Abstract
In adolescent idiopathic scoliotic girls, postural imbalance is attributed to a sensory rearrangement of the motor system on the representation of the body in space. The objectives of this study were to test if the anteroposterior (AP), mediolateral (ML) and resultant body–head and trunk center of mass (COM) horizontal offsets were similar in able-bodied and scoliotic girls and if these offsets were related to the center of pressure displacements. A total of 21 adolescent idiopathic scoliosis girls and 20 able-bodied girls participated in this study. Their body COM position and that of the head and trunk were estimated according to Damavandi et al. (Med Eng Phys 31:1187–1194, 2009). The COP range and speed in both AP and ML axes were calculated from force plate measurements in quiet standing. The AP offset of the able-bodied group was anterior to the body COM by 11.0 ± 15.9 mm, while that of the scoliotic group was posterior to it by −17.3 ± 11.2 mm. The able-bodied group maintained their head–trunk segment COM more to the right by 14.1 ± 13.1 mm, while that of the scoliotic group was nearly over their body centerline. The scoliotic girls presented higher values for COP range and COP speed than the able-bodied girls. The resultant COM offset was correlated with both the ML COP range and speed only for the scoliotic girls. The small ML COM offset in the scoliotic girls was attributed to a compensatory action of the spinal deformity in the frontal plane resulting in a backward resultant COM offset to regain postural balance concomitant to an increase in the ML neuromuscular demand.
Keywords: Adolescent idiopathic scoliosis, Trunk, Center of mass, Center of pressure, Standing balance
Introduction
Though adolescent idiopathic scoliosis (AIS) is characterized by a lateral deviation of the spine with resulting geometric changes in the trunk [2, 3] and rib cage [4], standing imbalance was reported by Sahlstrand et al. [5] and Byl and Gray [6]. Standing ability is usually defined by the amount of body sway when a subject is standing on a force plate [7]. The control of the center of mass (COM) with respect to the base of support is dependent on the point of application of the ground reaction forces known as the center of pressure (COP). The displacement of the COP is considered as a measure of body neuromuscular demand to maintain standing stability [8]. In AIS, postural imbalance was attributed to a sensory rearrangement of the motor system on the representation of the body in space [9]. Though the center of mass is the balance point of the body and the single best indicator of a body’s position, Engsberg et al. [10] stressed that the position and orientation of major body segments such as the trunk could play a more critical role in preoperative decision and evaluating efficacy. To our knowledge, the relationship between the body center of mass and that of the trunk to standing balance is still to be ascertained in AIS.
According to Gauchard et al. [11], the type and location of the spinal deformity modify balance control where patients with double major curves are more stable than those with lumbar curve. They concluded that the location of the major curve is not only important, but also had an effect on lateral upright disequilibrium. Interaction between standing posture and balance was documented by Nault et al. [12] who suggest a dysfunction in the postural regulation system of scoliotic subjects. Allard et al. [13] reported that postural responses appeared to be dependent on body somatotypes and in particular that ectomorphic girls had a tendency to lean further back favoring a hypokyphotic trunk attitude, increasing the risk of spinal deformity progression. These observations on spinal deformity and body shape alterations that modify trunk COM position imply a change in the body center of mass position that could perturb standing balance.
Using magnetic resonance imaging, Engsberg et al. [10] first reported values for the whole body COM in three scoliotic adults. They observed that the restoration of the coronal and sagittal plane body COM balance could be used to assist surgical planning and help assess surgical outcomes. Damavandi et al. [14] reported in a group of 21 AIS girls and in a comparable group of 20 able-bodied girls a greater horizontal COM offset in scoliotic girls. This offset was defined as the difference between the COM of the whole body minus that of the head and trunk segment. Nonetheless, they did not discuss if this COM offset could be linked to standing imbalance in AIS.
It is hypothesized here that an increase in the horizontal COM offset exacerbates standing balance requiring a greater neuromuscular demand in scoliotic girls. The objectives of this study were to test if the anteroposterior (AP), mediolateral (ML) and resultant COM offsets were similar in able-bodied and scoliotic girls and if these offsets were related to the center of pressure displacements.
