Abstract
Objective
Describe a case of secondary infertility due to the development of severe Asherman Syndrome after the B-Lynch compression suture and uterine artery ligation, and to review the B-Lynch technique and documented complications.
Design
Case report.
Setting
Tertiary care hospital.
Patient(s)
A 29-year-old primigravida patient.
Intervention(s)
B-Lynch suture and uterine artery ligation.
Main Outcome Measure(s)
Development of Asherman syndrome.
Result(s)
Development of secondary infertility due to Asherman syndrome after the B-Lynch suture.
Conclusion(s)
The B-Lynch suture is a highly successful conservative surgical technique used to treat this condition. There is little information regarding any potential for compromised future fertility, although there have been several reports of successful pregnancy after the use of the B-Lynch compression suture. In this report, we present a case of Asherman syndrome with complete obliteration of the uterine cavity after the B-Lynch suture.
Keywords: Asherman syndrome, B-Lynch technique, complication, postpartum hemorrhage, secondary infertility, uterine atony
Uterine atony, or failure of the uterus to contract adequately after childbirth, is the most common cause of postpartum hemorrhage (PPH) (1). The options for managing uterine atony are described in Table 1. Definitive surgical management of PPH with hysterectomy results in complete inability to host a future pregnancy. Conservative surgical management using uterine artery ligation, with the goal of preserving uterine function, was first described in 1966 by O’Leary. Many modifications and combinations of techniques have since been made (2, 3).
TABLE 1.
Summary of management options for postpartum hemorrhage.
| Medical therapy | Uterine conservation surgery | Definitive surgical management |
|---|---|---|
| Oxytocics | Artery ligation | Hysterectomy |
| Oxytocin (12) | Uterine artery ligation (16) | Subtotal (19) |
| PG-F2α (carboprost tromethamine) (13) | Hypogastric artery ligation (17) | Total (20) |
| Methylergonovine (14) | Utero-ovarian ligament (18) | |
| PG-E1 (misoprostol) (15) | Ovarian suspensory ligament (18) | |
| Compression sutures | ||
| B-Lynch technique (4) | ||
| Hayman technique (2) | ||
| Cho technique (3) |
A compression suture technique was first described by B-Lynch and Cowen in 1997 (4). Subsequent clinical studies have shown that the response to the B-Lynch suture technique is complete and recovery uneventful (5–7). There is little information regarding any potential for compromised future fertility, although there have been several reports of successful pregnancy after the use of the B-Lynch compression suture (8–11).
The objective of the present report is to describe a case of secondary infertility due to the development of severe Asherman syndrome after a B-Lynch compression suture and uterine artery ligation.
B-LYNCH SUTURE CASE REPORT
A healthy 29-year-old primigravida woman presented to Labour and Delivery at 39 weeks 4 days gestation in spontaneous active labor. She received an epidural anesthesia and underwent artificial rupture of membranes for meconium-stained amniotic fluid. Her labor progressed slowly and she required augmentation with IV oxytocin. Despite adequate contractions, she was diagnosed with labor dystocia, and an urgent lower-segment cesarean section was performed.
Aviable male infant, 3,813 grams, was delivered in direct occiput posterior position without difficulty. The placenta was delivered manually and was intact on examination. After delivery of the infant, the third stage of labor was managed actively with a bolus of 5 U oxytocin intravenously. Twenty units of oxytocin was added to 1 L of intravenous normal saline and titrated to vaginal flow. An extension of the uterine incision into the right parametrium was observed, extending inferiorly toward the cervix. The extension was repaired with a running locked chromic #1 suture, and the transverse incision was closed in two layers with #1 chromic suture in the usual fashion (21).
Uterine atony was diagnosed and medical management, including IM and IV oxytocin, initiated. A summary of the total dosage of subsequent medications used is described in Table 2.
TABLE 2.
Total uterotonic medications administered.
| Medication | Dosage |
|---|---|
| PG-F2α | 250 μg IM × 2 |
| Methylergonovine | 125 μg IM × 2 |
| PG-E1 | 800 μg PR × 1 |
The uterus remained atonic despite medical therapy. An intraoperative consultation was obtained from a second obstetrician. The patient developed hypotension and tachycardia and was resuscitated with IV crystalloid and colloid solutions. Initial laboratory investigations revealed no disseminated intravascular coagulopathy, hemoglobin of 103 mg/dL, and platelets of 142 (109/L).
