterized in the Duke Caregiver Study. Our findings indicated that residential arrangements moderated the impact of the stress of caregiving on depressive symptoms for black and white non-spouse or adult child caregivers. We replicated the typical findings where blacks report fewer depressive symptoms than whites, but this was seen only when caregivers and CRs live apart. In contrast, when living together, the pattern was opposite – with higher rates of depressive symptoms reported by blacks than by whites. The effect of residence on race was not explained by a wide range of potential mediators for CES-D, and the somatic and depressive affect components. We had expected that controlling for objective caregiver burden in the final model would account for this interaction. It did not. Our sample size prevented a more detailed test of potential explanations in this sample.
Race and living arrangements and component of depressive symptoms must all be taken into account to understand how intergenerational caregivers respond emotionally to the task of caring for a demented elder. Looking at proportions scoring above the cut-off of 16 is also instructive. The proportions with elevated scores are similar for blacks and whites when living together. In contrast, when dyads are living apart, whites were more likely to be at a higher risk for depressive illness, suggesting that different interventions may be required at different phases of the caregiving process that are reflected by living arrangements in our study.
Generally, caregiving studies have not included the three residential arrangements in our study or their interactions with race as a factor in the emotional health of caregivers. For example, in Roth et al. (2008) all of the CRs were community dwelling while the participants in Gaugler et al. (2009) were compared before and after institutionalization. Furthermore, when both spouse and other family caregivers are included in this study, the meaning of coresidence changes. This is due to the expectation that spouses will be more likely to be coresidents than intergenerational family members as well as the possible cultural differences in such arrangements (Dilworth-Anderson, 1998). The Pinquart and Sorensen (2005) meta-analysis neither noted racial differences in coresidence, but not as a factor in the prediction of depression, nor did they consider the caregiving situation when the CR was in LTC. The covariates in our model behaved as expected with income and education related to depression and measures of blood pressure to the somatic symptom component.
The Duke Caregiver Study, designed as an ecologically valid study of stress in the community, differs in important respects from the typical caregiver study. Many caregiving situations not found in a single study are present in this data set: caregivers have a broad range of living arrangements and are at all stages in the caregiving process with adequate numbers of both black and white intergenerational family caregiving dyads.
Our study has many limitations. It did not include any Hispanic participants and as such cannot speak to that ethnic variation that we were neither able to measure nor were we able to recruit large numbers of black caregiving couples. We limited these analyses to the adult child/grandchild caregivers in our study as distribution of living arrangements differed in our adult child and spouse caregivers. We did not observe any spouse pairs who lived apart in the community in two separate residences. For spouses, life-care communities with different levels of care provided that option. We did not measure the living arrangements of the adult child dyads before caregiving became necessary, or the record the owner of the house where coresidence occurred. Our sampling frame was community based but not population based. Particular attention was paid to matching the environmental circumstances of caregivers with controls. Our results are from a cross-sectional snapshot. We know that the process cannot be inferred from cross-sectional studies such as ours. The trajectories of caregiving for adult child as well as spouse caregivers depend on many factors that will require longitudinal studies to elucidate. The inclusion of only 25% of the Duke Caregiver Study participants (87/344), who it made sense to include in this report, resulted in the relatively small sample used for these analyses. This reduced our power to further explore the reasons for our findings. Replication of our findings from larger, more representative data sets is needed to see if our findings are generalizable.
Nonetheless, our findings suggest some directions for future research to understand racial similarities and differences on the effects of caregiving. Racial differences in meaning and time of institutionalization as part of the caregiving process need to be more fully explored. The length of longitudinal studies needs to increase as the time of survival of the CR with dementia increases, and the time needed to follow the caregiver after the death of the CR also increases. The impact of caregiving stressors does not end with the death of the CR and this time course may vary by race.
In conclusion, our findings have shown that there are circumstances or conditions – when intergenerational caregiving dyads are living together – where the lower level of depressive symptoms on the CES-D for black caregivers compared to white caregivers are not observed. In our study, living together was more distressing for blacks while living apart was more distressing for whites. These findings suggest that a more careful approach to the architecture of the caregiving process may help to individualize interventions for all caregivers. Research has shown that depression in caregivers is linked to the development of CVD (Mausbach, Patterson, Rabinowitz, Grant, & Schulz, 2007) and underestimating the role of depression in minority caregivers may lead to a cascade of negative health outcomes (American Heart Association Committee on Statistics, 2009; Vitaliano, Zhang, & Scanlan, 2003) adding to the negative impact of depression as a disorder. This attention to differential health outcomes is important as demographic projections for the United States show that by 2030, 22% of the population will be over the age of 65 years and those elders will be more ethnically and racially diverse with 25% composed of ethnic minorities. Recognizing this, the National Academy of Science’s recommendations for research to the Behavioral and Social Research Branch of the National Institute on Aging included developing a psychology of diversity in order to understand if fundamental psychological processes that are associated with aging and standard measures used in psychological research are reliable and valid across groups (Carstensen & Hartel, 2006). The study of psychosocial responses to caregiving in diverse groups provides an excellent vehicle for developing a psychology of diversity.
Figure 2.
Somatic symptoms subscale scores by race and residential location of the dyad.
