On march 1, 1963, orthotopic liver homotransplantation was performed in a 3-year-old child with congenital biliary atresia. Immediately after revascvtlarization of the hepatic homograft, uncontrollable bleeding developed which resulted in death a few hours later. Blood studies obtained at the time of the hemorrhagic crisis revealed an exceedingly sharp increase of plasma fibrinolytic activity, as well as hypofibrinogenemia.
As a result of this experience, laboratory investigations were undertaken to define with more predictability the changes in coagulation to be expected during and after canine hepatic homografting procedures. In addition, a collateral study of fibrinolytic activity was carried out in dogs subjected to total hepatectomy without homotransplantation.
Finally, the opportunity eventually became available to study some aspects of the clotting process in four additional patients who received whole-organ hepatic homografts after removal of their diseased livers. From this composite laboratory and clinical experience, a clear idea has emerged concerning the coagulation abnormalities which should be anticipated during and after orthotopic liver transplantation. It has also provided information which may be helpful in understanding the changes in coagulation which occur during other kinds of hepatic surgery.
Methods
Coagulation Studies
Coagulation tests were selected which could be determined repeatedly and quickly enough to be of value in planning therapy and which were expected to provide the maximum information. Fibrinolytic activity was estimated serially in the human cases with the euglobulin lysis time.1 For the dog, a modified technique 2 was used. Both methods measure the rate of spontaneous dissolution of a clot prepared from the euglobulin fraction of blood; increased fibrinolytic activity causes a shortening of the euglobulin lysis time (ELT). In man, the ELT is normally above 120 minutes. Normal ELT for dogs is 80 to 140 minutes. The ELT, which is thought to measure plasminogen activator, is a particularly useful test inasmuch as the results are readily available and are not influenced by either heparin or by ε-aminocaproic acid (EACA) despite the fact that the latter drug acts by inhibiting the plasminogen activator.3 In the clinical cases ELTs were supplemented with thrombelastograms 4 which provide a continous record of the formation of clot, development and degree of its firmness, and its pattern of dissolution.
Other tests performed included analysis of plasma fibrinogen,5 one-stage (Quick) determination of the prothrombin complex, and in some clinical cases the thrombin generation.6 Thrombin time 7 was also measured (normal, 14 to 16 seconds). With this battery of tests, it is possible to differentiate rapidly between hyper- and hypocoagulable states, evaluate the contributing causes of hypocoagulability, estimate the degree of fibrinolytic activity, and evaluate the trend of thrombin inhibitor.
Canine Experiments
Total hepatectomy was performed under ether anesthesia.8,9 Before the animals were anesthetized, a control blood sample was taken for determinations of euglobulin lysis time, thrombin time, and fibrinogen levels. During the actual removal of the liver, additional blood samples were taken before and after the liver was excluded from the circulation, immediately following hepatectomy, and ½,l,2,3,4,5,6, and 7½ hours thereafter.
Orthotopic liver homotransplantation was performed under pentobarbital narcosis.10 A control blood sample was obtained prior to induction of anesthesia. Subsequent samples were taken before and after exclusion of the recipient’s own liver from the circulation, immediately upon completion of transplantation, and at ½, 1, 1½, 3 and 24 hours thereafter.
Human Hepatic Homotransplantation
The details of the operative procedure and general care of these patients have been reported.11,12 In the first patient, the entire transplantation procedure was carried out in one stage. In the other four, complete mobilization of the recipient’s diseased liver with skeletonization of the vessels and extrahepatic biliary tree was performed as a preliminary first-stage procedure. Excision of the diseased organ and replacement with a cadaveric homograft was done as a second stage, 1 to 14 days later. Blood samples for analysis were obtained before any operative intervention, at the time of the preliminary first-stage operation in cases 2 to 4, and during and after the actual transplantation in cases 1 to 5.
Results
Canine Liver Transplantation
The ELT generally decreased after the animal’s own liver was excluded from the circulation or during subsequent completion of the transplantation. It dropped to one third of its control value in some animals and remained depressed in all animals for two to three hours after reestablishment of homograft circulation. In five dogs in which at 24 hours the test could be performed, the ELT had rebounded at this time above the control values. The composite histograms and curves representing the average values at each sample time of seven dogs is given in Fig 1.
Fig 1.
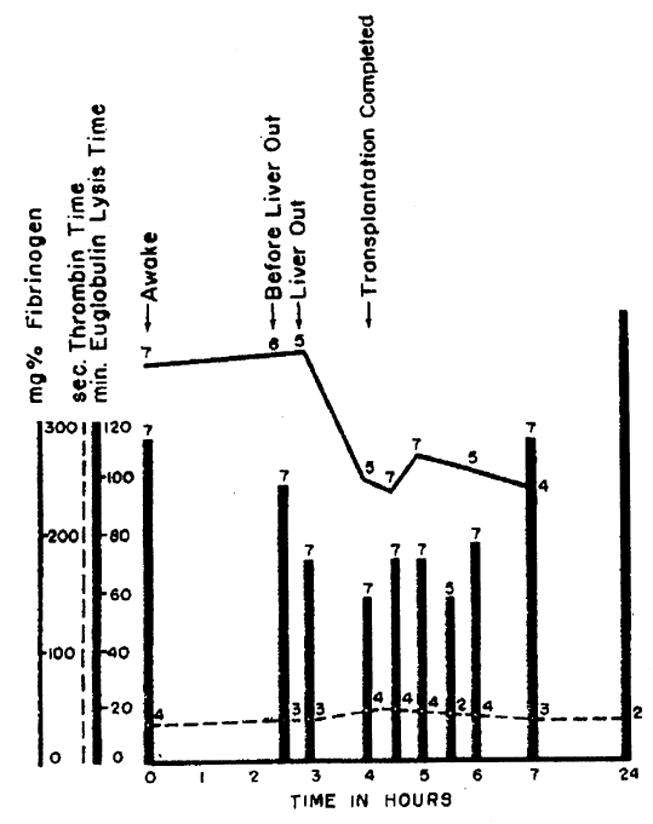
Trend of euglobulin lysis time and plasma fibrinogen concentration before, during, and after canine orthotopic liver homotransplantation (average values). Number of animals used to obtain average values is indicated. Note drop of ELT at time of liver removal followed by return to normal within five hours after placement of the homograft. The maximum decrease in ELT did not occur at same time; degree of fibrinolytic activity at some time during individual experiments was, therefore, generally greater than depicted by mean values.
