Abstract
Veterans have unique risk factors for cancer and comorbidities that may complicate cancer survivorship care. These population-specific characteristics compel research into the needs of veteran cancer survivors to inform best practice.
The lifetime risk of receiving a diagnosis of cancer is about one in two (40.35%) for every man and woman born in the United States today.1 Incidence rates for many cancers continue to rise, such as cancers of the liver, pancreas, kidney, esophagus, thyroid, brain, and bladder; non-Hodgkin lymphoma; leukemia; and myeloma, as well as melanoma of the skin in women, testicular cancer in men, and childhood cancers.1 Fortunately, due to improvements in the detection and treatment of cancer, survival rates are increasing. Indeed, death rates for the four most common cancers—prostate, breast, lung, and colorectal—and for all cancers combined continue to decline.1
Traditionally, survival has been the primary (and often only) concern of patients diagnosed with cancer. With the increasing number of cancer survivors, however, greater attention is now focused on the long-term health consequences of cancer and its treatment. Cancer treatments, for instance, can cause chronic and late appearing problems throughout the body, including the mouth and teeth; eyes; liver; kidneys; bone and soft tissue; respiratory, gastrointestinal, and genitourinary tracts; and the cardiovascular, endocrine, hematologic, immune, lymphatic, and nervous (central and peripheral) systems.2 In addition, treatment for cancer can cause second cancers.
Although most patients with cancer report improved health-related quality of life within 12 months after cancer treatment,3–5 some symptoms, such as fatigue, can long persist. Many physical symptoms may recede with time or diminish because of active interventions by the patient. Other adverse effects of cancer treatment, however, may worsen over time. For example, patients with prostate cancer who are treated with radiation experience worsening erectile dysfunction over time.4 Additionally, psychological symptoms, such as depression and anxiety, are common in cancer survivors, as are problems with employment, insurance, and social functioning.2 These psychosocial factors also may play a significant role in the trajectory of cancer treatment and recovery.
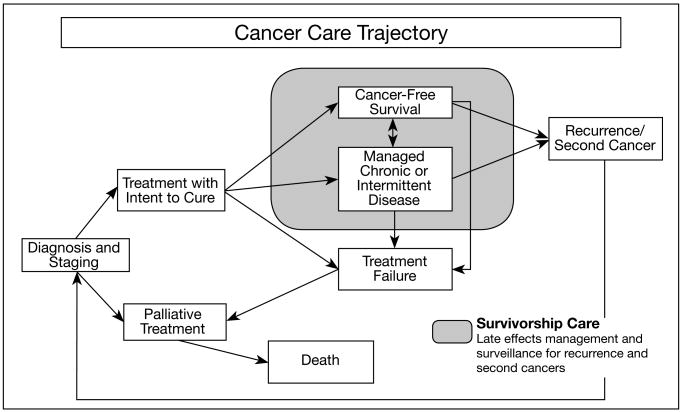
Cancer survivorship care involves medically addressing the long-term and late appearing adverse effects of cancer therapy and managing chronic and intermittent cancer (Figure).2 Cancer survivors also may need support and intervention as they negotiate the psychological and social complexities of cancer recovery. All the while, they must remain alert to possible recurrence or second cancers and cope with anxiety as they anticipate potential treatment failures.
Figure.
Cancer care trajectory.2 Reprinted with permission from the National Academies Press, Copyright 2005, National Academy of Sciences.
There are now 11 million cancer survivors in the United States,1 whose needs are receiving growing attention from the National Cancer Institute (NCI), the CDC, and other agencies. We aim to call attention to the growing prevalence of cancer survivors within the VA and the dearth of data specific to the needs of these cancer survivors. To help accomplish this, we examined and report here on the prevalence of cancer survivors within the VA for fiscal year 2007 and compare our findings to prevalence rates for the general U.S. population. We also summarize common symptom concerns of cancer survivors and outline care models that show promise in meeting the unique physical, emotional, functional, and social challenges veterans face following cancer treatment.
