Abstract
The US Indian health system utilizes a diverse range of health information technology and innovative tools to enhance health service delivery for American Indians and Alaska Natives. This article provides an overview of efforts and experience using such tools to achieve health equity for American Indian and Alaska Native communities. Specific attention is given to the Indian Health Service Electronic Health Record and to two examples of telehealth innovation.
Keywords: Indian Health Service, American Indians, Alaska Natives, telehealth
Introduction
The mission of the Indian Health Service (IHS) is to raise the physical, mental, social, and spiritual health of American Indians and Alaska Natives to the highest level. The IHS realizes this mission by providing comprehensive, culturally acceptable personal and public health services that are available and accessible to all federally recognized American Indian and Alaska Native people. The IHS foundation is designed to uphold the federal government's obligation to promote healthy American Indian and Alaska Native people, communities, and cultures, and to honor and protect the inherent sovereign rights of Tribes.
The IHS is the principal federal healthcare provider and health advocate for American Indian people, providing a comprehensive health service delivery system for approximately 1.9 million American Indians and Alaska Natives who belong to 564 federally recognized Tribes in 35 states. Approximately 57 percent of American Indians and Alaska Natives living in the United States rely on the IHS to provide access to healthcare services through a network of 45 hospitals and more than 600 other facilities operated by the IHS, Tribes, and Alaska Native corporations.
Although American Indian and Alaska Native people have long experienced lower health status when compared with other Americans, noteworthy improvements have been made in recent decades. For example, mortality rates resulting from unintentional injuries, homicides, alcohol-related deaths, and tuberculosis significantly decreased.1 Despite these improvements, disparities in access to care, preventable morbidity and mortality, and the burden of chronic disease persist. As evidence, the prevalence of heart disease, diabetes, and other conditions is considerably higher among American Indian and Alaska Natives compared with the rest of the US population.2 American Indians and Alaska Natives continue to die at higher rates than other Americans from tuberculosis (500 percent higher), alcoholism (519 percent higher), diabetes (195 percent higher), unintentional injuries (149 percent higher), homicide (92 percent higher), and suicide (72 percent higher).3
Bridging the Gap: The Role of Health Information Technology
Given persistent health status disparities, innovation in care delivery systems and models is a vital priority within Indian healthcare. Health information technology (HIT), in particular, is a key component of the expanded focus within Indian healthcare on effective quality health delivery and efficient resource management. Working in partnership with Tribes and Tribal programs, the IHS has emphasized the timely and strategic use of health information technology and system delivery innovation to support and address the preventive and treatment needs of American Indian and Alaska Native patients and communities. Electronic health records and telehealth service delivery are two noteworthy examples of this emphasis. These tools advance the long-standing focus within Indian health on comprehensive services for American Indian and Alaska Natives from birth to old age. They are also a critical component of initiatives supporting true patient-centered care within a community orientation and population health perspective.
The IHS Electronic Health Record
The Resource and Patient Management System (RPMS) is the IHS enterprise health information system. More than 25 years ago, RPMS began as an essential tool to provide early sentinel awareness of diarrheal outbreaks in remote communities. Since that inception, individual and aggregate data gathered through RPMS have been used to provide critical information from patient, provider, population, and community perspectives.
RPMS is based on a standard architecture that incorporates government and industry standards for the collection, processing, and transmission of information. It consists of more than 60 software applications that reflect the continuum of care provided within the Indian health system. Available through a user-friendly graphical user interface known as the RPMS Electronic Health Record (http://www.ehr.ihs.gov), this integrated HIT system is used at approximately 400 IHS, Tribal, and urban Indian health locations across the country.4
RPMS applications support direct clinical care (in medical and behavioral health settings), case management, population and public health, and clinical quality reporting. The suite of applications also includes practice management and revenue cycle capabilities. The RPMS is also a critical component of the IHS Improving Patient Care initiative. This business process redesign is predicated on rapid-cycle innovation; RPMS is used to implement as well as evaluate the outcomes of these changes. Since 2000, facilities have used RPMS to electronically aggregate and evaluate clinical quality, as well as population and public health status, in both planned and ad hoc manners.
The RPMS EHR exemplifies the IHS commitment to a community-oriented primary care delivery model. This unique approach to HIT continues with groundbreaking work in community and population HIT solutions, novel outcome perspectives (such as patient wellness summaries), development and inclusion of nontraditional standardized data fields, ad hoc community- and population-based reports, customizable interfaces, and the ability to meet requirements for meaningful use, interoperability, and data sharing. Considered together, these HIT pursuits are consistent with an integrated healthcare system committed to improving the health status of individuals, communities, and populations.
