Abstract
The objective of the study was to demonstrate the clinical characteristics of dural tears during percutaneous endoscopic lumbar discectomy (PELD) and to discuss how to prevent this unintended complication. The study used data from 816 consecutive patients who underwent PELD between 2003 and 2007. A total of nine patients (1.1%) experienced symptomatic dural tears. The clinical outcomes were evaluated using the visual analogue scale (VAS), the Oswestry disability index (ODI), and modified MacNab criteria. Intractable radicular pain was the most common symptom, while classical manifestations, such as CSF leakage or wound swelling, were rare. In three of the nine cases, the dural tears were detected intraoperatively, while the remaining six cases were not recognized during the procedure. Among the unrecognized patients, two patients were found with nerve root herniation causing profound neurological deficits. All patients were managed by secondary open repair surgeries. The mean follow-up period was 30.8 months. The mean VAS of radicular leg pain improved from 8.3 to 2.6, and that of back pain improved from 4.1 to 2.6. The mean ODI improved from 69.6 to 29.2%. The final outcomes were excellent in one, good in five, fair in one, and poor in two patients. As application of the endoscopic procedure has been broadened to more complex cases, the risk of dural tears may increase. Unrecognized dural tear with nerve root herniation may cause permanent neurological sequelae. Accurate information and proper technical considerations are essential to prevent this unpredictable complication.
Keywords: Dural tear, Endoscopic discectomy, Complication, Nerve root herniation
Introduction
Incidental dural tears during lumbar spine surgery have been reported in many clinical studies as one of the most important complications. The prevalence of unintended dural tears during lumbar disc surgery is variable, ranging from 1.8 to 17.4% [2, 3, 8, 10, 15–17, 19]. The clinical features and management protocol have also been described. Sometimes, the dural tears may cause long-term clinical sequelae and considerable medico-legal problems [4, 14].
Transforaminal percutaneous endoscopic lumbar discectomy (PELD) has been regarded as a safe, minimally invasive procedure for soft disc herniation. This novel procedure provides some benefits compared with open discectomy such as no need for bone or facet resection, less damage to muscular and ligamentous structures, shorter hospital stay and earlier return to function [6, 9, 11, 12]. Theoretically, the risk of dural sac retraction and subsequent dural tears may be relatively lower in PELD. Compared with the open posterior interlaminar approach, the posterolateral transforaminal approach enables access to the herniated fragment without dural sac retraction.
To date, the incidence and clinical effect of dural tears associated with PELD have been unclear or underestimated [20]. In our study, although the procedures were performed with no technical difficulty during their approach and the discectomy step, unintended symptomatic dural tears occurred. The clinical manifestation, natural course, and neurologic sequelae of dural tears associated with this procedure were different from those of open lumbar surgery. To our knowledge, there has been no previous clinical study about incidental dural tears during PELD.
Therefore, the purpose of this study was to present the clinical characteristics of dural tears during PELD and to discuss proper management strategies for this underestimated complication.
Materials and methods
Data collection
We examined our database to detect all patients who had undergone PELD at our hospital from January 2003 to December 2007. A total of 816 consecutive cases were treated with PELD by the authors (YA, SHL, and JHL). Radicular leg pain was present in all patients, and soft lumbar disc herniation was demonstrated on both computed tomography scan and magnetic resonance imaging (MRI) correlated to the clinical manifestations. Patients with segmental instability, bony stenosis, calcified disc herniation, or painless weakness were not candidates for the procedure. The medical records of the patients were retrospectively reviewed. Among the consecutive 816 cases, 9 cases of symptomatic dural tears associated with transforaminal PELD were found. In all patients, the dural tears were confirmed by secondary open surgeries. The clinical outcomes were evaluated using the visual analogue scale (VAS) for pain intensity and the Oswestry disability index (ODI) for the functional status. The clinical outcomes were also classified into excellent, good, fair, or poor, based on modified MacNab criteria.
