Summary
Data are lacking on long-term effects of HIV behavioural intervention programmes. In this study, we report intervention effects 36 months postintervention on condom use and relevant outcome variables from the theory-based programme ‘Focus on Youth in the Caribbean’ (FOYC). Participants (1360 sixth-grade youth) were randomized by school into: (1) FOYC, plus one of two brief parent interventions or (2) the control condition ‘Wondrous Wetlands’, plus a brief parent intervention. Mixed effect analysis demonstrated significant programme effects, including enhanced HIV/AIDS knowledge (effect size D = 0.44, 95% confidence interval [CI]: 0.43, 0.46), increased self-efficacy of (D = 0.42, 95% CI: 0.30, 0.54), skills for (D = 0.62, 95% CI: 0.56, 0.64) and intention to use a condom (D = 0.20, 95% CI: 0.03, 0.37). Youth who received FOYC plus the parental monitoring intervention had higher condom use rates (odds ratio = 1.49, 95% CI: 0.97, 2.28). Feedback effects from key variables were also detected, supporting the sustained effect.
Keywords: Protection Motivation Theory, preadolescent, HIV/AIDS, behavioural intervention
INTRODUCTION
Over the last quarter century, substantial progress has been made in effecting purposeful behavioural change to reduce HIV/AIDS risk behaviours.1 A vast literature describing randomized, controlled trials clearly demonstrates that interventions with attention to specific elements can be successful in reducing and preventing sexual risk behaviours.1–9 Support for consistent condom use beginning at the time of sexual debut is the cornerstone of adolescent HIV/AIDS prevention.7,9 A substantial body of literature indicates that the establishment of effective condom use behaviour requires HIV/AIDS knowledge, awareness of the benefits of condom use, skills regarding the use of condoms, confidence in these skills and awareness of the negative consequences of failure to use condoms.3,9–12
Despite advances overall in the field, specific demographic and sociogeographic subgroups remain at high risk. Among those remaining at high risk are adolescents and young adults, persons of colour and individuals in transitional and developing countries.1– 9,13 –15 A number of challenges continue to confront adolescent behavioural risk reduction interventions. Although available data indicate that intervention effects wane over time, there is a paucity of information regarding long-term effects from HIV prevention efforts and factors that may sustain such effects,11,16 –18 particularly among preadolescents and adolescents as they mature and face changing personal and social environments.19
The Bahamas has the second highest rate of HIV infection among the Caribbean nations. Heterosexual activity is the predominant mode of transmission. An estimated 3.3% of adults are infected, with an increased trend of infection among youth.3 A group of researchers from the USA, including paediatricians, an anthropologist, psychologists, epidemiologists and statisticians, and from The Bahamas, including educators, counsellors and physicians, have worked together for approximately a decade to address this problem through school-based HIV prevention efforts. This collaboration started at the peak of the HIV epidemic in The Bahamas when the Bahamian researchers learned of the USA researchers’ effective adolescent HIV prevention programme ‘Focus on Kids’ and parental monitoring programme ‘Informed Parents and Children Together’ (ImPACT).20– 22 The USA and Bahamian researchers adapted these programmes for use among preadolescent Bahamian youth (‘Focus on Youth in The Caribbean’ or FOYC) and their parents (‘Caribbean Informed Parents and Children Together’ or CImPACT). An alternative parent intervention (‘Goal for IT’ or GFI) was also employed without alterations among some of the parents. We have previously reported the effects from a randomized trial of the interventions through 24 months. Significant programme effects were detected from FOYC compared with the control condition, the ‘Wondrous Wetlands’ (WW, an educational environmental conservation programme), including improvements of HIV prevention knowledge and condom use skills, as well as positive changes in condom use perceptions and intentions.23–25
The purpose of this paper is to evaluate programme effects on condom use and related outcome variables 36 months postintervention. We hypothesized that the protective effects from the receipt of FOYC (including either parent intervention combination, e.g. FOYC/GFI or FOYC/CImPACT) on condom use observed through 24 months postintervention would be sustained through 36 months postintervention. In addition to programme effect evaluation, analyses were conducted to assess the role of variables reflective of the theoretic model guiding the intervention in mediating the intervention effect on the outcome variables.26
We also conducted analyses guided by Systems Theory and Feedback Control Theory27,28 to explore the potential role of positive feedback as a mechanism for sustaining longer-term effects of FOYC on condom use and influential factors. According to these theories, the output of a system (e.g. changes in outcome measures for an individual adolescent after he/she receives FOYC) will serve as feedback, which positively reinforces the intervention effect of FOYC. The feedback process may help maintain the status of the system until the feedback influence diminishes over time. In the current situation, receipt of FOYC is considered to be the original source of feedback that influences the system of behaviour change. Once the changes in the system components (e.g. HIV knowledge, condom use self-efficacy, skills, intention and condom use behaviour) have occurred, we hypothesize that they will continue to be reinforced through the feedback loops, thus sustaining the intervention effects. In addition, we hypothesize that the boosters serve as further input to strengthen the feedback loops, although this hypothesis could not be empirically assessed in the current design.
