Abstract
The correction rate (CR) and fulcrum bending correction index (FBCI) based on the fulcrum bending radiograph (FBR) were parameters introduced to measure the curve correcting ability; however, such parameters do not account for contributions by various, potential extraneous “X-Factors” (e.g. surgical technique, type and power of the instrumentation, anesthetic technique, etc.) involved in curve correction. As such, the purpose of the following study was to propose the concept of the “X-Factor Index” (XFI) as a new parameter for the assessment of the correcting ability of adolescent idiopathic scoliosis (AIS). A historical cohort radiographic analysis of the FBR in the setting of hook systems in AIS patients (Luk et al. in Spine 23:2303–2307, 1998) was performed to illustrate the concept of XFI. Thirty-five patients with AIS of the thoracic spine undergoing surgical correction were involved in the analysis. Plain posteroanterior (PA) plain radiographs were utilized and Cobb angles were obtained for each patient. Pre- and postoperative PA angles on standing radiograph and preoperative fulcrum bending angles were obtained for each patient. The fulcrum flexibility, curve CR, and FBCI were determined for all patients. The difference between the preoperative fulcrum bending angle and postoperative PA angle was defined as AngleXF, which accounted for the correction contributed by “X-Factors”. The XFI, designed to measure the curve correcting ability, was calculated by dividing AngleXF by the fulcrum flexibility. The XFI was compared with the curve CR and FBCI by re-evaluating the original data in the original paper (Luk et al. in Spine 23:2303–2307, 1998). The mean standing PA and FBR alignments of the main thoracic curve were 58.3° and 24.5°, respectively. The mean fulcrum flexibility was 58.8%. The mean postoperative standing PA alignment was 24.7°. The mean curve CR was 58.0% and the mean FBCI was 101.1%. The mean XFI was noted as 1.03%. The CR was significantly positively correlated to curve flexibility (r = 0.66; p < 0.01).The FBCI (r = −0.47; p = 0.005) and the XFI (r = −0.45; p = 0.007) were significantly negatively correlated to curve flexibility. The CR was not correlated to AngleXF (r = 0.29; p = 0.089).The FBCI (r = 0.97; p < 0.01) and the XFI (r = 0.961; p < 0.01) were significantly positively correlated to AngleXF. Variation in XFI was noted in some cases originally presenting with same FBCI values. The XFI attempts to quantify the curve correcting ability as contributed by “X-Factors” in the treatment of thoracic AIS. This index may be a valued added parameter to accompany the FBCI for comparing curve correction ability among different series of patients, instrumentation, and surgeons. It is recommended that the XFI should be used to document curve correction, compare between different techniques, and used to improve curve correction for the patient.
Keywords: Scoliosis, Fulcrum bending, Radiograph, Flexibility, Curve, Correction, Rate, Index, X-Factor
Introduction
The ability to surgically manage adolescent idiopathic scoliosis (AIS) has tremendously evolved since Harrington’s first introduction of spinal instrumentation for deformity correction in the late 1950s [6]. Not only various spinal instrumentation has been developed throughout the years, other advances have also improved the surgeon’s ability to manage AIS. For example, the ability to perform more aggressive release of anatomic structures, the development of pedicle subtraction osteotomies, improvements in anesthesia and spinal cord monitoring, more advantageous surgical positioning, enhanced techniques and biologics to improve fusion, and the use of intraoperative imaging have all enhanced our ability to treat patients with AIS and to achieve a greater amount of curve correction [7, 8].