Telehealth
Telehealth tools enhance timely consultation, diagnosis, and treatment. They support best-practice approaches to care. They enable new “connected care” models of service that emphasize relationships and communication while facilitating improved healthcare quality, cost-effectiveness, and value.
Two telehealth solutions typify the IHS commitment to service delivery innovation: the Alaska Federal Health Care Access Network solution and the IHS Joslin Vision Network tele-ophthalmology program. Both of these solutions are powerful examples of the ability of telehealth services to improve health equity.
The Alaska Federal Health Care Access Network
Healthcare disparities in Alaska are affected by the state's large land mass, low population density, and shortage of healthcare providers. As per the 2000 US Census, the population density of 1.1 persons per square mile is 70 times less than the national average, and 75 percent of Alaskan communities are not connected to a hospital by a road. Alaska is 48th among the states in the ratio of doctors to residents, and the proportion of specialists to primary care providers is much lower than the national average.5 Consequently, Alaskans have limited access to medical care, with fewer physicians to offer care, fewer specialists for difficult problems, and great barriers in distance, time, and expense for in-person encounters between patients and clinicians. While this situation affects all Alaskans, it reaches crisis levels for the 130,000 Alaska Natives. With rates of suicide, trauma, diabetes, colon cancer, middle ear disease, and pulmonary disease markedly higher than those of the non-Alaska Native populations, and even less access to medical care providers than fellow Alaskans, the care disparity for the Alaska Native community is a dire problem.6
Fortunately, the same reasons for limited access to care are strong reasons to use telehealth. Telehealth tools are able to effectively bridge time and distance, helping maximize the productivity and efficiency of available healthcare providers. In recent years, Alaska has benefited from federal funding to provide the infrastructure and initial equipment needed for telehealth. Due to challenges in telecommunication connectivity, this funding was targeted toward store-and-forward (i.e., asynchronous) telehealth system development, rather than live videoconferencing. As a result, Alaska has gained considerable experience in the use of store-and-forward telehealth solutions, including the ability of such tools to address healthcare disparities. This experience is well documented in the Alaska Tribal Health System (ATHS).
The Alaska Federal Health Care Access Network (AFHCAN) telehealth solution has been operational since 2001 and provides telehealth services to 248 sites across Alaska. In the past decade, more than 70,000 telehealth cases have been created within ATHS alone, for both primary and specialty care. AFHCAN has been active in collecting data from this diverse telehealth activity, with particular attention to how the use of telehealth has affected care delivery for Alaska Natives.
Store-and-forward telehealth has improved access to care, reduced the cost of care delivery, and improved the efficiency and productivity of providers. The experience of ear, nose, and throat (ENT) services is an important example. A 16-year review of patients referred to an ENT specialty clinic in Nome, Alaska, has shown that using store-and-forward telehealth via AFHCAN reduces waiting times for patients to see an ENT specialist at a field clinic. Prior to telehealth, over a 10-year period, 48 percent of all patients in Nome and surrounding communities waited at least five months to see a specialist. Now, after using telehealth for six years, waiting times have been dramatically reduced, and only 3 percent of all patients wait more than four months to see a specialist.7
Another ENT project involved the use of a traveling audiologist. Store-and-forward telehealth cases sent by this audiologist from remote villages to ENT specialists in Anchorage demonstrated both improved access for care and cost savings associated with avoidance of travel.8 In addition, a remarkable level of previously undiagnosed and untreated illness was recognized and treated.9
Store-and-forward telehealth has led to improvements in efficiency. For example, 20 percent of specialty consultations using AFHCAN within ATHS are completed in 60 minutes or less—before the patient leaves the village clinic. Almost 75 percent are completed in one business day.10 A review of more than 4,000 cases sent to specialists in Anchorage showed that store-and-forward consultations were quite time efficient, with 50 percent of all specialist consultations taking less than six minutes, leading to increased specialist productivity.11
Finally, a recent analysis demonstrated significant cost savings accrued to Alaska Medicaid from avoided travel for beneficiaries requiring specialty care. Over a five-year period, $3.1 million has been saved by Alaska Medicaid. More specifically, for every dollar spent by Alaska Medicaid to reimburse store-and-forward telehealth, $11.50 has been saved in avoided travel costs.12 These savings create opportunities for additional care for underserved populations.