Cancer in the VA: Policies and Directives
In addition to the cancer risk factors common in the general population, veterans have unique risk factors for particular cancers that are associated with military-related exposures. As of October 2009, the VA recognized 15 conditions as presumptively caused by exposure to the herbicide Agent Orange, including prostate, respiratory, and certain hematologic cancers and soft tissue sarcomas.6
In addition, combat-exposed veterans have high rates of posttraumatic stress disorder (PTSD), which have the potential to complicate psychosocial adjustment after cancer treatment as any cancer-related anxiety and depression interface with military-related PTSD.7 PTSD also may lead to higher rates of substance abuse, increasing the risk of developing some cancers. Furthermore, many older veterans have one or more comorbid conditions (including diabetes, congestive heart failure, and chronic obstructive pulmonary disease) that can negatively impact the morbidity and mortality of cancer survivors.8
VHA Directive 2003-034, VHA National Cancer Strategy, recognizes the severe and unique burden of cancer, including the potential psychological impact it may have, noting that cancer is “Arguably,…most feared of diseases, and its diagnosis imposes a significant emotional burden on both patients and their families.”9 Although the VHA strategy doesn't offer specific pathways to implementation, it offers objectives to ensure quality of care, to enhance access to care, to facilitate continuing care, and to contribute to the common good by establishing a national model for a systematic approach to the problem of cancer. The strategy emphasizes that, as the veteran population ages, the encumbrance to implement a national cancer strategy will increase.
VA Cancer Survivorship: Prevalence Rates and Characteristics
We examined the complete prevalence of cancer survivorship in veterans, following the Surveillance Epidemiology and End Results (SEER) method of the NCI, by calculating the percentage of people alive on a certain date in a population who previously had a diagnosis of the disease. Prevalence rates for cancer diagnoses were extracted from the VA Patient Treatment Files and Outpatient Care Files, part of the National Patient Care Database located at the Austin Automation Center, for 4,991,231 veteran patients who were alive in fiscal year 2007. Patient data were then sorted by age and grouped by primary cancer organ site. We then extracted similar statistics for the U.S. population using the Cancer Query System of the SEER web-based data extraction interface.10
The data extraction method we employed is limited by potential omissions on the patient problem list. As such, it may underestimate the true prevalence of cancer among veterans. The reliability of administrative records from the VA Patient Treatment and Outpatient Care Files has been validated previously by chart review for a wide spectrum of diagnostic categories, including cancer.11–13
In our extraction of VA data files, we found that 524,052 (11%) of veterans who were treated in the VA in fiscal year 2007 are cancer survivors according to the patient problem list (Table). The most common cancer types were prostate, skin (nonmelanoma), and colorectal, although relative prevalence varied by age, with younger adults more commonly diagnosed with blood, skin, thyroid, and melanoma neoplasms.
Table. Prevalence of cancer diagnoses among veterans treated in the VHA in fiscal year 2007.
| Type of cancer | Age, in years | ||||
|---|---|---|---|---|---|
| ≤ 39 | 40–59 | 60–79 | ≥ 80 | All ages | |
| Prostate | 49 | 18,476 | 13,1582 | 63,668 | 213,775 |
| Skin | 453 | 14,611 | 49,118 | 23,210 | 87,392 |
| Colorectal | 126 | 6,511 | 24,106 | 10,516 | 41,259 |
| Bladder | 42 | 3,150 | 17,438 | 8,902 | 29,532 |
| Lung and related | 48 | 4,695 | 18,102 | 5,259 | 28,104 |
| Head and neck | 220 | 8,799 | 16,806 | 3,406 | 29,231 |
| Blood | 555 | 4,728 | 13,730 | 5,326 | 24,339 |
| Melanoma | 247 | 2,754 | 7,874 | 2,798 | 13,673 |
| Kidney and related | 78 | 3,019 | 8,046 | 2,394 | 13,537 |
| Breast | 147 | 2,712 | 2,087 | 1,036 | 5,982 |
| Thyroid | 287 | 1,582 | 2,128 | 450 | 4,447 |
| Gastric/digestive | 20 | 758 | 2,175 | 850 | 3,803 |
| Esophageal | 20 | 787 | 2,374 | 594 | 3,775 |
| Lymph system | 50 | 1,162 | 2,088 | 433 | 3,733 |
| Liver | 11 | 1,233 | 1,477 | 341 | 3,062 |
| All other | 1,154 | 6,393 | 8,626 | 2,235 | 18,408 |
| Total | 3,507 | 8,1370 | 307,757 | 131,418 | 524,052 |
| % of all survivors | 1 | 16 | 59 | 25 | 100 |
Veterans vs. general U.S. population
In comparing our extraction of VA data files with U.S. SEER data files we found that the VA patient population is older than the general U.S. population. More than half (56%) of veterans who receive care within the VA are older than 60 years. As such, 84% of VA cancer survivors are older than 60 years, whereas 70% of cancer survivors are older than 60 years in the general U.S. population
The VA patient population is disproportionately male: 91% of veterans treated within the VA are male. Because of this, 97% of VA cancer survivors are male, compared with 45% of cancer survivors in the general U.S. population.