Plasma fibrinogen decreased during the procedure, the trend starting during the anhepatic phase, and continuing for short periods after reestablishment of circulation. These stabilized after vascularization of the transplanted organ (Fig 1). The thrombin time increased slightly during the surgical procedure and then rapidly returned to normal. In no animal did it rise above 21 seconds.
Although clotting studies were not carried out beyond 24 hours, coagulation disorders contributed to the death of two animals after this time. One dog died after 30 hours of massive intra-abdominal hemorrhage. Another, which died after 31 days of a perforated gastric ulcer, also was shown at autopsy to have multiple pulmonary emboli which originated from the terminal inferior vena cava.
The results obtained with this test series indicated that the euglobulin lysis time shortens considerably with occlusion of the liver circulation and tends to become longer than normal after resumption of function by the transplanted liver. It could be reasoned that the new liver was responsible for restoration of a normal equilibrium of the fibrinolytic system. In order to see if the same changes occurred without provision of a homograft, studies were carried out with hepatectomy alone.
Total Hepatectomy in Dogs
Within minutes after hepatectomy in five dogs the average ELT decreased to about one third of its preoperative value. Surprisingly, in four of the five dogs the ELT started to rise one to three hours after hepatectomy and reached normal prehepatectomy values within about two to five hours (Fig 2). These findings indicate that disappearance of fibrinolytic activity described in the preceding section after transplantation of a new liver is not solely due to resumption of liver function.
Fig 2.
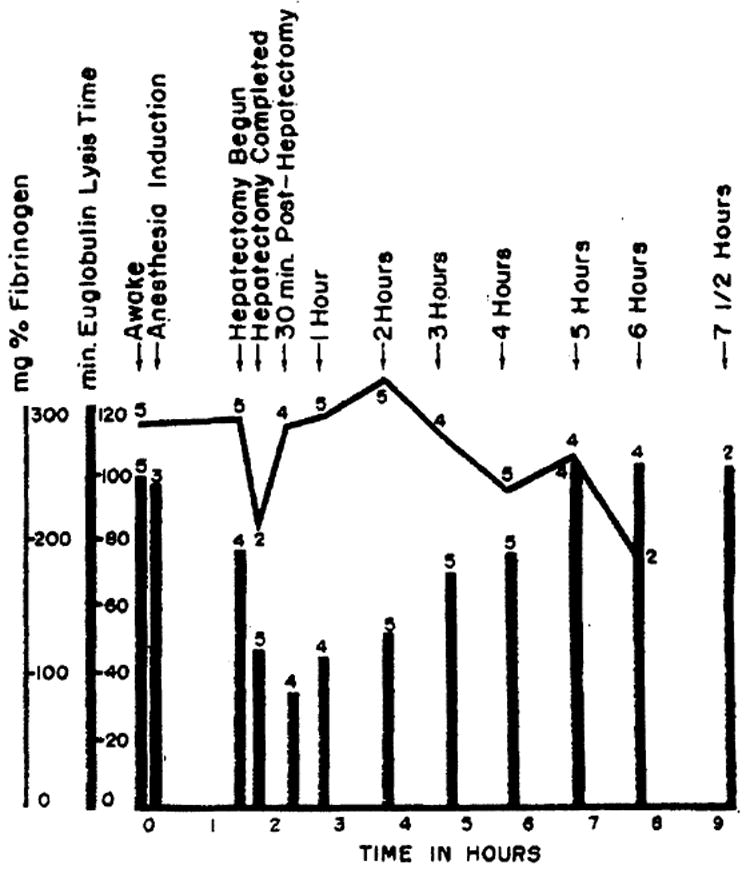
Trend of average euglobulin lysis time and plasma fibrinogen concentration before, during, and after canine hepatectomy. Number of animals used to obtain mean values is indicated. Note drop of ELT at time of liver removal followed by return to normal within five to six hours.
In all animals there was a moderate decrease of plasma fibrinogen within the first six hours (Fig 2). The thrombin time increased to 39 seconds after one and four hours, respectively, in the two dogs in which it was studied.
Human Liver Transplantation
Five patients were investigated. In each case the patient’s own liver was removed and replaced orthotopically with a cadaveric homograft. During the actual transplantation the inferior vena cava must be occluded, necessitating an external plastic bypass * from the femoral to the jugular system 12 which provides for return of inferior vena caval blood to the heart. Certain penalties are exacted by the necessity of such a bypass, including temporary violation of the venous system by a foreign body and prolonged contact of blood with the plastic. The complications to be described below in cases 2 to 4 may have been partly due to these mechanical factors.