Bilateral uterine artery ligation was performed with a 2-0 vicryl suture. The patient’s response was minimal with ongoing bleeding. A B-Lynch compression suture was then applied (Fig. 1). The uterus remained well compressed once the sutures were placed. A digital vaginal exam confirmed the cervix was patent. The patient was hemodynamically stable throughout the procedure and remained in the obstetrical observation unit for 24 hours. Total estimated blood loss was 2,000 mL.
FIGURE 1.
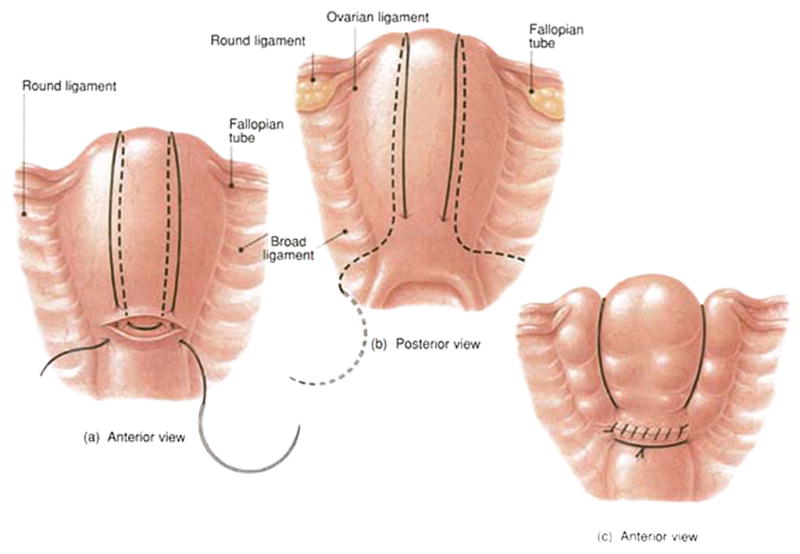
Illustration of B-Lynch suture. Reproduced with permission from B-Lynch et al. Br J Obstet Gynaecol 1997;104:372–5
The patient’s postoperative hemoglobin was 64 mg/dL. She was asymptomatic for anemia and was hemodynamically stable. A blood transfusion was declined. There was no evidence of postpartum infection. The remainder of the patient’s postoperative course was unremarkable. She was able to breastfeed successfully and was discharged on postoperative day 5.
The patient presented to a gynecologist 2 years later with secondary amenorrhea and infertility. During hysterosalpingography, the uterus could not be opacified. Extensive intrauterine adhesions were demonstrated at subsequent hysteroscopy. Severe Asherman syndrome was diagnosed and a concurrent laparoscopy revealed severe pelvic adhesive disease. The right adnexa could not be visualized, although the left tube and ovary appeared to be normal.
The patient was referred to a reproductive endocrinology and infertility specialist. A detailed history revealed cyclic moliminal symptoms, despite amenorrhea. She denied symptoms of ovarian failure, polycystic ovary syndrome, thyroid dysfunction, or hyper-prolactinemia. Laboratory investigations were normal (Table 3).
TABLE 3.
Hormone profile results (day 3).
| FSH | 5.9 U/L |
| LH | 2.8 U/L |
| E2 | 80 pmol/L |
A pelvic ultrasound examination showed that the uterus was of normal size, although it was slightly distorted in shape. Both ovaries were easily visualized and were of normal size, shape, and follicle population. Scars from the B-Lynch sutures were visible on the anterior fundus. Collagen reactions from the sutures were also visible within the myometrium (Fig. 2). There was no obvious endometrial tissue or cavity.
FIGURE 2.
