Abstract
Objective
To determine if increasing fatness interferes with the measurement of fat and bone mineral density (BMD) by dual-energy X-ray absorptiometry (Lunar iDXA).
Methods
We performed measurements of BMD and fat on a section of a beef femur defatted by prolonged boiling in detergent, completely surrounded by increasing thicknesses of lard. Initially the bone was placed in the marked spine area, overlying a 6L plastic bottle which was placed in the marked trunk area of the iDXA. The plastic bottle was then removed and further measurements were carried out with increasing thicknesses of lard surrounding the bone. Measurements were repeated 4 times.
Results
The reported measurement of BMD progressively increased with each increased layer of lard surrounding the bone. All the iDXA BMD measurements were significantly (P<0.01) different from one another. When surrounded by 3 layers of lard the reported BMD was 20.5% greater than the reported BMD when the bone was not surrounded by any lard. The differences between the actual amount of fat measured by chemical analysis and weighing, and the reported measurement of fat by iDXA were significant with all 3 thicknesses of lard (P<0.01); the percentage difference between the fat measured by iDXA and that measured chemically decreased as the number of layers of lard increased.
Conclusion
We found that iDXA overestimated fat by up to 11.1%. The percentage overestimation of fat diminished as the amount of fat increased. BMD was overestimated by 20.5% when surrounded by 3 layers of fat compared to when there was no surrounding fat. In contrast to fat, the percentage overestimation of BMD increased as increasing amounts of fat surrounding the bone Using earlier generation DXAs, others have reported that measurements were ± 20–50% inaccurate and differed according to the configuration of the phantoms. The measurement of BMD and fat is the main clinical purpose of iDXA; the present experiment has shown that there are substantial inaccuracies in the measurement of BMD and fat. It is not known how these inaccuracies compare with those of earlier generations of DXA machines.
Introduction
We have not found previous reports comparing the measurement of fat by DXA or iDXA with the actual amount of fat measured chemically. Thus we were interested to see how accurate were the measurements of fat by iDXA. We were also interested to see how accurate were the measurements of BMD by iDXA, as older generations of DXA machines were reported to be inaccurate in obese subjects. Inaccuracies were also reported in the measurement of BMD of the hip when it was internally or externally rotated [1]. Bolotin et al [2] showed that only relatively small extraosseous soft tissue inhomogeneities within the region of interest (ROI) of DXA scans can increase substantially the already sizable inaccuracies which they had shown earlier with uniformly distributed extraosseous soft tissues. The extent of these in vivo inaccuracies depended on the mean extraossous fat to lean areal density ratio and its degree of nonuniformity within the ROI. They found that in many cases, inaccuracies can be as large as 20–50%, particularly in osteopenic, osteoporotic, and elderly patients.
Given this background, we were interested to determine the accuracy of the current generation of DXA machines represented by the Lunar iDXA (GE-Healthcare, software version 11.4).
Methods
We performed measurements of fat and BMD of a beef bone surrounded by one, then two, and then finally three layers of lard. The bone was defatted by prolonged boiling in a detergent. Initially the bone was placed in the marked spine area overlying a 6L plastic bottle which was placed in the marked trunk area of an iDXA within the outline created by the machine to measure the human spine on the scanner table. The lard layers were wrapped around the bone to enclose it completely. The lard layers were weighed on a standard scale and the layers were determined by chemical analysis to be 77.46% fat (by weight). Thus the weight of fat in the lard was 0.7746 X the weight of lard (in Kg). The plastic bottle was then removed and further measurements were carried out with increasing thicknesses of lard surrounding the bone. The distance of the beef bone from the scanner was approximately the same as the distance of the spine from the scanner during a whole body scan of a human subject lying supine on the table of the iDXA machine. Measurements by iDXA, of BMD of the beef bone and the amount of fat surrounding it were done with one, two and then three layers of lard around the bone. The thickness of each lard layer was measured with calipers three times (layers were 1.5, 1, and 1cm thick). Each configuration of beef bone surrounded by fat was scanned four times. The iDXA machine printed out the results using the parameters of human whole body analysis with appendicular readings as zero as emphasis was on truncal fat and spinal BMD.
