ABSTRACT
Approximately 2400 years ago, Hippocrates performed the first phlebotomy to treat a varix. Since that time, modifications to the removal of varicose vein have evolved. It was Dr. Muller, a Swiss dermatologist, who reinvented and refined the technique of ambulatory phlebectomy. Although this technique was adopted slowly, it is now considered the standard method for treating varicose veins. The procedure is performed on an ambulatory patient under local anesthesia with little, if any, recovery time. After approximately a 2-mm puncture or incision made by an 18-gauge needle or a 15-degree ophthalmic blade, a small hook-like instrument coupled with fine clamps is employed to extract the varix. A dry sterile compression dressing and or class 2 stocking is applied. Significant complications are rare.
Keywords: Varicose vein, phlebectomy, stab avulsion, vein treatment
INTRODUCTION AND DEFINITION
In 400 years BC, Hippocrates was the first to conceptualize phlebotomy. Several sequential punctures in the vein would be used to get rid of the “bad blood” that fed an ulcer. It appears that Aulus Cornelius Celsus (56 BC to AD 40) was the first surgeon actually to perform a phlebectomy. According to historians who researched and wrote the history of ambulatory phlebectomy, most of Celsus' writings disappeared or were destroyed; however, some of the documents that were discovered attributed and described Celsus' venous contributions. Concerning phlebectomy, Celsus wrote: “The varicose veins were treated by exposure followed by avulsion with a blunt hook or by the touch of the cautery.”1 He made large incisions and used compressive bandages that allowed ambulation. It was Robert Muller, a dermatology-trained phlebologist from Neuchâtel, Switzerland, who reinvented and refined the technique that we now know as ambulatory phlebectomy. Disappointed by his results with large vein sclerotherapy, Muller began using small hooks (made from broken hemostats) to remove varicosities through small holes. By 1956, he had perfected this treatment, which he presented in 1967 to the French Society of Phlebology and in 1968 to the International Congress of Phlebology. These presentations were poorly received by most of the audience. However, some physicians visited Muller to learn his treatment method, which then spread slowly throughout the world. Not until recently was ambulatory phlebectomy adopted in the United States as the “gold standard” to remove segments of varicose or reticular veins of any size. Ambulatory phlebectomy, stab avulsion, microphlebectomy, and microextraction are synonymous terms that define this local-anesthetic, ambulatory, outpatient technique.
INDICATIONS FOR AMBULATORY PHLEBECTOMY
Asymptomatic varicose and reticular veins
Symptomatic varicose and reticular veins
Complications of varicose veins
CONTRADICTIONS
Infectious dermatitis, cellulitis in surrounding areas
Severe peripheral edema
Seriously ill patients
Anticoagulated patients—warfarin (Coumadin), etc.
Hypercoagulable states
TECHNIQUE-PREOPERATIVE MARKINGS
All varicose veins should be marked preoperatively while the patient is standing as they may be difficult or impossible to identify during recumbency. Surgical or permanent markers should be used to avoid their being washed away during site preparation. Warning: if subsequent incisions are placed directly though the ink used to outline veins preoperatively, permanent tattoos may result in and around the incision.
SURGICAL PLAN
The timing of ambulatory phlebectomy depends upon the nature and type of other venous procedures being performed. When ambulatory phlebectomy is coupled with intervention upon the great or small saphenous veins (endovenous thermal ablation or ligation and stripping), phlebectomy below the knee should be performed first. There is a transient increase in endoluminal pressure in caudal veins during saphenous treatment, which could result in bleeding if ambulatory phlebectomy was performed subsequently. The author often stages his procedures, treating the great or small saphenous vein first, followed several weeks later by ambulatory phlebectomy. This method allows the existing truncal varicosities to decrease in size prior to further procedures and sometimes disappear altogether.2
ANESTHESIA
The author utilizes 50–100 mL of 0.5% lidocaine with 1:200,000 epinephrine and 5 mL of sodium bicarbonate (a pH buffer) to provide local anesthesia. The mixture is infused through a 25-gauge, 1.5-inch-long needle. Other concentrations of local anesthetic have been used.