As a result of differences in age, gender, and risk factors, cancer site prevalence statistics vary between the VA and general U.S. cancer patient populations. For instance, 41% of veteran patients who are cancer survivors have had a diagnosis of prostate cancer, compared with 30% of general U.S. cancer survivors. And only 1% of veteran patients are breast cancer survivors, compared with 23% of general U.S. cancer survivors. More common cancer site diagnoses in the veteran cancer survivor population, compared with the general U.S. cancer survivor population, include the lung (5% versus 3%), head and neck (6% versus 3%), and esophagus (0.7% versus 0.2%). Although the rates of colorectal and hematologic cancers are considerable in the veteran patient population (8% and 5%, respectively), these rates are slightly higher in the general U.S. cancer population (10% and 8%, respectively).
Common Symptoms Experienced by Cancer Survivors
What makes cancer survivorship care unique from the posttreatment phase of other life threatening illnesses? From a physical standpoint, many treatments for cancer are quite invasive (such as surgical removal of the esophagus) with high toxicity (chemotherapy or radiation therapy), creating long standing physical sequelae. From a psychological standpoint, the patient's appraisal of threat when given a diagnosis of cancer is, for many, significant and sustained. Additionally, the experience of the diagnosis and the treatment (for example, bone marrow transplant) can be traumatic, and the threat of recurrence of the trauma is repeatedly reinvoked during routine surveillance or when symptoms reminiscent of the cancer occur.
Four common concerns that are reported by cancer survivors are sexual dysfunction, fatigue, anxiety, and depression.
Sexual dysfunction
Sexual problems are some of the most prevalent long-term complications after cancer treatment in both men and women.14 There are multiple dimensions to sexual function; alterations in physiologic, psychological, or social components of sexuality 15,16 can affect quality of life.16
Changes in sexual function following cancer diagnosis and treatment can have multiple etiologies that vary by cancer site, treatment type, and time since treatment. For instance, surgery, chemotherapy, and radiation treatment may result in direct physiologic interference with sexual function (such as disfigurement, loss of body part, or damage to pelvic neurovascular bundle).17 Ongoing adverse effects of treatment, including diarrhea and urinary incontinence, also may affect sexual desire and activity.18 In addition, sexual problems may stem from hormone therapy, changes in hormonal serum levels, disturbances in body image, symptoms of depression or anxiety, and alterations in relationships.19
Fatigue
Although less well studied than sexual function, fatigue is another common report among cancer survivors. For some survivors, fatigue resolves within 12 months; for others, it persists for years.16,20
Elevated inflammatory processes may contribute to chronic fatigue associated with cancer.21 Fatigue in cancer survivors is also associated with psychological distress and physical disability.22 In older adults, both cancer history and age predict functional disability associated with fatigue.23 Persistent problems with fatigue may affect vocational and leisure readjustment.24
Anxiety and depression
Cancer survivors report symptoms of emotional distress as a consequence of a cancer diagnosis and treatment—as diagnoses, treatments, and recurrences may instigate cycles of disbelief, dysphoria, and adaptation.25 Up to 67% of patients report symptoms of PTSD brought on by their experiences with cancer, such as intrusive memories and dreams, in the first year following cancer treatment.26,27 Whether these symptoms persist is impossible to determine conclusively, since most studies of cancer survivors are cross-sectional and involve participants who are anywhere from one to 20 years post-diagnosis.