METHODS
Intervention programme
FOYC, based on the Protection Motivation Theory (PMT),29 consists of 10 primary sessions (delivered weekly after baseline survey) and two annual boosters (delivered after 12 and 24 months postintervention assessment). The sessions are designed to augment decision-making skills, including the development of a lifelong perspective in decision-making, communication and listening skills, and protective knowledge and skills regarding safer sexual behaviour. GFI and CImPACT are parenting interventions. GFI includes a 20-minute video filmed in the USA, which addresses decision-making regarding future planning for the parent and child; the video is followed by a structured discussion among the participants. CImPACT includes a 20-minute video filmed in The Bahamas addressing parent–child communication about sexual decision-making, followed by role playing and a condom demonstration. Detailed descriptions of FOYC, GFI and CImPACT have been provided elsewhere.23–25
Randomization
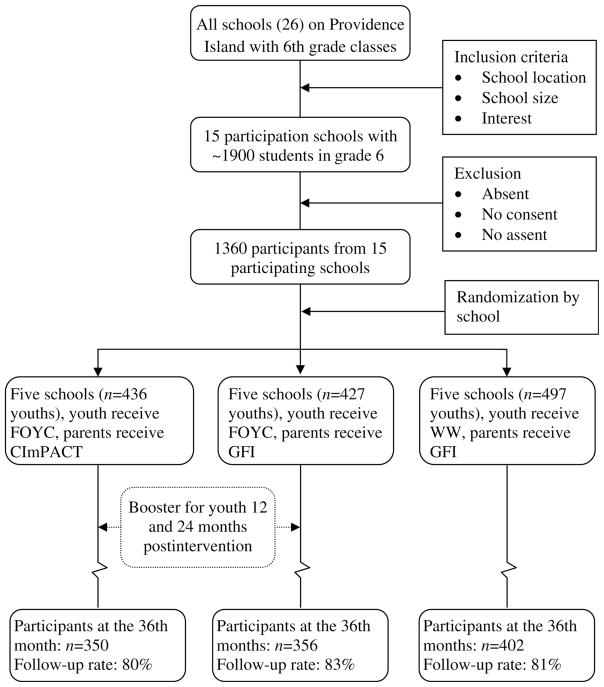
Participants were grade 6 students attending government elementary schools in New Providence, the most populous island of The Bahamas. Figure 1 summarizes the sampling and randomization of schools and students, intervention delivery and the timing of data collection. Detailed descriptions of this process are available in our earlier publications23–25 and are summarized here. Fifteen schools were selected from among all 26 government elementary schools of New Providence. The selection was based on expression of interest, school size and geographic distribution (e.g. the four geographic quadrants and rural/urban location). Enrollment occurred over two waves in two consecutive years yielding a final sample size of 1360 students. The 15 schools were randomized into three groups, each consisting of five schools. The first group of youth received FOYC and their parents received CImPACT, the second group of youth received FOYC and their parents received GFI, and the third group (serving as the control condition) of youth received WW and their parents received GFI. We elected to randomize participants by school to minimize potential intervention contamination.
Figure 1.
Flowchart of sampling, school randomization, intervention and evaluation 36 months postintervention. FOYC = Focus on Youth in the Caribbean; CImPACT = Caribbean Informed Parents and Children Together; GFI = Goal for IT
Data collection
Data were collected in classroom settings using the Bahamian Youth Health Risk Behavioral Inventory, a paper-and-pencil questionnaire adapted from the Youth Health Risk Behavioral Inventory30 through extensive ethnographic research and pilot testing. The baseline assessment was conducted prior to intervention randomization, and follow-up surveys were conducted at 6, 12, 18, 24 and 36 months postintervention, respectively. Survey data collected at the baseline and the 36-month follow-up are included in the present analysis. Both written parental consent and child assent were necessary for participation in the trial. Approval of the study protocol was obtained from the Human Investigation Committees at Wayne State University and at the Bahamian Ministry of Health.
Intervention variables
PMT constructs
As shown in Appendix A, questions assessing the seven constructs of PMT relevant to condom use were: self-efficacy, response efficacy and response cost; and intrinsic rewards, extrinsic rewards, severity and vulnerability.
HIV/AIDS knowledge
Eighteen items (Appendix B) were used to assess the levels of knowledge regarding HIV/AIDS, such as ‘If you touch someone with AIDS you can get AIDS’ (received no credit if answered ‘true’ and received one point if answered ‘false’). A mean score was derived for each individual participant based on the number of correct answers he or she provided in response to the 18 items. The computed scores were used for programme effect evaluation such that higher scores indicated more knowledge about HIV/AIDS transmission and prevention.
Condom use skills
Fourteen items (7 correctly phrased and 7 incorrectly phrased) were used to assess level of condom use skills (Appendix C). A mean score was derived for each individual based on the ratio of the total number of correct answers over 14 (the total number of items) such that higher scores indicated greater condom use skills.
Condom use intention and behaviours
Intention to use a condom was assessed among all youth (regardless of past sexual experience and/or future sexual intentions) by self-reported likelihood to use a condom if the individual were to have sex (1 = very unlikely and 5 = very likely). Condom use was assessed among those who initiated sex. A participant was categorized as having used a condom during sex for effective HIV prevention if he or she responded ‘all the time’ in response to the question: ‘How often did you use a condom when you had sex?’ (response options included ‘never’, ‘rarely’, ‘about half the time’, ‘more than half the time’ and ‘all the time’).
Demographic factors
Gender and chronological age were included as covariates. Although participants were randomly assigned into intervention and control conditions, our analyses revealed some significant baseline differences in several outcome variables (e.g. intention to use a condom, self-efficacy and response cost for condom use, and intrinsic rewards) across the intervention conditions (see Table 1). Therefore, in addition to gender and age, the outcome variables at baseline were adjusted so that the assessed programme effect would not be confounded.
Table 1.