Method
A total of 21 girls were diagnosed with adolescent idiopathic scoliosis by an orthopedic surgeon according to the criteria defined by Bunnel [15]. Their mean age, height and weight were 11.7 ± 3.1 years, 148.4 ± 17 cm and 40.0 ± 13.3 kg, respectively. All subjects had a right thoracic curve and none was under active treatment that could influence their standing balance. It was important to have a group of scoliotic subjects who displayed a wide range of Cobb angle to establish a relation between the COM offsets and standing balance parameters. Cobb angle varied from 5° to 28° reflecting a mean value of 13.5° ± 5.5°. A similar group of 20 girls formed the control group and none had any form of scoliosis and all were in general good health. This group was comparable in age (12.5 ± 1.3 years), height (156.3 ± 7.7 cm) and weight (43.7 ± 6.9 kg) to the scoliotic group. All the girls and their parents signed the informed consent form approved by the hospital ethics committee.
The procedure to estimate body COM position and that of the head and trunk is based on the work of Damavandi et al. [1]. First, the COM of the whole body is calculated. With the subject standing on the force plate (AMTI, Model OR6-5, Newton, MA), data were collected at 60 Hz for a period of 5 s and then filtered using a fourth-order low-pass Butterworth filter with a 6 Hz cutoff frequency [16]. The mean COP anteroposterior and mediolateral positions were calculated from the forces and moments measured by the force plate. These values correspond to the whole body COM [17]. The position of the COM with respect to the feet or its height is obtained by the reaction board method. This method requires that the subject lies on a heavy and rigid board supported at one end by the force plate and a triangular support at the other end. Using the equilibrium equations, the body COM is estimated within a 1% difference to that of the standing posture [18].
Generally, the COM position of the individual body segments is estimated from changes in force plate readings taken in two different positions while lying on the board [1]. Firstly, force plate data are obtained with the arms alongside the trunk of the subject. Afterward, a body segment is displaced; for example, the right upper limb is flexed to 90°. This was carried out for the other upper and lower limbs. Then, head and trunk COM position was calculated with respect to the mid-hip position. Damavandi et al. [1] reported that errors of 1.2 and 2.8 mm in the average COP values had negligible effect on the calculated mass and COM values when a body segment COM position was changed by 5 and 10 mm, respectively. The method to estimate the mass and center of mass of body segments described by Damavandi et al. (2009) was tested in individuals with different body mass index (i.e., lean, normal and obese) to verify its sensitivity. All the segmental mass and COM values obtained from the force plate method were within the range of those of the other methods. COM offset is defined as the difference between the head and trunk COM and that of the whole body. COM offsets were calculated along the AP and ML axes. The resultant offsets consisted of the square root of the sum of the squared AP and ML offsets.
Quiet standing balance was tested using the AMTI force plate. The feet position was standardized by means of a wooden rig lying on the force plate [19]. With the subject standing barefoot, the heels were spaced by 23 cm and the midline of the feet pointing externally by 15°. Once the subject was in position, the rig was removed. Subjects were then asked to stand quietly with their arms on each side and focused on a target placed at 1.2 m ahead and located at eye level. Three trials of 30 s were performed at a sampling frequency of 64 Hz [12, 13, 20]. The AP and ML COP values were calculated from the forces and moments measured during the trial. From these, the COP range that corresponds to difference between the maximal and minimal COP values and the mean COP speed (sum of COP displacements/30 s) in both AP and ML axes were calculated for each trial. A large COP range is suggestive of standing imbalance [21], while a high COP speed corresponds to a strong demand from the neuromuscular system [22] to avoid loss of balance.
ANCOVAs were performed on the AP, ML and resultant COM offsets as well as the AP and ML ranges and speeds with age, body mass and height as covariables. Post hoc analyses were carried out using a Bonferroni correction if a statistical difference was observed (P ≤ 0.05). Coefficients of correlation were calculated between the three COM offsets and the four balance parameters for both groups with a statistically significant level of P ≤ 0.05.