Assessing radiographic parameters provides a reflection of the amount of curve correction and an estimation of correcting ability resulting from surgical intervention. Correction rate (CR) is the most popular parameter used to describe the surgical outcome of curve correction. However, various studies assessing surgical outcomes of AIS patients have reported varying degrees of curve CR [4, 12]. Studies have shown that the curve CR is influenced by the curve’s preoperative flexibility [1, 10]. To address such an aspect of inherent curve characteristics, the fulcrum bending correction index (FBCI) was proposed in 1998 by Luk et al. [10] to account for the curve CR in the context of the curve’s flexibility. Fulcrum bending radiograph (FBR) with the patient lying sideways over a fulcrum made from a large plastic cylinder is taken to determine the fulcrum bending flexibility. The FBCI indicates how much the surgery has taken up the flexibility of the curve as revealed by FBR. However, the FBCI may not reflect how much “correcting ability” may be contributed by numerous, potentially extraneous “X-Factors” which are mentioned above, such as surgeon’s effort to maximize correction within the safe limits of the neurology, power of the instrumentation, anesthetic technique, etc.
To quantify the contribution of such potential “X-Factors” needed to achieve a certain correction, we propose another parameter—the “X-Factor Index” (XFI). Therefore, the objective of this study was to address the concept of the XFI by assessing radiographically the viability of CR, FBCI, and our new index to the surgical outcome of AIS curve correction by referring for illustrative purposes to the historical cohort of AIS patients initially reported in 1998 by Luk et al. [10] proposing the FBCI parameter.
Materials and methods
Our study utilized a historical cohort of AIS patients previously published by Luk et al. [10] for illustrating the concept of XFI. In the original paper proposing FBCI, 35 patients with AIS requiring surgical correction were studied prospectively. There were 6 males and 29 females with a mean age at the time of operation of 15 years (range 11–20 years). According to King’s classification of AIS [9], the curve types were as follows: 22 patients were type II, 11 patients were type III, 1 patient was type IV, and 1 patient was type V. Because the majority of patients had types II and III King curves; only the thoracic curves had arthrodesis; therefore, only correction of the thoracic curves was described. Plain coronal radiography was utilized in all patients. The Cobb angle (°) was obtained for all radiographic measurements of the coronal spinal alignment [3]. All patients underwent posterior spinal arthrodesis using TSRH instrumentation performed by the same group of surgeons using the same techniques. As part of the preoperative assessment, all patients underwent standing posteroanterior (PA) and FBR. These radiographs were compared with the correction shown on the first postoperative standing PA radiograph obtained 1 week after surgery. The technique of the FBR is described in detail elsewhere [1].
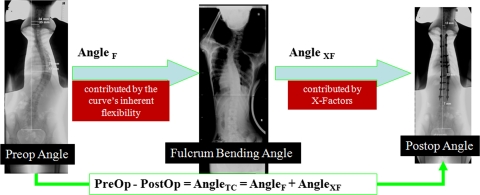
The difference between the Cobb angles measured on the preoperative and postoperative standing PA radiographs was defined as AngleTC, which signified the angle of total correction and consisted of two parts: (1) the angle contributed by the inherent flexibility of the curve (AngleF) and (2) the angle contributed by “X-Factors” (AngleXF) (Eq. 1) (Fig. 1). The difference between the Cobb angles measured on the preoperative standing PA radiograph and FBR was defined as AngleF, signifying the angles contributed by the inherent flexibility (Eq. 2) (Fig. 1). The difference between the Cobb angles measured on the preoperative FBR and postoperative standing PA radiographs was defined as AngleXF, which signified the angle contributed by the “X-Factors” (Eq. 3) (Fig. 1). The fulcrum flexibility, CR, FBCI, and XFI were calculated by Eqs. 4, 5, 6, 7.
 |
1 |
 |
2 |
 |
3 |
 |
4 |
 |
5 |
 |
6 |
 |
7 |
With regards to the XFI, when the index was negative, it implied that the correcting ability was less than that needed to take up the correctability permitted by the curve’s flexibility. A zero XFI did not imply that the surgical team or overall “X-Factors” did not devote a degree of effort to correct the curve; but rather there was no more correction ability needed to achieve the same correction permitted by the flexibility of the curve. Finally, in the event, the XFI was positive, the correction ability exceeded that which was needed to achieve the correctability of the curve as permitted by the curve’s flexibility. Correction ability was defined as being multi-faceted and consisted of numerous extraneous developing X-Factors as previously noted, such as the experience of the surgeon to correct the deformity within neurological limits, the power of the selected instrumentation, the surgical technique adopted, anesthetic technique, spinal cord monitoring, etc.