Considered together, the experiences within ATHS suggest that store-and-forward telehealth is an effective tool for addressing disparities in healthcare. It can improve access for underserved populations, avoid costs associated with unnecessary travel and time lost from work, maximize provider productivity, and help match provider availability and capacity with patients’ needs.
The IHS Joslin Vision Network Tele-Ophthalmology Program
Diabetes is 2.2 times more prevalent among American Indians and Alaska Natives than among the general US population.13 Diabetic retinopathy eventually affects almost all individuals with diabetes and is the most common cause of blindness among working-age adults. Unfortunately, while serious vision loss due to diabetes can nearly be eliminated by timely diagnosis and treatment, only half of all American Indian and Alaska Natives with diabetes receive an annual retinal examination. There are many causes for this limitation in retinopathy screening, but access to care is prominent among them.
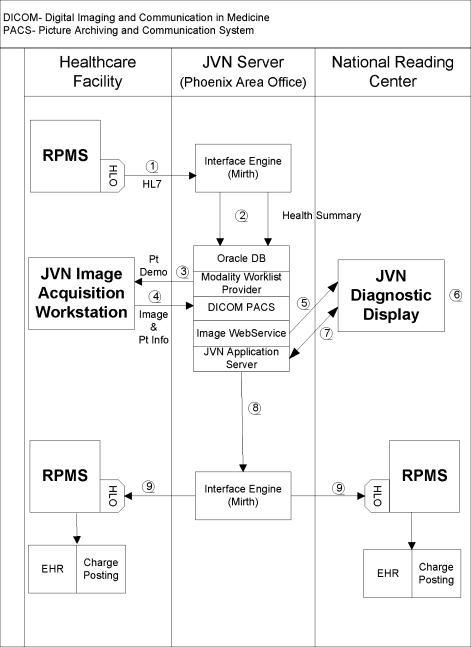
The IHS Joslin Vision Network (JVN) tele-ophthalmology program is a telemedicine solution deployed throughout Indian country for the remote diagnosis and management of diabetic retinopathy. JVN is a nonmydriatic (i.e., non-eye-dilating) system that has been validated to be equal or superior to a live exam for diagnosing diabetic retinopathy, and is able to replace a conventional dilated examination for this purpose.14 The system is operated by a technician with no previous medical experience other than three days of training. An imaging workstation is positioned in the primary care environment; patients with diabetes are imaged as a routine component of their diabetes care. Retinal images are automatically bundled with key EHR clinical and demographic data and are sent to a central server on the IHS network for review (Figure 1).
Figure 1.
IHS JVN Data Flow
All interpretations are provided by licensed and certified readers at a national reading center. A report is returned to the referring facility with a diagnosis of level of diabetic retinopathy and any other pathology noted. The report also contains management recommendations made in the context of patient health data contained in the EHR.
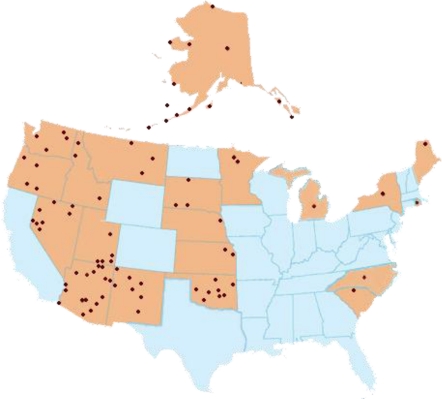
This solution has been installed at 75 sites in 20 states, with additional locations served through a portable deployment strategy (see Figure 2). To date, almost 50,000 studies have been completed. Of significant note, 10,000 individuals with diabetes not previously receiving annual retinal examinations were studied in 2010.
Figure 2.
Map of JVN Deployed Sites, October 2010
The IHS JVN program has been very effective in increasing compliance with the standard of care for diabetic retinopathy surveillance and bringing high-risk patients to timely treatment for the prevention of vision loss. In addition, reimbursement opportunities create a strong business case for the program, helping offset operational costs. However, several relative barriers to maximum use of this technology have been identified. Despite the strong public health and business case for the program, some sites demonstrate a low utilization rate. The reason for this is not clear, but failure to integrate the program into routine diabetes care appears to be part of the explanation.