Results
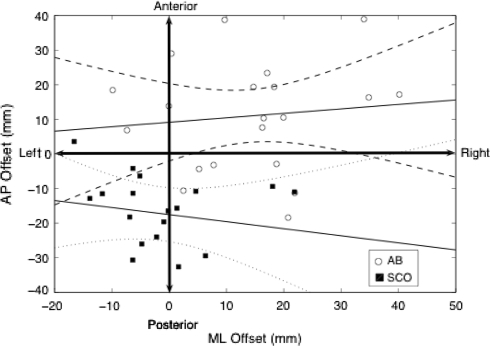
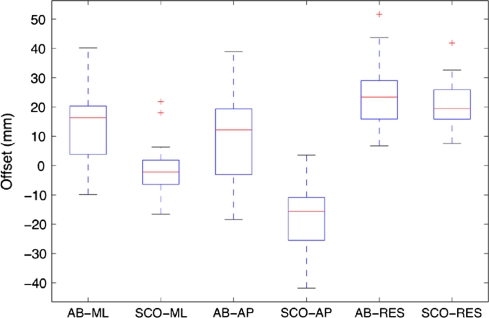
Figure 1 illustrates the horizontal positions of the COM of the head and trunk segment with respect to that of the COM of the whole body for able-bodied and scoliotic subjects. The mean anteroposterior offset of the able-bodied group shown in Fig. 2 is oriented anteriorly (P < 0.01) to the body COM by 11.0 ± 15.9 mm, while that of the scoliotic group is directed posteriorly at −17.3 ± 11.2 mm (P < 0.01). The able-bodied group maintained their mean head and trunk segment COM more to the right (P < 0.01) of the body COM by 14.1 ± 13.1 mm, while the head–trunk segment COM of the scoliotic group was nearly over their body centerline at −1.3 ± 9.6 mm (P < 0.01). No statistical difference (P = 0.32) was observed in the resultant offset of the able-bodied (24.2 ± 12.1 mm) and the scoliotic (20.8 ± 8.2 mm) girls.
Fig. 1.
Horizontal position of the center of mass of the head and trunk segment with respect to that of the whole body (offset in mm) in able-bodied and scoliotic girls
Fig. 2.
Anteroposterior (AP), mediolateral (ML) and resultant (RES) horizontal offsets in able-bodied (AB) and scoliotic (SCO) girls
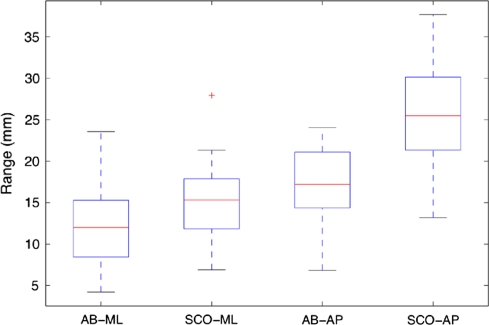
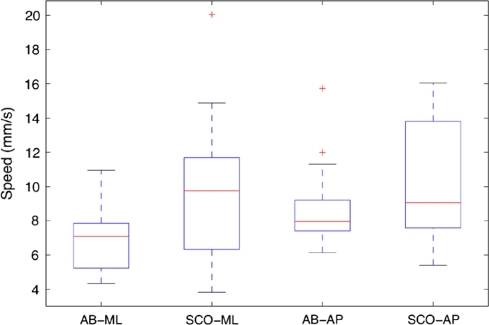
The values of AP and ML center of pressure range and speed are given in Figs. 3 and 4, respectively. Both the AP (P < 0.01) and ML (P = 0.02) COP ranges were significantly higher by 45 and 29% for the scoliotic group than those of the able-bodied girls. Similarly, the AP (P < 0.01) and ML (P < 0.01) COP speeds were higher by 16 and 29% for the scoliotic group.
Fig. 3.
Anteroposterior (AP) and mediolateral (ML) center of pressure range in able-bodied (AB) and scoliotic (SCO) girls
Fig. 4.