Fig. 1.
The difference between the Cobb angles measured on the preoperative and postoperative standing PA radiographs was defined as angleTC, which signified the angle of total correction and consisted of two parts: (1) the angle contributed by the inherent flexibility of the curve (AngleF) and (2) the angle contributed by “X-Factors” (AngleXF)
All data were collected and coded upon a spreadsheet. SPSS vr. 14 software (Chicago, USA) was utilized to perform the statistical analyses. Descriptive and frequency analyses were performed of the data set. Pearson’s test was performed to assess the correlation between continuous data parameters. As the “r value” of the correlation test approached the value of “1”, the strength of the association increased. An “r value” greater than 0.90 was regarded as demonstrating a high degree of correlation. Statistical significance was established at p < 0.05.
Results
A summary of the radiographic parameters is illustrated in Table 1. The mean standing and FBR Cobb angles were 58.3° and 24.5°, respectively. The mean FBR flexibility was 58.8%. Postoperatively, the mean AngleTC and AngleXF were 33.6° and −0.23°, respectively. The mean postoperative standing PA Cobb angle was 24.7°. The mean curve CR was 58.0% and the mean FBCI was 101.1%. The mean XFI was noted as 1.03.
Table 1.
Descriptive analyses of various demographic and radiographic parameters
| Mean (±SD, range) | |
|---|---|
| Preoperative | |
| Standing PA Cobb angle (degrees) | 58.3 (9.3, 40–77) |
| FBR Cobb angle (degrees) | 24.5 (11.1, 5–45) |
| FBR flexibility (%) | 58.8 (16.2; 26–90) |
| Postoperative | |
| AngleTC (degrees) | 33.6 (9.3, 10–55) |
| AngleXF (degrees) | −0.23 (7.0, −19–15) |
| Standing PA Cobb angle (degrees) | 24.7 (9.8, 8–44) |
| Correction rate (%) | 58.0 (14.4, 21–84) |
| FBCI (%) | 101.1 (20.6, 57–150) |
| XFI | 1.03 (12.0, −21.1–35.0) |
PA posteroanterior, FBR fulcrum bending radiograph, FBCI fulcrum bending correction index, AngleTC angle of total correction, AngleXF angle contributed by the surgical team, XFI X-Factor Index
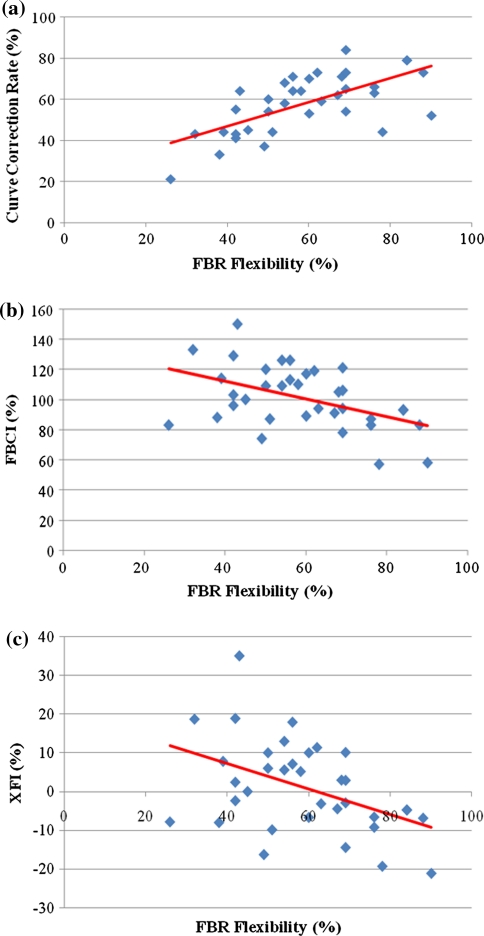
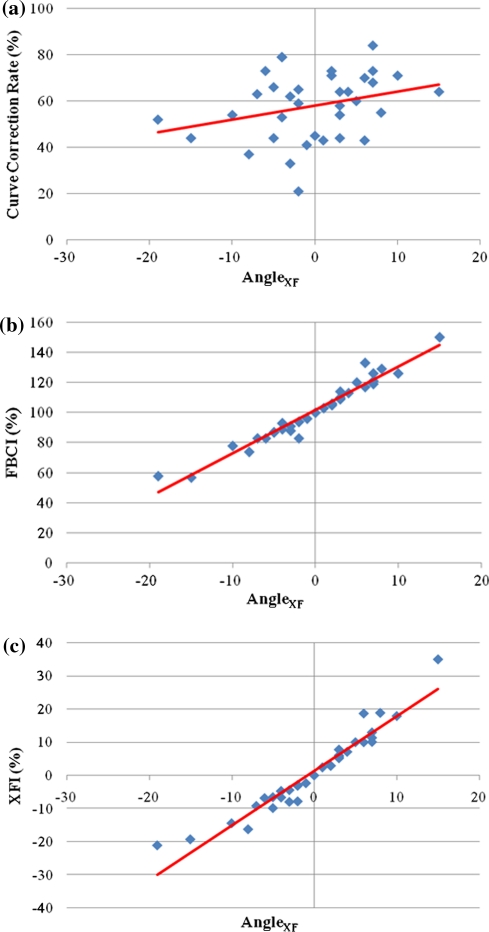
