Abstract
Serum opacity factor (SOF) is a streptococcal protein that disrupts the structure of human high density lipoproteins (HDL) releasing lipid-free apo A-I while forming a large cholesteryl ester-rich particle and a small neo HDL. Given its low cholesterol and high phospholipid contents, we tested the hypotheses that neo HDL is a better substrate for cholesterol esterification via lecithin:cholesterol acyltransferase (LCAT), better than HDL as an acceptor of THP-1 macrophage cholesterol efflux, and improves reduction of oxidized LDL-induced production of inflammatory markers. We observed that both cholesterol efflux and esterification were improved by recombinant (r)SOF treatment of whole plasma and that the underlying cause of the improved cholesterol esterification in plasma and macrophage cholesterol efflux to rSOF-treated plasma was due to the rSOF-mediated conversion of HDL to neo HDL. Moreover, the reduction of secretion of TNF-α and IL-6 by THP-1 cells by neo HDL was twice that of HDL. Studies in BHK cells overexpressing cholesterol transporters showed that efflux to neo HDL occurred primarily via ABCA1 not ABCG1. Thus, rSOF improves two steps in reverse cholesterol transport with a concomitant reduction in the release of macrophage markers of inflammation. We conclude that rSOF catalyzes a novel reaction that might be developed as a new therapy that prevents or reverses atherosclerosis via improved reverse cholesterol transport.
Keywords: Reverse cholesterol transport, HDL, Neo HDL, LCAT, Cholesterol efflux, Cholesteryl esters
Introduction
Cardiovascular disease (CVD) is the major cause of human mortality so that identification of new therapies that address its underlying causes is an important public health priority. Dysregulated lipid metabolism leading to elevated low density lipoprotein (LDL)-cholesterol (C) and low plasma high density lipoprotein (HDL)-C are important CVD risk factors [1–6]. With wider use of the statins, low HDL-C has emerged as the most important lipoprotein disorder for which current therapies are inadequate. The need for new approaches is highlighted by the failed trial of a cholesteryl ester transfer protein (CETP) inhibitor [7]. Although hypertriglyceridemia and low HDL-C are mechanistically linked, the latter is more strongly correlated with CVD mortality [2]. HDL-C and cardioprotection are mechanistically linked by reverse cholesterol transport (RCT), the transfer of cholesterol from macrophages in the subendothelial space to the liver for disposal [8]. The first two RCT steps are macrophage cholesterol efflux and cholesterol esterification in plasma [8]. Thus, an intervention that enhances both of these steps could be a therapeutically useful new approach to improve RCT.
A recombinant (r) virulence determinant from Streptococcus pyogenes [9], serum opacity factor (SOF), delipidates human HDL yielding a cholesteryl ester-rich microemulsion (CERM), lipid-free apo A-I and a “neo HDL” [10–12]. Given that neo HDL is more phospholipid-rich than HDL and that cholesterol efflux and esterification are increased by increased phospholipid content of acceptors and substrates, respectively [13–16], we tested the effects of SOF-mediated conversion of HDL in whole plasma to neo HDL on efflux and esterification.
Experimental Procedures
Materials
Total lipoproteins (TLP) and HDL were isolated from human plasma obtained from The Methodist Hospital Blood Donor Center by addition of KBr to d = 1.21 g/mL and flotation (48 h at 40,000 rpm, Beckman Ti 50.2 rotor). VLDL, LDL, HDL and lipoprotein-deficient serum (LPDS) were isolated by sequential flotation at d = 1.012, 1.063 and 1.21 g/mL, respectively. Lipoprotein purity was verified by size exclusion chromatography (SEC) and SDS-PAGE. Protein was determined with a kit (BioRad DC assay) using BSA as a standard. LDL was stored at 4 °C under nitrogen gas and used within 14 days. OxLDL was prepared by exposing LDL to 5 μmol/L CuSO4 for 24 h at 37 °C [17]. Lipid oxidation was verified by an assay for thiobarbituric acid-reactive substances; precautions were taken to exclude endotoxin. Neo HDL was prepared by incubating HDL (~2 mg/mL) and rSOF (1 μg/mL) in 47.5 mL overnight at 37 °C. The reaction mixture was adjusted to a d = 1.063 g/mL with KBr and centrifuged for 18 h at 45,000 rpm (Beckman Ti 50.2 rotor). The upper half of the tube was removed by aspiration. The bottom half was adjusted to a d = 1.24 g/mL with KBr and centrifuged as above for 40 h. The neo HDL removed from the top was pure as assessed by SEC [12]. Tris-buffered saline (TBS = 10 mM Tris, 100 mM NaCl, 1 mM EDTA, pH 7.4) was used throughout unless otherwise specified. [3H]Cholesterol was from Amersham Biosciences (Piscataway, NJ, USA). Buffer salts were from Fisher Scientific, Inc., (Rockville, MD, USA). A recombinant polyhistidine-tagged, truncated form of sof2, encoding amino acids 38–843 (rSOF) was cloned and expressed in Escherichia coli and purified by metal affinity chromatography [10].
Effect of rSOF on LCAT Cholesterol Esterification
HDL was labeled with [3H]cholesterol (~100 μCi) by injection of an ethanolic solution [15] and split into two equal aliquots; rSOF (1 μg/mL) was added to one and an equal volume of saline was added to the other and incubated overnight at 37 °C. On ice, the fractions were recombined as follows: (a) [3H]HDL + (LDL + VLDL) + LPDS, (b) rSOF-treated [3H]HDL + (LDL + VLDL) + LPDS, (c) [3H]HDL + LPDS, and (d) rSOF-treated [3H]HDL + LPDS. TBS was added to each sample to give equal volumes. The samples were incubated at 37 °C for 30 min and transferred to ice. Triplicate aliquots (100 μL) of each incubation were β-counted. Another set of triplicate aliquots were extracted with 4 mL hexane and the phases separated by low speed centrifugation for 5 min; 3-mL aliquots of the upper layer were evaporated under nitrogen and the residue dissolved in 30 μL chloroform. CE and FC were resolved by thin layer chromatography (Whatman TLC silica gel 60A plates) in hexane/diethyl ether/acetic acid (75:35:1, by volume). After spraying the plates with Primuline dye (Sigma–Aldrich, St. Louis, MO, USA), FC and CE bands were identified by comparison with standards. The FC and CE were collected and quantified by β-counting. A 200-μL aliquot of each incubation mixture was analyzed by SEC to determine the distribution of radiolabel into CERM, VLDL, LDL, HDL and neo HDL. SEC profiles of the LCAT reaction products were determined essentially as described [11] using an Amersham PharmaciaÄKTA chromatography system equipped with two Superose HR6 columns in tandem. Samples were injected into the chromatograph using a 0.2-mL sample loop, and eluted with TBS; 1-mL fractions were collected and analyzed by β-counting.