Characteristics of the study sample at baseline, overall and by intervention status
| Items and constructs | Intervention |
Control WW/GFI | Overall | ||
|---|---|---|---|---|---|
| FOYC/GFI | FOYC/CImPACT | Subtotal | |||
| Sample, n | 427 | 436 | 863 | 497 | 1360 |
| Boys, n (%) | 180 (42.2) | 231 (53.0)** | 411 (47.6) | 228 (45.9) | 639 (47.0) |
| Girls, n (%) | 247 (57.8) | 205 (47.0) | 452 (52.4) | 269 (54.1) | 721 (53.0) |
| Age in years, n (%) | |||||
| 10 − | 273 (65.5) | 259 (60.7)** | 523 (63.0)* | 305 (62.8) | 837 (62.9) |
| 11 − | 116 (27.8) | 115 (26.9) | 231 (27.4) | 155 (31.9) | 386 (29.0) |
| 12 + | 28 (6.7) | 53 (12.4) | 81 (9.6) | 26 (5.3) | 107 (8.1) |
| Mean (SD) | 10.4 (0.6) | 10.5 (0.8) | 10.4 (0.7)* | 10.4 (0.6) | 10.5 (0.7) |
| PMT perception, mean (SD) | |||||
| Coping appraisal for condom use | |||||
| Self-efficacy (α = 0.87) | 2.55 (1.16)* | 2.27 (1.17) | 2.41 (1.17) | 2.38 (1.17) | 2.40 (1.17) |
| Response efficacy (α = 0.71) | 3.95 (0.94) | 3.93 (0.96) | 3.94 (0.95) | 3.87 (0.97) | 3.92 (0.96) |
| Response cost (α = 0.39) | 3.33 (0.54)* | 3.29 (0.58) | 3.31 (0.56)* | 3.24 (0.59) | 3.28 (0.57) |
| Threat appraisal for condom use | |||||
| Extrinsic reward (NA) | 2.47 (1.49) | 2.71 (1.52)** | 2.60(1.51) | 2.42 (1.61) | 2.54 (1.54) |
| Intrinsic reward (NA) | 2.98 (0.93)** | 3.08 (1.04) | 3.03 (0.99) | 3.17 (1.00) | 3.08 (1.00) |
| Perceived severity (α = 0.65) | 4.73 (0.60) | 4.62 (0.70) | 4.67 (0.66) | 4.70 (0.62) | 4.69 (0.64) |
| Vulnerability (α = 0.75) | 1.59 (0.81) | 1.74 (0.92) | 1.67 (0.86) | 1.67 (0.85) | 1.67 (0.86) |
| Knowledge and skills, mean (SD) | |||||
| HIV/AIDS knowledge | 0.72 (0.16) | 0.71 (0.16) | 0.72 (0.16) | 0.70 (0.17) | 0.71 (0.16) |
| Condom use skills | 0.55 (0.13) | 0.55 (0.13) | 0.55 (0.13) | 0.56 (0.14) | 0.55 (0.13) |
| Intention and behaviour | |||||
| Intention to use condom mean (SD) | 2.85 (1.70) | 3.14 (1.67)** | 3.00 (1.69) | 2.80 (1.62) | 2.92 (1.67) |
| Rate of condom use among sexually experienced, n (%) | 3 (23.1) | 4 (16.7) | 7 (19.4) | 2 (10.5) | 9 (16.4) |
FOYC = Focus on Youth in the Caribbean; GFI = Goal for IT; CImPACT = Caribbean Informed Parents and Children Together; WW = Wondrous Wetlands; PMT = Protection Motivation Theory
Comparison of interventions with the control using Student’s t-test for continuous variables (e.g. age, PMT perceptions, HIV knowledge, etc.) and chi-square test for categorical variables (e.g. gender composition and rate of condom use)
P = < 0.05 and
P = < 0.01
Programme effect evaluation
Descriptive statistics (e.g. mean, SD, rate and ratio) were used to summarize the sample characteristics. Cronbach alpha was computed to assess the internal consistency of the measurement scales. Differences in the outcome measures were first assessed using bivariate analyses, including analysis of variance, Student’s t-test (for continuous variables) and chi-square test (for binary variables). Programme effect size was assessed using Cohen’s D (for continuous outcome measures such as HIV/AIDS knowledge, condom use skills and the 7 PMT constructs, etc.) and odds ratio (OR) for binary outcome variable (e.g. increases in condom use rate). Observed effect from the bivariate analysis was further analysed using the following the mixed effect model to adjust for the design effect due to randomization at the level of the school:
where Yikl represents an outcome measure assessed at 36 months for the ith subject (i = 1–1360) nested in kth school (k = 1–15) who received lth intervention (l = 3, e.g. 1 = control, 2 = FOYC/CImPACT and 3 = FOYC/GFI); μ = grand mean; Cl indicates the effect of lth intervention at 36 months postintervention; and Xa represents p covariates, including age and gender, and the outcome variables assessed at baseline. The term Gkl is included in the model as a random effect to correct intraclass correlation due to the design of cluster randomization.31 Variances that remained are captured by the term eikl.
Mediation analysis
To explore the manner in which FOYC exerts programme effects on condom use, we constructed four mediation models to assess four variables (condom use self-efficacy, condom use response efficacy, HIV knowledge and condom use skills) in mediating the effect of the two intervention combinations in predicting the variable ‘condom use intention’ (Figure 2). We selected these four variables because they remained significantly different between the intervention and the control at 36 months. The mediation analysis was conducted using the regression method.32 Because both age and gender influence sexual behaviour, these variables were included as covariates in the mediation models.
Figure 2.
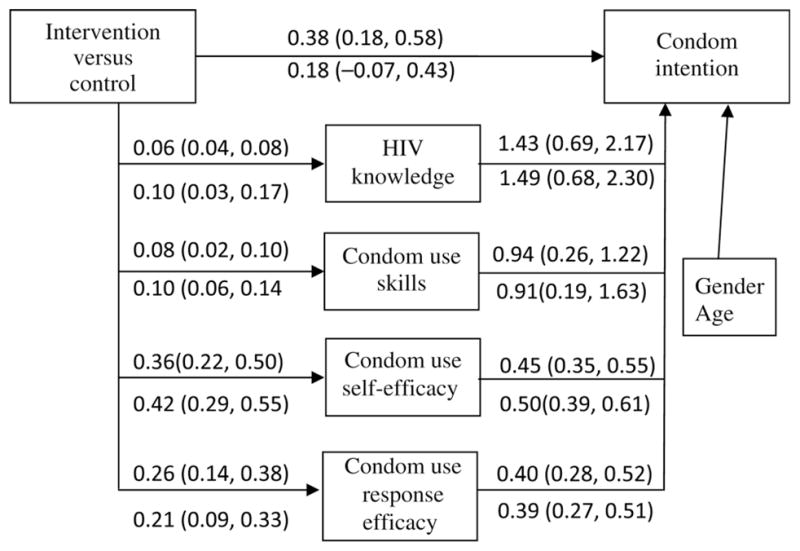
Mediation effect of four targeted variables related to condom intention, regression coefficients (95% CI). The numbers above the lines were for participants in the FOYC/CImPACT group and the numbers below the lines were for participants in the FOYC/GFI group. Each arrowed line indicates the direction of an effect. In addition to a direct effect from the intervention to condom use intention as the first line indicates, receipt of the intervention also affected condom use intention via HIV knowledge, condom use skills, condom use self-efficacy and condom use response efficacy. FOYC = Focus on Youth in the Caribbean; CImPACT = Caribbean Informed Parents and Children Together; GFI = Goal for IT
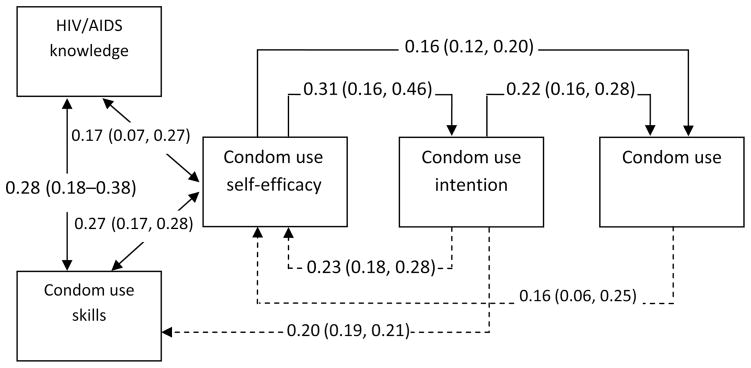
Feedback analysis
To explore factors influencing sustained effect of FOYC on condom use at 36 months postintervention, we assessed condom use and intention (assessed at 24 months) as feedback in predicting condom use skills, self-efficacy and condom use intention at 36 months using regression models (see Figure 3 later in this paper). The construction of the feedback loops was based on PMT theory; we selected those PMT-related measures that were affected significantly by the intervention (e.g. HIV knowledge, as well as condom use intention, skills, self-efficacy and response efficacy). According to General Systems Theory and Feedback Control Theory,27,28 positive internal feedback and boosters are two factors that may stabilize a system. In the present case, the maintenance of HIV knowledge and the enhancement of condom use intention, skills, self-efficacy, etc. consist of the positive internal feedback that are assumed to enhance condom use by the individual participants who received the external input (e.g. the FOYC intervention).
