Abstract
Background
There are data to suggest that anemia is associated with increased mortality in patients with chronic obstructive pulmonary disease (COPD). In contrast, critically ill patients with low hemoglobin levels (4.3–5.5 mmol/L, 7.0–9.0 g/dL) in general do not appear to have a worsened clinical outcome. The effects of anemia in critically ill patients with COPD remain to be clarified. We examined the association between anemia (hemoglobin <7.4 mmol/L, <12.0 g/dL) and 90-day mortality in COPD patients with acute respiratory failure treated with invasive mechanical ventilation in a single-institution follow-up study.
Method
We identified all COPD patients at our institution (n = 222) admitted for the first time to the intensive care unit (ICU) requiring invasive mechanical ventilation in 1994–2004. Data on patient characteristics (eg, hemoglobin, pH, blood transfusions, and Charlson Comorbidity Index), and mortality were obtained from population-based clinical and administrative registries and medical records. We used Cox’s regression analysis to estimate mortality rate ratios (MRR) in COPD patients with and without anemia.
Results
A total of 42 (18%) COPD patients were anemic at time of initiating invasive mechanical ventilation. The overall 90-day mortality among anemic COPD patients was 57.1% versus 25% in nonanemic patients. The corresponding adjusted 90-day MRR was 2.6 (95% confidence interval 1.5–4.5). Restricting analyses to patients not treated with blood transfusions during their intensive care unit stay did not materially change the MRR.
Conclusion
We found anemia to be associated with increased mortality among COPD patients with acute respiratory failure requiring invasive mechanical ventilation.
Keywords: anemia, mortality, chronic obstructive pulmonary disease, intensive care
Background
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity, disability, and mortality worldwide.1 Patients with advanced COPD are often hospitalized for acute respiratory failure and may require invasive mechanical ventilation, which is associated with high inhospital mortality rates ranging from 6% to 24%.2–9 Limited and inconsistent data exist on simple, readily available predictors of mortality in critically ill COPD patients requiring invasive mechanical ventilation. Emerging information from studies and reports describes increased morbidity and mortality in anemic patients with COPD.10–15 In contrast, studies of transfusion regimens have found that critically ill patients in the intensive care unit (ICU) appear to tolerate low hemoglobin levels (4.3–5.5 mmol/L, 7.0–9.0 g/dL), with the possible exception of patients with acute angina or myocardial infarction who appear to have improved survival if the hemoglobin is kept at a somewhat higher level (6.2–6.9 mmol/L, 10.0–11.0 g/dL).15,16 It remains uncertain to what extent anemia is associated with clinical outcome in critically ill COPD patients requiring invasive mechanical ventilation and how it should be managed.
We hypothesized that anemia was associated with increased mortality in COPD patients with acute respiratory failure treated with invasive mechanical ventilation and conducted a single-institution follow-up study to examine this hypothesis.
Methods
The study was conducted between January 1994 and December 2004 in patients admitted to the ICU at Silkeborg Hospital, Denmark. The hospital services a population of about 100,000. In Denmark, all critically ill patients are treated at public hospitals. The Danish Civil Registration System keeps electronic records on gender, date of birth, change of address, date of emigration, and changes in vital status since 1968. The records carry a unique 10-digit civil registration number, assigned at birth by the Civil Registration System, which is used in all public Danish registers, enabling unambiguous record linkage between them.
Patients with COPD
All patients admitted to the ICU were consecutively registered in a local clinical database.17 The registered data included cause of referral, main categories of disease, complications, and treatment. All patients older than 35 years admitted for the first time to our ICU with acute respiratory failure and requiring invasive mechanical ventilation were identified in the database. We only included each patient’s first admission during the study period in order to ensure independence between the events, although some patients had multiple admissions to the ICU during the study period. We reviewed all medical records of these patients to identify those with a verified diagnosis of COPD. COPD was defined according to The Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria based on pulmonary test results, if a test was performed within one year prior to ICU admission. However, the majority of patients did not have a pulmonary test performed within one year before ICU admission, thus we also had to rely on characteristic findings in the history and physical examination by the attending physician at the time of ICU admission, as is often done in studies of COPD. The decision to initiate invasive mechanical ventilation was taken by the ICU physicians treating the patient and based on departmental guidelines. Similarly, overall treatment and extubation decisions were made at the discretion of the ICU team. The ICU was staffed by the same group of consultants during the study period.