Statistical methods
Descriptive statistics, mean and standard deviation, were calculated for fat and BMD for each layer of lard. The t test was used to test the null hypothesis that the mean fat by iDXA was equal to the measured fat by chemical analysis. Separate analyses were performed for each layer of lard. An analysis of variance was used to test the null hypothesis that the means of the measured BMD by iDXA were equal for all layers of fat. Multiple comparisons among the means were performed using the Sidak Procedure. Linear regression was used to model the relationships between the mean values of fat and BMD by iDXA and the fat measured by chemical analysis. All statistical calculations were performed by STATA. The level of significance for all statistical tests of hypothesis was P ≤ 0.05.
Results
Table 1 shows that iDXA overestimated fat (determined chemically) with all three layers of lard, although the percentage error decreased as the number of layers of lard increased. iDXA measured fat is between 144 – 187 g more than the amount of fat determined chemically for each of the configurations of lard surrounding the bone. This relationship shows that as the amount of lard surrounding the bone increased, the percentage difference between iDXA measured fat and chemically determined fat, decreased.
Table 1.
Descriptive Statistics for Fat Measurments
| Lard Layers | Fat (g) | iDXA Fat Measurement (g) | Percent error | |
|---|---|---|---|---|
| Mean | Standard Deviation | |||
| 0 | 0 | 301 | 20 | |
| 1 | 1295 | 1439 | 2 | 11.1% |
| 2 | 2268 | 2455 | 10 | 8.2% |
| 3 | 3097 | 3283 | 9 | 6.0% |
Note: 1. Mean iDXA Fat Measurement was significantly greater than the fat by chemical analyses for all lard layers (P < 0.001).
2. Percent Error = 100(iDXA Fat − Fat)/Fat
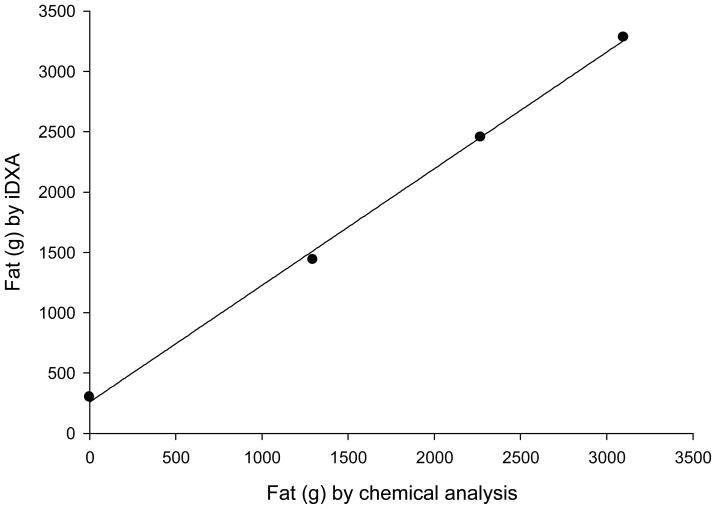
Figure 1 is a scatter plot illustrating the relationship between mean fat measured by iDXA and fat by chemical analysis. The solid line in the figure is the regression equation relating iDXA fat to fat by chemical analysis:
Figure 1.
Relationship of fat mass (g) as determined by chemical analysis versus fat mass (g) determined by iDXA.
The slope was not significantly different from unity (P=0.347); however, the line was significantly different from the line of identity (P=0.043). The intercept was significantly greater than zero (P=0.042).