Report of Cases
Case 1
A 3-year-old child with biliary atresia was treated with a one-stage orthotopic homotransplant. The preoperative prothrombin activity was 55% and thrombelastogram findings were essentially normal. Uncontrollable bleeding developed after placement of the homograft. The boy died on the operating table.
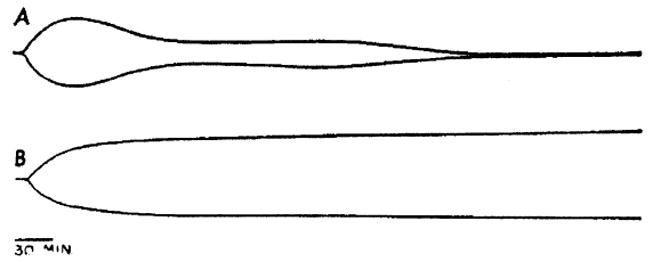
Almost immediately after the liver transplant was revascularized, there was extreme activation of the fibrinolytic system as demonstrated by a thrombelastogram (Fig 3 A) which showed dissolution of the clot nearly as fast as it was formed. Addition of one part of normal plasma to one part of patient’s plasma resulted in the appearance of a rather poor clot which never came to completion because it also dissolved rapidly (Fig 3 B). The clots obtained from plasma by thrombin during the determination of the thrombin time at this time dissolved on incubation within five minutes.
Fig 3.
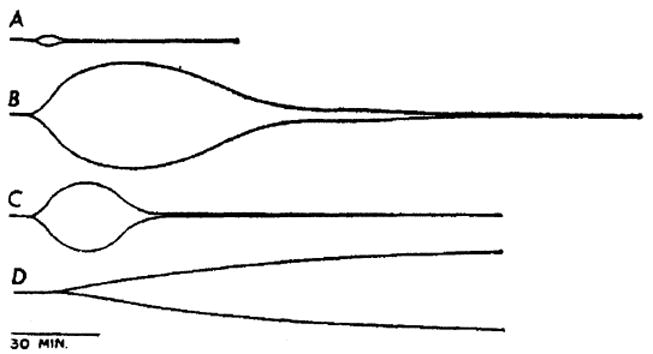
Thromboelastograms of recalcified citrated plasma obtained two hours after revascularization of orthotopic liver homograft in patient 1 of clinical series. (A) Untreated plasma. Clot dissolves as fast as it is formed. (B and C) 50% and 20%, respectively, of normal fresh plasma have been added to specimen of patient’s plasma. Fibrinolysis is slowed but not prevented. (D) after patient had been given intravenously EACA (0.1 gm/kg). Fibrinolytic reaction is abolished but there is poor clot due to low fibrinogen.
The ELT was five minutes. Intravenous administration of EACA, 0.1 gm/kg, caused the disappearance of the fibrinolysis pattern from the thrombelastogram (Fig 3 D). The clots formed normally, although they remained structurally poor; hypofibrinogenemia of 95 mg/100 cc was undoubtedly a contributing factor.
Case 2
A 48-year-old Negro man with a primary hepatoma was treated with a two-stage hepatic transplantation. At the first operation, all structures entering and leaving the liver were skeletonized for subsequent anastomoses. Considerable manipulation of the liver was required.
Prior to the first stage, there was a normal thrombelastogram and a normal prothrombin time. The preoperative fibrinogen was 393 mg/100 cc, and the ELT was longer than two hours. A marked increase in the fibrinolytic activity was evoked with mobilization of the liver as reflected by shortening of the ELT to 60 minutes. One hour later, the ELT was still 64 minutes (Fig 4). As the wound was being closed, the ELT had rebounded to longer than four hours. Fibrinogen levels remained essentially normal throughout the procedure. There was a transient rise of the thrombin time. Three units of fresh whole blood and 2 gm of human fibrinogen * were administered. The changes in ELT, fibrinogen concentration, and thrombin time are shown in Fig 4.
Fig 4.
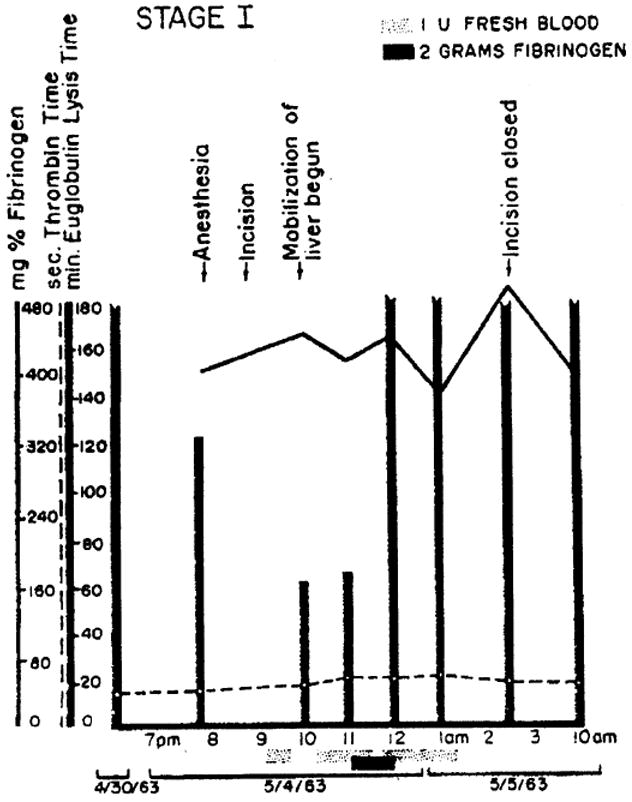
Changes in euglobulin lysis time, fibrinogen concentration, and thrombin time during stage 1 mobilization of liver in patient 2. Note decrease of euglobulin lysis time during manipulation of liver.