Effects of rSOF Activity Against Lipoproteins on Cellular Cholesterol Efflux
Plasma, TLP, HDL, and the products of their reactions with rSOF were extensively dialyzed at 4 °C against TBS and tested as acceptors of cholesterol from the human monocyte-derived macrophage cell line, THP-1 (American Type Culture Collection). THP-1 cells were maintained in RPMI 1640 with 10% FBS, 100 U/mL penicillin, 100 mg/mL streptomycin, 1 mM sodium pyruvate and 2 mM glutamine. Cholesterol efflux was assayed as described previously [15, 16, 18]. In brief, THP-1 cells were seeded and activated with 0.1 μg/mL phorbol 12-myristate 13-acetate for 24 h. Cells were then labeled in serum-containing medium with [1α, 2α(n)-3H]cholesterol (specific radioactivity 1.81 TBq/mmol, final radioactivity 74 KBq/mL) at 37 °C for 48 h in a CO2 incubator at which time they were ~80% confluent. After labeling, cells were washed twice to remove excess label, and incubated for an additional 18 h in serum-free medium to ensure equilibration of labeled cholesterol into all intracellular pools. During this phase, the THP-1 medium contained the LXR agonist T0901317 (1 μM) to activate the macrophage in a way that increased the activities of ABCA1 and ABCG1 in cells that were not cholesterol-loaded. To initiate the efflux assay, cells were washed and incubated for 0–2 h at 37 °C in serum-free medium containing various concentrations of human plasma (0–8%), TLP, HDL, or neo HDL (10–200 μg/mL). After incubation, the medium was collected, centrifuged, and the supernatant analyzed by β-counting. Cell lipids were extracted with isopropanol and analyzed by β-counting. Cholesterol efflux (%E) was expressed as the percentage of total labeled cholesterol transferred from cells to the medium. Efflux was compared on the basis of acceptor-protein concentration and the data were fitted to the equation %E = Emax × (LP)/[Km + (LP)], where LP was the lipoprotein concentration as protein, Emax was the maximum efflux and Km was the lipoprotein concentration at half Emax using Systat-Sigma Plot (Point Richmond, CA, USA).
Efflux via ABCA1 and ABCG1
Efflux from ABCA1 and ABCG1-expressing BHK cells under a mifepristone-inducible promoter and MOCK cells transfected with the pGene V5 His plasmid alone were tested as reported by Vaughan and Oram [19]. ABCA1- and ABCG1-expressing BHK cells were labeled with [3H]cholesterol to equilibrium 1 day prior to mifepristone treatment. ABCA1 and ABCG1 receptors were induced by incubating cells for 18–20 h in DMEM with 1 mg/mL fatty acid free bovine serum albumin and 10 nM mifepristone. Unactivated cells (no mifepristone) were used as a negative controls. Transporter-specific efflux was calculated as the difference between efflux from ABCA1 and ABCG1-expressing cells with and without activation.
Comparison of the Effects of HDL and Neo HDL on Inflammatory IL-6 and TNF-α
Mouse peritoneal macrophages were collected from C57Bl/6 J mice 2 days after mineral oil injection and seeded in RPMI-1640 medium supplemented with 5% BSA in 96-well plates at ~105cells/well and cultured for 1 day. HDL and neo HDL were preincubated with OxLDL at ratio of 1:1 protein for 1 h at 37 °C. Cells were treated with OxLDL(100 μg/mL), HDL(100 μg/mL) and neo HDL(100 μg/mL), HDL-OxLDL (100 μg/mL each), and neo HDL-OxLDL(100 μg/mL each), respectively. IL-6 and TNF-α concentrations in the media were measured by ELISA kits (BD Bioscience) 18 h after treatment.
Statistical Tests
Statistical analysis of data was done as indicated in the figure legends, using the t test for pairs of means, one-way ANOVA with Tukey's post hoc test for multiple comparisons, and two-way ANOVA with Bonferroni post tests for regression plots, using SPSS and GraphPad Prism statistical software.
Results
Macrophage Cholesterol Efflux
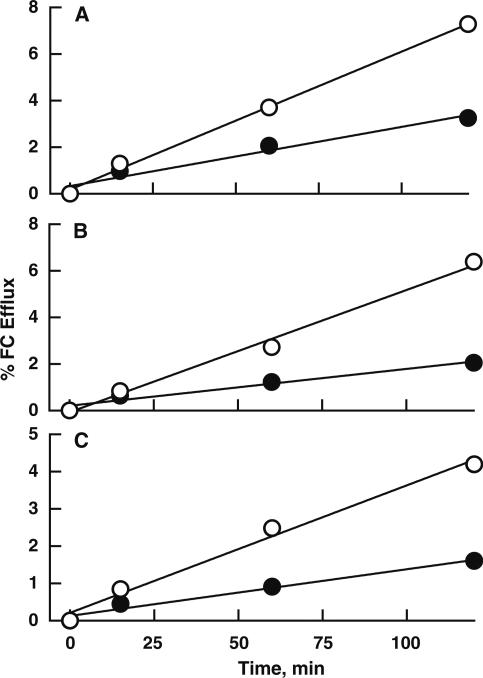
Cholesterol efflux from THP-1 macrophages to plasma (1%) and TLP (25 μg/mL) were linear with time and increased by preincubation with rSOF; efflux to neo HDL formed from treatment of HDL with rSOF was also higher than that to HDL (Fig. 1a–c). The respective ratios of the rates of efflux to the rSOF-derived acceptors to controls were 2.4, 3.3, and 2.6. Increasing the rSOF pre incubation time increased cholesterol efflux and the production of neo HDL and CERM (Supplementary Figs. 1, 2).
Fig. 1.