An increase in curve CR was significantly noted with elevated curve flexibility values (r = 0.66; p < 0.01) (Fig. 1a). However, curve CR was not correlated to AngleXF (r = 0.29; p = 0.089) (Fig. 2a). The FBCI (r = −0.47; p = 0.005) (Fig. 1b) and the XFI (r = −0.45; p = 0.007) (Fig. 1c) were significantly negatively correlated to curve flexibility, denoting that with an increase in curve flexibility the FBCI and the XFI values decreased. The FBCI (r = 0.97; p < 0.01) (Fig. 2b) and the XFI (r = 0.96; p < 0.01) (Figs. 2c, 3) were significantly positively correlated to AngleXF. In addition, there were similar FBCI values noted for 6 sets (1 set 3 patients, 5 sets 2 patients each), representing 13 patients in total; however, the XFI varied in 50% of the cases where the FBCI was similar.
Fig. 2.
Scatterplot distribution of the fulcrum bending radiograph (FBR) flexibility to the (a) curve correction rate, the (b) fulcrum bending correction index (FBCI) and the (c) X-Factor Index (XFI). The greater the deviation of the plotted points from the straight linear trend line, the decrease in association between the two variables
Fig. 3.
Scatterplot distribution of the angle contributed by “X-Factors” (AngleXF) to the (a) curve correction rate, the (b) fulcrum bending correction index (FBCI) and the (c) X-Factor Index (XFI). The greater the deviation of the plotted points from the straight linear trend line, the decrease in association between the two variables
Discussion
Spinal surgery has evolved and developed tremendously during the last few decades, enhancing the ability to treat patients with AIS and to achieve a greater amount of curve correction [7, 8]. Although curve correction solely is not the most important factor for surgical intervention in AIS, authors have noted that patients are more satisfied by more curve correction [5]. Surgeons seek to improve the curve correction by developing different techniques, instrumentation, surgical strategies, etc. Therefore, to improve upon such factors, the correcting ability by various, potentially extraneous “X-Factors” should be documented to facilitate scoliosis correction.