On the following day, the definitive transplantation was carried out. An ELT of 13 hours was demonstrated in blood samples drawn 9 hours preoperatively and also after induction of anesthesia for the second-stage procedure. The fibrinogen levels were 395 mg/100 cc and 423 mg/100 cc respectively. Thrombin times were normal. Occlusion of the inferior vena cava as the last preparatory step for hepatectomy was followed by a very pronounced drop of ELT to 28 minutes despite the preceding prophylactic infusion of fresh blood and human fibrinogen (Fig 5). EACA, 0.1 mg/kg, was then administered intravenously. After vascularization of the transplanted organ, the ELT was still only 18 minutes.
Fig 5.
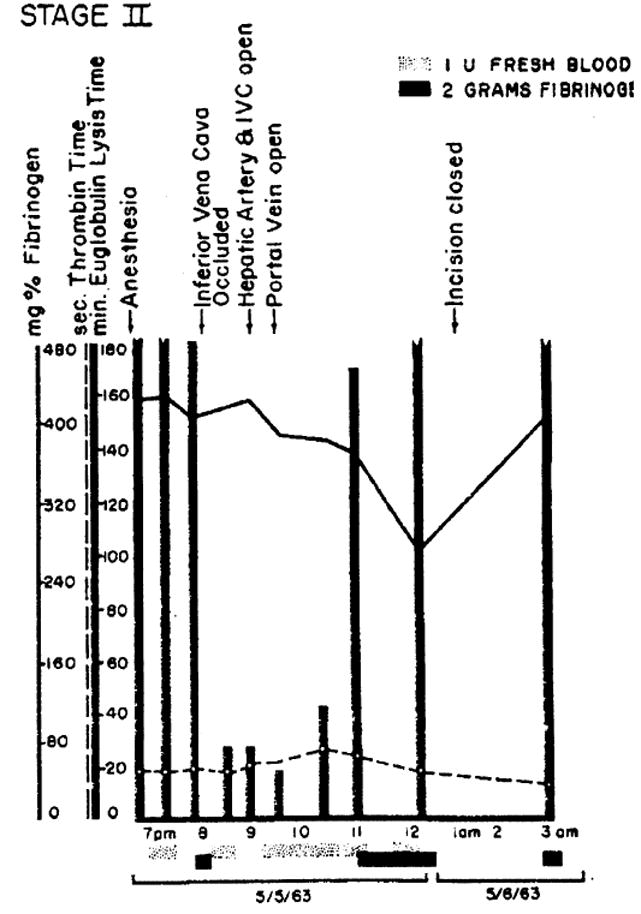
Changes in euglobulin lysis time, fibrinogen concentration, and thrombin time during actual liver transplantation in patient 2. Note extreme shortening of ELT during transplantation mg/kg) was given, I.V at 8:47 ™ with no influence on ELT by 9 ™; nevertheless EACA (0.1 thromboelastogram was restored to normal at this time. (See Fig 6).
However, bleeding was not of major significance. Since EACA does not precipitate with the euglobulins used for the determination of ELT, there was no correlation between the ELT and clinical fibrinolytic activity after treatment with EACA. Such correlation was provided by the thrombelastograms (Fig 6). The thrombelastogram A (ELT 28 minutes) prior to administration of EACA showed a clear-cut clot lysis. After administration of EACA, thrombelastogram B revealed abolition of the fibrinolytic activity (Fig 6) despite an ELT of 18 minutes. After vascularization of the transplanted liver, the ELT gradually rose to a normal level in l½ hours, indicating that the excess plasminogen activator was no longer present. Five hours after the beginning of the procedure, the ELT exceeded the control values and remained elevated throughout the postoperative period. Just after revascularization of the homograft, a transient rise of thrombin time to 25.4 seconds was observed. The fibrinogen levels decreased during the procedure, although they were maintained in a near-normal range by the intravenous infusion of fibrinogen (Fig 5).
Fig 6.
Thromboelastograms in patient 2. (A) Rapid clot dissolution during unhepatic state (ELT 28 min). (B) Thrombelastogram obtained few minutes later after intravenous EACA. Despite ELT of 18 minutes, clot lysis is controlled.
During the subsequent course several significant changes occurred. On the first postoperative day there was a transient rise in plasma fibrinogen with a progressive decrease from 506 to 106 mg/100 cc during the next week (Fig 7). Except for a value of 22% and 43% on the sixth and seventh postoperative days, the activity of the prothrombin complex remained above 60%. Platelet counts were markedly decreased during most of the postoperative period. From the first day onward the ELT was above six hours and from the fifth day onward the thrombelastograms showed accelerated fibrin formation. Postoperative thrombin times were normal except for a single elevation to 23 seconds on the 11th postoperative day.
Fig 7.