Time-dependence of cholesterol efflux from THP-1 macrophages. a Plasma (1%) and plasma (1%) after overnight incubation with rSOF (1 μg/mL) were incubated with [3H]cholesterol-labeled macrophages for 0–2 h and the amount of radiolabel transferred to media determined. b Similar data were collected for TLP (25 μg/mL) and TLP (25 μg/mL) after incubation overnight with rSOF. c Similar data for transfer of radiolabel to isolated HDL and neo HDL (both 25 μg/mL). The ratios of the slopes of rSOF derived acceptors to controls in a–c were 2.4, 3.3, and 2.6, respectively. r2 > 0.95 for all plots. Closed circles a control plasma, b control TLP, c HDL. Open circles a Plasma + rSOF, b TLP + rSOF, c neo HDL. The efflux values were means ± SD of two experiments in triplicate. In a–c the error bars were smaller than the symbols
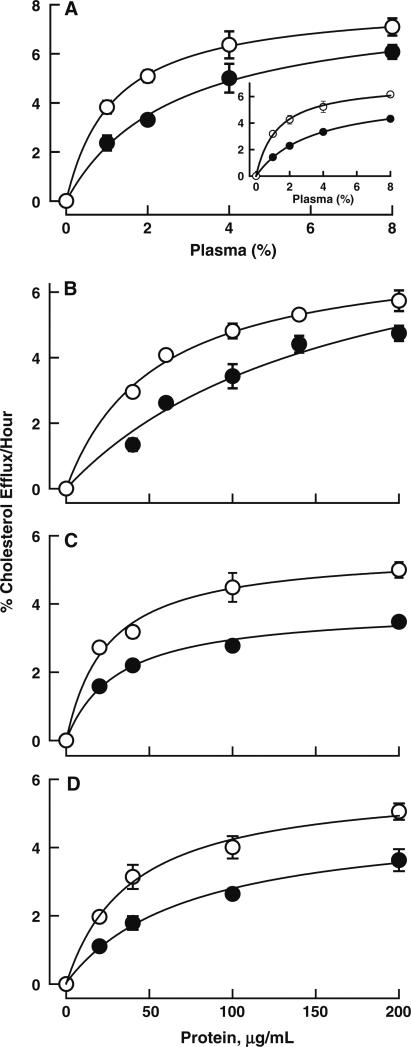
[3H]Cholesterol efflux kinetics from THP-1 macrophages to various acceptors with and without rSOF treatment were also measured. The acceptors were, respectively, plasma ± rSOF, TLP ± rSOF, HDL ± rSOF reaction mixtures and isolated HDL and neo HDL (Fig. 2a–d). Efflux from cholesterol-loaded macrophages to plasma was also measured (Fig. 2a, insert). rSOF treatment improved the global parameter of cholesterol efflux, Cateff = Vmax/Km(Supplementary Table 1). The Cateff for acceptors that were rSOF-derived were 2–3 times higher than those of the acceptors from which they were formed (Supplementary Table 1). When measured as mass, macrophage cholesterol efflux to HDL after incubation with rSOF increased with the addition of the LXR agonist (TO-901317) both with and without cholesterol loading (Supplementary Fig. 3).
Fig. 2.
[3H]Cholesterol efflux from THP-1 macrophages to various acceptors. The acceptors were plasma (a), TLP (b), and HDL (c) each with (open circles) and without (closed circles) preincubation with rSOF for 18 h. Efflux to isolated HDL (closed circles) and neo HDL formed from rSOF + HDL (open circles) is shown in (d). Insert in a shows efflux from cholesterol-loaded macrophages to plasma. Other details are in “Materials” and Fig. 1. Two-way ANOVA analysis of the regression plots indicated that rSOF pretreatment significantly increased efflux to all of the acceptors (p < 0.001), and Bonferroni post tests indicated this was true for all the concentrations tested (p < 0.01)
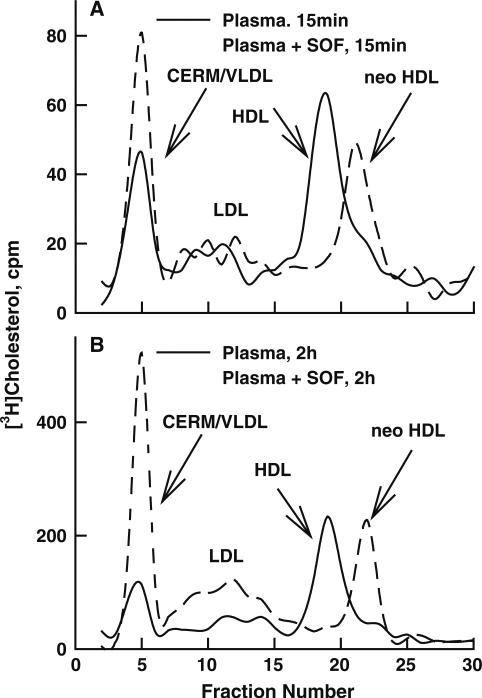
We identified the plasma acceptors of cellular [3H]cholesterol after 15 min and 2 h efflux times by SEC. After a 15-min incubation of 3% plasma with cells, most of the cell-derived [3H]cholesterol co-eluted with HDL and VLDL (Fig. 3a). In contrast, [3H]cholesterol effluxed to 3% plasma pre-treated for 3 h with rSOF co-eluted with neo HDL and CERM + VLDL (Fig. 3a). After longer incubation (2 h) with macrophages the SEC profiles indicated more transfer to CERM and LDL for rSOF-treated plasma than to VLDL and LDL for control (Fig. 3b). Similar experiments were conducted with TLP, which lacks lipid transfer protein and LCAT activities. At 15 min, [3H]cholesterol appeared in all lipoprotein subclasses but at 2 h, a greater fraction was in LDL. (Supplementary Fig. 4). Similarly, SEC showed that cell-derived cholesterol associates with HDL and neo HDL when they were used as acceptors (Supplementary Fig. 5a, c), and efflux to all acceptors was greater at 2 h than at 15 min. When the total rSOF-HDL reaction mixture was used as acceptor, [3H]cholesterol was found in both the neo HDL and the CERM (Supplementary Fig. 5b), and the presence of CERM promoted more total efflux than neo HDL alone at both 15 min and 2 h. Finally, macrophage cholesterol efflux to plasma depleted of apo B-containing lipoproteins increased when the preincubation time with rSOF was increased from 15 to 120 min. With the longer preincubation time, more neo HDL and CERM were formed, and there was a corresponding increase in association of [3H]cholesterol with CERM and neo HDL instead of HDL (Supplementary Fig. 6).
Fig. 3.