Figure 3.
Feedback model for sustained effect of FOYC on condom use through HIV knowledge, and self-efficacy and skills for condom use, and intentions to use a condom during sex. Note: Double arrowed line: correlation coefficients (95% CI that was computed using z-distribution with SE = 1/sqrt [n − 3]) assessed at 36 months postintervention; single-arrowed solid line: standard regression coefficients (95% CI) for the independent variables assessed at 24 months predicting the dependent variables assessed at 36 months; and single-arrowed dashed line: standard regression coefficients (95% CI) for the dependent variables assessed as 24 months reversely predicting the independent variables assessed at 36 months (see the text on the Feedback analysis for details). FOYC = Focus on Youth in the Caribbean
Survey data were manually entered. A double-entry protocol was used to minimize errors from data entry. Data quality was assessed and errors corrected against the original survey. Significance levels were assessed using 95% confidence intervals (CI), with the CI not containing zero (for assessing differences in means) or not containing 1 (for assessing an OR) as the criterion for statistical inference. Statistical analyses were conducted using the software SAS 9.2 (SAS Institute Inc, Cary, NC, USA).
RESULTS
Baseline comparability and attrition
Data in Figure 1 and Table 1 indicate that among the 1360 participants, 497 (37%) were randomized to receive WW and their parents to receive GFI; 863 were randomized to receive FOYC (63%), among whom the parents of 427 were randomized to receive GFI and 436 to receive CImPACT. The participants were 10–12 years old (mean age = 10.5, SD = 0.7 years) and 639 (47%) were male. There were no significant differences in the mean age of the participants between each of the two intervention groups and the control group. However, there were significantly more boys in the FOYC/CImPACT group than in the control group (P < 0.01). The majority of the outcome measures at baseline were similar for students in the three different intervention conditions. Compared with youth in the control group, youth in the FOYC/GFI group had a higher baseline assessment of perceived condom use self-efficacy (2.55 versus 2.40, P < 0.016) and response cost (3.33 versus 3.24, P = 0.012), and a lower perceived assessment of intrinsic rewards for engaging in sex without a condom (2.98, versus 3.17, P = 0.003). Youth in the FOYC/CImPACT group exhibited higher intentions to use a condom (3.14 versus 2.80, P = 0.0022).
Among the 1360 participants at baseline, data from 1108 (81%) were available at 36 months postintervention and were analysed. The follow-up rate was 80%, 83% and 81% for the FOYC/CImPACT, the FOYC/GFI and the control groups, respectively, and the differences were not statistically significant. The demographic (age and gender) and outcome-related variables did not differ significantly between participants who were retained in the trial at 36 months and those who were lost to follow-up. One hundred and fifty-six youth in the FOYC/CImPACT group, 117 in the FOYC/GFI group and 130 in the control group were sexually experienced.
Programme effect
Data in Table 2 indicate that youth who received FOYC scored significantly higher in condom use self-efficacy (Cohn’s D = 0.42, 95% CI: 0.30, 0.57) and condom use response efficacy (Cohn’s D = 0.30, 95% CI: 0.20, 0.41) compared with the control youth. Similar effects were observed for youth in the FOYC/CImPACT subgroup and the FOYC/GFI subgroup. These differences were statistically significant after controlling for the design effect due to cluster randomization, the baseline differences in these two measures and the demographic variables age and gender.
Table 2.