Hemoglobin, pH, and blood transfusions
We obtained data on hemoglobin levels and arterial blood gas pH taken before initiation of mechanical ventilation from the medical records. Only arterial blood gas measurements obtained six hours or less before intubation were considered relevant. All blood gas analyses were done using Radiometer ABL 3, 520, or 725 analyzers (Radiometer, Copenhagen, Denmark). We decided to make the cutoff point for anemia as set by the hospital laboratory, ie, hemoglobin <7.4 mmol/L (<12.0 g/dL) for both men and women. Three levels of hemoglobin were defined: hemoglobin <7.4 mmol/L (<12.0 g/dL, anemia); 7.4–9.3 mmol/L (12.0–15.0 g/dL, normal); hemoglobin >9.3 mmol/L (15.0 g/dL, high). Data on blood transfusions received during the ICU stay were obtained from the hospital transfusion service database.
Comorbidity
The Hospital Discharge Registry of Aarhus County contains data on all hospitalizations from nonpsychiatric hospitals in the county since 1977, including dates of admission and discharge, and up to 20 discharge diagnoses assigned by the treating physician and coded according to the International Classification of Diseases, 8th revision (ICD-8) until the end of 1993, and 10th revision (ICD-10) thereafter. We computed the comorbidity index score developed by Charlson et al18 for each patient, based on discharge diagnoses from the Discharge Registry registered before the date of ICU admission. The Charlson Comorbidity Index has previously been validated for the prediction of short-term and long-term mortality in critically ill patients.19 Diagnoses of COPD were excluded from the index because they defined our cohort.
Mortality
Complete follow-up data for death, emigration, or immigration were obtained through linkage to the Danish Civil Registration System.
Statistical analysis
Follow-up extended for 90 days after ICU admission, until death or migration, whichever came first. We analyzed data by obtaining contingency tables for cumulative mortality based on Kaplan-Meier estimates and the main study variables, ie, hemoglobin groups, pH, comorbidity, gender, and age. We used Cox’s regression analysis to compute mortality rate ratios (MRR) 90 days after ICU admission according to the three levels of hemoglobin adjusted for gender, age, Charlson Comorbidity Index score (0 [low], 1–2 [medium], and >2 [high]), and pH (<7.15, 7.15–7.30, and >7.30). Because there is no clear definition of anemia in critically ill patients, we repeated the analyses using alternative cutoff points for defining anemia, ie, hemoglobin <6.2 mmol/L (10.0 g/dL) or <5.5 mmol/L (9.0 g/dL). Furthermore, separate analyses were done according to gender and whether the patients were admitted in the early (before 1999) or later (after 1999) part of the study period.
Finally, in order to assess the impact of blood transfusion on our results, we repeated the regression analyses, including only patients who did not receive transfusion during their ICU stay. All risk estimates are presented with 95% confidence intervals (CI). All analyses were performed using the SAS version 8.2 (SAS Institute Inc. Cary, NC, USA).
Results
We identified 244 patients with COPD who required invasive mechanical ventilation. Twenty-two patients (9%) were excluded because we were unable to identify their hemoglobin or pH values measured within six hours of initiation of invasive mechanical ventilation, leaving a total of 222 patients available for analysis. There was no difference in mortality between the included and excluded patients.
The majority of patients were female (n = 122, 55%) and 148 patients (66%) were 65 years or older (Table 1). A total of 42 (18%) patients had hemoglobin values lower than 7.4 mmol/L (12.0 g/dL), 132 (60%) had hemoglobin values of 7.4–9.3 mmol/L (12.0–15.0 g/dL), and 48 patients (22%) had hemoglobin values higher than 9.3 mmol/L (15.0 g/dL). The most frequent comorbidity was cardiovascular disease, including congestive heart failure (39%) and previous acute myocardial infarction (11%).