SEC of 3% plasma, with and without rSOF pretreatment (3 h), after incubation with [3H]cholesterol-labeled THP-1 macrophages. Cells were labeled and treated as in Fig. 1. a Fifteen min incubation, b 2 h incubation. Plasma (continuous lines), plasma post-rSOF (dashed lines). Media were transferred to tubes in wet ice and immediately analyzed by SEC in which the effluent was monitored by absorbance at 280 nm (not shown) and by the radioactivity of collected fractions. The peak elution fractions for CERM/VLDL, LDL, HDL, and neo were 4, 12, 19, and 22 mL, respectively
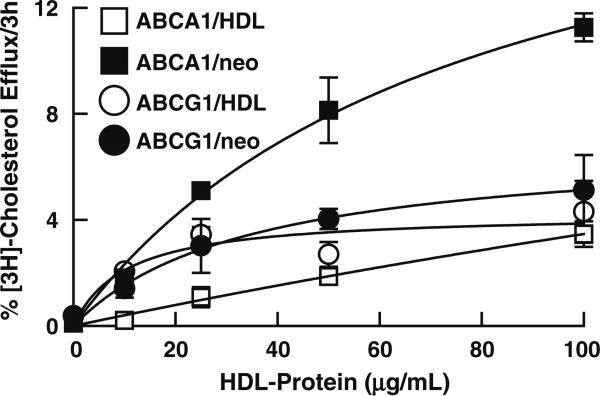
Efflux via ABCA1 and ABCG1
FC efflux from ABCG1-expressing BHK cells to neo HDL and HDL were not significantly different (Fig. 4). In contrast, FC efflux from ABCA1-expressing BHK cells to neo HDL was higher than that to HDL (Fig. 4).
Fig. 4.
[3H]Cholesterol efflux from ABCA1- and ABCG1-transfected BHK cells to various protein concentrations of HDL and neo HDL. HDL and neo HDL were incubated with radiolabeled, mifepristone-induced cells for 3 h and the amount of the radiolabel transferred to media determined. The control assays were done with non-induced cells. The efflux values are means ± SD of two experiments in triplicate. Two-way ANOVA analysis of the regression plots indicated that efflux to neo HDL was significantly greater than to HDL for the ABCA1 cells (p = 0.002) but that efflux to neo HDL and HDL was not significantly different for the ABCG1 cells
Remodeling of HDL and Neo HDL
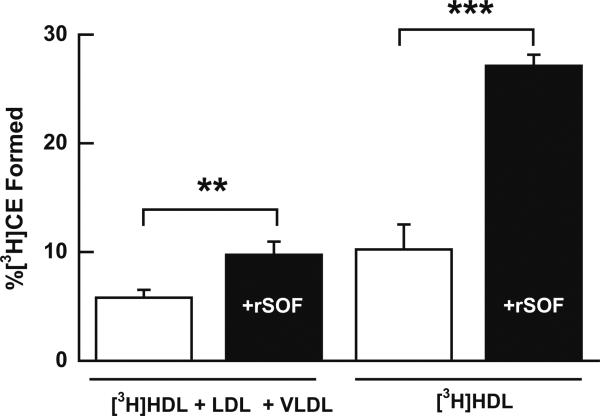
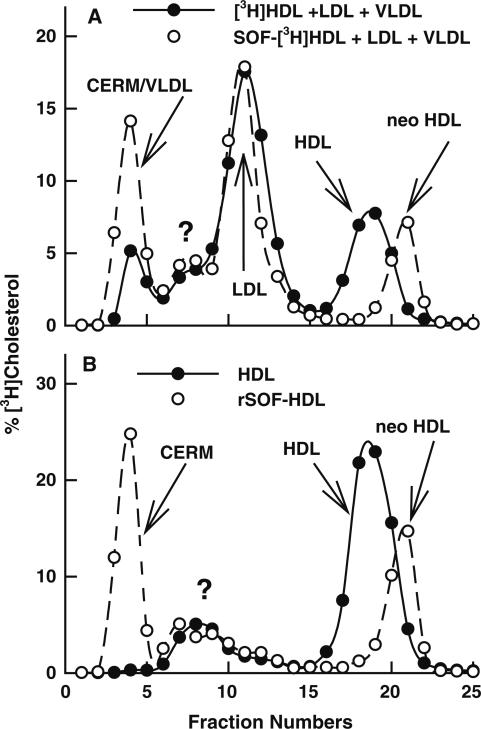
HDL-[3H]cholesterol and neo HDL-[3H]cholesterol were incubated with HDL-deficient plasma in amounts that restored the original plasma protein compositions. The LCAT reactivity of neo HDL was higher (+68%) than that of HDL (Fig. 5, left bars). Comparison of the LCAT reactivity of neo HDL and HDL (Fig. 5, right bars), showed CE production from neo HDL was higher than that from HDL (+165%). These samples were also analyzed by SEC, which showed that association of radiolabel with lipoproteins decreased as LDL > HDL > VLDL (Fig. 6a). When the HDL was replaced by rSOF-treated HDL the distribution decreased as LDL > CERM > neo HDL. The experiment with HDL and neo HDL without the apo B-containing lipoproteins showed that most remodeled neo HDL-[3H]cholesterol was associated with CERM while most HDL-[3H]cholesterol remained in the HDL peak (Fig. 6b). The enhancement of cholesterol esterification increased with rSOF dose (Supplementary Fig. 7).
Fig. 5.
Effect of rSOF reaction on cholesterol esterification via LCAT. Isolated HDL was labeled with [3H]FC as described in “Materials” and recombined with (LDL + VLDL) and LPDS using amounts that returned all components to their original plasma concentrations. The incubations were for 30 min at 37 °C. The esterification rates are means ± SD of two experiments in triplicate. Statistical analysis by t test of HDL versus neo HDL under the same conditions, **p < 0.01, ***p < 0.001
Fig. 6.
Distribution of [3H]cholesterol among lipoprotein subclasses after incubation with LPDS for 30 min. Labeling is as in “Materials”. a Reconstituted whole plasma. SOF treatment of plasma TLP increased non HDL-associated cholesterol from 69 to 86%. b HDL or rSOF-HDL plus LPDS. Subtracting the radiolabel in HDL or neo HDL showed that SOF treatment increased the non HDL-associated cholesterol from 22 to 65%. A similar pattern was observed when the incubation with LPDS was reduced to 15 min. Some [3H]cholesterol associated with a peak labeled “?” that was not identified but was likely a component of LPDS because it appears both a and b
The major fractions from Fig. 6 were used to determine the fraction of cholesterol as ester. HDL-[3H]cholesterol and rSOF-treated HDL-[3H]cholesterol, which contains CERM, neo HDL and lipid-free apo A-I [11], were incubated with HDL-deficient plasma and the distribution of [3H]cholesterol into CE determined (Supplementary Fig. 8a). With rSOF treatment the formation of [3H]CE increases and shifts to the non HDL fractions. The fractions of [3H]CE in the neo HDL and the CERM/VLDL fraction were highest. A similar experiment in which LPDS was incubated with HDL-[3H]cholesterol at their original plasma concentrations showed that at 30 min ~40% of the total cholesterol in HDL was CE (Supplementary Fig. 8b). When HDL-[3H]cholesterol was replaced by rSOF-treated HDL-[3H]cholesterol only 20% of the total cholesterol in neo HDL was esterified. However, more than 60% of the total cholesterol in the coexisting CERM fraction was esterified. Thus, most of the [3H]cholesterol in the CERM peak in Fig. 6a was CE.