Anteroposterior (AP) and mediolateral (ML) center of pressure speed in able-bodied (AB) and scoliotic (SCO) girls
Table 1 presents the coefficient of correlation between the body and trunk center of mass anteroposterior (AP), mediolateral (ML) and resultant horizontal offsets and standing balance parameters. Generally, the coefficients of correlation were higher in the scoliotic group than in the able-bodied girls with the higher values obtained for the resultant offsets. None of the coefficients of correlation was statistically significant in the able-bodied group where their highest coefficient was 0.454. For the scoliotic girls, only the resultant offset was correlated with both the ML range (P = 0.01) and speed (P < 0.01). After adjusting for age, weight and height, the significant correlations shown in Table 1 remain statistically significant.
Table 1.
Coefficient of correlation between the body and trunk center of mass anteroposterior (AP), mediolateral (ML) and resultant horizontal offsets and standing balance parameters in able-bodied and scoliotic girls
| Able-bodied girls | Scoliotic girls | |||||
|---|---|---|---|---|---|---|
| AP offset | ML offset | Resultant offset | AP offset | ML offset | Resultant offset | |
| Range ML | 0.238 | 0.351 | 0.202 | 0.542 | 0.231 | 0.650* |
| Range AP | 0.295 | 0.128 | 0.297 | 0.237 | 0.294 | 0.279 |
| Speed ML | 0.306 | 0.454 | 0.261 | 0.589 | 0.180 | 0.657* |
| Speed AP | 0.348 | 0.432 | 0.258 | 0.340 | 0.132 | 0.418 |
* Denotes a statistically significant correlation where P < 0.05
Discussion
The first objective of this study was to test if the anteroposterior, mediolateral and resultant COM offsets were similar in able-bodied and scoliotic girls. Damavandi et al. [14] was the first to report body–head and trunk COM offsets in scoliotic girls and attributed the AP difference to a pelvic anterior tilt [23] and a backward trunk inclination [12, 24]. The smaller mean ML COM offset in scoliotic girls could reflect a compensatory action due to the spinal deformity leading to a backward COM shift to regain postural balance as suggested by Burwell et al. [25]. An important finding of this study is the lack of statistical difference in the resultant COM offset between the two groups. Though the head and trunk COM of the scoliotic and able-bodied girls are located, respectively, on either side of the whole body COM, their mean resultant distance from it are similar. It emerges that the trunk COM to body COM orientation plays a central role in trunk balance. This is clarified in part when examining the relation between the resultant COM offsets to the balance parameters.
Statistically significant correlations between the COM offsets and the balance parameters were observed in the scoliotic girls. It appears that a posterior displacement of the head and trunk COM increases balance instability. This was observed by Allard et al. [13] in a group of ectomorphic scoliotic girls who were characterized by a hypokyphotic trunk attitude. Dalleau et al. [26] further suggest that standing imbalance in scoliotic subjects is related to an asymmetric control of the trunk about the vertical axis. Though correlations were found when the COM offset increased posteriorly, it seems that balance parameters are unaffected when the head and trunk segment is displaced anteriorly as was reported in the able-bodied group.
The ML range and speed were both statistically correlated to the resultant COM offset in the scoliotic group indicating not only an increase in standing imbalance, but also in the neuromuscular demand. This is supported by Gauchard et al. [11] who reported that the spinal deformity has an effect on lateral standing instability. The relation between the resultant backward COM offset and larger ML instabilities could be due in part to rib–vertebra angle asymmetry in association with a short lordotic segment as suggested by Burwell et al. [25]. Thus, in an attempt to realign frontal plane balance, a backward shift of the head and trunk COM occurs causing an increase in the ML neuromuscular demand. As Engsberg et al. [10] noted, the position and orientation of major body segments such as the relation between body and trunk horizontal center of mass offset could play a more significant role in body bracing or in preoperative decisions. To our knowledge, the relation of the head and trunk COM, whole body COM or their offsets with standing balance parameters have not been used to assess frontal and sagittal plane overall postural and standing balance in AIS. Though our subjects did not require bracing or surgery at the time of this study, the results seem to indicate that standing imbalance increases with COM offset. Since this offset is due in part to the spinal deformity, it is reasonable to assume that trunk realignment could be one indicator to consider prior to body bracing or in surgical planning, and to assess the amount of correction provided by a body brace or spinal instrumentation.