In our study, the curve correction (AngleTC, angle of total correction), expressed as the difference between the angles on pre- and postoperative PA radiographs, consists of two parts: the correction attributed to the inherent flexibility of the curve (AngleF) which is a constant for a given curve and the correction attributed to “X-Factors” (AngleXF), which may vary (Eq. 1, Fig. 1). AngleF represents the maximum correction permitted by the inherent flexibility of the curve (Eq. 2). For a given curve, it theoretically is an inherent characteristic, which may be estimated based on the curve’s flexibility. AngleXF (Eq. 3) represents the contribution by “X-Factors” to the total correction (AngleXF), which can be calculated by subtracting AngleF from AngleTC. As previously described, many factors may potentially contribute to AngleXF. These factors cannot be isolated and may act in combination during surgery. Therefore, the X-Factors were used to represent such a concept. However, such factors are always evolving and with their improvement the correcting ability is improved and AngleXF may be enhanced accordingly. For example, for a given curve corrected by different surgical teams, if AngleTC is different following surgery, the difference is due to the part of AngleXF which reflects factors part of the surgical management. Improved developments in spinal surgery can only increase the component of AngleXF. The amount of AngleXF can partially reflect the ability/effort to correct the deformity. To some degree, the flexibility of the curve may represent difficulties in curve correction. Most surgeons agree that it would obviously be more difficult to achieve the same correction in a rigid than in a flexible curve [11]. Thus, to simplify this problem, the flexibility of the indexed curve is accounted to signify the correcting difficulty. As such, the concept of XFI may be introduced, which is expressed as AngleXF divided by the curve’s flexibility as revealed by the FBR. In our series, the fulcrum bending method was used; thus, the XFI was calculated accounting for both the “X-Factors” and the curve’s inherent flexibility (Eq. 7).
The “CR” is the most popular parameter based on curve correction in describing the surgical outcome of scoliosis correction, but studies have shown that CR is positively correlated with the fulcrum flexibility of the curve [11], which is also revealed by this study (Fig. 2a). Thus, curve CR reflects the intrinsic character of the curve and a higher CR does not necessarily mean a higher correction ability. Similarly, a lower CR does not necessarily mean a lower correction ability. Based on the equation of the curve CR (Eq. 5), it also can be seen that AngleF is part of the numerator, which implies that CR includes the contribution of the inherent flexibility of the curve. As such, the curve CR may not allow comparisons between different “X-Factors” and may at times be deceiving [11].
Being well aware of the limitations associated with the curve CR, the senior authors of this article introduced the FBCI (Eq. 6) to describe frontal plane correction [10]. In the original paper describing FBCI, the authors concluded that the FBCI took into account the curve flexibility and was therefore superior than the CR for comparing curve correction and use of instrumentation systems between different series of patients [11]. The FBCI can signify how much the surgical correction has taken up the flexibility of the curve as revealed by the FBR [10, 11]. As such, a FBCI of 100% indicates that the surgical correction has taken up all the flexibility of the curve as revealed by the FBR.
It is well known that to achieve a certain degree of correction, the more rigid the curve, the more correction ability is required [2, 10]. In our study, a similar significant high correlation was noted between AngleXF to that of FBCI and XFI. However, in assessing the individual cases in our historical cohort initially reported by Luk et al. [10] the following cases noted in Table 2 may serve as a good example to illustrate the potential weakness of the FBCI in comparison to the curve correcting ability contributed by “X-Factors”. For example, both cases 29 and 5 demonstrated the same AngleTC and AngleXF after surgery, even though the curve of case 29 is smaller and more flexible than that of case 5. Thus, the correction ability attributed to various potential “X-Factors” should vary. However, the FBCI of cases 29 and 5 are the same, which may not reflect the difference of correction ability by the “X-Factors”. In a similar manner, the same FBCI in cases 11 and 33 also does not reflect the difference of such correcting ability. Therefore, such variations are suggestive that the XFI may possess a heightened sensitivity to added factors involved in the correction of the curve in AIS patients.
Table 2.