Despite the high percentage of cancer survivors experiencing PTSD symptoms after cancer treatment, few meet the criteria for a PTSD syndrome. Existing models of PTSD do not fit completely with the prospective anxiety experienced by cancer survivors.28 As much as 30% to 40% of cancer survivors report ongoing fears of recurrence and of diagnostic tests.29 In fact, according to a survey of primary care physicians practicing in the southeastern United States, addressing patients' fears of cancer recurrence and death is among the most difficult challenges of treating cancer survivors.30
Patients recovering from cancer also may experience depression. Up to 43% of cancer survivors report depressive symptoms, and 26% meet criteria for a depression diagnosis.31 Depression often results in significant additional disability in survivors who already are struggling to deal with their medical condition. The risk of developing depressive symptoms is highest in the first year following treatment; studies conflict as to whether the depression risk continues to be higher in long-term cancer survivors or whether the risk is equal to that of the general population.32,33
Recommendations for VA research
The current medical literature on the problems experienced by cancer survivors is limited. Most studies focus on middle-aged survivors of breast, blood, and prostate cancers. There is little to no research involving survivors of other types of cancer. And, other than studies of prostate cancer survivors that include veterans, little research has been published addressing cancer survivorship among veteran populations. (An electronic search of EBSCOhost's Academic Search Premier and Military and Government Collection databases and PsycARTICLES for the keywords “veteran(s)”, “cancer”, and “survivor(s)” in the title or abstract yielded no results.)
Given that the veteran cancer survivor population is older than the general population, it is crucial to have more data specific to older cancer survivors: These patients are more likely to have disease comorbidity; to be concerned with maximizing functional abilities; and, when undergoing treatment, to be sensitive to cardiac, kidney, and liver toxicities. In addition, older patients with cancer are more likely to have physical and functional limitations than older adults without cancer. They also report longer periods of disability than older adults without cancer,34 although the trajectories of disability are poorly understood.35 In the general older adult population, limitations in functioning impair capacities to remain independent when it comes to valued activities, such as sexual activity and daily self-care.36
Differences between the general population of cancer survivors and veteran cancer survivors warrant veteran-specific research, including the role of military exposures (combat, radiation, and herbicides) and their sequelae (including PTSD) in causing cancer or intersecting with persisting symptoms and the course of recovery after treatment. Such research should pay special attention to survivorship for cancers common in the veteran population, including prostate, colorectal, urinary tract (bladder and kidney), lung, head and neck, blood, and digestive tract (esophageal, stomach, and intestine) cancers. The VA offers ample opportunity for multisite designs that allow for sufficient sample size, particularly for understudied cancers. In these studies, it will be crucial to consider functional capacities that are especially at risk for decline in older patient populations (such as balance, strength, cognition, and activities of daily living) and psychological conditions that are more prevalent in combat-exposed individuals (such as PTSD and depression).
While it is important that these studies be comprehensive, it can be challenging to assess all variables of interest adequately without overburdening research participants. Another challenge will be maintaining a clear theoretical model and statistical design approach in the face of multiple interacting variables. To construct accurate evidence-based models of the variables most predictive of health outcomes over time, longitudinal research is imperative.
Models of Cancer Survivorship Care
Four models of care may be relevant to improving care for veteran cancer survivors: (1) cancer survivorship clinics, (2) cancer care transition plans, (3) rehabilitation, and (4) chronic disease management.
Cancer survivorship clinics
Increasingly national cancer centers are developing clinical services specific to cancer survivors, in the form of cancer survivorship clinics. Although there is no consistent set of characteristics that define these clinics, they offer treatment, consultative care, and psychosocial interventions by a team of interdisciplinary providers who are expert in posttreatment and survivorship care. Advanced practice nurses often take the lead in posttreatment symptom management in these clinics.
Despite the clear benefits, such a model of care may risk dissociating the cancer survivorship care from ongoing primary care provided by the patient's internist or geriatrician. If this model were to be enacted within the VA, appropriately trained advanced practice nurses and psychosocial clinicians would need to be recruited from national cancer centers, or existing VA staff would require appropriate training.