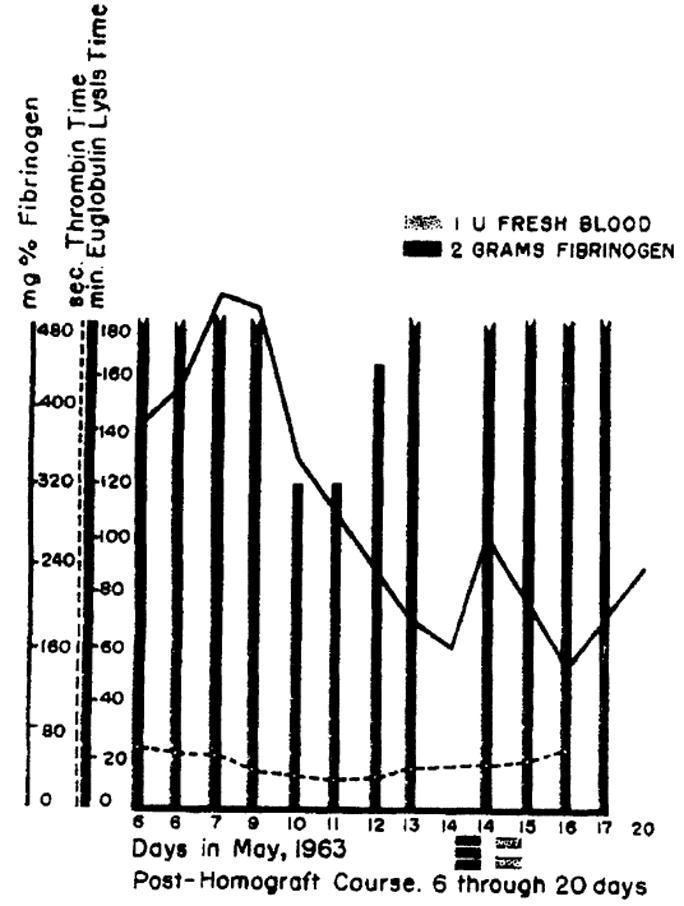
Euglobulin lysis time, fibrinogen concentration, and thrombin time during postoperative period of patient 2. Note progressive decrease of fibrinogen level in absence of any increase of spontaneous fibrinolytic activity.
In retrospect, the combination of thrombocytopenia, decreasing plasma fibrinogen content, and accelerated fibrin formation in the thrombelastogram probably indicated intravascular clotting during the first postoperative week. By the tenth postoperative day clinically evident thrombophlebitis had developed, affecting the leg into which the plastic bypass had been placed during operation. The patient was given 6 gm of fibrinogen because of the continuous drop of fibrinogen (Fig 7). Intravenous heparin therapy was administered for four days and then discontinued because of gastrointestinal hemorrhage. The patient died on the 22nd postoperative day from multiple pulmonary emboli. A few hours before death the ELT was longer than 24 hours, indicating the absence of any spontaneous fibrinolytic activity. At autopsy there was right ileofemoral thrombosis extending into the terminal inferior vena cava. The homograft was very well preserved and microscopically there were no unequivocal signs of rejection.
Case 3
A 67-year-old man with bile duct carcinoma received a two-stage orthotopic homotransplantation. During the first stage the ELT and fibrinogen levels were unchanged although there was a transient rise in the thrombin time.
The second stage was performed 14 days later and, in addition, a vena caval plication 13 was performed below the renal veins. The ELT and fibrinogen exhibited the same intra-operative changes as in patient 2 with a somewhat more prolonged drop in ELT (Fig 8). He received 0.1 gm/kg EACA as soon as the euglobulin lysis had fallen below 40 minutes. However, within two hours after revascularization of the homograft the thromboelastograms revealed accelerated coagulation with abnormally firm clot formed. These findings persisted until shortly before death, when poor clots were again observed at a time when the plasma fibrinogen had dropped to 96 mg/100 cc. Thrombin times were elevated during operation and for the entire subsequent course. Platelet counts were depressed.
Fig 8.
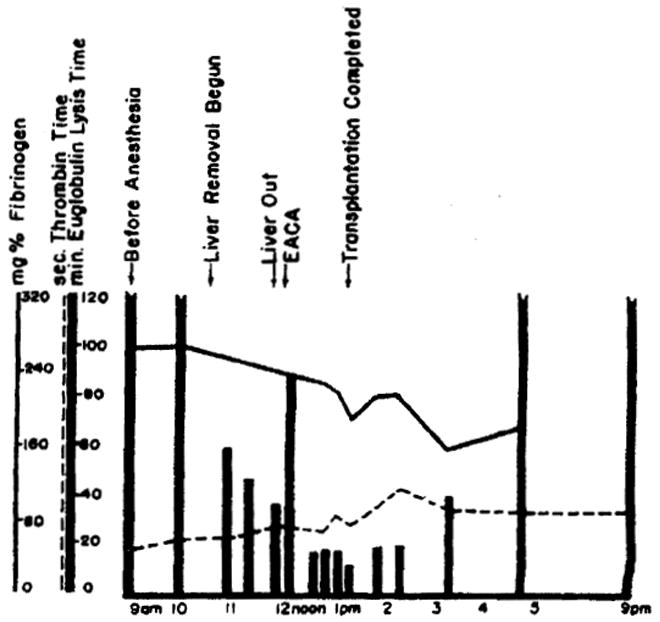
Euglobulin lysis time, fibrinogen concentration, and thrombin time in patient 3. Note temporary shortening of ELT during and after transplantation, but with subsequent return to normal or prolonged values.
The tendency to hypercoagulability with the declining fibrinogen content and reduced platelet counts were compatible with the diagnosis of intravascular clotting. Episodes of pulmonary embolizaticon occurred one and two days after operation. At the time of autopsy one week after operation, multiple pulmonary emboli were found but no peripheral source could be identified. It is possible that these clots were formed in the bypass tubing and passed into the pulmonary circulation during the surgical procedure. Alternatively, these may have represented primary thrombosis during the phase of hypercoagulability. The liver did not have histologic evidence of rejection.