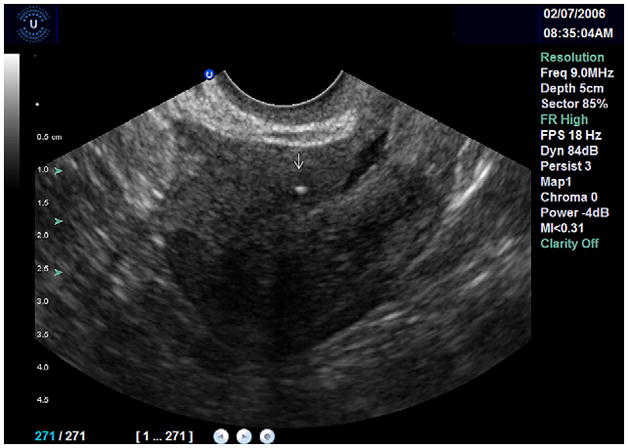
Ultrasound image of the uterus in saggital plane. The cervix is to the right of the image and the fundus is seen to the left. Collagen reaction from B-Lynch suture visible within myometrium (arrow).
The uterine arteries were located with color flow Doppler ultrasonography and measured. The uterine artery diameter was <1.0 mm bilaterally (Fig. 3). The average diameter of the uterine artery in nonpregnant women is 1.4 ± 0.1 mm (22). Kurjak and Kupesic (23) have analyzed uterine and ovarian perfusion with transvaginal Doppler studies of the uterine, ovarian, and spiral arteries and demonstrated that blood flow impedence is best expressed as resistance index (RI). The mean RI of the uterine artery in normal women during the proliferative phase is 0.88 and during the luteal phase 0.84. The right uterine artery RI could not be measured, but the left uterine artery RI was reduced to 0.31. This is attributed to decreased diameter of the vessel.
FIGURE 3.
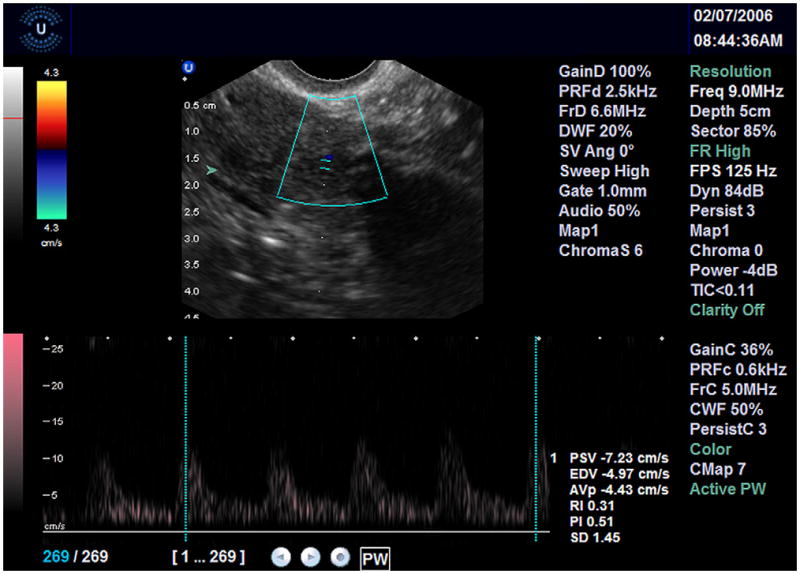
Uterine artery located with Doppler and measured ultrasound. Uterine artery diameter <50% of normal value bilaterally.
Doppler examination of the endometrial cavity revealed minimal capillary flow around the endometrium (Fig. 4). The spiral arteries were not well visualized, owing to poor endometrial perfusion. Spiral arteries are normally visualized at the level of the myometrial-endometrial junction. Normal spiral artery RI in premenopausal women is 0.64 in the proliferative phase and 0.50 in the luteal phase (23). In the initial studies of uterine blood flow, signals were unable to be obtained from the periphery of the endometrium if the patient was >6 years postmenopausal. Inability to visualize the spiral arteries was attributed to the lower estrogen environment of menopause and does not explain the finding of minimal endometrial perfusion.
FIGURE 4.