Table 1.
Descriptive characteristics of 222 chronic obstructive pulmonary disease patients with acute respiratory failure treated with invasive mechanical ventilation admitted to Silkeborg Hospital, Denmark 1994–2004
| Hemoglobin |
|||
|---|---|---|---|
| <7.4 mmol/L (12.0 g/dL) n (%) | 7.4–9.3 mmol/L (12.0–15.0 g/dL) n (%) | >9.3 mmol/L (15.0 g/dL) n (%) | |
| Gender | |||
| Female | 20 (9.0%) | 77 (34.7%) | 25 (11.3%) |
| Male | 22 (10.0%) | 55 (25.0%) | 23 (10.4%) |
| Age (years) | |||
| <65 | 10 (4.5%) | 49 (22.1%) | 15 (6.8%) |
| 65–75 | 16 (7.2%) | 47 (21.2%) | 26 (11.7%) |
| >75 | 16 (7.2%) | 36 (16.2%) | 7 (3.2%) |
| Comorbidity levela | |||
| Low | 9 (4.1%) | 53 (23.9%) | 16 (7.2%) |
| Medium | 23 (10.4%) | 61 (27.5%) | 26 (11.7%) |
| High | 10 (4.5%) | 18 (8.1%) | 6 (2.7%) |
| pH | |||
| <7.15 | 7 (3.2%) | 29 (13.1%) | 9 (4.1%) |
| 7.15–7.30 | 14 (6.3%) | 55 (25%) | 22 (10%) |
| >7.30 | 21 (9.5%) | 48 (21.6%) | 17 (7.7%) |
Note: Three levels of the index were defined: low (Charlson Index Score), corresponding to patients with no underlying diseases implemented in the Charlson Index, medium (Charlson Index Score 1–2), and high (Charlson Index Score >2).
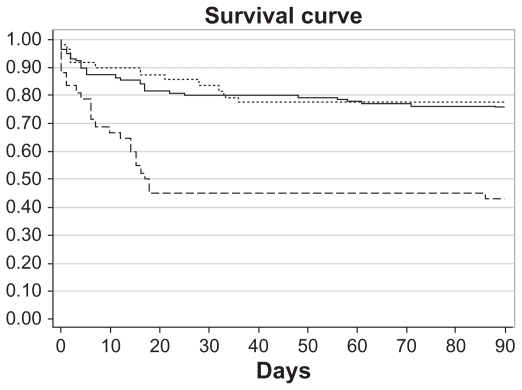
The Kaplan-Meier survival curve showed a clear diversion of the low hemoglobin group from the normal and high hemoglobin groups early after ICU admission and throughout the study period (see Figure 1).
Figure 1.
Survival curves according to hemoglobin levels at ICU admission for chronic obstructive pulmonary disease patients treated with mechanical ventilation [----Hb < 7.4 mmol/L (12.0 g/dL); — 7.4 mmol/L (12.0 g/dL) < Hb < 9.3 mmol/L (15.0 g/dL);  Hgb > 9.3 mmol/L (15.0 g/dL)].
Hgb > 9.3 mmol/L (15.0 g/dL)].
The 30-day mortality was 54.8% in COPD patients with anemia and 19.8% in those without anemia, corresponding to an adjusted MRR of 3.1 (95% CI 1.6–5.9) after adjusting for gender, age, comorbidity, and pH at ICU admission (Table 2). The 90-day mortality was 57.1% in anemic COPD patients and 25.0% in nonanemic COPD patients (adjusted MRR 2.6 [95% CI 1.5–4.5]).
Table 2.