Effect of the programme FOYC assessed 36 months postintervention (adjusted mean, rate, effect size and odds ratio with 95% confidence interval)
| Variables | Control (n = 402) | FOYC (n = 706) |
FOYC/CImPACT (n = 350) |
FOYC/GFI (n = 356) |
|||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean/rate (95% CI) | ES/OR (95% CI) | Mean/rate (95% CI) | ES/OR (95% CI) | Mean/rate (95% CI) | ES/OR (95% CI) | |
| Coping appraisal (condom use) | |||||||
| Self-efficacy (α = 0.81) | 3.54 (3.45, 3.63) | 3.92 (3.85, 3.99) | 0.42 (0.30, 0.54) | 3.91 (3.82, 4.01) | 0.40 (0.25, 0.54) | 3.93 (3.83, 4.01) | 0.43 (0.30, 0.57) |
| Response efficacy (α = 0.76) | 4.13 (4.05, 4.21) | 4.38 (4.32, 4.44) | 0.30 (0.20, 0.41) | 4.40 (4.32, 4.49) | 0.35 (0.23, 0.46) | 4.35 (4.27, 4.44) | 0.26 (0.14, 0.38) |
| Response cost (α = 0.49) | 3.30 (3.26, 3.35) | 3.24 (3.21, 3.28) | 0.11 (0.05, 0.17) | 3.29 (3.23, 3.34) | 0.01 (−0.06, 0.08) | 3.20 (3.15, 3.25) | 0.21 (0.14, 0.28) |
| Threat appraisal (condom use) | |||||||
| Extrinsic rewards (single item) | 3.30 (3.26, 3.35) | 3.53 (3.34, 3.72) | 0.13 (−0.07, 0.33) | 3.49 (3.24, 3.74) | 0.17 (−0.05, 0.40) | 3.58 (3.29, 3.87) | 0.06 (−0.18, 0.30) |
| Intrinsic rewards (single item) | 2.99 (2.91, 3.06) | 2.97 (2.92, 3.03) | 0.01 (−0.18, 1.10) | 2.90 (92.82, 2.98) | 0.12 (0.10, 0.23) | 3.04 (2.96, 312) | 0.11 (0.01, 0.21) |
| Severity (α = 0.44) | 4.80 (4.75, 4.85) | 4.77 (4.74, 4.81) | 0.08 (0.01, 0.14) | 4.73 (4.68, 4.74) | 0.18 (0.10, 0.26) | 4.81 (4.76, 4.84) | 0.03 (−0.03, 0.10) |
| Vulnerability (α = 0.42) | 1.25 (1.20, 1.30) | 1.25 (1.22, 1.30) | 0.04 (−0.03, 0.10) | 1.31 (1.25, 1.37) | 0.16 (0.08, 0.25) | 1.21 (1.15, 1.26) | 0.11 (0.03, 0.18) |
| Knowledge/skills | |||||||
| HIV knowledge | 0.86 (0.85, 0.87) | 0.92 (0.91, 0.93) | 0.44 (0.43, 0.46) | 0.92 (0.91, 0.93) | 0.43 (0.41, 0.45) | 0.91 (0.90, 0.93) | 0.43 (0.41, 0.45) |
| Condom use skills | 0.57 (0.55, 0.59) | 0.67 (0.66, 0.68) | 0.62 (0.56, 0.64) | 0.66 (0.64, 0.68) | 0.56 (0.54, 0.59) | 0.67 (0.66, 0.69) | 0.68 (0.66, 0.71) |
| Intention and behaviour | |||||||
| Condom use intention (single item) | 4.08 (3.93, 4.23) | 4.36 (4.26, 4.46) | 0.20 (0.03, 0.37) | 4.46 (4.33, 4.58) | 0.27 (0.07,0.47) | 4.26 (4.11, 4.41) | 0.12 (−0.09, 3.30) |
| Condom use (%) | 27.3 (16.7, 37.9) | 35.5 (27.6, 43.4) | 1.49 (0.97, 2.28) | 38.4 (28.7, 48.1) | 1.69 (1.05, 2.73) | 31.3 (17.5, 45.1) | 1.15 (0.68, 1.94) |
FOYC = Focus on Youth in the Caribbean; GFI = Goal for IT; CImPACT = Caribbean Informed Parents and Children Together
Note: Results were estimated using the mixed effect modelling analysis (for the continuous variables) and the general linear mixed effect modelling analysis (for the binary condom use variable) to assess the differences between intervention and control by adjusting design effect from cluster randomization, gender, age and differences in the baseline measures
ES = Effect size (or Cohen’s D) was used to assess mean differences between one of the two intervention groups and the control group; OR = Odds ratio was used to assess differences in the rate of condom use between one of the two intervention groups and the control group
Significant differences were also observed between the control group and the FOYC group as a whole in HIV knowledge (Cohn’s D = 0.44, 95% CI: 0.43, 0.46), condom use skills (Cohn’s D = 0.62, 95% CI: 0.06, 0.64) and intention to use a condom (Cohn’s D = 0.20, 95% CI: 0.03, 0.37). Similar effects were also observed when each of the two subgroups FOYC/CImPACT and FOYC/GFI was compared with the control. Intention to use a condom during sex was stronger among FOYC youth as a whole (Cohn’s D = 0.20, 95% CI: 0.03, 0.37) and among the FOYC/CImPACT subgroup (Cohn’s D = 0.27, 95% CI: 0.07–0.47). Finally, a significantly higher rate of condom use during sex was observed for youth in the FOYC/CImPACT group compared with control youth (44.9% versus 31.5%, OR = 1.73, 95% CI: 1.09, 2.87).
Mediation effect
Figure 2 presents the analytical results for the four variables that significantly mediated the effect in each of the two intervention condition subgroups (FOYC/GFI and FOYC/CImPACT) on intention to use a condom during sex. After controlling for age and gender, all the connection paths were statistically significant except the direction effect from the intervention FOYC/GFI to condom use intention (regression coefficient b = 0.18, and 95% CI: −0.07, 0.43 that containing zero). For example, in addition to a direct effect (b = 0.18, and 95% CI: 0.18, 0.58), receiving FOYC/CImPACT was associated with increased condom use skills (b = 0.08, and 95% CI: 0.02, 0.10), which in turn resulted in greater intention to use a condom during sex (b = 0.94, and 95% CI: 0.26, 1.22). When condom use was included as the outcome variable, the same mediation analysis indicated that among the four variables, self-efficacy significantly mediated the intervention effect for both FOYC/CImPACT and the FOYC/GFI subgroups, respectively, using the same 95% CI criterion (data not shown in the figure).
Feedback effect
Feedback analysis (the dashed lines in Figure 3) indicated that after controlling for gender and age, intention to use a condom (standard regression coefficient b = 0.23, 95% CI: 0.18–0.28) and actual condom use (b = 0.16, 95% CI: 0.06, 0.25) at 24 months significantly predicted self-efficacy at 36 months. Condom use intention (b = 0.22, 95% CI: 0.19, 0.21) and self-efficacy (b = 0.16, 95% CI: 0.12, 0.20) at 24 months each significantly predicted condom use at 36 months, respectively.