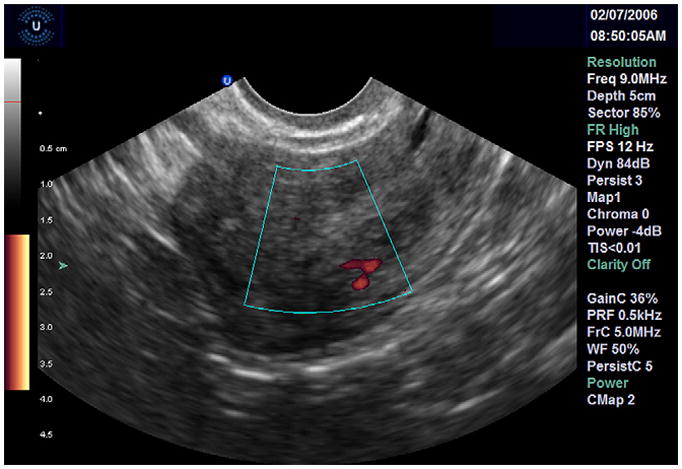
Doppler ultrasound examination of endometrial cavity. Minimal perfusion to endometrium.
A diagnosis of Asherman syndrome was made and deemed to be secondary to uterine devascularization from the B-Lynch suture and/or uterine artery ligation. Resection of intrauterine adhesions was not determined to be feasible, given the lack of blood flow to the endometrial cavity.
DISCUSSION
Severe PPH is a leading cause of maternal death worldwide (24). Uterine atony is the most common cause of PPH. The first-line treatment is the use of uterotonic agents with or without tamponade techniques (intrauterine packing, foley catheter, etc.). When these measures fail to control bleeding, conservative surgical options should be considered (25).
The B-Lynch surgical technique for the conservative surgical management of massive PPH has been used successfully since 1997 in cases where bleeding was secondary to uterine atony with failed conservative medical management. The procedure allows for conservation of the uterus for subsequent menstrual function and pregnancies (26). It is particularly useful because of its simplicity of application, life-saving potential, and relative safety (27), and it is generally considered to be effective and free of short- and long-term complications.
The standard B-Lynch suture technique was described in 1997 (Fig. 1). It was applied successfully in five cases in the original report without apparent complications (28). Briefly, a large Mayo needle with #2 chromic catgut is used to enter and exit the uterus in the lateral lower anterior segment. The stitch is looped over the fundus, taken across the posterior lower segment, then looped back over the fundus and anchored by entering the lateral lower anterior uterine segment opposite and parallel to the initial bite. The free ends are tied down securely to compress the uterus (7). The original B-Lynch technique required a hysterotomy to allow exploration of the uterine cavity, exclude retained products of conception, evacuate large blood clots, and diagnose abnormal placentation, decidual tears, damage, and bleeding (29). Modifications to the original B-Lynch compression technique have been made, including the Hayman compression suture (2) and Cho square suture technique (3).
The success rate of the B-Lynch suture, defined as avoiding hysterectomy, is 86.4% (30), and the procedure has become widely recommended to control PPH (25). However, success as defined by preservation of the uterus and fertility is more difficult to establish. There have been only isolated reports of successful subsequent pregnancies (8–10). Seven uneventful pregnancies after uterine compression sutures were reported in the largest review (30). The authors concluded that uterine compression sutures for severe post-partum hemorrhage may obviate the need for hysterectomy and do not appear to jeopardize subsequent pregnancy.
Isolated complications of conservative surgical management for PPH, including compression and ligation techniques, have been reported. The Cho method has been associated with uterine cavity synechiae (Asherman syndrome) and pyometra (33, 34). Wu and Yeh (33) described a patient who developed menstrual irregularities secondary to intrauterine synechiae after placement of the Cho compression suture. Hysteroscopic resection of adhesions was required to restore the uterine cavity. Akoury and Sherman (34) commented on a patient who required both B-Lynch and Cho compression sutures. Uterine synechiae developed early in the postoperative period, and were subsequently resected hysteroscopically. After the patient carried a full-term pregnancy 1 year later, an area of full-thickness myometrial necrosis was noted, which required operative resection. The authors hypothesized that pressure produced by the compression sutures may have caused progressive myometrial necrosis. Partial ischemic necrosis of the uterus has also been described (35–37). Treloar et al (37) reported the development of uterine necrosis, which presented three weeks into the postpartum period, after B-Lynch suture placement. A hysterectomy for persistent symptoms was ultimately required 2 months postpartum. B-Lynch suture erosion through the uterine wall at 6 weeks postpartum has also been reported (35), attributed to the use of delayed-absorbable suture.