Acknowledgments
This research was supported by grant no. IIRG-08-89565 from the Alzheimer’s Association, R01 AG19605 from the National Institute on Aging with co-funding by the National Institute of Environmental Health Sciences, the National Institute of Mental Health, and P01HL36587 from the National Heart Lung and Blood Institute, The Claude D. Pepper Older Americans Independence Centers grant no. P30 AG028716, and the Duke Behavioral Medicine Research Center. The authors thank Jaye Efland and Shirley Austin for their excellent staff work on the study, Robin French for programming and data management, and Michael J. Helms and John Barefoot for statistical advice. Lisa Gwyther and Edna Ballard contributed to the design of this study.
References
- American Heart Association Committee on Statistics. Heart disease and stroke statistics-2009 update. Circulation. 2009;119:e1–e161. doi: 10.1161/CIRCULATIONAHA.108.191261. (Table 21–3, e157) [DOI] [PubMed] [Google Scholar]
- Brummett BH, Siegler IC, Rohe WM, Barefoot JC, Vitaliano PP, Surwit RS, et al. Neighborhood characteristics moderate effects of caregiving on glucose metabolism. Psychosomatic Medicine. 2005;67:752–758. doi: 10.1097/01.psy.0000174171.24930.11. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Hartel CR. When I’m 64. Committee on aging frontiers in social psychology, personality and adult developmental psychology. Washington, DC: National Academies Press; 2006. [Google Scholar]
- Dilworth-Anderson P. Emotional well-being in adult a later life among African Americans: A cultural and socio-cultural perspective. In: Schaie KW, Lawton MP, editors. Annual review of gerontology and geriatrics: Vol. 17. Focus on emotion and adult development. New York: Springer Publishing Company; 1998. pp. 282–303. [Google Scholar]
- Dilworth-Anderson P, Brummett BH, Goodwin P, Williams SW, Williams RB, Siegler IC. Effect of race on cultural justifications for caregiving. Journal of Gerontology: Social Sciences. 2005;60B:257–262. doi: 10.1093/geronb/60.5.s257. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Goodwin PY, Williams SW. Can culture help explain the physical health effects of caregiving over time among African American caregivers? Journal of Gerontology: Social Sciences. 2004;59B:S138–S145. doi: 10.1093/geronb/59.3.s138. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity and culture in caregiving research: A 20-year review (1980–2000) The Gerontologist. 2002;42(2):237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Mittleman MS, Hepburn K, Newcomer R. Predictors of change in caregiver burden and depressive symptoms following nursing home admission. Psychology and Aging. 2009;24:385–396. doi: 10.1037/a0016052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley WE, West CAC, Wadley VG, Ford GR, White FA, Barrett JJ, et al. Psychological, social and health impact of caregiving: A comparison of black and white dementia family caregivers and non-caregivers. Psychology and Aging. 1995;10:540–552. [PubMed] [Google Scholar]
- Jackson JJ, Antonucci TC, Brown E. A cultural lens on biopsychosocial models of aging. In: Costa PT, Siegler IC, editors. Recent advances in psychology and aging: Vol. 15. Advances in cell aging and gerontology. Amsterdam, The Netherlands: Elsevier; 2004. pp. 221–241. [Google Scholar]
- Jalbert JJ, Daiellio LA, Lapane KL. Dementia of the Alzheimer type. Epidemiologic Reviews. 2008;30:15–34. doi: 10.1093/epirev/mxn008. [DOI] [PubMed] [Google Scholar]
- Kim D. Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiologic Reviews. 2008;30:101–117. doi: 10.1093/epirev/mxn009. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Patterson TL, Rabinowitz YG, Grant I, Schulz R. Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psychology. 2007;26:539–544. doi: 10.1037/0278-6133.26.5.539. [DOI] [PubMed] [Google Scholar]
- Morris JC, McKeel DW, Fulling K, Torack RM, Berg L. Validation of clinical diagnostic criteria for Alzheimer’s disease. Annals of Neurology. 1988;24:17–22. doi: 10.1002/ana.410240105. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Ethnic differences in stressors, resources and psychological outcomes of family caregiving: A meta-analysis. The Gerontologist. 2005;45:90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Roth DL, Ackerman MI, Okonkwo OC, Burgio L. The four-factor model of depressive symptoms in dementia caregivers: A structural equation model of ethnic differences. Psychology and Aging. 2008;23:567–576. doi: 10.1037/a0013287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth DL, Haley WE, Owen JE, Clay OJ, Goode KT. Latent growth models and the longitudinal effects of dementia caregiving: A comparison of African American and White family caregivers. Psychology and Aging. 2001;16:427–436. [PubMed] [Google Scholar]
- SAS (Version 9.1) (2002–2003). [Computer software] Cary, NC: SAS Institute; [Google Scholar]
- Shafer AB. Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton and Zung. Journal of Clinical Psychology. 2006;62:123–146. doi: 10.1002/jclp.20213. [DOI] [PubMed] [Google Scholar]
- Shaffer DR, Dooley WK, Williamson GM. Endorsement of proactively aggressive caregiving strategies moderates the relationship between caregiver mental health and potentially harmful caregiver behavior. Psychology and Aging. 2007;22:494–504. doi: 10.1037/0882-7974.22.3.494. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychological Bulletin. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Williams RB. Neurobiology, cellular and molecular biology, and psychosomatic medicine. Psychosomatic Medicine. 1994;56:308–315. doi: 10.1097/00006842-199407000-00006. [DOI] [PubMed] [Google Scholar]
- Williams RB. Psychosocial and biobehavioral factors and their interplay in coronary heart disease. Annual Review of Clinical Psychology. 2008;4:349–365. doi: 10.1146/annurev.clinpsy.4.022007.141237. [DOI] [PubMed] [Google Scholar]