Cases examples derived from Luk et al. [10] showing the weakness of the FBCI
| Case no. | Preoperative standing PA Cobb angle (degrees) | FBR Cobb angle (degrees) | Fulcrum flexibility (%) | Postoperative standing PA Cobb angle (degrees) | AngleTC (degrees) | AngleF (degrees) | AngleXF (degrees) | FBCI (%) | XFI |
|---|---|---|---|---|---|---|---|---|---|
| 5 | 70 | 35 | 50 | 32 | 38 | 35 | 3 | 109 | 6.00 |
| 29 | 65 | 30 | 54 | 27 | 38 | 35 | 3 | 109 | 5.57 |
| 11 | 75 | 37 | 51 | 42 | 33 | 38 | −5 | 87 | −9.87 |
| 33 | 50 | 12 | 76 | 17 | 33 | 38 | −5 | 87 | −6.58 |
PA posteroanterior, FBCI fulcrum bending correction index, AngleTC angle of total correction, AngleXF angle contributed by the surgical team, XFI X-Factor Index
Table 3 further illustrates the weakness of the curve CR and the FBCI. It is obvious that the curve in case 1 is much larger and more rigid than in case 2. A total curve correction of 40° was achieved in both cases. Apparently, more correcting ability is needed in case 1. However, when using the curve CR and FBCI to evaluate the surgical outcome, we obtain confusing results—the CR of case 2 is twice that of case 1 and the FBCIs are the same. Obviously, half of the higher curve CR of case 2 is attributed to the inherent higher flexibility of the curve and does not indicate that more effort has been contributed by the “X-Factors.” Similarly, the same FBCIs in both cases also cannot distinguish the difference of the correcting ability attributed during the surgery. This is due to the fact that FBCI measures the correcting ability indirectly by calculating how much the surgery has taken up the flexibility. In addition, Eq. 6 shows that AngleF is also part of the numerator, which signifies that FBCI does not remove the contribution of the curve flexibility. When compared with CR and FBCI, the new parameter of XFI removes the contribution of the curve flexibility and measure the correcting ability directly. So whenever the correcting ability is concerned, XFI should be used to document the surgical outcome.
Table 3.
Case examples
| Case | Preoperative standing PA Cobb angle (degrees) | FBR Cobb angle (degrees) | Fulcrum flexibility (%) | Postoperative standing PA Cobb angle (degrees) | AngleTC (degrees) | AngleF (degrees) | AngleXF (degrees) | Curve correction rate | FBCI (%) | XFI |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 100 | 80 | 20 | 60 | 40 | 20 | 20 | 40 | 200 | 100 |
| 2 | 50 | 30 | 40 | 10 | 40 | 20 | 20 | 80 | 200 | 50 |
PA posteroanterior, FBR fulcrum bending radiograph, AngleXF angle contributed by the surgical team, FBCI fulcrum bending correction index, XFI X-Factor Index
There are four salient issues to be mindful of with regards to the XFI. First, the XFI takes into account both the flexibility of the curve based on the FBR and the correcting contribution of “X-Factors” as previously discussed contributing to the correction. Thus, correcting ability does not simply mean the correcting force and it is always evolving with technological advancements, improved surgical strategies and techniques, and other factors. Secondly, the XFI is just an indicator of the correcting ability, not an accurate measurement. This is due to the fact that the relationship between correcting ability and correction may not be linear, that the flexibility beyond and below the correctability permitted by the FBR may be different and that there are some inherent deficiencies/limitations associated with the FBR which can only approach but not reveal the maximal flexibility. Thirdly, when the XFI is used to compare the correcting ability between different series, the flexibility evaluating methods should be the same. The parameters used to calculate XFI should be utilized in the context of the method used to assess the curve’s flexibility. For example, when active lateral side bending is used to evaluate the curve’s flexibility, the XFI can account for such a method; however, further study and validation should be addressed. The closer the flexibility revealed approaches the “maximum flexibility,” the more accurate the XFI, otherwise, the ability will be exaggerated. Finally, the primary goal of AIS surgery is to achieve a balanced spine. As such, surgeons should not try to maximize their X-Factors by compromising this goal, but rather utilize the XFI to monitor and maximize their X-Factors as they see fit.
