Abstract
NiTinol shape memory alloy is characterized by its malleability at low temperatures and its ability to return to a preconfigured shape above its activation temperature. This process can be utilized to assist in scoliosis correction. The goal of this retrospective study was to evaluate the clinical and radiographic results of intraoperative use of shape memory alloy rod in the correction of scoliosis. From May 2002 to September 2006, 38 scoliosis patients (ranging from 50° to 120°; 22 cases over 70°) who underwent shape memory alloy-assisted correction in our institute were reviewed. During the operation, a shape memory alloy rod served as a temporary correction tool. Following correction, the rod was replaced by a rigid rod. The mean blood loss at surgery was 680 ± 584 ml; the mean operative time was 278 ± 62 min. The major Cobb angle improved from an average 78.4° preoperatively to 24.3° postoperatively (total percent correction 71.4%). In 16 patients with a major curve <70° and flexibility of 52.7%, the deformity improved from 58.4° preoperatively to 12.3° postoperatively (percent correction, 78.9%). In 22 patients with a major curve >70° and flexibility of 25.6%, the deformity improved from 94.1° preoperatively to 30.1° postoperatively (percent correction, 68.1%). Only one case had a deep infection. There were no neurologic, vascular or correction-related complications such as screw pullout or metal fracture. The study shows that the intraoperative use of a shape memory rod is a safe and effective method to correct scoliosis.
Electronic supplementary material
The online version of this article (doi:10.1007/s00586-010-1514-7) contains supplementary material, which is available to authorized users.
Keywords: Scoliosis, Shape memory alloy, NiTi, Posterior surgery
Introduction
A shape memory material is generally characterized by having two distinct states. In its austenitic state (above its activation temperature), the shape memory material is stiff and has a preconfigured shape. In its martensitic state (below its activation temperature), the shape memory material is malleable and can be contoured to assume a variety of shapes [20]. Once the material is warmed to its austenitic state, it will automatically resume its original, preconfigured shape.
These distinct characteristics make the shape memory alloy useful in orthodontic tooth alignment, vascular applications [2, 10] and spine surgery [1, 3, 15–17]. We used a shape memory rod as a temporary tool to assist in scoliosis correction. The goal of this study was to investigate the clinical and radiographic results following the use of temporary shape memory rods in scoliosis surgery.
Materials and methods
Patient demographics
From May 2002 to September 2006, 38 scoliosis patients who underwent shape memory alloy rod-assisted scoliosis correction in our institute were reviewed. Initially, the shape memory alloy rods were used on patients with curves less than 70°. Later as we gained greater experience with the technique, the temporary shape memory alloy rod was employed on scoliosis greater than 70°.
The diagnoses included 32 idiopathic, 3 congenital and 3 neuromuscular scoliosis. Of the 32 idiopathic patients, 4 were adults. Indications for surgery included a Cobb angle greater than 50°. The average age at the time of surgery was 17.8 years (9–34 years); 21 were female and 17 were male. Patients with prior spinal surgery were excluded. All patients were examined radiographically and clinically (Fig. 1). Cell saver was used to save blood during operation for congenital and neuromuscular scoliosis and patients with spinal osteotomy. Woke test was performed after correction for all patients, and additional somatosensory-evoked potentials was performed for patients with spinal osteotomy.
Fig. 1.
a–d In a 22-year-old woman with a severe idiopathic thoracic scoliosis and a 92° Cobb angle, the flexibility of the main curve was 21%. e, f The patient underwent a posterior instrumentation from T2 to L3. The shape memory alloy rod was served as a temporary correction template and was replaced by a rigid rod at the end of correction intraoperatively. The Cobb angle was corrected from 92° preoperatively to 32° postoperatively with a normal sagittal profile; the correction rate was 65%
Operative techniques
All patients underwent posterior fusion and instrumentation through a standard posterior midline incision. The soft tissue was dissected away from the bony spine in a subperiosteal fashion from the proximal to distal direction. Using anteroposterior and lateral radiographs, the ideal entry point and direction of pedicle screws were determined. The conventional fluoroscopy-based “free-hand” insertion technique was employed.