DISCUSSION AND CONCLUSIONS
At 36 months postintervention, youth who received FOYC (with either parent intervention) compared with control youth showed significantly higher levels of HIV knowledge (effect size D = 0.44, 95% CI: 0.43, 0.46), condom use skills (D = 0.62, 95% CI: 0.56, 0.64), self-efficacy (D = 0.42, 95% CI: 0.30, 0.54), response-efficacy and intention to use a condom (D = 0.30, 95% CI: 0.20, 0.41). In addition, compared with control youth, FOYC youth whose parents received CImPACT demonstrated significantly higher rates of condom use (OR = 1.69, 95% CI: 1.05, 2.73). Previous postintervention assessments had revealed significant intervention effects on skills and self-efficacy for condom use and intention to use condoms. These effects were significantly higher among FOYC youth as a whole compared with control youth, and were particularly striking among FOYC/CImPACT youth.23–25 For example, the mean condom use self-efficacy scores (95% CI) at 12 months postintervention were 3.18 (2.99, 3.36) among FOYC/CImPACT youth and 2.85 (2.66, 3.03) among the controls (P < 0.05) and at 24 months were 3.59 (3.48, 3.70) and 3.15 (3.04, 3.26), respectively (P < 0.01).25 These results are important because they indicate that an HIV prevention intervention delivered to preadolescent youth prior to sexual initiation can result in consistent increases in condom use, even among youth whose sexual debut occurred up to three years after receipt of the primary intervention.
An intervention impact that has persisted over three years during early adolescence, a time of great change and development, is noteworthy. Few studies have examined intervention impact over such a long period and fewer have found evidence of sustained effect. In addition, the effect sizes of Cohn’s D and odds ratio observed in this study are comparable to or even greater than many reported studies in the same line of research but typically with much shorter periods of follow up. For example, a meta-analysis synthesized data from over 40 randomized controlled trials for adolescent sexual risk reduction revealed a mean effect size of Cohn’s D = 0.30 (95% CI: 0.09, 0.51) for condom use skills over 6–12 months postintervention33; however, many of the observed Cohn’s D at 36 months postintervention in the present study varied between 0.4 and 0.5.
Findings from the mediation analysis support the importance of the emphasis in FOYC on condom use self-efficacy, encouraging adolescents that they can actively protect themselves against HIV infection. Consistent with the literature presented in the Introduction,9–12 a significant component of the effect from FOYC in elevating intentions to use and actual use of condoms was mediated by changes in self-efficacy. HIV knowledge and condom use skills also played a role in mediating the intervention effect. These findings support the conclusion that theory-based educational programmes incorporating self-efficacy skills are effective.34 The absence of programme effect for FOYC/GFI on condom use (despite the positive impact on condom use self-efficacy and other variables) may be explained by the absence of a parent HIV prevention intervention and thus reduced parental reinforcement/feedback.
A further contribution of this study derives from the feedback analysis. The analytic results support our hypothesis that levels of intention and actual use of condoms during sex (logically being resulted from condom use self-efficacy) at 24 months were positively associated with condom use self-efficacy at 36 months, forming several nested positive feedback loops. In addition, condom use intention at 24 months was positively associated with condom use skills at 36 months, which was in turn correlated with HIV knowledge and self-efficacy, further strengthening the positive feedback loops. The findings from the feedback analysis strengthened the results from the mediation analysis, providing additional understanding of the mechanisms for the sustained effect from receiving FOYC.
A limitation of this study is the low Cronbach alpha values for two of the PMT constructs, severity and vulnerability. While we were pleased to be able to follow 80% of the participants at 36 months postintervention, 20% of the participants were not available and so we cannot directly assess how their presence might or might not have impacted the findings. Also, the independent effect (if any) of the booster intervention on the sustained effect could not be assessed with the current design. Finally, while this manuscript is concerned with condom use rather than other sexual risk behaviour and protective barriers, we do note a higher rate of sexual initiation among FOYC/CImPACT youth (41.5%), as compared to the control youth (30.6%, P < 0.01). As we described in detail in another manuscript,35 this difference can be explained by the significantly higher proportion of males in the FOYC/CImPACT group compared to the control group. Males in both the intervention and the control groups reported significantly higher rates of sexual initiation than females. Furthermore, as we described elsewhere,35 analyses indicated that more students in the schools with poor academic performance were assigned, by chance, to the FOYC/CImPACT group, resulting in groups of unequal risk at baseline.
In conclusion, a significant long-term programme effect of FOYC was found at 36 months postintervention. There is strong evidence for mediation and feedback effects as theoretical mechanisms supporting the programme effect. These results support the use of FOYC and CImPACT for increasing condom use as a means to prevent HIV in Caribbean nations.
Acknowledgments
This research was supported by the National Institute/National of Mental Health (R01MH069229). The Bahamas National Trust provided support for training teachers in the Wondrous Wetlands Program and provision of materials for the content of the programme. We also thank Glenda Rolle, Director, Health and Family Life Education Unit, Ministry of Education for her tireless support of this research. The NCT study registration number is NCT00774592.