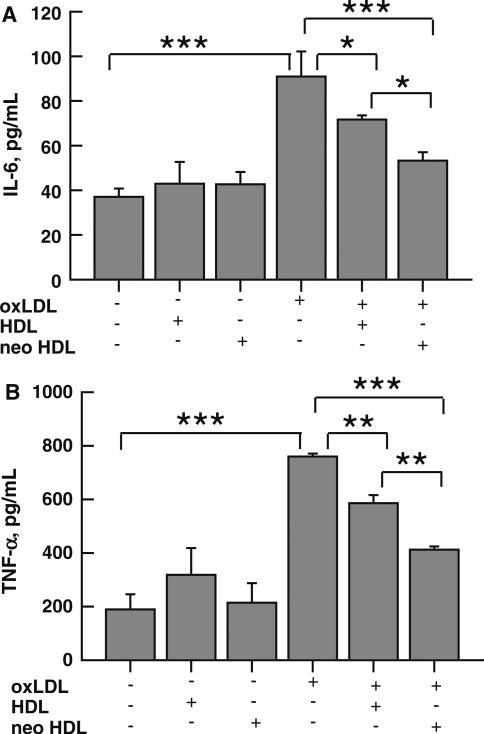
Comparative Attenuation of OxLDL-Induced Cytokine Secretion by Mouse Peritoneal Macrophages by HDL and Neo HDL
The effects of HDL and neo HDL on the secretion of the cytokines, IL-6 and TNF-α, by mouse peritoneal macrophages exposed to OxLDL were compared. Both lipoproteins elicited a dose-dependent reduction in IL-6 and TNF-α secretion that was greater for neo HDL (Supplementary Fig. 9). The effects at a single concentration were compared in detail (Fig. 7). These data showed that neither HDL nor neo HDL alone affected cytokine secretion elicited by LDL. In contrast, TNF-α and IL-6 secretion elicited by incubation of macrophages with OxLDL was reduced by coincubation with either HDL or neo HDL, with the effect of the latter being 96 and 103% greater (p < 0.05 for both).
Fig. 7.
Comparative attenuation of OxLDL-induced secretion of cytokines by HDL and neo HDL. HDL and neo HDL attenuated OxLDL-induced IL-6 and TNF-α production in a dose-dependent manner (Supplemental Fig. 9). For the data shown here, OxLDL (100 μg/mL) was preincubated with 100 μg/mL of HDL or neo HDL for 1 h at 37 °C. Cells were then incubated with OxLDL, HDL, neo HDL, HDL + OxLDL and neo HDL + OxLDL for 16 h. IL-6 and TNF-α secretion were measured by ELISA. One-way ANOVA analysis with Tukey's post-test indicated the means were significant as indicated ***p < 0.001, **p < 0.01, *p < 0.05
Discussion
To simulate a physiological setting, we compared efflux to plasma with and without preincubation with rSOF and found that the parameters for efflux were improved by rSOF treatment and that efflux increased with longer incubation times. Kinetic parameters for efflux to TLP, which lacks the lipid transfer proteins and LCAT of plasma, were similarly improved. In both plasma and TLP, the initial acceptor with and without rSOF-treatment, respectively, appears to be neo HDL and HDL because the fraction of [3H]cholesterol in these particles was higher at 15 min than at 2 h (Fig. 3 and Supplemental Fig. 4). At both 15 min and 2 h, the distribution of [3H]cholesterol was different for plasma and TLP. With plasma as the acceptor, more of the radiolabel was in the VLDL/CERM fraction, while with the TLP acceptor, more radiolabel was in LDL, an effect that was more profound at 2 h than at 15 min. This difference was likely due to the presence of CETP and LCAT activities in plasma but not in TLP. In the absence of LCAT activity, [3H]cholesterol remained unesterified and was spontaneously transferred from HDL or neo HDL to other lipoproteins. In contrast, in plasma [3H]cholesterol was converted to its ester, which requires CETP for transfer to other lipoproteins, a process that was much slower than that of spontaneous [3H]cholesterol transfer from HDL [20–23].
[3H]Cholesterol efflux to rSOF-treated HDL and isolated neo HDL was greater than that to HDL. This finding further supports the hypothesis that the increased efflux to plasma and TLP post-rSOF treatment is due to a more rapid initial transfer to neo HDL than to HDL (Supplementary Fig. 5a, c). Notably, a large fraction of the [3H]cholesterol efflux to rSOF-treated HDL appeared in the CERM fraction (Supplementary Fig. 5b). As with TLP, the fraction of [3H]cholesterol in the CERM was greater at 2 h than at 15 min. This further supported our hypothesis that [3H]cholesterol transfer to non-neo HDL fractions in TLP was spontaneous free cholesterol transfer and that cholesterol desorbs more rapidly from neo HDL than from HDL. This was consistent with data showing that spontaneous lipid transfer rates increase with decreasing particle size according to the Kelvin equation [21].
Differences in the size, charge, apo composition and PL content of neo HDL and HDL might be mechanistically linked to differences in cholesterol efflux. Size probably does not play an important role in the rate differences. When normalized to PL content, there was no difference in efflux to rHDL of varying size and when normalized to particle number at constant PL concentration, cellular FC efflux to larger particles was more efficient [22], the opposite of our observations. Although HDL can have either α or pre β mobility and the latter was a preferred plasma acceptor of cholesterol, there was little evidence that charge was an important efflux discriminator. In contrast, the higher PL and apo A-II content of neo HDL compared to HDL [10, 11] could underlie the differences. Other studies support this; normalized to PL content ABCG1-mediated FC to rHDL efflux is more highly correlated with apo A-II (r2 = 0.7) than with apoA-I (r2 = 0.5); the underlying mechanism for this has not been identified. On the other hand, both spontaneous and ABCG1-mediated efflux increases with HDL-PL [24, 25]. This is supported by numerous studies with both rHDL and modified plasma HDL [13–16]. Indeed, the similar increases in efflux to neo HDL and to rSOF-treated plasma versus HDL and untreated plasma, respectively, are compelling evidence that neo HDL and not lipid-free apo A-I, which is also formed by rSOF [10], is the mechanistic link to increased efflux in plasma.