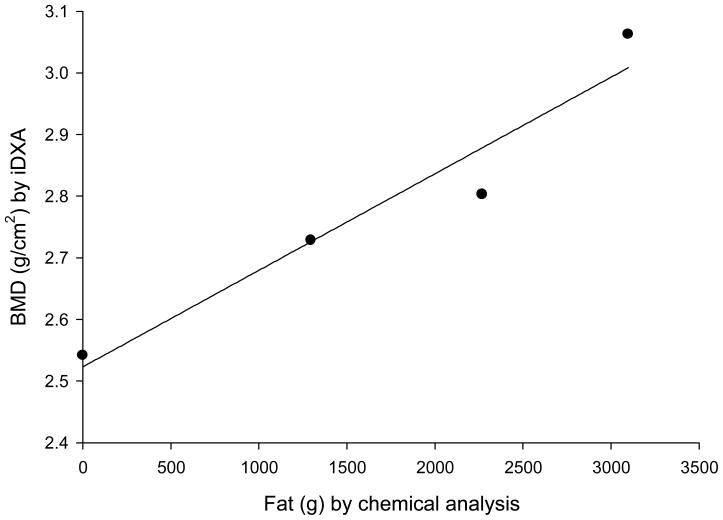
Table 2 shows that the measured BMD by iDXA increased as the number of layers of lard surrounding the beef bone increased, so that with 3 surrounding layers of lard (3097 g fat), the measured BMD was 20.5% greater than when there was no lard surrounding the bone. This relationship is shown graphically in Figure 2. The solid line in the figure is the regression equation relating iDXA mean BMD to fat by chemical analysis:
Table 2.
Descriptive Statistics for BMD Measurments
| Lard Layers | Fat (g) | iDXA BMD Measurement (g/cm2) | Percent error | |
|---|---|---|---|---|
| Mean | Standard Deviation | |||
| 0 | 0 | 2.542 | 0.013 | |
| 1 | 1295 | 2.729 | 0.007 | 7.4% |
| 2 | 2268 | 2.803 | 0.004 | 10.3% |
| 3 | 3097 | 3.063 | 0.013 | 20.5% |
Note: 1. Mean iDXA BMD Measurements were significantly different from each other (P < 0.001).
2. Percent error = 100(at Layer_i − 2.542)/2.542 for i=1,2,3
Figure 2.
Relationship of fat mass (g) as determined by chemical analysis and bone mineral density (BMD) determined by iDXA.
The slope was significantly greater than zero (P=0.033). Using this equation, one kilogram increase in lard increases the BMD measurement by 0.157 g/cm2 (6.2% of the measured BMD without lard).
Discussion
This study shows that the measurement of BMD of a beef bone by iDXA was increased by 21% when it was surrounded by 3 layers of lard. The close linear relationship between the measured BMD and the quantity of fat surrounding the bone, suggests that the absorption of photons by fat gives a spuriously high reading of BMD, and that this effect has nothing to do with changes in the configurations of fat and bone, which as noted below, also spuriously alter measured BMD. The measurement of fat was increased by up to 11% compared with the amount of fat measured chemically, with a lesser percent increase in the measured fat as the total amount of fat was increased.
The precision achieved in measuring BMD by DXA is around 1% [3], but accuracy is considerably worse, due to inhomogeneous distribution of fat and lean, and errors of 20–50% have been reported in vitro (using phantoms with different configurations of lean, fat, and bone) and in vivo in DXA measurements by the older pencil beam DXA machine [2]. The accuracy of iDXA in measuring BMD has not been previously reported to our knowledge. In another in vitro study using a different phantom configuration, we have found that iDXA overestimated fat by 2–29%, and underestimated BMD by 7.2% with the thickest layer of lard [4]. Thus the measurements of BMD, BMC, and fat by iDXA are changed by the configuration of the phantom in relation to fat, or bone in relation to fat, emphasizing that the configuration of fat and bone have a marked influence on the results of fat and bone reported by iDXA. This accords with the findings of Bolotin et al when they used the older DXA machine to measure phantoms of fat, bone, and lean arranged in different configurations. Weigart and Cann compared spinal T scores determined by DXA with spinal T scores determined by quantitative CT (QCT) in control and obese groups. Their results suggested that DXA scanning in obese patients can have substantial errors, overestimating BMD by 1 or 2 T score units and causing misdiagnosis of the patient if DXA is used as the primary diagnostic methods. They stated that DXA may not be a suitable technique for evaluation of spinal BMD and QCT may be a more accurate alternative [5]. Others have reported similar findings [6, 7].