Surgical procedure
The standard PELD was performed under local anaesthesia as previously described [1, 20]. The patient was placed prone on the radiolucent table, and was kept conscious during the procedure to enable the important monitoring of any changes in the symptoms and signs. A fluoroscopic-guided posterolateral transforaminal approach through the foraminal window was performed. After a safe transforaminal approach, an ellipsoidal working channel endoscope (Wolf, Tuttlingen, Germany) was inserted. Herniated fragments were removed selectively using endoscopic forceps and side-firing Holmium-YAG laser under endoscopic vision. Finally, anatomical details of the epidural and foraminal area, including the decompressed nerve root and dural sac, were confirmed.
Results
Demographics and types of dural tear
Nine (1.1%) of the 816 patients experienced symptomatic dural tears associated with PELD. There were five women and four men, with a mean age of 47.3 years (range 18–70 years). In three of the nine patients, the dural tears were detected intraoperatively, and the patients had subsequent open surgery for primary repair (recognized type, Fig. 1). Three patients of the recognized type complained of headache with back pain as the CSF leakage happened. The remaining six had delayed diagnosis of symptomatic dural tears after a symptom-free interval (unrecognized type, Figs. 2, 3).
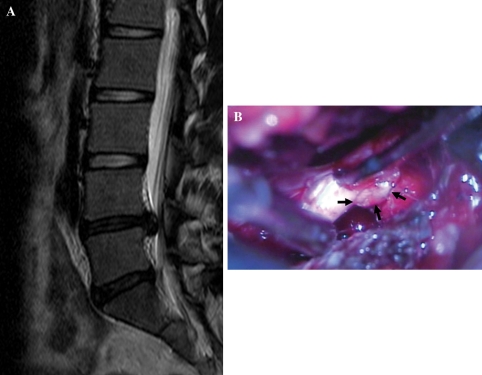
Fig. 1.
Case illustration of recognized dural tear (case No. 9). An 18-year-old female patient underwent transforaminal percutaneous endoscopic lumbar discectomy (PELD) for right-sided disc herniation at the L4-5 level (a). A dural tear and nerve root exposure were detected intraoperatively. The procedure was stopped and open repair was performed. On the operative finding, the nerve root was popped out (arrows) and entrapped though the dural defect (b)
Fig. 2.
Case illustration of unrecognized, nerve root herniation (case No. 1). A 64-year-old male patient underwent transforaminal percutaneous endoscopic lumbar discectomy (PELD) for right-sided disc herniation at the L4-5 level (a). Four hours later, sudden recurrent leg pain and progressive motor weakness developed. Postoperative MRI showed transdural nerve root herniation into the disc space (b)
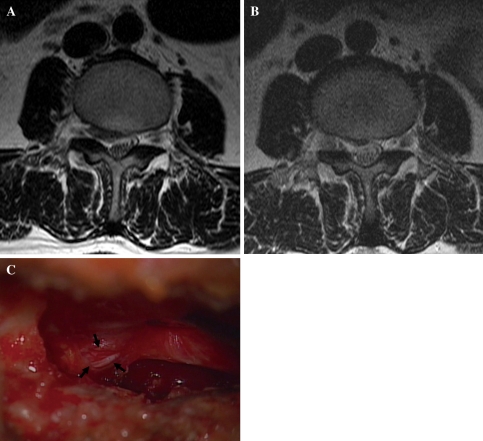
Fig. 3.
Case illustration of unrecognized, nerve root irritation (case No. 5). A 44-year-old female patient underwent transforaminal percutaneous endoscopic lumbar discectomy (PELD) for right-sided disc herniation at the L3–4 level (a). After the procedure, the patient’s pain was relieved, and the postoperative MRI showed a well-decompressed dural sac (b). Seven days later, however, the patient’s leg pain reoccurred and progressed gradually. Open exploration was performed. There was no evidence of recurrent disc herniation. Instead, a small dural defect was found on the operative field. A nerve root was exposed through the dural defect (arrows) and irritated by the surrounding tissues (c)
The average time for clinical manifestation of the unrecognized type was 2.5 days (range 0–7 days). When the unrecognized-type patients presented with aggravation of their symptoms, an MRI was performed to find out the cause of the pain or weakness. The MRI showed no definite disc reherniation or mechanical compression. Rather, there may have been findings of secondary effects of dural tears, such as nerve root entrapment or CSF collection in the disc space. The typical clinical manifestation was intractable leg pain with or without neurological deficit. The leg pain was severe, electric shock-like in nature, aggravated by spinal motion, and unresponsive to any conservative managements, including physical therapy, medication, and epidural injection therapy. Definite diagnosis and treatment of the dural tears were achieved through subsequent open explorations in all patients.