Another problem is the cost of the system, making deployment in small communities (less than 250 patients with diabetes) impractical. For this reason, a portable system has been developed and deployed in 14 small remote communities in Alaska and North Carolina. This portable system has been very successful in extending the standard of care to small remote communities. The portable system is being refined with the development of a smaller, less expensive camera. This improvement will enhance its suitability for fixed and mobile applications for American Indian and Alaska Native communities across the country.
Barriers and Challenges
While the use of RPMS EHR, AFHCAN telehealth, and the IHS JVN tele-ophthalmology solution demonstrate significant progress in achieving health equity through innovation, challenges remain. There exist many barriers to both the implementation and the spread of emerging HIT and telehealth innovation across a health system. Infrastructure, constrained resources, technical support, and resistance to change are key examples. Because of the expanding blend of innovative delivery systems (e.g., telehealth) and electronic records, successful integration of patient health information across a health enterprise warrants special consideration.
Despite progress, many telehealth systems across the United States are not integrated with electronic health record (EHR) systems. This shortcoming is due, in part, to the absence of appropriate EHR fields for unique data sets contained in telehealth encounters. In addition, there are complexities inherent in the integration of telehealth data sets with varied EHRs, and difficulties in cross-identifying patients across organizational boundaries without the presence of intra- or interorganizational master patient indices.
The rapid adoption of EHRs is helping drive health data integration across domains. Many of the “meaningful use” criteria are motivating adoption of interface standards to meet specific requirements, and the evolution and adoption of health information exchanges (HIEs) and regional health information organizations (RHIOs) further accelerates the expectation that healthcare data will not only move over geographic distances (such as in telehealth) but will eventually reside in the EHR itself rather than in separate systems and software.
Fortunately, much work has been done on national interface standards to guide health data integration. For example, standards promulgated by the Nationwide Health Information Network (NHIN), the Direct Project, and the Healthcare Information Technology Standards Panel (HITSP) specify the shape and detail of data exchanges, with a focus on the well-defined and enforceable “document” or “encounter” level, rather than previously used levels (e.g., HL7 messaging) that often required custom specifications and allowed for ambiguity and confusion.
Using these new standards, the AFHCAN telehealth program has worked closely with the IHS to develop HITSP-compliant interfaces between RPMS EHR and the AFHCAN tConsult system. This is especially relevant to Tribal and IHS clinical sites as many patients receiving telehealth consultation via AFHCAN are already registered in RPMS. Presently, the AFHCAN solution recognizes RPMS as the definitive source of patient information and demographics for cases locally created in Indian health facilities using RPMS.
A more complex issue concerns the delivery of a health summary from an EHR to a telehealth system. This issue is especially pertinent in Alaska, as 25 percent of all telehealth cases created in AFHCAN are sent outside the originating site's organizational boundary to another healthcare organization that does not have access to the originating site's EHR. IHS now provides this interface through the C32 document standard—an XML document that follows the Clinical Document Architecture standards defined by HL7 Version 3 and whose actual contents are defined by HITSP standards. IHS is currently prototyping this interface as part of an ongoing effort to interface with the NHIN, and has made this technology available to beta test sites in Alaska as of fall 2010. The IHS is working with AFHCAN to share these C32 documents on a query/response mechanism, a cost-effective step toward the full implementation of a NHIN interface.
The final component of a fully bidirectional interface is the transmission of data and reports from telehealth systems into EHRs. The IHS JVN program is nearing completion of software upgrades that will automate bidirectional data exchange with the RPMS EHR. A similar solution is under development between AFHCAN and the RPMS EHR, utilizing the C48 and C84 HITSP document constructs. Completion of both RPMS-JVN and RPMS-AFHCAN bidirectional interfaces is anticipated in 2011.
Looking to the Future
IHS and Tribal health programs are committed to the delivery of quality healthcare via service innovation and health information technology. This commitment is realized through robust and expanding HIT and telehealth solutions. Within the next 12 months, the IHS plans completion of ambulatory and inpatient certification of the IHS EHR so that all Indian health sites utilizing the IHS EHR will be able to successfully achieve the criteria for meaningful use as announced by the Centers for Medicare and Medicaid Services. IHS and Tribal sites will also continue collaboration on telehealth service planning and implementation so that more American Indian and Alaska Native communities can benefit from medical home models of care using telehealth innovation.
A continued emphasis on health information technology, telehealth, and related innovation will help the IHS and Tribes address persistent disparities in health status affecting American Indians and Alaska Natives. Health information technology and telehealth are important components of ongoing strategies within the IHS to accomplish its mission of raising the physical, mental, social, and spiritual health of American Indians and Alaska Natives to the highest level.