Total numbers and relative risk (mortality rate ratio) of 30-day and 90-day mortality of 222 chronic obstructive pulmonary disease patients treated with invasive mechanical ventilation at Silkeborg Hospital, Denmark, 1994–2004
| Mortality (n) | Mortality (%) | Crude risk MRR (95% CI) | Adjusted risk MRR (95% CI)* | |
|---|---|---|---|---|
| 30 days | ||||
| Hb <7.4 mmol/L (12.0 g/dL) | 23 | 54.8 | 3.5 (1.8–6.6) | 3.1 (1.6–5.9) |
| Hb 7.4–9.3 mmol/L (12–15 g/dL) | 27 | 20.5 | 1 (Ref.) | 1 (Ref.) |
| Hb >9.3 mmol/L (15.0 g/dL) | 8 | 16.7 | 0.9 (0.4–2.1) | 1.0 (0.4–2.4) |
| 90 days | ||||
| Hb <7.4 mmol/L (12.0 g/dL) | 24 | 57.1 | 3.0 (1.8–5.2) | 2.6 (1.5–4.5) |
| Hb 7.4–9.3 mmol/L (12–15 g/dL) | 33 | 25.0 | 1 (Ref.) | 1 (Ref.) |
| Hb >9.3 mmol/L (15.0 g/dL) | 11 | 22.9 | 0.9 (0.4–1.8) | 1.1 (0.5–2.1) |
Note: Adjusted by Cox-proportional hazards regression analysis for gender, age, comorbidity, and pH at intensive care unit admission.
Abbreviations: Hb, hemoglobin; MRR, mortality rate ratios.
Defining anemia as hemoglobin below 6.2 mmol/L (10.0 g/dL) yielded adjusted 30- and 90-day MRRs of 2.36 (95% CI 0.94–5.84) and 2.42 (95% CI 1.04–5.62), respectively. When lowering the cutoff point to 5.5 mmol/L (9.0 g/dL), the adjusted 30-day and 90-day MRRs were further elevated to 7.79 (95% CI 2.42–5.01) and 6.81 (95% CI 2.14–21.70), respectively.
Furthermore, anemia was associated with higher mortality in both women (adjusted 90-day MRR 3.4 [95% CI 1.5–7.7]) and men (adjusted 90-day MRR 2.4 [95% CI 1.1–5.2]). The increased mortality associated with anemia was found both in the early adjusted 90-day MRR (3.5, 95% CI 1.6–7.5) or late adjusted 90-day MRR (3.1, 95% CI 1.4–7.2) part of the study period.
A total of 13 patients in the low hemoglobin group and 22 patients in the normal hemoglobin group had blood transfusions. Six patients received more than four units of blood. Restricting analyses to patients who did not receive blood transfusions revealed slightly increased MRRs (anemic COPD patients: adjusted 30-day MRR 3.7 [95% CI 1.9–7.0] and adjusted 90-day MRR 3.2 [95% CI 1.7–5.9]).
Discussion
In this follow-up study, including more than 200 COPD patients treated with invasive mechanical ventilation, we found that low hemoglobin levels were associated with substantially increased mortality within the first 90 days following admission. The association was found in both women and men and throughout the entire study period. Furthermore, it remained also after excluding patients who received blood transfusions, indicating that blood transfusion could not explain the increased mortality in anemic patients.
Anemia in critically ill ICU patients has been investigated in a number of studies, which demonstrate that anemia is a frequent phenomenon, and that a low hemoglobin level is well tolerated by most patients, with the possible exception of patients with ischemic heart disease.15,16 Furthermore, the use of blood transfusions in critical ill patients has been questioned because transfusions have been linked with increased mortality.15,16,20
We have not been able to identify available data on the relationship between anemia and clinical outcome specifically among critically ill COPD patients, which is a problem because a number of observational studies have found that anemia in stable patients with COPD is independently associated with increased mortality and morbidity.10–14,21 The studies are not directly comparable because different definitions of anemia have been used, but the overall pattern of lower hemoglobin levels being associated with an adverse clinical outcome is consistently found. Anemia in patients with COPD appears to be associated with older age as well as a higher Charlson Comorbidity Index and Bode index compared with nonanemic and polycythemic patients with COPD.11 Our findings support the hypothesis that the possible adverse effects of anemia/low hemoglobin levels found in stable COPD patients also exist among critically ill COPD patients requiring invasive mechanical ventilation.
The main strengths of the present study include the availability of an unselected patient population (thus reducing the risk of selection and referral bias), the availability of clinical data which had been prospectively collected during routine clinical work independently of the study hypothesis, and the complete follow-up.