According to the nerve root involvement, the unrecognized cases could be classified into two categories: nerve root herniation, in which the nerve root popped out through the dural defect (Fig. 2), and nerve root irritation, in which the nerve root was exposed and irritated but not herniated out of the dural membrane (Fig. 3). Two of the six unrecognized patients were categorized as having nerve root herniation. The remaining four unrecognized patients were categorized as having nerve root irritation. The patients with nerve root herniation presented with leg pain and neurological deficit, and the herniation was detected by MRI. In contrast, the patients with nerve root irritation presented with intractable leg pain without neurological deficit, which was difficult to detect by imaging studies.
Regardless of the type of dural defect, all patients underwent open repair surgery with a standard microscope-assisted interlaminar approach. One patient with an unrecognized dural tear with nerve root herniation had to have subsequent fusion surgery at the same level. In the open exploration, herniated nerve root in the disc space with CSF leakage could be observed in all of the nerve root herniation cases. In contrast, there was no definite CSF leakage in the nerve root irritation cases. Primary suturing was possible in only two cases in which the dural tears occurred on the ventro-lateral side of the dural sac. In the other cases, watertight-primary suturing was not possible because most dural defects were located on the ventral side of the dural sac at the paramedian zone. Therefore, various shielding materials, such as cadaveric dura, fibrin glue, and Tachocomb® (Nycomed Austria GmbH, Linz, Austria) were used to reinforce the dural repair. The demographic findings are summarized in Table 1.
Table 1.
Demographic and clinical features of dural tears (DTs) in percutaneous endoscopic lumbar discectomy (PELD)
| Case No. | Sex/age | Levels | Recognition | Nerve root statusa | Site of DTs | Time to recognition | Symptom | Neurologic deficit | Treatment (time interval) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M/64 | L4–5 | Unrecognized | Herniated | Ventral | 4 h | Leg pain | Foot drop | Open repair (1 day) |
| 2 | F/38 | L4–5 | Recognized | Ventral | Intraop | Back pain/headache | Ankle weak (recovered) | Open repair (0 day) | |
| 3 | M/40 | L3–4 | Unrecognized | Irritated | Ventral | 3 days | Leg pain | – | Open repair (2 weeks) |
| 4 | F/54 | L3–4 | Recognized | Ventral | Intraop | Back pain/headache | Ankle weak (recovered) | Open repair (0 day) | |
| 5 | F/44 | L3–4 | Unrecognized | Irritated | Ventro-lateral | 7 days | Leg pain | – | Open repair (3 months) |
| 6 | M/41 | L3–4 | Unrecognized | Irritated | Ventro-lateral | 3 days | Leg pain | – | Open repair (3 weeks) |
| 7 | M/70 | L4–5 | Unrecognized | Herniated | Ventral | 1 day | Leg pain | Ankle weak | Open repair (1 day) (later fusion) |
| 8 | F/57 | L4–5 | Unrecognized | Irritated | Ventral | 1 day | Leg pain | – | Open repair (1 day) |
| 9 | F/18 | L4–5 | Recognized | Ventral | Intraop | Headache/voiding sense | – | Open repair (0 day) |
aIn the unrecognized cases
Clinical outcomes
The mean follow-up period was 30.8 months (range 18–44 months). The mean VAS of radicular leg pain improved from 8.3 (SD 0.9) to 2.6 (SD 1.3) and that of back pain improved from 4.1 (SD 1.4) to 2.6 (SD 0.9). The mean ODI improved from 69.6% (SD 11.9%) to 29.2% (SD 17.2%). Based on modified MacNab criteria, the final outcome was found to be excellent in one patient, good in five patients, fair in one patient, and poor in two patients. Both patients of the unrecognized, nerve root herniation type rated poor outcomes (Table 2).
Table 2.