Before the operation, a preconfigured shape memory rod (usually 6 mm) was cooled in an asepsis ice bath. The predetermined shape used was that of a spine with normal coronal and sagittal alignment. Once the rod was cooled (below 4°C; the effect may be better if the rod was frozen in a refrigerator) and became malleable, it was contoured according to the shape of the spinal deformity. This allowed the rod to be easily seated in the concave pedicle screws. To ensure that the rod did not return to its preconfigured shape before it was completely seated, one surgeon filled the incision with a little crushed ice around the rod to control the local temperature. With the set screws loose and the rod in the appropriate sagittal alignment, the rod was warmed up using warm water (about 40°C). The shape memory rod returned to its predetermined shape gradually, resulting in a correction of the scoliotic deformity (Fig. 2). Concave distraction between adjacent level pedicle screws was applied to further reduce the major curve. After the correction, a permanent rigid spinal rod was fixed with anchors on the supporting side (convex side). The temporary shape memory rod was then replaced with a permanent rigid spinal rod. Additional compression and distraction were done to achieve better balance in the coronal plane. Facet decortication was performed using a high-speed burr, and facet fusion was performed with either allogenic bone graft or autogenous iliac crest bone graft.
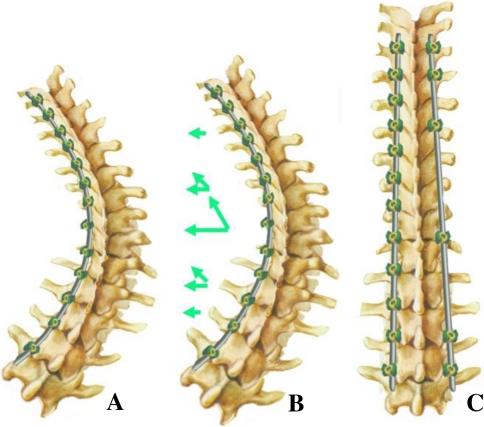
Fig. 2.
When the bent shape memory metal rod returned to its original shape (physiological curve of the spine in the sagittal plane and straight in the coronal plane), both axial torque and pulling forces were performed on the concave side of the spine, and derotation and translation were achieved simultaneously
Results
Surgical data
The mean blood loss at surgery was 680 ± 584 ml; the mean operative time was 278 ± 62 min; and the total hospital stay averaged 14.5 ± 3.9 days. Of the 22 patients with severe scoliosis, 18 (>70°) needed an average of 320 ml (200–600 ml) of homologous blood. Of the 16 patients with less severe scoliosis (<70°), only 3 needed homologous blood (Table 1).
Table 1.
Clinical and radiographic results of 22 severe scoliosis patients
| Patients | Lenke type | Major curve Cobb angle (°) | Flexibility of major curve (%) | Correction rate of major curve (%) | Osteotomy | Operation time (min) | Blood loss (ml) | Fusion lever | Complication | |
|---|---|---|---|---|---|---|---|---|---|---|
| Preoperatively IMPO | ||||||||||
| 1 | 1C− | 116 | 38 | 18 | 69 | No | 350 | 1,200 | T3–L3 | |
| 2 | 4AN | 92 | 32 | 21 | 65 | No | 220 | 400 | T2–L3 | |
| 3 | CON* | 80 | 24 | 26 | 70 | No | 385 | 680 | T3–L3 | |
| 4 | 4A− | 118 | 44 | 24 | 63 | No | 320 | 1,100 | T4–L4 | |
| 5 | 2A− | 95 | 28 | 16 | 70 | No | 260 | 380 | T2–L3 | |
| 6 | 1AN | 78 | 24 | 34 | 69 | No | 240 | 350 | T5–L2 | |
| 7 | 4CN | 112 | 29 | 41 | 74 | No | 350 | 800 | T2–L5 | |
| 8 | 2A+ | 87 | 30 | 25 | 65 | No | 245 | 380 | T2–L1 | |
| 9 | NM | 98 | 28 | 34 | 71 | No | 280 | 450 | T2–L3 | |
| 10 | 3CN* | 90/86 | 44/28 | 31/43 | 51/67 | No | 315 | 1,200 | T4–L4 | |
| 11 | 4A+ | 89 | 32 | 15 | 64 | No | 285 | 520 | T3–L3 | |
| 12 | 6CN | 96 | 30 | 28 | 69 | No | 320 | 580 | T4–L4 | |
| 13 | 4B+ | 86 | 25 | 31 | 71 | No | 260 | 420 | T2–L4 | |
| 14 | 1AN | 82 | 28 | 24 | 65 | No | 215 | 240 | T3–L2 | |
| 15 | CON | 105 | 42 | 14 | 60 | Yes | 420 | 1,800 | T4–L4 | |
| 16 | NM | 98 | 32 | 15 | 67 | Yes | 360 | 1,600 | T5–L4 | |
| 17 | 2AN | 84 | 26 | 30 | 69 | No | 280 | 480 | T3–L3 | |
| 18 | 2A+ | 84 | 30 | 23 | 64 | No | 215 | 350 | T2–L1 | |
| 19 | CON | 120 | 40 | 15 | 67 | Yes | 380 | 2,000 | T5–L4 | Deep infection |
| 20 | 4BN | 78 | 24 | 31 | 69 | No | 220 | 700 | T2–L4 | |
| 21 | NM | 88 | 30 | 34 | 65 | No | 280 | 900 | T5–L2 | |
| 22 | 4BN | 98 | 31 | 22 | 69 | No | 240 | 650 | T2–L4 | |
NM neuromuscular, CON congenital, IMPO immediate postoperative
Radiographic data