Footnotes
Special thanks to Chris Patricoski, MD; Phillip Smith, MD, MPH; Howard Hays, MD; and Mark Veazie, DrPH, for their review and assistance with this article's preparation.
The opinions in this article reflect those of the authors and do not necessarily reflect those of the Indian Health Service or the Alaska Native Tribal Health Consortium. No sponsorships or competing interests are disclosed for this article.
Contributor Information
Mark Carroll, the Indian Health Service.
Theresa Cullen, the Indian Health Service.
Stewart Ferguson, the Alaska Native Tribal Health Consortium.
Nathan Hogge, the Alaska Federal Health Care Access Network.
Mark Horton, Joslin Vision Network tele-ophthalmology program.
John Kokesh, the Alaska Native Medical Center.
Notes
- 1.Indian Health Service. Trends in Indian Health, 2002-2003 Edition. Available at http://www.ihs.gov/NonMedicalPrograms/IHS stats/index.cfm?module=hqPubTrends03 (accessed September 9, 2010).
- 2.Barnes P.M, Adams P.F, Powell-Griner E. Health Characteristics of the American Indian or Alaska Native Adult Population: United States, 2004-2008. National Health Statistics Reports 20. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 3.Indian Health Service. IHS Fact Sheets: Indian Health Disparities. Available at http://info.ihs.gov/Disparities.asp (accessed September 9, 2010).
- 4.Sequist T, Cullen C, Hays H, Taualii M.M, Simon S.R, Bates D.W. “Implementation and Use of an Electronic Health Record within the Indian Health Service”. Journal of the American Medical Informatics Association. 2007;14:191–97. doi: 10.1197/jamia.M2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.State of Alaska Rural Health Plan, 2001. Available at http://www.hss.state.ak.us/dhcs/healthplanning/publications/assets/rural_health_plan.pdf
- 6.Alaska Native Tribal Health Consortium, Division of Planning, Evaluation and Health Statistics. Alaska Native Mortality, 1980-1998. Available at http://www.inchr.com/Doc/February05/mortality-98-report.pdf.
- 7.Hofstetter P.J, Kokesh J, Ferguson A.S, Hood L.J. “The Impact of Telehealth on Wait Time for ENT Specialty Care”. Telemedicine and e-Health. 2010;16(no. 5):551–56. doi: 10.1089/tmj.2009.0142. [DOI] [PubMed] [Google Scholar]
- 8.Kokesh J, Ferguson A.S, Patricoski C, LeMaster B. “Traveling an Audiologist to Provide Otolaryngology Care Using Store-and-Forward Telemedicine”. Telemedicine and e-Health. 2009;15(no. 8):758–63. doi: 10.1089/tmj.2009.0046. [DOI] [PubMed] [Google Scholar]
- 9.Kokesh, J., A. S. Ferguson, and C. Patricoski. “The Alaska Experience Using Store-and- Forward Telemedicine for ENT Care in Alaska.” Otolaryngologic Clinics of North America 44, no. 3 (forthcoming). [DOI] [PubMed]
- 10.AFHCAN Usage Report-generated from AFHCAN servers on a quarterly basis.
- 11.Ferguson A.S, Kokesh J, Patricoski C, Hofstetter P.J, Hogge N. Impact of Store-and-Forward Telehealth in Alaska: A Seven Year Retrospective. Anchorage, AK: Alaska Native Tribal Health Consortium; 2008. [Google Scholar]
- 12.Ferguson, A. S., J. Kokesh, and C. Patricoski. “Savings in Travel Costs for Alaska Medicaid: A Case for Store-and-Forward Telehealth Specialty Care.” Unpublished manuscript.
- 13.Centers for Disease Control and Prevention. 2007 National Diabetes Fact Sheet. Available at http://www.cdc.gov/diabetes/pubs/estimates07.htm#4 (accessed March 12, 2010).
- 14.Bursell S.E, Cavallerano J.D, Cavallerano A.A, Clermont A.C, Birkmire-Peters D, Aiello L.P, et al. “Stereo Nonmydriatic Digital-Video Color Retinal Imaging Compared with Early Treatment Diabetic Retinopathy Study Seven Standard Field 35-mm Stereo Color Photos for Determining Level of Diabetic Retinopathy”. Ophthalmology. 2001;108(no. 3):572–85. doi: 10.1016/s0161-6420(00)00604-7. [DOI] [PubMed] [Google Scholar]