APPENDIX A: PMT CONSTRUCTS WITH REGARD TO CONDOM USE FOR HIV/AIDS PREVENTION
Threat appraisal for condom use
Extrinsic reward
Of the boys you know who have sex, how many of them use condoms? (most = 5, some = 3, none = 1)
Intrinsic reward
Condoms make sex feel better (strongly agree = 1, strongly disagree = 5)
Perceived severity
How would you feel if you were to be infected with HIV? (very bad = 5, very good = 1)
How would you feel if you were to get an STD? (very bad = 5, very good = 1)
How would you feel if you were to get pregnant (or get a girl pregnant)? (very bad = 5, very good = 1)
Vulnerability
In the next six months I will become infected with HIV (very likely = 5, very unlikely = 1)
In the next six months I will get an STD (very likely = 5, very unlikely = 1)
In the next six months I will get pregnant (or I will get a girl pregnant) (very likely = 5, very unlikely = 1)
Coping appraisal for condom use
Self-efficacy
I could get condoms (strongly agree = 5, strongly disagree = 1)
I could put on a condom correctly (strongly agree = 5, strongly disagree = 1)
I could convince my sexual partner to use a condom (strongly agree = 5, strongly disagree = 1)
I could ask for condoms in a store (strongly agree = 5, strongly disagree = 1)
I could ask for condoms in a clinic (strongly agree = 5, strongly disagree = 1)
I could refuse to have sex if my partner will not use a condom (strongly agree = 5, strongly disagree = 1)
Response-efficacy
Condoms are an important way to prevent a pregnancy (strongly agree = 5, strongly disagree = 1)
Condoms are an important way to prevent you from getting an STD (strongly agree = 5, strongly disagree = 1)
Condoms are an important way to prevent you from AIDS (strongly agree = 5, strongly disagree = 1)
Response cost
If a girl carries condoms people think she is having sex (strongly agree = 5, strongly disagree = 1)
Condoms make sex hurt for a girl (strongly agree = 5, strongly disagree = 1)
Condoms take away the feelings that a guy has during sex (strongly agree = 5, strongly disagree = 1)
When a guy and a girl are in a serious relationship they do not use condoms (strongly agree = 5, strongly disagree = 1)
Youths do not want other youths to think they are using condoms (strongly agree = 5, strongly disagree = 1)
It would be difficult for a younger girl or boy to ask an older sexual partner to use a condom (strongly agree = 5, strongly disagree = 1)
APPENDIX B: ITEMS AND SCORING FOR ASSESSING HIV/AIDS KNOWLEDGE
If you touch someone with AIDS you can get AIDS (true = 1, false = 0)
What you eat can give you AIDS (true = 0, false = 1)
Anybody can get AIDS (true = 1, false = 0)
You can get AIDS from sharing needles for tattoos or piercing (true = 1, false = 0)
Using a condom during sex is a way to protect yourself from getting AIDS (true = 1, false = 0)
AIDS can be cured if treated early (true = 0, false = 1)
You can tell if someone is not infected with the AIDS virus just by looking at them (true = 0, false = 1)
Going to the bathroom after sex is one way to reduce the chance of becoming infected with the AIDS virus (true = 0, false = 1)
Taking birth control pills is one way to protect yourself from becoming infected with the AIDS virus (true = 0, false = 1)
You can get AIDS the first time you have sex (true = 1, false = 0)
You can get AIDS even if you are only having sex with one person (true = 1, false = 0)
If a condom breaks during sex, you can become infected with the HIV virus (true = 1, false = 0)
Abstinence is the best protection from AIDS (true = 1, false = 0)
Plastic wrap can be used instead of condoms to protect against HIV/AIDS (true = 0, false = 1)
Keeping in good physical shape is the best way to keep from getting AIDS (true = 0, false = 1)
A shower after sex reduces the risk of getting AIDS (true = 0, false = 1)
The AIDS virus does not go through unbroken skin (true = 1, false = 0)
A good diet and plenty of sleep will keep a person from getting AIDS (true = 0, false = 1)
APPENDIX C: ITEMS USED FOR ASSESSING CONDOM USE SKILLS
Tear along one side of the foil, being sure not to rip the condom inside (correct = 1, incorrect = 0)
Put the condom on when the penis is erect, before there is any contact between the penis and your partner’s body (correct = 1, incorrect = 0)
Squeeze the closed end of the condom between your fore-finger and the thumb and place the condom over the erect penis (correct = 1, incorrect = 0)
Unroll the condom to the base of the penis (correct = 1, incorrect = 0)
Apply a water-based lubricant (correct = 1, incorrect = 0)
Withdraw the penis while it is still erect by holding the condom firmly in place. (correct = 1, incorrect = 0)
Remove the condom (correct = 1, incorrect = 0)
Unroll condom before placing on the penis (correct = 1, incorrect = 0)
Apply oil-based lubricant (incorrect = 1, correct = 0)
Wrap the used condom back in the foil to save for next time (incorrect = 1, correct = 0)
Put the condom on any time before you ejaculate (incorrect = 1, correct = 0)
Put the condom on before the penis erect, before there is any contact between the penis and your partner’s body (incorrect = 1, correct = 0)
Unroll the closed end of the condom so that there is two inches between the end of the condom and the tip of the penis (incorrect = 1, correct = 0)
Unroll the condom to approximately three-quarters of the way down the penis (incorrect = 1, correct = 0)
Withdraw the penis after it is no longer erect by holding the condom fully in place. Remove the condom (incorrect = 1, correct = 0)
References
- 1.UNAIDS. [last accessed 12 January 2008];Uniting the world against AIDS. 2008 http://www.stopaidsnow.org/documents/WPP-Conference08-Bhatupe%20Mhango-UNAIDS.pdf.
- 2.Auerbach JD, Hayes RJ, Kandathil SM. Overview of effective and promising interventions to prevent HIV infection. World Health Organ Tech Rep Ser. 2006;938:43–78. 317–41. [PubMed] [Google Scholar]
- 3.Institute of Medicine. [last accessed 12 January 2008];Brief no time to lose: getting the most from HIV prevention. See http://www.iom.edu/file.aspid=4131.