Case 4
A 53-year-old man with a hepatoma received a homotransplantation with a one-day delay between the first and second stages. During the external bypass, 2 mg/kg heparin were administered with later neutralization by hexadimethrine bromide after discontinuance of the bypass. The inferior limb of the bypass was inserted through the common femoral vein, which was subsequently ligated.
During the preliminary procedure, the ELT, decreased from a control of eight hours to three hours at the time the abdomen was opened, was about five hours at the time of liver mobilization, and remained longer than four hours by the end of the procedure. There was a transient rise in the thrombin time to 23.1 seconds. The fibrinogen concentration was 261 mg/100 cc at the beginning, 161 mg/100 cc at the time of liver mobilization, and 234 mg/100 cc at the end of the procedure.
During the definitive homotransplantation, the ELT decreased from a control value of 275 minutes to 60 minutes, one hour after vascularization of the transplanted organ, and then, rapidly rose to normal value. At the beginning of the procedure, the fibrinogen level was only 47.7 mg/100 cc. During the procedure, the fibrinogen level was maintained at 52 to 107 mg/100 cc by the intravenous administration of fibrinogen and had risen to 244 mg/100 cc three hours posttransplantation. Heparinization of the patient vitiated meaningful thrombin time tests. Two days postoperatively, the patient developed respiratory distress. This was treated with tracheostomy and positive pressure respiration in addition to heparinization for presumed pulmonary emboli. Despite these measures, the patient died on the sixth postoperative day. Necropsy revealed a thrombus extending from the right femoral vein through the inferior vena cava to the right atrium and pulmonary artery, multiple small peripheral pulmonary emboli, subendocardial petechiae, and a fibrinous pericarditis with pericardial effusion. The origin of the thrombus was at the site of the previous ligation of the femoral vein.
Case 5
A 29-year-old woman with a primary hepatoma had a first-stage procedure on Oct 2, 1963. Orthotopic homotransplantation was performed two days later. There were several differences in procedure between that used on this patient and those previously described. During the preliminary operation, a vagotomy and pyloroplasty were performed electively in an attempt to prevent the postoperative gastrointestinal hemorrhage that had occurred in patients 2 and 3. The following modifications were designed to prevent intravascular clotting. EACA and fibrinogen were not used during the definitive homotransplantation procedure. The polyethylene shunt was inserted into the femoral vein via the saphenous vein at the groin. The saphenous vein was ligated at the saphenous femoral junction immediately after discontinuing the shunt. During the period of bypass, the patient was heparinized and the heparin was not subsequently neutralized. Bleeding during surgery was controlled by suture and ligature. Eighteen units of fresh whole blood were used.
Coagulation studies were not performed during the preliminary procedure. ELT before and after induction of anesthesia for the second stage one day later was, with 17 and 18 hours, respectively, unusually long. The ELT decreased drastically to 65 minutes at the time of the inferior vena caval anastomosis and then rose to eight hours by the end of the procedure. The fibrinogen level remained essentially unchanged until after the inferior vena caval anastomosis and then decreased to 30% of its original value. The thrombin time was not measured in the heparinized patient.
The postoperative ELTs were with one exception within normal limits. They never reached the long values as in the previous patients who experienced intravascular clotting (Table). Postoperatively, fibrinogen concentration remained reduced and decreased further on the 20th postoperative day to 70.5 mg/100 cc. Thrombin times were slightly elevated postoperatively to 18.8 seconds. The postoperative activity of the prothrombin complex fell progressively from 45% on the first postoperative day to 8% and 9% on the last two days of life (Table). Serial thromboelastograms revealed deterioration of the clotting process in the posttransplantation period, particularly in the structure of the clot formed. Reduced thrombin generation reflected equally a deterioration of the clotting process (Table). There was no sign of hypercoagulability clinically and by laboratory tests.
Homotransplantation of the Liver in Patient 5 *
| Sample | ELT, Min | Fibrinogen, Mg/100 Cc | Thrombin Time, Sec | Prothrombin Complex, % | Clot Formation in Thrombelastogram: Speed & Structure | Thrombin Generation: Speed & Yield |
|---|---|---|---|---|---|---|
| Preanesthesia | 1,020 | 323 | 12.8 | |||
| Postinduction | 1,080 | 394 | 12.2 | |||
| Hepatectomy begun | 240 | 398 | 13.0 | |||
| ICV, anastomosis complete | 65 | 394 | ||||
| Transplant vascularization | 112 | |||||
| Incision closed | 480 | 113 | 22.6 | |||
| Posttransplantation: | ||||||
| Day 1 | 45 | |||||
| 2 | 20 | |||||
| 3 | 143 | 28 | slow | |||
| poor | ||||||
| 4 | 180 | 14.8 | 32 | slow | normal | |
| poor | reduced | |||||
| 5 | 96 | 159 | 16.6 | 21 | normal | |
| normal | ||||||
| 6 | 130 | 138 | 15.0 | 27 | slow | reduced |
| normal | reduced | |||||
| 7 | 150 | 145 | 15.3 | 32 | fast | |
| normal | ||||||
| 8 | 136 | 116 | 17.0 | 25 | normal | |
| poor | ||||||
| 10 | 133 | 124 | 15.5 | … | normal | |
| poor | ||||||
| 11 | 140 | 97 | 18.4 | 20 | ||
| 12 | 23 | slow | ||||
| poor | ||||||
| 13 | 23 | |||||
| 14 | 152 | 123 | 15.2 | 24 | normal | reduced |
| very poor | near normal | |||||
| 17 | 24 | |||||
| 20 | 225 | 70.5 | 16.3 | 10 | normal | very reduced |
| very poor | reduced | |||||
| 22 | 8 | |||||
| 23 | 9 |
Trend of euglobulin lysis time (ELT), fibrinogen concentration, activity of prothrombin complex, thrombelastographic pattern, and thrombin generation before, during, and after the procedure.