PROCEDURAL EQUIPMENT
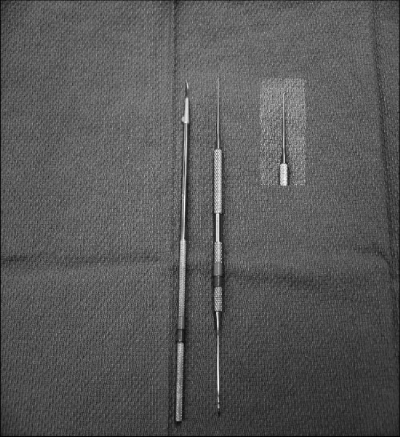
Incisions or punctures can be made with various devices, including hypodermic needles and knife blades. The most common instruments are an 18-gauge cutting needle, a no. 11 blade, and a 15-degree ophthalmologic Alcon blade (the author's preference). The no. 11 blade, anecdotally, causes greater scarring. After phlebectomy is completed, ½-inch Steri-Strips are utilized to close these punctures.
Several different hooks are available for purchase, varying by size, shape, and sharpness of the hook. The most widely known hooks are Muller, Oesch, Tretbar, Ramelet, Verady, and Dortu-Mortimbeau hooks.3 It is important for the proceduralist to be comfortable with a particular set of hooks, and he or she should make a selection after trying the gamut.
The clamps used for vein extraction should have a fine tip so that they can grip close to the skin. A serrated face is helpful in maintaining firm traction without slippage. The operator should have at least three clamps available, but five or more are preferable (Fig. 1).
Figure 1.
Tray set up: local anesthesia, 15-degree ophthalmologic Alcon blade, phlebectomy hook and spatula, no. 1 Muller hook, clamps, scissor, Steri-Strips, and gauze.
PROCEDURE
After the anesthetic has been injected into the perivenous tissues, a microincision or puncture is made near the vein. Most are oriented vertically, except around the knee, where they should be oriented along tension lines (Langer's lines). A blunt-tip spatula may be inserted into the opening, although this is not mandatory (Fig. 2). It does, however, enable a hook to be inserted without interference from surrounding tissues and without enlarging the entrance hole. (Fig. 3) Once the hook has been inserted, the vein is grasped blindly and brought up and out of the opening (Fig. 4). The vein is then grasped between clamps and transected by a small scissors (Figs. 5 and 6). Using gentle traction on the hemostat in a “windshield wiper movement,” one end of the varix is teased out of the puncture site. Successive hemostats are applied to the varix as it is extracted from its position, keeping in mind that the vein will eventually tear (Fig. 7). Very long segments can often be removed through a single puncture site. Once a segment has been extracted, the operator moves along the vein by a roughly equivalent distance, makes another incision, and the process is repeated.
Figure 2.
15-degree ophthalmologic blade and handle, and phlebectomy hook and spatula. Inset: Muller-type hook.
Figure 3.
Spatula insertion through skin opening.
Figure 4.
Hooked vein.
Figure 5.
Loop of vein teased out of puncture site.
Figure 6.
Vein loop cut with small scissors.
Figure 7.
Vein extraction with clamps.