In light of these results, we suggest that the COM offset could be calculated to estimate postural imbalance prior to body bracing or in surgical planning, and to assess the amount of correction provided by a body brace or spinal instrumentation. The difficulty lies in estimating the head and trunk COM position, since the horizontal body COM can be calculated from force plate data, namely the average COP position. A first approximation can be obtained by applying the head and trunk segment COM position to the mid-hip to C7 ratio given by Damavandi et al. [14] for non-treated scoliotic girls. Although the ratio represents an approximation, Damavandi et al. [14] reported no statistical difference between the use of mean ratio values and the corresponding and measured trunk segment COM values.
Conclusion
The head and trunk COM of the scoliotic and able-bodied girls was found to be located, respectively, on either side of the whole body COM, posteriorly for the scoliotic group, whereas their mean resultant COM offset were similar in length. The small mean ML COM offset in the scoliotic girls was attributed to a compensatory action due to spinal deformity in the frontal plane, resulting in a backward COM offset to regain postural balance. This was supported in part by a concomitant increase in the resultant backward COM offset distance and ML neuromuscular demand. We recommend the use of the COM offsets as a means of evaluating postural balance in non-treated scoliotic girls and assessing treatment efficacy.
Acknowledgments
The authors wish to express their gratitude to Mr. Totoch Tonnet-Naine for his technical assistance. This work was funded in part by the Natural Sciences and Engineering Research Council of Canada.
References
- 1.Damavandi M, Farahpour N, Allard P. Determination of body segment masses and centers of mass using a force plate method in individuals of different morphology. Med Eng Phys. 2009;31:1187–1194. doi: 10.1016/j.medengphy.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg CJ, Fogarty EE, Moore DP, Dowling FE. Scoliosis and developmental theory: adolescent idiopathic scoliosis. Spine. 1997;22:2228–2237. doi: 10.1097/00007632-199710010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg CJ, Kaliszer M, Moore DP, Fogarty EE, Dowling FE. Surface topography, Cobb angles, and cosmetic change in scoliosis. Spine. 2001;26:E55–E63. doi: 10.1097/00007632-200102150-00005. [DOI] [PubMed] [Google Scholar]
- 4.Stokes IA, Dansereau J, Moreland MS. Rib cage asymmetry in idiopathic scoliosis. J Orthop Res. 1989;7:599–606. doi: 10.1002/jor.1100070419. [DOI] [PubMed] [Google Scholar]
- 5.Sahlstrand T, Ortengen R, Nachemson A. Postural equilibrium in adolescent idiopathic scoliosis. Acta Orthop Scand. 1978;49:354–365. doi: 10.3109/17453677809050088. [DOI] [PubMed] [Google Scholar]
- 6.Byl NN, Gray JM. Complex balance reactions in different sensory conditions: adolescents with and without idiopathic scoliosis. J Orthop Res. 1993;11:215–227. doi: 10.1002/jor.1100110209. [DOI] [PubMed] [Google Scholar]
- 7.Goldie PA, Bach TM, Evans OM. Force platform measures for evaluating postural control: reliability and validity. Arch Phys Med Rehabil. 1989;70:510–517. [PubMed] [Google Scholar]
- 8.Hasan SS, Lichtenstein MJ, Shiavi RG. Effect of loss of balance on biomechanics platform measures of sway: influence of stance and a method for adjustment. J Biomech. 1990;23:783–789. doi: 10.1016/0021-9290(90)90025-X. [DOI] [PubMed] [Google Scholar]
- 9.Herman R, Mixon J, Fisher A, Maulucci R, Stuyck J. Idiopathic scoliosis and the central nervous system: a motor control problem. The Harrington lecture. Spine. 1985;10:1–14. doi: 10.1097/00007632-198501000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Engsberg JR, Lenke LG, Hollander KW, Uhrich ML, Commean PK, Lee JR, Bae KT. Methods to locate center of gravity in scoliosis. Spine. 2003;28:E483–E489. doi: 10.1097/01.BRS.0000099093.36335.16. [DOI] [PubMed] [Google Scholar]