Conclusion
Spinal surgeons should be cognizant of additional factors needed for curve correction that may not be solely illustrated by the curve’s flexibility on FBR assessment, such as those contributed by various, potential extraneous “X-Factors.” The XFI attempts to quantify the curve’s correcting ability as contributed by such “X-Factors” in the treatment of thoracic AIS. This index may measure the correcting ability directly and is a better indicator than the curve CR and FBCI for comparing curve correction ability among different series of patients. However, since high correlation and utility has been documented with the FBCI, the XFI is a new parameter not intended to replace the FBCI but be utilized in conjunction to account for potential variation in curve correction. Overall, it is recommended that the XFI should be used to document curve correction, comparisons between different techniques, and used to improve curve correction for the patient.
Conflict of interest
The authors have no financial or competing interests related to this work to disclose.
Abbreviation list
- AIS
Adolescent idiopathic scoliosis
- FBR
Fulcrum bending radiograph
- CR
Correction rate
- FBCI
Fulcrum bending correction index
- XFI
X-Factor Index
- AngleTC
The angle of total correction
- AngleF
The correction angle contributed by the inherent flexibility of the curve
- AngleXF
The correction angle contributed by “X-Factors”
Contributor Information
Dino Samartzis, Email: dsamartzis@msn.com.
Keith D. K. Luk, Phone: +852-22554254, FAX: +852-28174392, Email: hrmoldk@hku.hk
References
- 1.Cheung KM, Luk KD. Prediction of correction of scoliosis with use of the fulcrum bending radiograph. J Bone Joint Surg Am. 1997;79:1144–1150. doi: 10.2106/00004623-199708000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Cheung KMC, Natarajan D, Samartzis D, Wong YW, Cheung WY, Luk KDK. Predictability of the fulcrum bending radiograph in thoracic adolescent idiopathic scoliosis correction with alternate level pedicle screw fixation. J Bone Joint Surg (Am) 2010;92:169–176. doi: 10.2106/JBJS.H.01831. [DOI] [PubMed] [Google Scholar]
- 3.Cobb JR. Conditions involving the spine and thorax exclusive of those in the lower part of the back. Arch Surg. 1949;59:1335–1346. [PubMed] [Google Scholar]
- 4.Dobbs MB, Lenke LG, Kim YJ, Luhmann SJ, Bridwell KH. Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90 degrees. Spine. 2006;31:2386–2391. doi: 10.1097/01.brs.0000238965.81013.c5. [DOI] [PubMed] [Google Scholar]
- 5.Haher TR, Merola A, Zipnick RI, Gorup J, Mannor D, Orchowski J. Meta-analysis of surgical outcome in adolescent idiopathic scoliosis. A 35-year English literature review of 11,000 patients. Spine. 1995;20:1575–1584. doi: 10.1097/00007632-199507150-00005. [DOI] [PubMed] [Google Scholar]
- 6.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44-A:591–610. [PubMed] [Google Scholar]
- 7.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2004;29:2040–2048. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 8.Kim YJ, Lenke LG, Kim J, Bridwell KH, Cho SK, Cheh G, Sides B. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2006;31:291–298. doi: 10.1097/01.brs.0000197865.20803.d4. [DOI] [PubMed] [Google Scholar]
- 9.King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:1302–1313. [PubMed] [Google Scholar]
- 10.Luk KD, Cheung KM, Lu DS, Leong JC. Assessment of scoliosis correction in relation to flexibility using the fulcrum bending correction index. Spine. 1998;23:2303–2307. doi: 10.1097/00007632-199811010-00011. [DOI] [PubMed] [Google Scholar]
- 11.Luk KD, Lu DS, Cheung KM, Wong YW. A prospective comparison of the coronal deformity correction in thoracic scoliosis using four different instrumentations and the fulcrum bending radiograph. Spine. 2004;29:560–563. doi: 10.1097/01.BRS.0000106494.14707.B2. [DOI] [PubMed] [Google Scholar]
- 12.Wojcik AS, Webb JK, Burwell RG. Harrington–Luque and Cotrel–Dubousset instrumentation for idiopathic thoracic scoliosis. A postoperative comparison using segmental radiologic analysis. Spine. 1990;15:424–431. doi: 10.1097/00007632-199005000-00015. [DOI] [PubMed] [Google Scholar]