We relied on clinical findings by experienced physicians for diagnosing COPD in the majority of patients, who did not have a pulmonary function test done within one year of ICU admission, as is often done in observational studies on COPD.22 Signs and symptoms of heart failure and COPD overlap, so the cause for acute respiratory failure in an emergency setting can be difficult to diagnose. Their combined presence seems common but studies on the subject are scarce.23 Any misclassification of COPD patients was unlikely to be related to hemoglobin levels, and may therefore potentially have attenuated our relative mortality estimates toward unity.
As in any observational study, our study findings may potentially have been influenced by confounding factors. We controlled for a wide range of covariates in the data analyses, including demographics, comorbidity, and level of acidosis, none of which materially changed the association found. However, we lacked more detailed data on ICU treatment, including ventilator modality, and severity of COPD including FEV1, functional capacity, nutritional condition, and home oxygen requirements. We also had no information regarding the etiology of the anemia. However, major bleeding was not a dominant cause because the majority of patients received less than four units of blood. The strict intubation policy for end-stage COPD patients in our department limited the number of these patients in our study. Still, we cannot entirely rule out the possibility that anemia was a marker of end-stage COPD, and therefore associated with increased mortality. Furthermore, a relatively large number of COPD patients was included in our study, although the statistical precision of the risk estimates was modest, in particular in the subanalyses. Finally, this was a single-institution study, and although the patient population and management practice at our ICU was probably comparable with that of many other departments in the same time period, some caution should be taken before generalizing the findings to other settings.
In conclusion, our study showed that anemia in critically ill COPD patients treated with invasive mechanical ventilation was associated with substantially increased mortality. Further studies are needed to clarify whether increasing the hemoglobin level in critically ill patients with COPD to a higher level than is presently accepted for ICU patients in general will improve outcome.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Global Initiative for Chronic Obstructive Lung Disease. Guidelines on COPD. [Accessed on Nov 23 2010]. Available at: www.goldcopd.org.
- 2.Martin TR, Lewis SW, Albert RK. The prognosis of patients with chronic obstructive pulmonary disease after hospitalization for acute respiratory failure. Chest. 1982;82:310–314. doi: 10.1378/chest.82.3.310. [DOI] [PubMed] [Google Scholar]
- 3.Gillespie DJ, March HM, Divertie MB, Meadows JA. Clinical outcome of respiratory failure in patients requiring prolonged (>24 hours) mechanical ventilation. Chest. 1986;90:364–369. doi: 10.1378/chest.90.3.364. [DOI] [PubMed] [Google Scholar]
- 4.Connors AF, Jr, Dawson NV, Thomas C, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. Am J Respir Crit Care Med. 1996;154:959–967. doi: 10.1164/ajrccm.154.4.8887592. [DOI] [PubMed] [Google Scholar]
- 5.Confalonieri M, Gorini M, Ambrosino N, Mollica C, Corrado A. Respiratory intensive care units in Italy: A national census and prospective cohort study. Thorax. 2001;56:373–378. doi: 10.1136/thorax.56.5.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seneff MG, Wagner DP, Wagner RP, Zimmerman JE, Knaus NA. Hospital and 1-year survival of patients admitted to intensive care units with acute exacerbation of chronic obstructive pulmonary disease. JAMA. 1995;274:1852–1857. [PubMed] [Google Scholar]