Clinical outcome of second treatment for dural tears (DTs) associated with percutaneous endoscopic lumbar discectomy (PELD)
| Case No. | VAS_leg | VAS_back | Oswestry disability index | McNab criteria | Follow-up (months) | |||
|---|---|---|---|---|---|---|---|---|
| Preop | Postop | Preop | Postop | Preop | Postop | |||
| 1 | 8 | 2 | 5 | 3 | 34/50 (68%) | 28/50 (56%) | Poor | 31 |
| 2 | 8 | 3 | 6 | 2 | 39/50 (78%) | 15/50 (30%) | Good | 44 |
| 3 | 7 | 4 | 5 | 3 | 19/45 (42.2%) | 8/45 (17.8%) | Fair | 42 |
| 4 | 8 | 2 | 3 | 2 | 31/50 (62%) | 9/50 (18%) | Good | 34 |
| 5 | 9 | 3 | 3 | 2 | 36/45 (80%) | 14/50 (28%) | Good | 30 |
| 6 | 8 | 2 | 3 | 3 | 31/45 (68.9%) | 10/45 (22.2%) | Good | 29 |
| 7 | 9 | 5 | 3 | 4 | 39/50 (78%) | 27/45 (60%) | Poor | 25 |
| 8 | 8 | 1 | 6 | 3 | 32/45 (71.1%) | 8/45 (17.8%) | Good | 24 |
| 9 | 10 | 1 | 3 | 1 | 35/45 (77.8%) | 6/45 (13.3%) | Excellent | 18 |
Discussion
The iatrogenic dural tear is a well-known complication in open lumbar spinal surgery. In contrast, reports of dural tears during the percutaneous spinal procedure have been very rare [5, 20]. Transforaminal endoscopic discectomy has been evolved from the indirect central decompression level to the direct selective fragmentectomy level. As the procedure becomes more direct and selective, the incidence of trauma to the dural membrane may increase. However, the risk of this complication has been underestimated. Most dural tears occur during the selective discectomy step. The predisposing conditions include fibrotic adhesion, eroded dura, or redundant dura in patients with large disc herniation [2]. A more aggressive challenge by mechanical tools to remove the migrated disc herniation may also cause direct dural trauma.
Types of dural tears according to the recognition and nerve root status
In the recognized cases, the dural damage was detected during the procedure. In three of the nine patients, the dural tears were diagnosed by seeing the exposed nerve root and by typical clinical signs. Once a dural tear occurs, patients usually feel back pain or leg numbness. Sometimes the patients may feel the urge to urinate. It is usually accompanied by headache or neck stiffness as CSF leakage started. In our series, the intraoperative attempt to repair the defect by shielding materials under the endoscopic visualization was ineffective. The proper management option was immediate open conversion and direct repair under microscopic visualization. After the secondary open surgery, the patients with the recognized type showed excellent outcomes without any neurological sequelae.
However, in the unrecognized cases, the clinical courses were more complex. It is inherently difficult to detect a dural laceration during the procedure, unlike in open surgery. The operation field is usually filled with irrigation solution. Therefore, a small amount of CSF leakage due to minor dural tears cannot be easily detected. Moreover, the positive pressure of the irrigation fluid may prevent the rootlets from being exposed or popping out during the procedure. An unrecognized small dural tear may not cause any neurological symptoms during the procedure or in the immediate postoperative period. However, this is the most dangerous situation. As time passes, delayed widening of the dural opening due to the increased intraspinal pressure may cause significant neural entrapment syndrome. In general, the cardinal signs of dural tears associated with open surgery are wound swelling, headache, or dizziness caused by CSF leakage [10]. However, they are not typical in the PELD-associated unrecognized dural tear, because there is not enough space for collection of the CSF created by the PELD procedure. Rather, the typical symptom is relapse of intractable radicular pain. The pain nature may be either dermatomal or non-dermatomal, and electric shock-like in nature, depending on the location of the dural tear. The pain is frequently aggravated by walking or position change. The pain may be accompanied by various neurological deficits. It is determined by the status of the nerve root involvement. If the nerve root is just exposed through small dural defect but not herniated, there is no neurologic deficit showing only radicular pain. In contrast, the nerve root herniation type in which the nerve fibres pop out beyond the border of dural membrane may cause significant neurological deficit. There have been some reports of nerve root herniation after lumbar disc surgery or procedures [5, 13, 18]. However, there have been no reports of the event after percutaneous discectomy. The clinical outcome of the unrecognized nerve root herniation type may be unfavourable, causing cauda equina syndrome or permanent motor weakness. Two patients who experienced unrecognized nerve root herniation had considerable pain and motor weakness, even after the revision surgery.