Cancer care transition plans
Another model of cancer survivorship care rests on the creation of a “transition plan” by the oncology provider to ease the patient's transition back to primary care after cancer treatment and to facilitate coordination of care and referral to appropriate specialists for follow-up on specific concerns. Such transition plans have received much attention and are endorsed by the Institute of Medicine (IOM),2 the American Society of Clinical Oncology (ASCO),37 the NCI, and the CDC. They have not, however, been considered for endorsement within the VA. Model transition plans established by the IOM and ASCO create a record of cancer care (which consists of critical information for the patient to carry to subsequent providers, particularly those outside the patient's current care system) and provide standards for surveillance, information on possible late and long-term effects of treatment, and lists of resources.
While these transition care plans represent an important advance in cancer survivor treatment, their primary emphasis is to create a record of care. These plans do not appear to be necessarily focused on the patient's goals for care going forward or to be adapted to the needs of older patients (the majority of survivors). These needs tend to focus on preservation of independent function and quality of life in the face of aggressive treatment.38 Nor have these plans been adapted for veteran patients, whose treatment needs may differ and whose health system offers opportunities for coordination of care through the computerized patient record system (CPRS).
Rehabilitation
The VA National Cancer Strategy states that rehabilitation is an integral component of cancer care and requires every facility caring for patients with cancer to provide such services. Rehabilitation is a useful framework for viewing the concerns of cancer survivors because the long-term sequelae of cancer and its treatment may require accommodations similar to those in other VA rehabilitation populations (such as spinal cord injury, traumatic brain injury, and serious mental illness). For example, a veteran with urinary or bowel incontinence may need to negotiate new job requirements and conditions (a workstation near a restroom and the ability to leave the work environment frequently to urinate) to maintain employment.
Rehabilitation from cancer can be conceived as having two components: (1) recovery from physical and psychological dysfunction and return to homeostasis and (2) adaptation to losses in function for those symptoms that do not remit. In addition, “prehabilitation” (rehabilitation that takes place before the injury) programs may be particularly effective at providing focused physical therapy, gait and mobility training, and symptom management for older veterans,39 both before and during cancer treatment.
Chronic disease management
A targeted symptom management model, which uses nurse-assisted management and cognitive-behavioral therapies, has been successful at reducing such cancer-associated symptoms as depression, anxiety, fatigue, and pain.40 These models of symptom management are conceptually similar to those used in chronic disease management. The comanagement by internists and other specialists of chronic diseases during or immediately after active cancer chemotherapy however, has not been tested. The integration of chronic care models for such comorbid conditions as diabetes and heart failure may improve the survival and quality of life among cancer survivors further, given the increased mortality associated with these comorbid conditions.8,41 Modification of existing symptom management strategies may be an efficient and effective way of integrating chronic disease management into cancer care and survivorship.
Recommendations for VA research
Innovative features of VA care (including integrated mental health care, strong geriatrics and extended care, integrated pharmacy and laboratory services, and electronic medical records) offer a unique opportunity to test components of the different cancer survivorship care models alone and in various combinations to determine which is most effective in providing coordinated care and better long-term outcomes. For example, survivor care plans could be created by cancer care providers in collaboration with the veteran patient and integrated into the CPRS. Alerts could be created to remind providers to screen for late-stage complications of cancer treatment associated with chemotherapy or to make recommendations for radiographic surveillance that consider the patient's cumulative radiation exposure. Integrating the survivorship care and transition plan into the CPRS also could facilitate needed referrals to psychosocial, rehabilitation, and other services to offer survivors necessary follow-up care to maintain and improve posttreatment functional status and quality of life. The survivorship care plan also could be linked to MyHealthe-Vet to promote self-care for veteran patients who are using care models already developed for chronic disease management in veterans.