The studies of efflux from cells expressing ABCA1 and ABCG1 provide clues to the source of the increased efflux to neo HDL (Fig. 4). The higher efflux to neo HDL versus HDL again showed that neo HDL was a superior acceptor. More importantly, the higher efflux from the ABCA1-expressing cells suggests that this transporter mediates the efflux to neo HDL. A role for lipid-free apo A-I cannot be excluded in the efflux from plasma and TLP. However, the similar increases in Cateff for efflux to plasma, TLP and isolated neo HDL, which contains no lipid-free apo A-I, suggests that neo HDL and not lipid-free apo A-I was the major acceptor. Although it has been suggested that ABCG1 is an important mediator of efflux to lipidated species [26], other studies have not supported this and have shown that pre β1-HDL is an efficient FC acceptor via ABCA1 [27]. Given the similarity between neo HDL and pre β1-HDL particles with respect to size, smaller than HDL, efficient efflux via ABCA1 was not unexpected. This finding was interesting in the context of the report that cholesterol efflux to plasma correlates better with the concentration of pre β1-HDL than with that of HDL [28].
LCAT Reactivity of HDL and Neo HDL
CE formation via LCAT was higher (+68%) in plasma treated with rSOF than in untreated control plasma. LCAT catalyzed CE formation in neo HDL, the product of rSOF, was even higher (+165%) than that of HDL. The smaller increase in whole plasma may be due to some binding of LCAT to other lipoproteins such as LDL which is a poorer substrate [29]. Similarly, the higher rate of CE formation from neo HDL than from HDL suggests that higher neo HDL-reactivity underlies the differences observed in plasma. The higher rate of esterification in both rSOF-treated plasma versus control plasma and isolated HDL versus neo HDL, may be due to the higher PL content of neo HDL versus HDL [10, 11] and the transfer of CE to CERM which could produce some modest relief of product inhibition. The more likely explanation is that neo HDL has a lower FC/PL ratio than HDL and that high cholesterol concentrations are inhibitory; the optimal FC/PL ratio for LCAT activity is 12.5 mol%, above which activity declines [30]. This optimum is considerably lower than the FC/PL ratio of native HDL, ~25 mol% [31].
According to SEC of the respective products of the LCAT reaction against HDL and rSOF-treated HDL in whole plasma, most of the radiolabel occurs with LDL + VLDL and LDL + VLDL/CERM. However, the radiolabel in the VLDL/CERM fractions was higher than that of the VLDL (Fig. 6a). A similar experiment in which the reaction mixture does not contain VLDL or LDL also showed increased radiolabel in the CERM (Fig. 6b) suggesting that the increased radiolabel seen in the void volume of Fig. 6a was bound to CERM as CE and not to VLDL (Fig. 6). Whether the appearance of additional cholesterol in apo B lipoproteins is beneficial cannot be stated with certainty. One view is that any increase in cholesterol in VLDL and LDL is atherogenic. However, others opine that transfer to the apo B lipoproteins helps clear more cholesterol via the non-HDL receptors. New work in our laboratory shows that the CE transferred from HDL to CERM by rSOF is rapidly taken up by hepatocytes in vitro [32] and in vivo in mice, cleared from plasma into the liver (Rosales et al., unpublished work).
Enhanced Reduction of Cytokine Secretion by Neo HDL Versus HDL
Hypercholesterolemia is associated with increased numbers of arterial macrophage foam cells, a hallmark of an inflammatory state. HDL has anti inflammatory properties that oppose the inflammatory properties of OxLDL, an effect that may be due to enhanced cholesterol efflux to HDL [33, 34]. Our data, which compare the effects of HDL and neo HDL on the OxLDL-induced secretion of TNF-α and IL-6, show neo HDL producing nearly twice the suppression of these two markers of inflammation. Thus, the rSOF reaction has the potential to reduce inflammation via the formation of neo HDL.
rSOF: A Path to Improved RCT
Thus, rSOF activity against plasma might improve key steps in RCT, which comprises macrophage cholesterol efflux that forms nascent HDL and esterification of nascent HDL-cholesterol by LCAT. First, rSOF treatment increased cholesterol efflux under all conditions, plasma, TLP, and isolated HDL. Cholesterol accumulation in macrophage foam cells induces an inflammatory response, apoptosis, and other adverse effects associated with atherogenesis [35]. Cholesterol efflux from macrophages to HDL and apoA-I is one mechanism of atheroprotection [36, 37].
Second, neo HDL was a better LCAT substrate than HDL even in whole plasma. Although recent studies have shown that LCAT may be less important in RCT than once thought [38], in the context of rSOF the LCAT reaction may be important to the final RCT step, hepatic CE uptake, because a major fraction of HDL-cholesterol was transferred to the CERM mostly as its ester. Future studies in vivo will determine the feasibility of an SOF-based therapy, and provide a rationale for finding small molecules or peptides that catalyze the SOF reaction.
Supplementary Material
Acknowledgments
Dr. Urbain Tchoua dedicates this publication to his father, Jean-Pierre Tchoua, who passed away during its preparation. We thank Dr. Joshua S. Wooten for help with statistical analyses. Supported by grants-in-aid from the National Institutes of Health (HJP, HL-30914 and HL-56865), the Merck-UNCF Science Inititative (UT) and the Department of Veterans Affairs (HSC).
Abbreviations
- Apo
Apolipoprotein
- rSOF
Recombinant serum opacity factor
- RCT
Reverse cholesterol transport
- HDL
High density lipoprotein
- rHDL
Reconstituted HDL
- LDL
Low density lipoprotein
- oxLDL
Oxidized LDL
- VLDL
Very low density lipoprotein
- TLP
Total lipoprotein
- LPDS
Lipoprotein depleted serum
- LCAT
Lecithin:cholesterol acyltransferase
- ABC
ATP-binding cassette transporter.
- SEC
Size exclusion chromatography
- CVD
Cardiovascular disease
- FC
Free cholesterol
- CE
Cholesteryl ester
- CERM
CE-rich microemulsion
- TLC
Thin layer chromatography
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s11745-010-3484-2) contains supplementary material, which is available to authorized users.