Radiological findings
There are some imaging findings suggesting a dural defect or neural entrapment after PELD. The secondary effects of the dural tear, such as nerve root herniation, CSF collection in the disc space, or pseudomeningocele, could be detected by MRI. However, in some cases, a small dural tear with nerve root irritation may not be detected by imaging studies. Therefore, proper acknowledgement of the clinical characteristics is important to diagnose the dural tears. If there is no evidence of nerve root compression by recurrent disc herniation or infection on imaging studies, nerve root irritation or herniation secondary to the incidental dural tear should be included in the differential diagnosis of recurrent symptoms after PELD. Of the six unrecognized cases, two cases with nerve root herniation type, the herniated rootlets into the disc space, were observed in the postoperative MRI. The other four cases were diagnosed by clinical manifestations or operative findings rather than imaging findings. We think that if the practitioner does not keep in mind the possibility of this complication, the findings suggesting dural tears in PELD could be overlooked in imaging studies.
Management and preventive strategies
Incidental durotomy may bring about long-term clinical sequelae [14]. In our series, the unrecognized nerve root herniation type showed an unfavourable outcome with neurologic sequelae. Therefore, a proper management strategy is important. The best way to treat this complication is prevention. We focused on the preventive strategies of this unexpected complication during PELD. First, we think that the risk of dural tears may be higher in cases of migrated or large central disc herniation, since the chance of dural adhesion or the need of dural manipulation is greater in those cases. Second, a surgeon’s aggressive actions to expose the neural tissues for thorough decompression may be harmful to the dural membrane. Especially, instrumental manipulation of the narrow, invisible epidural space should be avoided. Actually, most dural tears occurred during removal of extruded disc fragment, which was adherent to the dural sac or behind the bony structures, using endoscopic disc forceps. Finally, the surgeon should try to preserve the intact annulus as much as possible, to offer a tamponade effect preventing nerve root herniation or entrapment. The basic concept of the current endoscopic discectomy technique is a selective target removal of herniated disc fragment to preserve surrounding anatomical structures.
Regardless of the surgeon’s best effort, unexpected dural tears may develop. However, if an early diagnosis and proper management are performed, long-term sequelae may be preventable [8, 19]. Once a significant nerve root herniation occurs before recognition, a permanent neurological deficit may be brought about. Diagnosis of an unexpected dural tear can be made by typical clinical features and imaging studies. In case of suspicion, early postoperative MRI should be checked and the patient should be closely observed for at least 24 h. Most dural tears can be effectively controlled by open repair using dural stitches and shielding materials [7].
The occurrence of dural tears in PELD may be closely related to the technical evolution. In the early era of the percutaneous procedure, the main concept was indirect decompression, and the occurrence of dural tears was negligible. However, the concept of current percutaneous endoscopic surgery has evolved to selective fragmentectomy and direct neural decompression. Therefore, the risk of dural tears may become a considerable complication of PELD. In our experience, most dural tears occurred when the surgeon pursued more definite decompression and clearer visualization of the decompressed neural tissues. As the surgeon becomes overconfident in his technique and the application of PELD is broadened to cases of greater complexity, the risk of dural tears may increase.
Conclusion
Although PELD is a minimally invasive and relatively safe procedure, surgeons should bear in mind the possibility of dural tear during the procedure. Its clinical manifestations may be different from those in open surgery. The unrecognized nerve root herniation type of dural tear may cause considerable neurologic deficit. To prevent the unintended dural tears in PELD, accurate information and proper technical considerations are essential.