Conclusions
Due to improvements in the detection and treatment of cancer, the number of patients surviving cancer in the short or long term is increasing. Cancer survivorship care must integrate the physical and mental health needs of survivors; address potential functional declines and social consequences; and involve coordination across oncology, primary, and mental health care providers. A number of care models—cancer survivorship clinics, cancer care transition plans, rehabilitation, and chronic disease management—need development, testing, and appropriate implementation within the VA. It will be crucial to balance services that meet the unique needs of veteran cancer survivors with the need to integrate treatment for cancer survivorship symptoms with other ongoing medical and mental health treatment.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Boston VA Medical Center and the Boston VA Research Institute, both in Boston, MA, for Drs. Moye and Schuster. Additional support was provided by the Houston VA Health Services Research & Development Center of Excellence (HEP90-020) at the Michael E. DeBakey VA Medical Center, Houston, TX for Drs. Naik and Latini. Dr. Latini is supported by Mentored Research Scholar Grant 06-083-01-CPPB from the American Cancer Society. We thank the VA South Central (VISN 16) Mental Illness Research, Education, and Clinical Center (MIRECC), North Little Rock, AR, who performed the national data extraction. Additional support is from National Institute of Aging Career Development Award (5K23AG027144) and a Doris Duke Charitable Foundation Clinical Scientist Development Award given to Dr. Naik. We thank Elizabeth Archambault, Michele Karel, Mark Kunik, Kelly Trevino, and Hongjen Yu for their input. We are indebted to the many veterans who have allowed us to participate in their health care and who have contributed to our research studies.
Footnotes
Disclaimer: The opinions expressed herein are those of the authors and do not necessarily reflect those of Albert Einstein College of Medicine, Federal Practitioner, Quadrant HealthCom Inc., the U.S. government, or any of its agencies. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
References
- 1.Horner MJ, Ries LG, Krapcho M, editors. SEER Cancer Statistics Review, 1975–2006. Bethesda, MD: National Cancer Institute; 2008. [February 23, 2010]. http://seer.cancer.gov/csr/1975_2006/. Updated January 28, 2010. [Google Scholar]
- 2.Hewitt M, Greenfield S, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 3.McQuellon RP, Russell GB, Rambo TD, et al. Quality of life and psychological distress of bone marrow transplant recipients: The ‘time trajectory’ to recovery over the first year. Bone Marrow Transplant. 1998;21(5):477–486. doi: 10.1038/sj.bmt.1701115. [DOI] [PubMed] [Google Scholar]
- 4.Lubeck DP, Litwin MS, Henning JM, Stoddard ML, Flanders SC, Carroll PR. Changes in health-related quality of life in the first year after treatment for prostate cancer: Results from CaPSURE. Urology. 1999;53(1):180–186. doi: 10.1016/s0090-4295(98)00408-7. [DOI] [PubMed] [Google Scholar]
- 5.Abendstein H, Nordgren M, Boysen M, et al. Quality of life and head and neck cancer: A 5 year prospective study. Laryngoscope. 2005;115(12):2183–2192. doi: 10.1097/01.MLG.0000181507.69620.14. [DOI] [PubMed] [Google Scholar]
- 6.Agent Orange: Diseases associated with Agent Orange exposure. US Dept of Veterans Affairs, Office of Environmental Health and Hazards web site. [March 1, 2010]; http://www.publichealth.va.gov/exposures/agentorange/diseases.asp#veterans. Updated January 8, 2010.
- 7.Andrykowski MA, Cordova MJ. Factors associated with PTSD symptoms following treatment for breast cancer: Test of the Andersen model. J Trauma Stress. 1998;11(2):189–203. doi: 10.1023/A:1024490718043. [DOI] [PubMed] [Google Scholar]
- 8.Gross CP, Guo Z, McAvay GJ, Allore HG, Young M, Tinetti ME. Multimorbidity and survival in older persons with colorectal cancer. J Am Geriatr Soc. 2006;54(12):1898–1904. doi: 10.1111/j.1532-5415.2006.00973.x. [DOI] [PubMed] [Google Scholar]
- 9.Veterans Health Administration . VHA Directive 2003-034: National Cancer Strategy. Washington, DC: US Dept of Veterans Affairs, Veterans Health Administration; Jun 20, 2003. [February 19, 2010]. http://www1.va.gov/cancer/docs/NationalCancerDirective.doc. [Google Scholar]
- 10.Surveillance Epidemiology and End Results: Cancer query systems. National Cancer Institute web site. [March 1, 2010]; http://seer.cancer.gov/canques/index.html.