Of the 38 patients, 34 achieved a minimum of 2 years follow-up, while 4 were lost. The Cobb angle of the primary curve improved from average 78.4° preoperatively to 24.3° postoperatively (71.4% correction). In the 16 patients with the major curve <0°, the deformity improved from an average 56.7° preoperatively to 15.8° postoperatively (76% correction). In the 22 patients with the major curve >70°, the deformity improved from an average 94.1° preoperatively to 30.5° postoperatively (68% correction). There was about 2% loss of correction between the immediate postoperative radiographs to the final follow-up.
Clinical data
There were no neurologic or vascular complications. Only one case of deep postoperative infection was found within 2 months after the operation, and the patient recovered following thorough surgical debridement. There were no correction-related complications, such as screw pullout, loosening or metal fracture.
Discussion
Scoliosis is a three-dimensional deformity of the spine for which corrective surgery frequently is required. The goals of surgical treatment include: prevention of curve progression, correction of deformity, preservation of sagittal and coronal balance, improvement of cosmesis, preservation of pulmonary function, and minimization of morbidity or back pain [4, 7]. The correction techniques in scoliosis surgery, developed from Harrington principles of concave distraction, have evolved to include segmental realignment by rod derotation, cantilever and translation methods [6, 8, 12]. The ability to obtain greater fixation of the spine with current instrumentation has increased coronal plane deformity correction from 18% to nearly 70%, while maintaining global sagittal parameters [5, 9, 14]. Segmental pedicle screw fixation can further improve the three-dimensional correction by engaging all three columns of the spine [19], and segmental pedicle screw fixation with “direct vertebral rotation” showed better rotational and coronal correction than “simple rod derotation” [11, 13].
Current spinal corrective devices and techniques rely on forcing displaced vertebral bodies into alignment, usually by manual force, such that a rigid rod can be attached to the spine. A surgeon generally must make a compromise between the starting, deformed shape of the spine and the desired shape so that the spinal rods can be connected. The forces required to pull the vertebral bodies into alignment can be large, unevenly applied and sometimes difficult to control. Such techniques can be challenging for the surgeon especially when a large number of monoaxial pedicle screws are inserted at the apex. These procedures can lead to excessive stress on the pedicle screw resulting in screw pullout or screw damage.
Compared to rigid rod, such as stainless steel, titanium alloy or chrome cobalt-type rods, shape memory metal rod have two distinct states: austenitic and martensitic states. At low temperatures (usually below 4°C), the metal is in an austenitic state: it is malleable and can be easily contoured. This allows the rod to be seated into the deformed spine without any difficulty. Once the material is heated above its activation temperature (about 40°C, the activate point can be controlled by special technology), the shape memory material is stiff and automatically returns to its original, preselected shape. With shape memory alloy rod, the shape recovery forces were used to achieve a gradual three-dimensional scoliosis correction. Forces induce a bending moment to correct the lateral and sagittal curves of the scoliotic spine, and a torque to correct the axial rotation. Schmerling et al. [18] experimented with a shape memory metal rod to replace a standard Harrington rod in a human cadaver in the early 1970s. Lu [15] reported on surgical procedures in patients with an idiopathic scoliosis using shape memory metal rods instead of Luque rods in 1986. Wever [23] used a shape memory metal rod successfully to induce a scoliotic curve instead of correcting one in six pigs.