In this report, we present a case of Asherman syndrome with complete obliteration of the uterine cavity after the B-Lynch suture. The present report adds debate to the impact of this procedure on fertility potential. The concomitant uterine artery ligation performed in this case may appear to confound the development of reduced fertility potential; however, isolated bilateral uterine artery ligation for PPH has not been shown to compromise women’s subsequent fertility and obstetrical outcome (39).
The B-Lynch suture is very successful in preventing the need for hysterectomy during intractable PPH unresponsive to medical management. However, the effects of the B-Lynch suture on future fertility potential require further investigation. There is difficulty following fertility outcomes in the cohort of patients who have received B-Lynch sutures. Many do not desire future pregnancy, possibly owing to fear of recurring PPH. We agree with a proposed national registry, developed to document successes, failures, and short- and long-term consequences of compression sutures (37). Although isolated case reports of successful pregnancies are reassuring, patients and physicians need to be aware of the potential for complications. Informing the patients of the possible outcomes will allow them to seek fertility assessment and assistance early if the couple is having difficulty conceiving.
Footnotes
C.G. has nothing to disclose. A.C. has nothing to disclose. R.P. has nothing to disclose.
Presented as a poster at the Canadian Fertility and Andrology Society Annual Clinical Meeting, Ottawa, Canada, November 2006: Goojha CA, Case AM, Baerwald AR, Pierson RA. B Lynch suture: a fertility preserving procedure?
References
- 1.Khan KS, Wojclyle D, Say L, Gulmazoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;267:1066–74. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 2.Hayman RG, Arulkumaran S, Steer PJ. Uterine compression sutures: surgical management of postpartum hemorrhage. Obstet Gynecol. 2002;99:502–6. doi: 10.1016/s0029-7844(01)01643-x. [DOI] [PubMed] [Google Scholar]
- 3.Cho JH, Jun HS, Lee CN. Hemostatic suturing technique for uterine bleeding during cesarean delivery. Obstet Gynecol. 2000;96:129–31. doi: 10.1016/s0029-7844(00)00852-8. [DOI] [PubMed] [Google Scholar]
- 4.B-Lynch C, Cowen MJ. A new nonradical surgical treatment of massive postpartum hemorrhage. Con-temp Rev Obstet Gynaecol. 1997:19–24. [Google Scholar]
- 5.B-Lynch C, Coker A, Lawal AH, Abu J, Cowen MJ. B-Lynch surgical technique for the control of massive postpartum haemorrhage: an alternative to hysterectomy? Five cases reported. Br J Obstet Gynaecol. 1997;194:372–5. doi: 10.1111/j.1471-0528.1997.tb11471.x. [DOI] [PubMed] [Google Scholar]
- 6.Pal M, Biswas AK, Bhattacharya SM. B-Lynch brace suturing in primary post-partum hemorrhage during caesarean section. J Obstet Gynaecol Res. 2003;29:317–20. doi: 10.1046/j.1341-8076.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- 7.Smith KL, Baskett TF. Uterine compression sutures as an alternative to hysterectomy for severe postpartum hemorrhage. J Obstet Gynaecol Can. 2003;25:197–200. doi: 10.1016/s1701-2163(16)30106-2. [DOI] [PubMed] [Google Scholar]
- 8.Habek D, Vranjes M, Bobic Vukovic J, Krcmar V, Simunac J. Successful term pregnancy after B-Lynch compression suture in a previous pregnancy on account of massive primary postpartum hemorrhage. Fetal Diagn Ther. 2006;21(5):475–6. doi: 10.1159/000093892. [DOI] [PubMed] [Google Scholar]