- 4.Johnson BT, Carey MP, Marsh KL, Levin KD, Scott-Sheldon LA. Interventions to reduce sexual risk for the human immunodeficiency virus in adolescents, 1985–2000: a research synthesis. Arch Pediatr Adolesc Med. 2003;157:381–8. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- 5.Kirby D. Effective approaches to reducing adolescent unprotected sex, pregnancy, and childbearing. J Sex Res. 2002;39:51–7. doi: 10.1080/00224490209552120. [DOI] [PubMed] [Google Scholar]
- 6.Kirby D. Emerging Answers 2007: Research Findings on Programs to Reduce Teen Pregnancy and Sexually Transmitted Diseases. Washington, DC: National Campaign to Prevent Teen and Unplanned Pregnancy; 2007. [Google Scholar]
- 7.Lyles CM, Kay LS, Crepaz N, et al. Best-evidence interventions: findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. Am J Public Health. 2007;97:133–43. doi: 10.2105/AJPH.2005.076182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mullen PD, Ramirez G, Strouse D, Hedges LV, Sogolow E. Meta-analysis of the effects of behavioral HIV prevention interventions on the sexual risk behavior of sexually experienced adolescents in controlled studies in the United States. J Acquir Immune Defic Syndr. 2002;30(Suppl 1):S94–105. [PubMed] [Google Scholar]
- 9.Robin L, Dittus P, Whitaker D, et al. Behavioral interventions to reduce incidence of HIV, STD, and pregnancy among adolescents: a decade in review. J Adolesc Health. 2004;34:3–26. doi: 10.1016/s1054-139x(03)00244-1. [DOI] [PubMed] [Google Scholar]
- 10.Buhi ER, Goodson P. Predictors of adolescent sexual behavior and intention: a theory-guided systematic review. J Adolesc Health. 2007;40:4–21. doi: 10.1016/j.jadohealth.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 11.DiClemente RJ, Salazar LF, Crosby RA. A review of STD/HIV preventive interventions for adolescents: sustaining effects using an ecological approach. J Pediatric Psychol. 2007;32:888–906. doi: 10.1093/jpepsy/jsm056. [DOI] [PubMed] [Google Scholar]
- 12.Kirby DB, Baumler E, Coyle KK, et al. The “Safer Choices” intervention: its impact on the sexual behaviors of different subgroups of high school students. J Adolesc Health. 2004;35:442–52. doi: 10.1016/j.jadohealth.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Monasch R, Mahy M. Young people: the centre of the HIV epidemic. World Health Organ Tech Rep Ser. 2006;938:15–41. discussion 317–41. [PubMed] [Google Scholar]
- 14.Rangel MC, Gavin L, Reed C, Fowler MG, Lee LM. Epidemiology of HIV and AIDS among adolescents and young adults in the United States. J Adolesc Health. 2006;39:156–63. doi: 10.1016/j.jadohealth.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 15.Stephenson J, Obasi A. HIV risk-reduction in adolescents. Lancet. 2004;363:1177–8. doi: 10.1016/S0140-6736(04)15983-7. [DOI] [PubMed] [Google Scholar]
- 16.Pedlow CT, Carey MP. HIV sexual risk-reduction interventions for youth: a review and methodological critique of randomized controlled trials. Behav Modif. 2003;27:135–90. doi: 10.1177/0145445503251562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Darbes L, Crepaz N, Lyles C, Kennedy G, Rutherford G. The efficacy of behavioral interventions in reducing HIV risk behaviors and incident sexually transmitted diseases in heterosexual African Americans. AIDS. 2008;22:1177–94. doi: 10.1097/QAD.0b013e3282ff624e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet. 2008;372:669–84. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kirby D, Obasi A, Laris BA. The effectiveness of sex education and HIV education interventions in schools in developing countries. World Health Organ Tech Rep Ser. 2006;938:103–50. discussion 317–41. [PubMed] [Google Scholar]
- 20.Stanton B, Cole M, Galbraith J, et al. Randomized trial of a parent intervention: parents can make a difference in long-term adolescent risk behaviors, perceptions, and knowledge. Arch Pediatr Adolesc Med. 2004;158:947–55. doi: 10.1001/archpedi.158.10.947. [DOI] [PubMed] [Google Scholar]
- 21.Stanton BF, Li XM, Ricardo I, Galbraith J, Feigelman S, Kaljee L. A randomized, controlled effectiveness trial of an AIDS prevention program for low-income African-American youths. Arch Pediatr Adolesc Med. 1996;150:363–72. doi: 10.1001/archpedi.1996.02170290029004. [DOI] [PubMed] [Google Scholar]
- 22.Wu Y, Stanton BF, Galbraith J, et al. Sustaining and broadening intervention impact: a longitudinal randomized trial of 3 adolescent risk reduction approaches. Pediatrics. 2003;111:e32–8. doi: 10.1542/peds.111.1.e32. [DOI] [PubMed] [Google Scholar]
- 23.Chen X, Lunn S, Deveaux L, et al. A cluster randomized controlled trial of an adolescent HIV prevention program among Bahamian Youth: effect at 12 months post-intervention. AIDS Behav. 2009;13:499–508. doi: 10.1007/s10461-008-9511-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deveaux L, Stanton B, Lunn S, et al. Reduction in human immunodeficiency virus risk among youth in developing countries. Arch Pediatr Adolesc Med. 2007;161:1130–9. doi: 10.1001/archpedi.161.12.1130. [DOI] [PubMed] [Google Scholar]
- 25.Gong J, Stanton B, Lunn S, et al. Effects through 24 months of an HIV/AIDS prevention intervention program based on protection motivation theory among preadolescents in the Bahamas. Pediatrics. 2009;123:e917–28. doi: 10.1542/peds.2008-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tein JY, Sandler IN, MacKinnon DP, Wolchik SA. How did it work? Who did it work for? Mediation in the context of a moderated prevention effect for children of divorce. J Consult Clin Psychol. 2004;72:617–24. doi: 10.1037/0022-006X.72.4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bertalanffy L. General System Theory: Foundations, Development, Applications. New York: George Braziller; 1976. (revised edition) [Google Scholar]
- 28.Doyle J, Francis B, Tannenbaum A. Feedback Control Theory. New York: Dovver Pubns; 1990. [Google Scholar]
- 29.Rippetoe PA, Rogers RW. Effects of components of protection-motivation theory on adaptive and maladaptive coping with a health threat. J Pers Soc Psychol. 1987;52:596–604. doi: 10.1037//0022-3514.52.3.596. [DOI] [PubMed] [Google Scholar]
- 30.Stanton B, Black M, Feigelman S, et al. Development of a culturally, theoretically and developmentally based survey instrument for assessing risk behaviors among African-American early adolescents living in urban low-income neighborhoods. AIDS Educ Prev. 1995;7:160–77. [PubMed] [Google Scholar]
- 31.Murray DM. Design and Analysis of Group-Randomized Trials. New York/Oxford: Oxford University Press; 1998. [Google Scholar]
- 32.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 33.Johnson BT, Carey MP, Marsh KL, Levin KD, Scott-Sheldon LA. Interventions to reduce sexual risk for the human immunodeficiency virus in adolescents, 1985–2000: a research synthesis. Arch Pediatr Adolesc Med. 2003;157:381–88. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- 34.DiClemente RJ, Crittenden CP, Rose E, et al. Psychosocial predictors of HIV-associated sexual behaviors and the efficacy of prevention interventions in adolescents at-risk for HIV infection: what works and what doesn’t work? Psychosom Med. 2008;70:598–605. doi: 10.1097/PSY.0b013e3181775edb. [DOI] [PubMed] [Google Scholar]
- 35.Dinaj-Koci V, Brathwaite N, Deveaux L, et al. Assessing the effectiveness of cluster randomization when outcome events are rare at baseline. (submitted for publication) [DOI] [PMC free article] [PubMed] [Google Scholar]