- 11.Gauchard GC, Lascombes P, Kuhnast M, Perrin PP. Influence of different types of progressive idiopathic scoliosis on static and dynamic postural control. Spine. 2001;26:1052–1058. doi: 10.1097/00007632-200105010-00014. [DOI] [PubMed] [Google Scholar]
- 12.Nault ML, Allard P, Hinse S, Blanc RL, Caron O, Labelle H, Sadeghi H. Relationships between standing stability and body posture parameters in adolescent idiopathic scoliosis. Spine. 2002;27:1911–1917. doi: 10.1097/00007632-200209010-00018. [DOI] [PubMed] [Google Scholar]
- 13.Allard P, Chavet P, Barbier F, Gatto L, Labelle H, Sadeghi H. Effect of body morphology on standing balance in adolescent idiopathic scoliosis. Am J Phys Med Rehabil. 2004;83:689–697. doi: 10.1097/01.PHM.0000137344.95784.15. [DOI] [PubMed] [Google Scholar]
- 14.Damavandi M, Dalleau G, Stylianides G, Rivard C, Allard P (2010) Head and trunk mass and center of mass position estimations in able-bodied and scoliotic girls. Eur Spine J (submitted) [DOI] [PubMed]
- 15.Bunnel WP. The natural history of idiopathic scoliosis before skeletal maturity. Spine. 1986;11:773–776. doi: 10.1097/00007632-198610000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Carpenter MG, Frank JS, Winter DA, Peysar GW. Sampling duration effects on centre of pressure summary measures. Gait Posture. 2001;13:35–40. doi: 10.1016/S0966-6362(00)00093-X. [DOI] [PubMed] [Google Scholar]
- 17.Murray MP, Seireg A, Scholz RC. Center of gravity, center of pressure and supportive forces during human activities. J Appl Physiol. 1967;23:831–838. doi: 10.1152/jappl.1967.23.6.831. [DOI] [PubMed] [Google Scholar]
- 18.Zatsiorsky VM. Kinetics of Human Motion. Champaign: Human Kinetics; 2002. [Google Scholar]
- 19.McIlroy WE, Maki BE. Preferred placement of the feet during quiet stance: development of a standardized foot placement for the balancing test. Clin Biomech. 1997;12:66–70. doi: 10.1016/S0268-0033(96)00040-X. [DOI] [PubMed] [Google Scholar]
- 20.Allard P, Nault ML, Hinse S. Relationship between morphologic somatotypes and standing posture equilibrium. Ann Hum Biol. 2001;28:624–633. doi: 10.1080/03014460110047946. [DOI] [PubMed] [Google Scholar]
- 21.Simoneau M, Mercier P, Blouin J, Allard P, Teasdale N. Altered sensory-weighting mechanisms is observed in adolescents with idiopathic scoliosis. BMC Neurosci. 2006;7:68. doi: 10.1186/1471-2202-7-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maki BE, Holliday PJ, Topper AK. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol. 1994;49:M72–M84. doi: 10.1093/geronj/49.2.m72. [DOI] [PubMed] [Google Scholar]
- 23.Zabjek KF, Leroux MA, Coillard C, Rivard CH, Prince F. Evaluation of segmental postural characteristics during quiet standing in control and idiopathic scoliosis patients. Clin Biomech (Bristol, Avon) 2005;20:483–490. doi: 10.1016/j.clinbiomech.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Jackson RP, Peterson MD, McManus AC, Hales C. Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine. 1998;23:1750–1767. doi: 10.1097/00007632-199808150-00008. [DOI] [PubMed] [Google Scholar]
- 25.Burwell RG, Burwell RG, Cole AA, Cook TA, Grivas TB, Kiel AW, Moulton A, Thirlwall AS, Upadhyay SS, Webb JK, Wemyss-Holden SA. Pathogenesis of idiopathic scoliosis. The Nottingham concept. Acta Orthop Belg. 1992;58(Suppl 1):33–58. [PubMed] [Google Scholar]
- 26.Dalleau G, Allard MS, Beaulieu M, Rivard CH, Allard P. Free moment contribution to quiet standing in able-bodied and scoliotic girls. Eur Spine J. 2007;16:1593–1599. doi: 10.1007/s00586-007-0404-0. [DOI] [PMC free article] [PubMed] [Google Scholar]