- 9.Api M, Api O, Yayla M. Fertility after B-Lynch suture and hypogastric artery ligation. Fertil Steril. 2005;84:509, e5–9. doi: 10.1016/j.fertnstert.2005.01.140. [DOI] [PubMed] [Google Scholar]
- 10.Sentilhes L, Gromez A, Trichot C, Ricbourg-Schneider A, Descamps P, Marpeau L. Fertility after B-Lynch suture and stepwise uterine devascularization. Fertil Steril. 2009;91:934, e5–9. doi: 10.1016/j.fertnstert.2008.09.082. [DOI] [PubMed] [Google Scholar]
- 11.Ferguson JE, Bourgeois FJ, Underwood PB. B-Lynch suture for postpartum hemorrhage. Obstet Gynecol. 2000;95(6 Pt 2):1020–2. doi: 10.1016/s0029-7844(99)00590-6. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham FG, Hauth JC, Leveno KJ, Gilstrap L, Bloom SL, Wenstrom KD, editors. Williams obstetrics. 22. New York: McGraw-Hill Medical; 2005. Obstetrical hemorrhage. [Google Scholar]
- 13.Oleen MA, Mariano JP. Controlling refractory atonic postpartum hemorrhage with Hemabate sterile solution. Am J Obstet Gynecol. 1990;162:205–8. doi: 10.1016/0002-9378(90)90851-w. [DOI] [PubMed] [Google Scholar]
- 14.De Groot AN, van Dongen PW, Vree TB, Hekster YA, van Roosmalen J. Ergot alkaloids. Current status and review of clinical pharmacology and therapeutic use compared with other oxytocics in obstetrics and gynecology. Drugs. 1998;56:523–35. doi: 10.2165/00003495-199856040-00002. [DOI] [PubMed] [Google Scholar]
- 15.Abdel-Aleem H, El-Nashar I, Abdel-Aleem A. Management of severe postpartum hemorrhage with misoprostol. Int J Gynecol Obstet. 2001;72:75–6. doi: 10.1016/s0020-7292(00)00321-0. [DOI] [PubMed] [Google Scholar]
- 16.O’Leary JL, O’Leary JA. Uterine artery ligation in the control of intractable postpartum hemorrhage. Am J Obstet Gynecol. 1966;94:920–4. doi: 10.1016/0002-9378(66)90026-3. [DOI] [PubMed] [Google Scholar]
- 17.Burchell RC. Internal artery ligation. Lancet. 1964;84:97–9. [PubMed] [Google Scholar]
- 18.AbdRabbo SA. Stepwise uterine devascularisation: a novel technique for management of uncontrolled postpartum hemorrhage with preservation of the uterus. Am J Obstet Gynecol. 1994;171:694–700. doi: 10.1016/0002-9378(94)90084-1. [DOI] [PubMed] [Google Scholar]
- 19.Langdana F, Geary M, Haw W, Keane D. Peripartum hysterectomy in the 1990s: any new lessons? J Obstet Gynaecol. 2001;21:121–3. doi: 10.1080/01443610020025976. [DOI] [PubMed] [Google Scholar]
- 20.Jones HW III, editor. Te Linde’s operative gynecology. 10. New York: Lippincott-Raven; 1997. Abdominal hysterectomy; pp. 727–43. [Google Scholar]
- 21.Oxorn H. Human labor and birth. 5. Connecticut: Appleton-Century-Crofts; 1986. Cesarean section; pp. 791–820. [Google Scholar]
- 22.Palmer S, Zamudio S, Coffin C, Parker S, Stamm E, Moore LG. Quantitative estimation of human uterine artery blood flow and pelvic blood flow redistribution in pregnancy. Obstet Gynecol. 1992;80:1000. [PubMed] [Google Scholar]
- 23.Kurjak A, Kupesic S. Ovarian senescence and its significance on uterine and ovarian perfusion. Fertil Steril. 1995;64:532. doi: 10.1016/s0015-0282(16)57788-7. [DOI] [PubMed] [Google Scholar]
- 24.Abou Zhar C. Global burden or maternal death and disability. Br Med Bull. 2003;67:1–11. doi: 10.1093/bmb/ldg015. [DOI] [PubMed] [Google Scholar]