Contributor Information
Urbain Tchoua, Department of Medicine, Baylor College of Medicine, MSA601, One Baylor Plaza, Houston, TX 77030, USA.
Corina Rosales, Department of Medicine, Baylor College of Medicine, MSA601, One Baylor Plaza, Houston, TX 77030, USA.
Daming Tang, Department of Medicine, Baylor College of Medicine, MSA601, One Baylor Plaza, Houston, TX 77030, USA.
Baiba K. Gillard, Department of Medicine, Baylor College of Medicine, MSA601, One Baylor Plaza, Houston, TX 77030, USA
Ashley Vaughan, Seattle Biomedical Research Institute, Seattle, WA 98195, USA.
Hu Yu Lin, Department of Medicine, Baylor College of Medicine, MSA601, One Baylor Plaza, Houston, TX 77030, USA.
Harry S. Courtney, Veterans Affairs Medical Center and Department of Medicine, University of Tennessee HSC, Memphis, TN 38104, USA
Henry J. Pownall, Department of Medicine, Baylor College of Medicine, MSA601, One Baylor Plaza, Houston, TX 77030, USA hpownall@bcm.tmc.edu
References
- 1.Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, Huttunen JK, Kaitaniemi P, Koskinen P, Manninen V. Helsinki heart study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 2003;317:1237–1245. doi: 10.1056/NEJM198711123172001. [DOI] [PubMed] [Google Scholar]
- 2.Manninen V, Elo MO, Frick M, Haapa K, Heinonen OP, Heinsalm P, Helo P, Huttunen JK, Kaitaniem P, Koskinen P. Lipid alterations and decline in the incidence of coronary heart disease in the Helsinki heart study. JAMA. 1988;260:641–651. [PubMed] [Google Scholar]
- 3.Rhoads GG, Gulbrandsen CL, Kagan A. Serum lipoproteins and coronary heart disease in a population study of Hawaii Japanese men. N Engl J Med. 1976;294:293–298. doi: 10.1056/NEJM197602052940601. [DOI] [PubMed] [Google Scholar]
- 4.Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease: the Framingham study. Am J Med. 1977;66:707–714. doi: 10.1016/0002-9343(77)90874-9. [DOI] [PubMed] [Google Scholar]
- 5.Miller NE, Thelle DS, Førde OH, Mjøs OD. The Tromsø heart study: high-density lipoprotein and coronary heart-disease: a prospective case–control study. Lancet. 1977;1:964–968. doi: 10.1016/s0140-6736(77)92274-7. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs DR, Jr, Mebane IL, Bangdiwala SI, Criqu MH, Tyroler HA. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the lipid research clinics prevalence study. Am J Epidemiol. 1990;131:32–47. doi: 10.1093/oxfordjournals.aje.a115483. [DOI] [PubMed] [Google Scholar]
- 7.Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, Lopez-Sendon J, Mosca L, Tardif JC, Waters DD, Shear CL, Revkin JH, Buhr KA, Fisher MR, Tall AR, Brewer HB. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357L:2109–2122. doi: 10.1056/NEJMoa0706628. [DOI] [PubMed] [Google Scholar]
- 8.Cuchel M, Rader DJ. Macrophage reverse cholesterol transport: key to the regression of atherosclerosis? Circulation. 2006;113:2548–2555. doi: 10.1161/CIRCULATIONAHA.104.475715. [DOI] [PubMed] [Google Scholar]
- 9.Courtney HS, Zhang YM, Frank MW, Rock CO. Serum opacity factor, a streptococcal virulence factor that binds to apolipoproteins A-I and A-II and disrupts high density lipoprotein structure. J Biol Chem. 2006;281:5515–5521. doi: 10.1074/jbc.M512538200. [DOI] [PubMed] [Google Scholar]
- 10.Gillard BK, Courtney HS, Massey JB, Pownall HJ. Serum opacity factor unmasks human plasma high density lipoprotein instability via selective delipidation and apolipoprotein A-I desorption. Biochemistry. 2007;46:12968–12978. doi: 10.1021/bi701525w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pownall HJ, Courtney HS, Gillard BK, Massey JB. Properties of the products formed by the activity of serum opacity factor against human plasma high density lipoproteins. Chem Phys Lipids. 2008;156:45–51. doi: 10.1016/j.chemphyslip.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han M, Gillard BK, Courtney HS, Ward K, Rosales C, Khant H, Ludtke SJ, Pownall HJ. Disruption of human plasma high density lipoproteins by streptococcal serum opacity factor requires labile apolipoprotein A-I. Biochemistry. 2009;48:1481–1487. doi: 10.1021/bi802287q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Picardo M, Massey JB, Kuhn DE, Gotto AM, Jr, Gianturco SH, Pownall HJ. Partially reassembled high density lipoproteins effects on cholesterol flux, synthesis, and esterification in normal human skin fibroblasts. Arteriosclerosis. 1986;6:434–441. doi: 10.1161/01.atv.6.4.434. [DOI] [PubMed] [Google Scholar]
- 14.Yancey PG, De la Llera-Moya M, Swarnakar S, Monzo P, Klein SM, Connelly MA, Johnson WJ, Williams DL, Rothblat GH. High density lipoprotein phospholipid composition is a major determinant of the bi-directional flux and net movement of cellular free cholesterol mediated by scavenger receptor BI. J Biol Chem. 2000;275:36596–36604. doi: 10.1074/jbc.M006924200. [DOI] [PubMed] [Google Scholar]
- 15.Tchoua U, Gillard BK, Pownall HJ. HDL superphospholipidation enhances key steps in reverse cholesterol transport. Atherosclerosis. 2010;209:430–435. doi: 10.1016/j.atherosclerosis.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pownall HJ. Detergent-mediated phospholipidation of plasma lipoproteins increases HDL cholesterophilicity and cholesterol efflux via SR-BI. Biochemistry. 2006;45(38):11514–11522. doi: 10.1021/bi0608717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steinbrecher UP. Oxidation of human low density lipoprotein results in derivatization of lysine residues of apolipoprotein B by lipid peroxide decomposition products. J Biol Chem. 1987;262:3603–3608. [PubMed] [Google Scholar]