- 7.Afessa B, Morales IJ, Scanlon PD, Peters SG. Prognostic factors, clinical course, and hospital outcome of patients with chronic obstructive pulmonary disease admitted to an intensive care unit for acute respiratory failure. Crit Care Med. 2002;30:1610–1615. doi: 10.1097/00003246-200207000-00035. [DOI] [PubMed] [Google Scholar]
- 8.Almagro P, Calbo E, Ochoa de Echagüen A, et al. Mortality after hospitalization for COPD. Chest. 2002;121:1441–1448. doi: 10.1378/chest.121.5.1441. [DOI] [PubMed] [Google Scholar]
- 9.Piccioni P, Caria E, Bignamini E, et al. Predictors of survival in a group of patients with chronic airflow obstruction. J Clin Epidemiol. 1998;51:547–555. doi: 10.1016/s0895-4356(98)00022-5. [DOI] [PubMed] [Google Scholar]
- 10.Chambellan A, Chailleux E, Similowski T. Prognostic value of the hematocrit in patients with severe COPD receiving long-term oxygen therapy. Chest. 2005;128:1201–1208. doi: 10.1378/chest.128.3.1201. [DOI] [PubMed] [Google Scholar]
- 11.Cote C, Zilberberg M, Mody SH, Dordelly LJ, Celli B. Hemoglobin level and its clinical impact in a cohort of patients with COPD. Eur Respir J. 2007;29:923–929. doi: 10.1183/09031936.00137106. [DOI] [PubMed] [Google Scholar]
- 12.Halpern MT, Zilberberg MD, Schmier JK, Lau EC, Shorr AF. Anemia, cost and mortality in chronic obstructive pulmonary disease. Cost Effect Res Alloc. 2006;4:17. doi: 10.1186/1478-7547-4-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zilberberg MD, Stern L, Wiederkehr DP, Doyle JJ, Shorr AF. Anemia, transfusion and hospital outcomes among critically ill patients on prolonged acute mechanical ventilation: A retrospective cohort study. Crit Care. 2008;12:R60. doi: 10.1186/cc6885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Upchurch GR, Jr, Proctor MC, Henke PK, et al. Predictors of severe morbidity and death after elective abdominal aortic aneurysmectomy in patients with chronic obstructive pulmonary disease. J Vasc Surg. 2003;37:594–599. doi: 10.1067/mva.2003.22. [DOI] [PubMed] [Google Scholar]
- 15.Hébert P, Wells G, Blajchman M, et al. A multicenter randomized controlled clinical trial of transfusion requirements in critical care. NEJM. 1999;340:409–417. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- 16.Corwin HL, Gettinger A, Pearl RG, et al. The CRIT study: Anemia and blood transfusion in the critically ill – current clinical practice in the United States. Crit Care Med. 2004;32:39–52. doi: 10.1097/01.CCM.0000104112.34142.79. [DOI] [PubMed] [Google Scholar]
- 17.Christensen S, Rasmussen L, Horváth-Puho E, et al. Arterial blood gas derangement and level of comorbidity are not predictors of long-term mortality of COPD patients treated with mechanical ventilation. Eur J Anaesthesiol. 2008;25:550–556. doi: 10.1017/S0265021508004225. [DOI] [PubMed] [Google Scholar]
- 18.Charlson M, Pompei P, Ales K, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1986;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Poses RM, McClish DK, Smith WR, Bekes C, Scott WE. Prediction of survival of critical ill patients by admission comorbidity. J Clin Epidemiol. 1996;49:743–747. doi: 10.1016/0895-4356(96)00021-2. [DOI] [PubMed] [Google Scholar]
- 20.Vincent JL, Baron JF, Reinhart K, et al. Anemia and blood transfusion in critically ill patients. JAMA. 2002;288:1499–1507. doi: 10.1001/jama.288.12.1499. [DOI] [PubMed] [Google Scholar]
- 21.Reade MC, Weissgeld L, Angus DC, Kellum JA, Milbrandt EB. The prevalence of anemia and its association with 90-day mortality in hospitalized community-acquired pneumonia. BMC Pulm Med. 2010;10:15. doi: 10.1186/1471-2466-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nevins ML, Epstein SK. Predictors of outcome for patients with COPD requiring invasive mechanical ventilation. Chest. 2001;119:1840–1849. doi: 10.1378/chest.119.6.1840. [DOI] [PubMed] [Google Scholar]
- 23.Rutten FH, Cramer MJ, Lammers SW, Grobbee DE, Hoes AW. Heart failure and chronic Obstructive pulmonary disease: An ignored combination. Eur J Heart Fail. 2006;8:706–711. doi: 10.1016/j.ejheart.2006.01.010. [DOI] [PubMed] [Google Scholar]