- 11.Kashner TM. Agreement between administrative files and written medical records: A case of the Department of Veterans Affairs. Med Care. 1998;36(9):1324–1336. doi: 10.1097/00005650-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Abraham NS, Gossey JT, Davila JA, Al-Oudat S, Kramer JK. Receipt of recommended therapy by patients with advanced colorectal cancer. Am J Gastroenterol. 2006;101(6):1320–1328. doi: 10.1111/j.1572-0241.2006.00545.x. [DOI] [PubMed] [Google Scholar]
- 13.Kramer JR, Davila JA, Miller ED, Richardson P, Giordano TP, El-Serag HB. The validity of viral hepatitis and chronic liver disease diagnoses in Veterans Affairs administrative databases. Aliment Pharmacol Ther. 2008;27(3):274–282. doi: 10.1111/j.1365-2036.2007.03572.x. [DOI] [PubMed] [Google Scholar]
- 14.Ananth H, Jones L, King M, Tookman A. The impact of cancer on sexual function: A controlled study. Palliat Med. 2003;17(2):202–205. doi: 10.1191/0269216303pm759oa. [DOI] [PubMed] [Google Scholar]
- 15.Tierney DK. Sexuality: A quality-of-life issue for cancer survivors. Semin Oncol Nurs. 2008;24(2):71–79. doi: 10.1016/j.soncn.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 16.Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112(suppl 11):2577–2592. doi: 10.1002/cncr.23448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monga U, Kerrigan AJ, Thornby J, Monga TN, Zimmermann KP. Longitudinal study of quality of life in patients with localized prostate cancer undergoing radiotherapy. J Rehabil Res Dev. 2005;42(3):391–399. doi: 10.1682/jrrd.2004.06.0071. [DOI] [PubMed] [Google Scholar]
- 18.Ganz PA, editor. Cancer Survivorship: Today and Tomorrow. New York, NY: Springer; 2007. [Google Scholar]
- 19.Gotay CC, Muraoka MY. Quality of life in long-term survivors of adult-onset cancers. J Natl Cancer Inst. 1998;90(9):656–667. doi: 10.1093/jnci/90.9.656. [DOI] [PubMed] [Google Scholar]
- 20.Donovan KA, Jacobsen PB, Andrykowski MA, et al. Course of fatigue in women receiving chemotherapy and/or radiotherapy for early stage breast cancer. J Pain Symptom Manage. 2004;28(4):373–380. doi: 10.1016/j.jpainsymman.2004.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Collado-Hidalgo A, Bower JE, Ganz PA, Irwin MR, Cole SW. Cytokine gene polymorphisms and fatigue in breast cancer survivors: Early findings. Brain Behav Immun. 2008;22(8):1197–1200. doi: 10.1016/j.bbi.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meeske K, Smith AW, Alfano CM, et al. Fatigue in breast cancer survivors two to five years post diagnosis: A HEAL Study report. Qual Life Res. 2007;16(6):947–960. doi: 10.1007/s11136-007-9215-3. [DOI] [PubMed] [Google Scholar]
- 23.Deimling GT, Bowman KF, Wagner LJ. The effects of cancer-related pain and fatigue on functioning of older adult, long-term cancer survivors. Cancer Nurs. 2007;30(6):421–433. doi: 10.1097/01.NCC.0000300168.88089.2b. [DOI] [PubMed] [Google Scholar]
- 24.Lee MK, Lee KM, Bae JM, et al. Employment status and work-related difficulties in stomach cancer survivors compared with the general population. Br J Cancer. 2008;98(4):708–715. doi: 10.1038/sj.bjc.6604236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spencer SM, Carver CS, Price AA. Psychological and social factors in adaptation. In: Holland JC, Breitbart W, Jacobsen PB, editors. Psycho-oncology. New York, NY: Oxford; 1998. pp. 211–222. [Google Scholar]
- 26.Kangas M, Henry JL, Bryant RA. Posttraumatic stress disorder following cancer: A conceptual and empirical review. Clin Psychol Rev. 2002;22(4):499–524. doi: 10.1016/s0272-7358(01)00118-0. [DOI] [PubMed] [Google Scholar]