- 25.American Congress of Obstetricians and Gynecologists. ACOG practice bulletin. Clinical management guidelines for obstetrician-gynecologists. No. 76. Oct. 2006: postpartum hemorrhage. Compend Select Pub. 2007:843–51. [Google Scholar]
- 26.Tsitlakidis C, Alalade A, Danso D, B-Lynch C. Ten year follow up of effect of the B-Lynch uterine compression suture for massive postpartum hemorrhage. Int J Fertil Womens Med. 2006;51:262–5. [PubMed] [Google Scholar]
- 27.Price N, B-Lynch C. Technical description of the B-Lynch brace suture for treatment of massive postpartum hemorrhage and review of published cases. Int J Fertil Womens Med. 2005;50:148–63. [PubMed] [Google Scholar]
- 28.B-Lynch C, Coker A, Lawal AH, Abu J, Cowen MJ. The B-Lynch surgical technique for the control of massive postpartum hemorrhage: an alternative to hysterectomy? Five cases reported. Br J Obstet Gynaecol. 1997;104:372–5. doi: 10.1111/j.1471-0528.1997.tb11471.x. [DOI] [PubMed] [Google Scholar]
- 29.B-Lynch C, Louis K, Lalonde A, Mahantesh K. A textbook of postpartum hemorrhage: a comprehensive guide to evaluation, management, and surgical intervention. 2006. [Google Scholar]
- 30.Baskett TF. Uterine compression sutures for postpartum hemorrhage. Obstet Gynecol. 2007;110:68–71. doi: 10.1097/01.AOG.0000267499.40531.a4. [DOI] [PubMed] [Google Scholar]
- 31.American Congress of Obstetricians and Gynecologists. ACOG practice bulletin. Clinical Management Guidelines for Obstetrician-Gynecologists. No. 76. Oct. 2006: postpartum hemorrhage. Obstet Gynecol. 2006;108:1039–47. doi: 10.1097/00006250-200610000-00046. [DOI] [PubMed] [Google Scholar]
- 32.Sentilhes L, Gromez A, Trichot C, Ricbourg-Schneider A, Descamps P, Marpeau L. Fertility after B-Lynch suture and stepwise uterine devascularization. Fertil Steril. 2009;91:934. doi: 10.1016/j.fertnstert.2008.09.082. [DOI] [PubMed] [Google Scholar]
- 33.Wu H, Yeh GP. Uterine cavity synechiae after haemostatic square suturing technique. Obstet Gynecol. 2005;105:1176–8. doi: 10.1097/01.AOG.0000159978.26472.a4. [DOI] [PubMed] [Google Scholar]
- 34.Akoury H, Sherman C. Uterine wall partial necrosis following combined B-Lynch and Cho square sutures for the treatment of primary postpartum hemorrhage. J Obstet Gynaecol Can. 2008;30:421–4. doi: 10.1016/s1701-2163(16)32827-4. [DOI] [PubMed] [Google Scholar]
- 35.Ochoa M, Allaire AD, Stitely ML. Pyometria after hemostatic square suture technique. Obstet Gynecol. 2002;99:506–9. doi: 10.1016/s0029-7844(01)01712-4. [DOI] [PubMed] [Google Scholar]
- 36.Joshi VM, Shrivastava M. Partial ischemic necrosis of the uterus following uterine brace compression suture. BJOG. 2004;111:279–80. doi: 10.1111/j.1471-0528.2004.00056.x. [DOI] [PubMed] [Google Scholar]
- 37.Treloar EJ, Anderson RS, Andrews HS, Bailey JL. Uterine necrosis following B-Lynch suture for primary postpartum haemorrhage. BJOG. 2006;113:486–8. doi: 10.1111/j.1471-0528.2006.00890.x. [DOI] [PubMed] [Google Scholar]
- 38.Grotegut CA, Larsen FW, Jones MR, Livingston E. Erosion of a B-Lynch suture through the uterine wall: a case report. J Reprod Med. 2004;49:849–52. [PubMed] [Google Scholar]
- 39.Sentilhes L, Trichot C, Resch B, Sergent F, Roman H, Marpeau L, Verspuck E. Fertility and pregnancy outcomes following uterine devascularisation for severe postpartum haemorrhage. Human Reproduction. 2008;23:1087–92. doi: 10.1093/humrep/den049. [DOI] [PubMed] [Google Scholar]