Undoubtedly, from a scientific point of view the permanent shape memory effect in vivo is not quite well understood. In addition, there is a fear of releasing wear debris at the junction between the rod and the anchoring system [21, 22]. In case of pseudoarthrosis, cyclic movements at the non-fused level may initiate corrosion and fretting processes, which may cause an increase in release of particulate wear debris. This was minimized since we used the shape memory rod as a temporary correction tool. The shape memory alloy rod was replaced by rigid rod at the end of correction. Therefore, this procedure takes advantage of the shape memory alloy, while minimizing its potential disadvantages.
Compared to traditional methods, shape memory metal-based correction is a novel form of scoliosis correction, in which a shape memory metal rod functions as the correcting element. By returning to its original shape (physiological curve of the spine in the sagittal plane and straight in the coronal plane), using the pedicles as points of attachment, applying both bending moment to correct the lateral and sagittal curves of the scoliotic spine and a torque to correct the axial rotation by means of external heating, a predominantly frontal scoliotic deformity is converted into a “normal” sagittal thoracic kyphosis or lumbar lordosis. This procedure includes two different, but coincident, processes: derotation and translation. So, shape memory metal rod-based correction is a three-dimensional scoliosis correction.
We have employed shape memory metal rod to correct scoliosis in pedicle construct. To gain further experience with the temporary tool, we first used it on patients with less severe scoliosis (<70°). The use of shape memory metal rod solves many of the concerns seen with more traditional techniques. The cooled rod can be contoured to easily fit the deformed spine. In addition, because this is an en bloc derotation and translation, the corrective forces are dispersed to all the pedicle screws rather than a single screw. This minimizes the concentration of stress and thereby avoids screw dislodgement and possibly minimizes operative time or blood loss.
In this study, woke test was performed after correction for all patients, and additional intraoperative somatosensory-evoked potentials was performed for patients with spinal osteotomy. We did not find significant loss of signal amplitude during the corrective phase. The reason may be owing to the characters of the shape memory alloy-based correction that it is a gradual correction rather than an acute one.
Since great results were achieved in patients with moderate scoliosis (<70°), the technique was also applied to patients with severe scoliosis (>70°), as well as patients with congenital scoliosis. In all cases, satisfactory results were obtained without any complications related to its use. We also believe that shape memory metal rod based scoliosis correction can be combined with other technique such as derotation, translation, as well as decancellation and vertebral resections.
Conclusion
In summary, given the results in this study, it is expected that the nitinol shape memory alloy rod can be safely and effectively used as a temporary tool during scoliosis correction. The advantages of this technique are excellent three-dimensional scoliosis correction, ease of use and decreased screw failure. In addition, this technique can be utilized for severe scoliosis.
Key points
Intraoperative use of the shape memory metal has advantage of physical features, while minimizing its potential disadvantages.
Shape memory metal-based correction is an independent form of scoliosis correction, in which a shape memory metal rod functions as the correcting element.