- 27.Palmer BW, Dunn LB, Appelbaum PS, Jeste DV. Correlates of treatment-related decision-making capacity among middle-aged and older patients with schizophrenia. Arch Gen Psychiatry. 2004;61(3):230–236. doi: 10.1001/archpsyc.61.3.230. [DOI] [PubMed] [Google Scholar]
- 28.DuHamel KN, Ostrof J, Ashman T, et al. Construct validity of the posttraumatic stress disorder checklist in cancer survivors: Analyses based on two samples. Psychol Assess. 2004;16(3):255–266. doi: 10.1037/1040-3590.16.3.255. [DOI] [PubMed] [Google Scholar]
- 29.Deimling GT, Bowman KF, Sterns S, Wagner LJ, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15(4):306–320. doi: 10.1002/pon.955. [DOI] [PubMed] [Google Scholar]
- 30.Burg MA, Grant K, Hatch R. Caring for patients with cancer histories in community-based primary care settings: A survey of primary care physicians in the southeastern US. Prim health Care Res Devel. 2005;6(3):244–250. [Google Scholar]
- 31.Mehnert A, Koch U. Psychological comorbidity and health-related quality of life and its association with awareness, utilization, and need for psychosocial support in a cancer register-based sample of long-term breast cancer survivors. J Psychosom Res. 2008;64(4):383–391. doi: 10.1016/j.jpsychores.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 32.Honda K, Goodwin RD. Cancer and mental disorders in a national community sample: Findings from the national comorbidity survey. Psychother Psychosom. 2004;73(4):235–242. doi: 10.1159/000077742. [DOI] [PubMed] [Google Scholar]
- 33.Keating NL, Norredam M, Landrum MB, Huskamp HA, Meara E. Physical and mental health status of older long-term cancer survivors. J Am Geriatr Soc. 2005;53(12):2145–2152. doi: 10.1111/j.1532-5415.2005.00507.x. [DOI] [PubMed] [Google Scholar]
- 34.Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: Age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003;58(1):82–91. doi: 10.1093/gerona/58.1.m82. [DOI] [PubMed] [Google Scholar]
- 35.Schubert CC, Gross C, Hurria A. Functional assessment of the older patient with cancer. Oncology. 2008;22(8):916–922. [PubMed] [Google Scholar]
- 36.Naik AD, Concato J, Gill TM. Bathing disability in community-living older persons: Common, consequential, and complex. J Am Geriatr Soc. 2004;52(11):1805–1810. doi: 10.1111/j.1532-5415.2004.52513.x. [DOI] [PubMed] [Google Scholar]
- 37.American Society of Clinical Oncology . Cancer Treatment Plan and Summary. Alexandria, VA: American Society of Clinical Oncology; 2008. [November 28, 2008]. http://www.asco.org/ASCO/Downloads/Cancer%20Policy%20and%20Clinical%20Affairs/Quality%20of%20Care/Generic%20Treatment%20Plan%20and%20Summary%20Final%203.3.08.doc. [Google Scholar]
- 38.Fried TR, Bradley EH. What matters to seriously ill older persons making end-of-life treatment decisions?: A qualitative study. J Palliat Med. 2003;6(2):237–244. doi: 10.1089/109662103764978489. [DOI] [PubMed] [Google Scholar]
- 39.Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, Byers A. A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med. 2002;347(14):1068–1074. doi: 10.1056/NEJMoa020423. [DOI] [PubMed] [Google Scholar]
- 40.Given CW, Sikorskii A, Tamkus D, et al. Managing symptoms among patients with breast cancer during chemotherapy: Results of a two-arm behavioral trial. J Clin Oncol. 2008;26(36):5855–5862. doi: 10.1200/JCO.2008.16.8872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barone BB, Yeh HC, Snyder CF, et al. Long-term all-cause mortality in cancer patients with preexisting diabetes mellitus: A systematic review and meta-analysis. JAMA. 2008;300(23):2754–2764. doi: 10.1001/jama.2008.824. [DOI] [PMC free article] [PubMed] [Google Scholar]