- 18.Mukhamedova N, Escher G, D'Souza W, Tchoua U, Grant A, Krozowski Z, Bukrinsky M, Sviridov D. Enhancing apolipoprotein A-I-dependent cholesterol efflux elevates cholesterol export from macrophages in vivo. J Lipid Res. 2008;49:2312–2322. doi: 10.1194/jlr.M800095-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vaughan AM, Oram JF. ABCA1 and ABCG1 or ABCG4 act sequentially to remove cellular cholesterol and generate cholesterol-rich HDL. J Lipid Res. 2006;47:2433–2443. doi: 10.1194/jlr.M600218-JLR200. [DOI] [PubMed] [Google Scholar]
- 20.Lund-Katz S, Hammerschlag B, Phillips MC. Kinetics and mechanism of free cholesterol exchange between human serum high- and low-density lipoproteins. Biochemistry. 1982;21:2964–2969. doi: 10.1021/bi00541a025. [DOI] [PubMed] [Google Scholar]
- 21.Massey JB, Hickson D, She HS, Sparrow JT, Via DP, Gotto AM, Jr, Pownall HJ. Measurement and prediction of the rates of spontaneous transfer of phospholipids between plasma lipoproteins. Biochim Biophys Acta. 1984;794:274–280. doi: 10.1016/0005-2760(84)90156-5. [DOI] [PubMed] [Google Scholar]
- 22.Pownall HJ, Bick DL, Massey JB. Spontaneous phospholipid transfer: development of a quantitative model. Biochemistry. 1991;30:5696–5700. doi: 10.1021/bi00237a009. [DOI] [PubMed] [Google Scholar]
- 23.Pownall HJ, Brauchi D, Kilinç C, Osmundsen K, Pao Q, Payton-Ross C, Gotto AM, Ballantyne CM. Correlation of serum triglyceride and its reduction by ω-3 fatty acids with lipid transfer activity and the neutral lipid compositions of high-density and low-density lipoproteins. Atherosclerosis. 1999;143:285–297. doi: 10.1016/s0021-9150(98)00301-3. [DOI] [PubMed] [Google Scholar]
- 24.Davidson WS, Rodriguez WV, Lund-Katz S, Johnson WJ, Rothblat GH, Phillips MC. Effects of acceptor particle size on the efflux of cellular free cholesterol. J Biol Chem. 1995;270:17106–17113. doi: 10.1074/jbc.270.29.17106. [DOI] [PubMed] [Google Scholar]
- 25.Sankaranarayanan S, Oram JF, Asztalos BF, Vaughan AM, Lund-Katz S, Adorni MP, Phillips MC, Rothblat GH. Effects of acceptor composition and mechanism of ABCG1-mediated cellular free cholesterol efflux. J Lipid Res. 2009;50:275–284. doi: 10.1194/jlr.M800362-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang N, Lan D, Chen W, Matsuura F, Tall AR. ATP-binding cassette transporters G1 and G4 mediate cellular cholesterol efflux to high-density lipoproteins. Proc Natl Acad Sci USA. 2004;101:9774–9779. doi: 10.1073/pnas.0403506101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duong PT, Weibel GL, Lund-Katz S, Rothblat GH, Phillips MC. Characterization and properties of pre beta-HDL particles formed by ABCA1-mediated cellular lipid efflux to apo A-I. J Lipid Res. 2008;49:1006–1014. doi: 10.1194/jlr.M700506-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de la Llera-Moya M, Drazul-Schrader D, Asztalos BF, Cuchel M, Rader DJ, Rothblat GH. The ability to promote efflux via ABCA1 determines the capacity of serum specimens with similar high-density lipoprotein cholesterol to remove cholesterol from macrophages. Arterioscler Thromb Vasc Biol. 2010;30:796–801. doi: 10.1161/ATVBAHA.109.199158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen CH, Albers JJ. Distribution of lecithin–cholesterol acyltransferase (LCAT) in human plasma lipoprotein fractions evidence for the association of active LCAT with low density lipoproteins. Biochem Biophys Res Commun. 1982;107:1091–1096. doi: 10.1016/0006-291x(82)90633-7. [DOI] [PubMed] [Google Scholar]
- 30.Aron L, Jones S, Fielding CJ. Human plasma lecithincholesterol acyltransferase: characterization of cofactor-dependent phospholipase activity. J Biol Chem. 1978;253:7220–7226. [PubMed] [Google Scholar]
- 31.Havel RJ, Goldstein JL, Brown MS, Bondy PK, Rosenberg LE. Lipoproteins and lipid transport in the context of metabolic disease. Saunders Publishing; Philadelphia: 1980. pp. 393–494. [Google Scholar]
- 32.Gillard BK, Rosales C, Lin H-Y, Courtney HS, Pownall HJ. Treatment of human HDL with serum opacity factor increases the rate of cholesterol ester uptake by human hepatoma cells. Biochemistry. 2010 doi: 10.1021/bi101412m. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barter PJ, Nicholls S, Rye KA, Anantharamaiah GM, Navab M, Fogelman AM. Antiinflammatory properties of HDL. Circ Res. 2004;95(8):764–772. doi: 10.1161/01.RES.0000146094.59640.13. [DOI] [PubMed] [Google Scholar]
- 34.Robbesyn F, Garcia V, Auge N, Vieira O, Frisach MF, Salvayre R, Negre-Salvarye A. HDL counterbalance the proinflammatory effect of oxidized LDL by inhibiting intracellular reactive oxygen species rise, proteasome activation, and subsequent NF-kappaB activation in smooth muscle cells. FASEB J. 2003;17(6):743–745. doi: 10.1096/fj.02-0240fje. [DOI] [PubMed] [Google Scholar]
- 35.Tall AR. Cholesterol efflux pathways and other potential mechanisms involved in the athero-protective effect of high density lipoproteins. J Intern Med. 2008;263(3):256–273. doi: 10.1111/j.1365-2796.2007.01898.x. [DOI] [PubMed] [Google Scholar]
- 36.Rader DJ. Mechanisms of disease: HDL metabolism as a target for novel therapies. Nat Clin Pract Cardiovasc Med. 2007;4:102–109. doi: 10.1038/ncpcardio0768. [DOI] [PubMed] [Google Scholar]
- 37.Tabas I. Consequences and therapeutic implications of macrophage apoptosis in atherosclerosis: the importance of lesion stage and phagocytic efficiency. Arterioscler Thromb Vasc Biol. 2005;25:2255–2264. doi: 10.1161/01.ATV.0000184783.04864.9f. [DOI] [PubMed] [Google Scholar]
- 38.Tanigawa H, Billheimer JT, Tohyama J, Fuki IV, Ng DS, Rothblat GH, Rader DJ. Lecithin-cholesterol acyltransferase expression has minimal effects on macrophage reverse cholesterol transport in vivo. Circulation. 2009;120:160–169. doi: 10.1161/CIRCULATIONAHA.108.825109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.