Bolotin pointed out that in anatomically realistic simulations studies based on a cadaveric lumbar vertebra and a broad range of soft tissue anthopometric representations, inaccuracies in DXA measurement may exceed 20% at lumbar vertebral sites, especially for osteopenic/osteoporotic postmenopausal, and elderly patients [8].
In a cadaver study, Goh et al [1] reported that precision in proximal femur bone density testing was highly dependent on the amount of rotation of the proximal femur from study to study. Internally rotating the femur 15 to 20° provided the lowest values (for the femoral neck). If the femoral neck rotation was increased or decreased, the value increased by as much as 52%. However, iDXA measurements of human subjects are carried out in such a way that the configuration of bone, fat, and lean body mass is fairly constant – when the subjects are of similar build. Thus one subject can be compared to another, although the absolute values of BMD, BMC, and fat may not be accurate. These comparisons are less valid, when the subjects used in the control data base are of different build from the subjects being measured. Thus DXA or iDXA may be more accurate for measuring BMD in normal subjects than in abnormally thin or abnormally fat subjects - in whom the measurement is extremely important.
Our study demonstrates that iDXA suffers limitations similar to those that have been found with the older DXA machines. It is unclear whether iDXA is more accurate than DXA in measuring fat and bone. This inaccuracy represents a serious limitation in the use of this technology for reliably evaluating BMD in patients, and comparing BMD in subjects of different builds because patients may be categorized into an artifactually reduced or increased fracture risk
References
- 1.Goh JC, Low SL, Bose K. Effect of femoral rotation on bone mineral measurements with dual energy X-ray absorptiometry. Calcif Tissue Int. 1995;57:340–3. doi: 10.1007/BF00302069. [DOI] [PubMed] [Google Scholar]
- 2.Bolotin HH, Sievanen H, Grashuis JL. Patient specific DXA bone mineral density inaccuracies: Quantitative effects of nonuniform extraosseous fat distributions. J Bone Miner Res. 2003;18:1020–7. doi: 10.1359/jbmr.2003.18.6.1020. [DOI] [PubMed] [Google Scholar]
- 3.Michael GJ, Henderson CJ. Monte Carlo modeling of an extended DXA technique. Phys Med Biol. 1998;43:2583–96. doi: 10.1088/0031-9155/43/9/011. [DOI] [PubMed] [Google Scholar]
- 4.Javed F, Wang J, Colt E, Allen L, Yu W, Thornton J, Gallagher D. The validity of iDXA in determining bone mineral content (BMC), bone mineral density (BMD) and body fat (BF with changes in subcutaneous tissue thickness (STT) Int J Body Comp Res. 2008;6(74):15-P. [Google Scholar]
- 5.Weigert JM, Cann CE. Dual energy X-ray absorptiometry (DXA) in obese patient: Are normal values really normal? J Women’s Imaging. 1999;1:11–7. [Google Scholar]
- 6.Guiglielmi G, Grimston SK, Fischer KC, Pacifici R. Osteoporosis: Diagnosis with lateral and posteroanterior dual X-ray absorptiometry compared with quantitative CT. Radiology. 1994;192:845–50. doi: 10.1148/radiology.192.3.8058958. [DOI] [PubMed] [Google Scholar]
- 7.Grampp S, Genant HK, Mathur A, et al. Comparison of noninvasive bone mineral measurement in assessing age-related loss, fracture discrimination, and diagnostic classification. J Bone Miner Res. 1997;12:697–711. doi: 10.1359/jbmr.1997.12.5.697. [DOI] [PubMed] [Google Scholar]
- 8.Bolotin H. Inaccuracies inherent in DXA absorptiometry in vivo may flaw osteopenic/osteoporotic interpretations and mislead assessment of antiresorptive therapy effectiveness. Bone. 2001;28:548–55. doi: 10.1016/s8756-3282(01)00423-9. [DOI] [PubMed] [Google Scholar]