References
- 1.Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine. 2004;29:E326. doi: 10.1097/01.BRS.0000134591.32462.98. [DOI] [PubMed] [Google Scholar]
- 2.Bosacco SJ, Gardner MJ, Guille JT. Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin Orthop Relat Res. 2001;389:238–247. doi: 10.1097/00003086-200108000-00033. [DOI] [PubMed] [Google Scholar]
- 3.Cammisa FP, Jr, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine. 2000;25:2663–2667. doi: 10.1097/00007632-200010150-00019. [DOI] [PubMed] [Google Scholar]
- 4.Goodkin R, Laska LL. Unintended “incidental” durotomy during surgery of the lumbar spine: medicolegal implications. Surg Neurol. 1995;43:4–12. doi: 10.1016/0090-3019(95)80031-B. [DOI] [PubMed] [Google Scholar]
- 5.Hasegawa K, Yamamoto N. Nerve root herniation secondary to lumbar puncture in the patient with lumbar canal stenosis. A case report. Spine. 1999;24:915–917. doi: 10.1097/00007632-199905010-00015. [DOI] [PubMed] [Google Scholar]
- 6.Hermantin FU, Peters T, Quartararo L, Kambin P. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am. 1999;81:958–965. doi: 10.2106/00004623-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Hodges SD, Humphreys SC, Eck JC, Covington LA. Management of incidental durotomy without mandatory bed rest. A retrospective review of 20 cases. Spine. 1999;24:2062–2064. doi: 10.1097/00007632-199910010-00017. [DOI] [PubMed] [Google Scholar]
- 8.Jones AA, Stambough JL, Balderston RA, Rothman RH, Booth RE., Jr Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine. 1989;14:443–446. doi: 10.1097/00007632-198904000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Kambin P, Brager MD. Percutaneous posterolateral discectomy. Anatomy and mechanism. Clin Orthop Relat Res. 1987;223:145–154. [PubMed] [Google Scholar]
- 10.Khan MH, Rihn J, Steele G, Davis R, Donaldson WF, 3rd, Kang JD, Lee JY. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: a review of 3,183 consecutive degenerative lumbar cases. Spine. 2006;31:2609–2613. doi: 10.1097/01.brs.0000241066.55849.41. [DOI] [PubMed] [Google Scholar]
- 11.Knight M, Goswami A. Management of isthmic spondylolisthesis with posterolateral endoscopic foraminal decompression. Spine. 2003;28:573–581. doi: 10.1097/00007632-200303150-00012. [DOI] [PubMed] [Google Scholar]
- 12.Maroon JC. Current concepts in minimally invasive discectomy. Neurosurgery. 2002;51:S137–S145. doi: 10.1097/00006123-200211002-00019. [DOI] [PubMed] [Google Scholar]
- 13.Nishi S, Hashimoto N, Takagi Y, Tsukahara T. Herniation and entrapment of a nerve root secondary to an unrepaired small dural laceration at lumbar hemilaminectomies. Spine. 1995;20:2576–2579. doi: 10.1097/00007632-199512000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Saxler G, Krämer J, Barden B, Kurt A, Pförtner J, Bernsmann K. The long-term clinical sequelae of incidental durotomy in lumbar disc surgery. Spine. 2005;30:2298–2302. doi: 10.1097/01.brs.0000182131.44670.f7. [DOI] [PubMed] [Google Scholar]
- 15.Sin AH, Caldito G, Smith D, Rashidi M, Willis B, Nanda A. Predictive factors for dural tear and cerebrospinal fluid leakage in patients undergoing lumbar surgery. J Neurosurg Spine. 2006;5:224–227. doi: 10.3171/spi.2006.5.3.224. [DOI] [PubMed] [Google Scholar]
- 16.Stolke D, Sollmann WP, Seifert V. Intra- and postoperative complications in lumbar disc surgery. Spine. 1989;14:56–59. doi: 10.1097/00007632-198901000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Tafazal SI, Sell PJ. Incidental durotomy in lumbar spine surgery: incidence and management. Eur Spine J. 2005;14:287–290. doi: 10.1007/s00586-004-0821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Töppich HG, Feldmann H, Sandvoss G, Meyer F. Intervertebral space nerve root entrapment after lumbar disc surgery. two cases. Spine. 1994;19:249–250. doi: 10.1097/00007632-199401001-00021. [DOI] [PubMed] [Google Scholar]
- 19.Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty-eight patients. J Bone Joint Surg Am. 1998;80:1728–1732. doi: 10.1302/0301-620X.80B6.8966. [DOI] [PubMed] [Google Scholar]
- 20.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002;27:722–731. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]