On the 19th postoperative day the patient became lethargic and increasingly jaundiced. She died on the 23rd day. At autopsy, diffuse bile peritonitis was found due to necrosis of the donor portion of the reconstructed common duct. Focal necrosis of the homograft was present histologically. Whether this was due to rejection or to other factors could not be determined.
Comment
Pathologically increased fibrinolytic activity has been demonstrated in a variety of clinical and experimental states 14 including thoracic and hepatic surgery,* cirrhosis of the liver, shock from various causes, venous and arterial occlusion, and severe hemorrhage. Anoxia was present in several of these conditions and its role as one of the underlying mechanisms leading to activation of the plasmin-plasminogen system in vivo has been postulated.14,15
There is apparently a more specific explanation for the increased fibrinolytic activity under the circumstances of the present studies. From the data presented, it is evident that total hepatectomy with or without subsequent orthotopic hepatic homotransplantation results in profound alterations of normal hemostasis. The anhepatic phase is characterized by a sudden fibrinolytic reaction, an observation which is not surprising inasmuch as the liver is thought to eliminate excess fibrinolytic activity,16,17 possibly by clearing plasminogen activator from the circulating blood. An apparently secondary event is a more gradual, moderate decline in plasma fibrinogen which could theoretically be explained as the result of the temporary loss of its source of synthesis, by fibrinolytic digestion, by intravascular clotting, or a combination thereof.
These findings are in agreement with those of Chabal 18 who observed a fibrinolytic reaction in hepatectomized dogs, but they are at variance with the results of Drapanas and his associates 19 who were unable to demonstrate fibrinolysis after two-stage canine hepatectomy. The protocol of the latter authors involved a less-sensitive ELT test (adding bovine fibrinogen to the reaction mixture) and, in addition, the exact time of sampling was not specified. It was noted in the present study that this fibrinolytic crisis was transitory after total hepatectomy and would be missed if sampling were delayed.
While the increased fibrinolytic activity after loss of liver function is thus not surprising, the subsequent spontaneous disappearance of this abnormality in dogs with total hepatectomy is less easy to explain. Experiments with rats suggest that exhaustion of the fibrinolytic system is not the cause. In the latter investigations 20 rats with complete liver bypass exhibited the same early increase in fibrinolytic activity with subsequent restoration toward normal. Intravenous injection of carbachol, a drug which increases fibrinolysis in rats, precipitated a pronounced shortening of the ELT. The delayed rebound increase in ELT in both the hepatectomized dog and rats without liver circulation suggests that organ systems other than the liver play a role in the regulation of fibrinolytic activity.
Whatever the counter-regulatory mechanisms are which tend to restrain sustained fibrinolytic activity, they appear to have introduced a delayed hazard after homotransplantation since the threat of acute bleeding is succeeded by the danger of intravascular thrombosis, particularly when good homograft function is obtained. This sequence of events was demonstrable in the canine experiments in which clot-promoting drugs were not administered. In patients there was, after transplantation, a persistent marked prolongation of the euglobulin lysis time to values not seen in normal persons. This indicates the absence or near-absence of normally present spontaneous fibrinolytic activity, a situation favorable for intravascular clotting. The use of EACA and human fibrinogen undoubtedly exaggerated the risk of intravascular clotting since three of the four patients who survived orthotopic homotransplantation ultimately developed pulmonary emboli. Patient 5, who did not receive these agents, was the only one to escape this complication. In this case, total heparinization was also carried out at the time of the external bypass, but the resultant bleeding was so severe that this practice is thought to be unwise for future application.
In view of the experience on animals in which clinically significant bleeding or clotting tendency has not been a major problem,21 the best course for future clinical trials would seem to be avoidance of pharmacologic manipulation of the coagulation process. In addition, certain technical precautions can minimize trauma to the peripheral and central veins. The external bypass tubing can be introduced through a side branch of the femoral system and the tributary vessel subsequently ligated. Additional studies will be necessary on the behavior of the plastic bypass, since in patieint 3 it is possible that microemboli formed in the external tubing during the operation. In this patient, multiple pulmonary emboli were found at autopsy despite the fact that the patient had received a vena caval plication and in spite of the postmortem absence of any demonstrable peripheral source of clot.
Summary
There is a marked acute increase in fibrinolytic activity after canine hepatectomy and after canine or human orthotopic liver transplantation. However, in the majority of anhepatic dogs, the elevated fibrinolytic activity of blood tends to spontaneously decrease after a few hours, a finding which suggests that organ systems other than the liver participate in the regulation of fibrinolytic activity.
In both dogs and man, the provision of a well-functioning homograft for the anhepatic recipient results in a very rapid correction of the clotting defects induced by hepatectomy and within a few hours may lead to hypercoagulable state. In clinical cases the administration of ε-aminocaproic acid (EACA) and fibrinogen seemed to have exaggerated this rebound inasmuch as three of the four patients who survived orthotopic homotransplantation developed pulmonary embolization which either directly accounted for or was an important contributory cause of death. Recommendations for the management of these coagulation changes are made for application in future trials.