This is an en bloc derotation and translation, and the corrective power is dispersed to overall pedicle screws rather than a single screw.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Betz RR, Kim J, D’Andrea LP, et al. An innovative technique of vertebral body stapling for the treatment of patients with adolescent idiopathic scoliosis: a feasibility, safety, and utility study. Spine. 2003;28(Suppl 20):255–265. doi: 10.1097/01.BRS.0000092484.31316.32. [DOI] [PubMed] [Google Scholar]
- 2.Bezzi M, Orsi F, Salvatori FM, et al. Self-expandable nitinol stent for the management of biliary obstruction: long-term clinical results. J Vasc Intervent Radiol. 1994;5:287–293. doi: 10.1016/S1051-0443(94)71485-8. [DOI] [PubMed] [Google Scholar]
- 3.Braun JT, Hines JL, Akyuz E. Relative versus absolute modulation of growth in the fusionless treatment of experimental scoliosis. Spine. 2006;15:1776–1782. doi: 10.1097/01.brs.0000227263.43060.50. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH. Surgical treatment of idiopathic adolescent scoliosis. Spine. 1999;24:2607–2616. doi: 10.1097/00007632-199912150-00008. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell KH, Hanson DS, Rhee JM, et al. Correction of thoracic adolescent idiopathic scoliosis with segmental hooks, rods, and Wisconsin wires posteriorly: it’s bad and obsolete, correct? Spine. 2002;27:2059–2066. doi: 10.1097/00007632-200209150-00018. [DOI] [PubMed] [Google Scholar]
- 6.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop. 1988;227:10–23. [PubMed] [Google Scholar]
- 7.Haher TR, Merola A, Zipnick RI, et al. Metaanalysis of surgical outcome in adolescent idiopathic scoliosis. A 35-year English literature review of 11,000 patients. Spine. 1995;20:1575–1584. doi: 10.1097/00007632-199507150-00005. [DOI] [PubMed] [Google Scholar]
- 8.Harrington PR. Treatment of scoliosis: correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44:591–610. [PubMed] [Google Scholar]
- 9.Helenius I, Remes V, Yrjonen T, et al. Harrington and Cotrel-Dubousset instrumentation in adolescent idiopathic scoliosis. Long-term functional and radiographic outcomes. J Bone Joint Surg Am. 2003;85:2303–2309. doi: 10.2106/00004623-200312000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Henry M, Amor M, Beyar R, et al. Clinical experience with a new nitinol self-expanding stent in peripheral arteries. J Endovasc Surg. 1996;3:369–379. doi: 10.1583/1074-6218(1996)003<0369:CEWANN>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Kadoury S, Cheriet F, Beauséjour M, et al. A three-dimensional retrospective analysis of the evolution of spinal instrumentation for the correction of adolescent idiopathic scoliosis. Eur Spine J. 2009;18:23–37. doi: 10.1007/s00586-008-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Labelle H, Dansereau J, Bellefleur C, et al. Comparison between preoperative and postoperative three-dimensional reconstructions of idiopathic scoliosis with the Cotrel-Dubousset procedure. Spine. 1995;20:2487–2492. doi: 10.1097/00007632-199512000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Lee SM, Suk S, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine. 2004;29:343–349. doi: 10.1097/01.BRS.0000109991.88149.19. [DOI] [PubMed] [Google Scholar]
- 14.Liljenqvist U, Hackenberg L, Link TM, et al. Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg. 2001;67:157–163. [PubMed] [Google Scholar]
- 15.Lu SB, Wang JF, Guo JF et al (1986) Treatment of scoliosis with a shape-memory alloy rod. Zhonghua Wai Ke Za Zhi 24:129–132, 187 [PubMed]
- 16.Puttlitz CM, Masaru F, Barkley A, Diab M, et al. A biomechanical assessment of thoracic spine stapling. Spine. 2007;32:766–771. doi: 10.1097/01.brs.0000259073.16006.ed. [DOI] [PubMed] [Google Scholar]
- 17.Sanders JO, Sanders AE, More R, et al. A preliminary investigation of shape memory alloys in the surgical correction of scoliosis. Spine. 1993;18:1640–1646. doi: 10.1097/00007632-199309000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Schmerling MA, Wilkov MA, Sanders AE, et al. Using the shape recovery of nitinol in the Harrington rod treatment of scoliosis. J Biomed Mater Res. 1976;10:879–892. doi: 10.1002/jbm.820100607. [DOI] [PubMed] [Google Scholar]
- 19.Suk S, Lee CK, Kim W, et al. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 20.Szold A. Nitinol: shape-memory and super-elastic materials in surgery. Surg Endosc. 2006;20:1493–1496. doi: 10.1007/s00464-005-0867-1. [DOI] [PubMed] [Google Scholar]
- 21.Vieweg U, van Roost D, Wolf HK, et al. Corrosion on an internal spinal fixator system. Spine. 1999;24:946–951. doi: 10.1097/00007632-199905150-00004. [DOI] [PubMed] [Google Scholar]
- 22.Wang JC, Yu WD, Sandhu HS, et al. Metal debris from titanium spinal implants. Spine. 1999;24:899–903. doi: 10.1097/00007632-199905010-00011. [DOI] [PubMed] [Google Scholar]
- 23.Wever DJ, Elstrodt JA, Veldhuizen AG, et al. Scoliosis correction with shape-memory metal: results of an experimental study. Eur Spine J. 2002;11:100–106. doi: 10.1007/s005860100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.