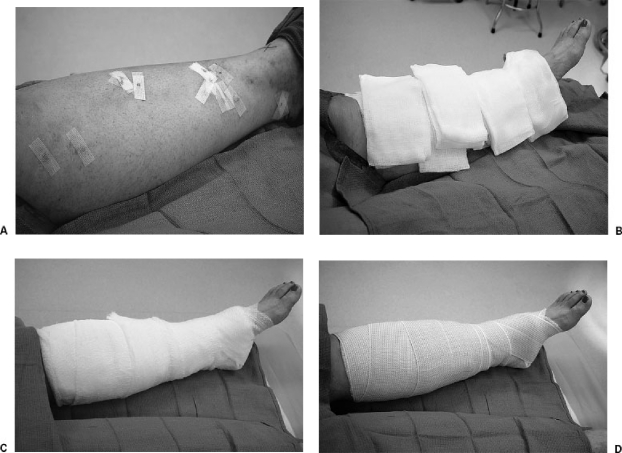
The operator is encouraged to attempt to remove all parts of the varix (without leaving isolated segments behind) to reduce the possible inflammatory response from thrombosis of the retained segment. However, as long as most of the segment is removed, the patient should have an excellent result. There is rarely cause to ligate a vessel, except when a perforator, peripheral foot or hand vessel, or a large varix (> 1 cm) is exposed. Perforating veins are recognized as a branch in the vein, often with an orientation perpendicular to the skin, and associated with a deep pulling sensation by the patient. The puncture sites are covered with Steri-Strips, sterile 4 × 4 dressings, and wrapped with a soft gauze roll and Ace bandages (Fig. 8A–D).
Figure 8.
Placement of (A) Steri-Strips over vein extraction sites, (B) sterile gauze, (C) sterile soft gauze wrap, and (D) stretch bandage.
DISCHARGE RECOMMENDATIONS
The patient can be safely discharged from the facility after ambulating.
Provide a prescription for oxycodone-acetaminophen (Percocet) with instructions to try acetaminophen initially (most patients take only acetaminophen).
Instruct patient to return to office the following day for bandage removal and placement of class 2 compression hose.
Have patient wear compression hose (class 2, 30–40 mm) for at least 2 weeks.
Instruct patient to return to activities of daily living, with no heavy aerobic exercise that would involve the lower extremities for 2 weeks.
Leave Steri-Strips in place for 2 weeks.
Follow up in 2 weeks, 8 weeks, 6 months, and 1 year.
COMPLICATIONS OF AMBULATORY PHLEBECTOMY
Complications arising from ambulatory phlebectomy are quite rare but do exist. The following list is compiled from several physicians: Jose Olivencia, Robert Muller, Stefeno Ricci, and Lowell Kabnick.1,2,4,5
Anesthetic Complications
Technique related—placement of injection
Allergic reaction—preservative, lidocaine
Emotionally labile patient
Skin Complications
Blister
Keloid formation
Dimpling
Infection
Induration
Hypo- or hyperpigmentation (incision)
Tattooing
Pigmentation, transitory or permanent
Compression Bandage Complications
Swelling
Blisters
Ischemia
Skin necrosis
Contact dermatitis
Vascular Complications
Bleeding, seroma
Superficial thrombosis
Deep venous thrombosis
Pulmonary embolism
Telangiectasias
Matting
Lymphatic Complications
Lymphorrhea
Persisting edema
Lymphocele
Neurological Complications
Nerve damage—saphenous, sural, peroneal, etc. nerves
Temporary hypoesthesia
Dysesthesia (temporary or permanent)
Traumatic neuroma
REFERENCES
- Ricci S. Ambulatory Phlebectomy. St. Louis: Mosby; 1995.
- Kabnick L. Should we consider a paradigm shift for the treatment of GSV and branch varicosities? San Diego: Abstract at the 2003 UIP World Congress Phlebology Chapter Meeting; August 2003.
- Dortu J, Raymond-Martimbeau P. Ambulatory Phlebectomy. Houston: PMR Editions; 1993.
- Olivencia J A. Complications of ambulatory phlebectomy: review of 1,000 consecutive cases. Dermatol Surg. 1997;23:51–54. [PubMed] [Google Scholar]
- Olivencia J A. Ambulatory phlebectomy turned 2400 years old. Dermatol Surg. 2004;30:704–708. doi: 10.1111/j.1524-4725.2004.30210.x. [DOI] [PubMed] [Google Scholar]