Generic and Trade Names of Drug
Aminocaproic acid–Amicar.
Acknowledgments
This work was supported by grant-in-aid HE 5538 from the National Heart Institute, USPHS: and AM 06283, AM 06344, HE 07735, AM 07772, AI 04152, and FR 00051 from the US Public Health Service.
Footnotes
Tygon, American Stoneware Co., Akron, Ohio.
Merck Sharp & Dohme, division of Merck & Co., West Point, Penn.
We observed recently an ELT of seven minutes and a whole blood clot lysis time of 65 minutes with partial left lobe hepatectomy in man. The resulting hemorrhage was checked with EACA.
References
- 1.von Kaulla KN, Schultz RL. Methods for Evaluation of Human Fibrinolysis: Studies With Two Combined Techniques. Amer J Clin Path. 1958;29:104. doi: 10.1093/ajcp/29.2.104. [DOI] [PubMed] [Google Scholar]
- 2.Rahn B, von Kaulla KN. Pharmacological Induction of Fibrinolytic Activity in the Dog. Proc Soc Exp Biol Med. 1964;115:359. doi: 10.3181/00379727-115-28913. [DOI] [PubMed] [Google Scholar]
- 3.Alkjaersig N, Fletcher AP, Sherry S. E-Aminocaproic Acid, an Inhibitor of Plasminogen Activation. J Biol Chem. 1959;234:832. [PubMed] [Google Scholar]
- 4.von Kaulla KN. Continuous Automatic Recording of Fibrin Formation and Fibrinolysis. J Lab Clin Med. 1957;49:304. [PubMed] [Google Scholar]
- 5.Ratnoff OD, Menzie C. New Method for Determination of Fibrinogen in Small Samples of Plasma. J Lab Clin Med. 1951;37:316. [PubMed] [Google Scholar]
- 6.von Kaulla KN, von Kaulla E. Thrombin Generation in Normal Subjects and in Cardiac Patients. Circ Res. 1964;14:436. doi: 10.1161/01.res.14.5.436. [DOI] [PubMed] [Google Scholar]
- 7.von Kaulla KN, von Kaulla E. Estimation of the Thrombin Time of Plasma. In: Tocantius LM, Kazal LA, editors. Blood Coagulation, Hemorrhage and Thrombosis. New York: Grune and Stratton, Inc; 1964. p. 335. [Google Scholar]
- 8.Kaupp HA, Jr, Starzl TE. The Use of an External Bypass During Experimental Total Hepatectomy. Surgery. 1960;48:330. [PMC free article] [PubMed] [Google Scholar]
- 9.Starzl TE, et al. A New Method for One-Stage Hepatectomy for Dogs. Surgery. 1959;46:880. [PMC free article] [PubMed] [Google Scholar]
- 10.Starzl TE, et al. Reconstructive Problems in Canine Liver Homotransplantation With Special Reference to the Postoperative Role of Hepatic Venous Flow. Surg Gynec Obstet. 1960;111:733. [PMC free article] [PubMed] [Google Scholar]
- 11.Starzl TE, et al. Clinical Experience With Organ Transplantation. Southern Med J. 1965;58:131. doi: 10.1097/00007611-196502000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Starzl TE, et al. Homotransplantation of the Liver in Humans. Surg Gynec Obstet. 1963;117:659. [PMC free article] [PubMed] [Google Scholar]
- 13.Spencer FC, et al. Plication of the Inferior Vena Cava for Pulmonary Embolism: A Report of 20 Cases. Ann Surg. 1962;155:827. doi: 10.1097/00000658-196215560-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.von Kaulla KN. Chemistry of Thrombolysis: Human Fibrinolytic Enzymes. Springfield, Ill: Charles C Thomas, Publisher; 1963. [Google Scholar]
- 15.Muellertz S. Fibrinolytic Activity of Human Blood After Death. Acta Physiol Scand. 1953;28:29. doi: 10.1111/j.1748-1716.1953.tb00942.x. [DOI] [PubMed] [Google Scholar]
- 16.Fletcher AP, et al. Abnormal Plasminogen-Plasmin System Activity (Fibrinolysis) in Patients With Hepatic Cirrhosis: Its Causes and Consequences. J Clin Invest. 1964;43:681. doi: 10.1172/JCI104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rousselot LM, Grossi CE, Panke WF. Alterations des facteurs de coagulation et fibrinolyse chez les cirrhotiques au cours des anastomoses portocaves. Presse Med. 1962;70:1975. [PubMed] [Google Scholar]
- 18.Chabel J, Métais M, Duffrene D. L’hépatectomie totale experimentale chez le chien. Lyon Chir. 1963;50:29. [PubMed] [Google Scholar]
- 19.Drapanas T, Shim WKT, Stewart JD. Studies of Fibrinolytic Activity After Hepatectomy. Arch Surg. 1963;87:64. [Google Scholar]
- 20.Wasantapruek S, von Kaulla KN. Rat Serial Microeugiobulin Lysis Time in Liver Bypass and Drug-Induced Fibrinolysis. Fed Proc. 1965;24:1430. [Google Scholar]
- 21.Starzl TE, et al. Factors Determining Short- and Long-Term Survival After Orthotopic Liver Homotransplantation in the Dog. Surg. 1965;58:131. [PMC free article] [PubMed] [Google Scholar]


