ABSTRACT
The transjugular intrahepatic portosystemic shunt (TIPS) is one of the most complex procedures performed by interventional radiologists. Most of these procedures are straightforward and may be successfully completed within 2 hours. In some cases, TIPS creation may be extremely difficult, for example in situations such as: variant anatomy, portal vein thrombosis, hepatic vein thrombosis, or preexisting TIPS. In this article we describe some maneuvers that may be attempted in cases where creation of the shunt proves to be difficult.
Keywords: Transjugular intrahepatic portosystemic shunts, portal hypertension, portal vein thrombosis, hepatic vein thrombosis
The transjugular intrahepatic portosystemic shunt (TIPS) procedure was first performed in a human in Germany in 1988.1 During its first stages, the procedure was found to be complex and technically difficult, and as a matter of fact, it was not unusual to observe an interventional radiologist struggle through a TIPS procedure for 6 or 7 hours before the shunt was successfully created. The most challenging step of the procedure is to gain access into the portal vein and so, from the technical standpoint, the interventional radiologists performing TIPS have focused on trying to make it easier to localize and enter the portal vein.2 Several techniques have been described to make it easier to identify a suitable portal vein branch during a TIPS procedure including: placing an angiographic catheter, small wire, or retrieval basket within the portal vein; placing a catheter into the left portal vein through a patent paraumbilical vein; marking the hepatic artery with a microcatheter; performing the procedure with the assistance of ultrasound guidance, magnetic resonance imaging, indirect contrast portography, wedge CO2 portography, and, recently, using intravascular ultrasound to localize the portal vein.3,4,5,6,7,8,9 Interventional radiologists should be able to successfully complete a TIPS procedure in over 95% of the cases with less than 5% complication rate.10 The noncomplicated TIPS procedure should be completed within 60 to 90 minutes; however, in some cases, the procedure is not so easy and the interventional radiologist needs to use additional “tricks” or maneuvers to be able to successfully complete the creation of the shunt. The purpose of this review is to illustrate some technically difficult TIPS procedures where unusual maneuvers or approaches were employed to successfully create the shunt. The authors will emphasize on special precautions required with these “unusual” maneuvers.
PROBLEM: LACK OF HEPATIC VEINS; SOLUTION: TRANSPARENCHYMAL PUNCTURE
Patients with Budd-Chiari syndrome may have total occlusion of the hepatic veins and present only a small stump and classic “spiderweb” appearance (Fig. 1). Axial imaging in these patients usually demonstrates an enlarged liver, large caudate lobe, patent portal vein, and absence of hepatic veins (Fig. 2). Performing a TIPS in these patients represents a technical challenge because a suitable hepatic vein cannot be catheterized for the placement of the transjugular access system. In these cases, we recommend starting the TIPS procedure with a left internal jugular vein approach.11,12,13 It appears that the use of the left internal jugular vein provides a more favorable angle in patients who do not have patent right or middle hepatic veins. The transjugular access system is then carefully embedded within the liver parenchyma using moderate amount of forward pressure to anchor the needle system within the liver parenchyma. The small hepatic vein stump is used as an anchoring structure (Fig. 3). A small amount of contrast may be injected to confirm good position of the needle system within the liver parenchyma (Fig. 3). At this point, a CO2 portogram can be performed through the transjugular access needle to localize the portal vein (Fig. 4). Once the portal vein is localized, the needle is torqued in the correct orientation and the transhepatic punctures may be performed in the usual fashion for the creation of the shunt. The remainder of the procedure proceeds in the usual fashion and the TIPS can be completed successfully (Fig. 5).
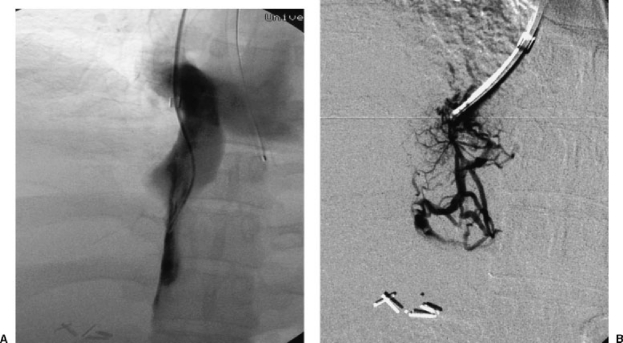
Figure 1.
(A) Cavagram in a patient with Budd-Chiari demonstrates only a small hepatic vein stump but no reflux of contrast into the right hepatic vein. (B) Direct parenchymal injection in the same patient demonstrates the classic “spiderweb” appearance, classic for complete hepatic vein occlusion in patients with Budd-Chiari.
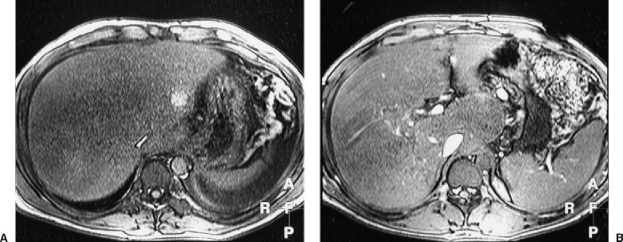
Figure 2.
(A) Axial image in a magnetic resonance imaging study demonstrates heterogeneous liver parenchyma, enlarged liver, absence of hepatic veins, and compression of the intrahepatic portion of the inferior vena cava. (B) Axial image in a magnetic resonance imaging study in the same patient at a lower level demonstrates enlarged caudate lobe, lack of hepatic veins, and patent portal vein branches.
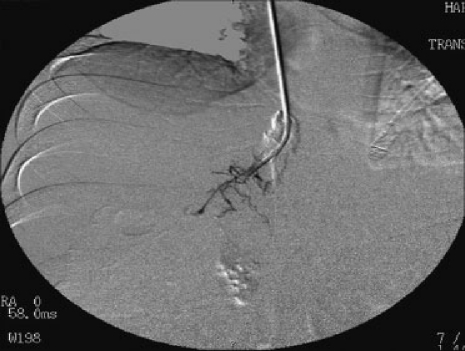
Figure 3.
Spot film demonstrates the transjugular access set embedded in the liver parenchyma. A small amount of contrast has been injected to confirm position of the needle within the parenchyma. The spiderweb image is again demonstrated.
Figure 4.
Intraparenchymal CO2 injection demonstrating opacification of the right branches of the portal vein and main portal vein.
Figure 5.
Portogram after completion of TIPS shows a successful creation of the shunt. The shunt appears widely patent.
PROBLEM: LARGE LIVER TUMOR AND NO SUITABLE HEPATIC VEINS FOR ACCESS; SOLUTION: TRANSCAVAL TIPS
The presence of liver tumors may represent a challenge in the creation of a TIPS. In many instances, the presence of a tumor in the liver has been considered to be a contraindication to the creation of the shunt.14 One of the biggest concerns among clinicians and interventional radiologists has been the possibility of endovascular seeding of malignant liver cells to the lungs. This may occur during the transhepatic puncture attempts to enter the portal vein.14 Axial imaging using a three-phase computed tomography (CT) scan is extremely useful in the planning of the procedure (Fig. 6). In some cases when the tumor is not in the pathway for shunt creation, the TIPS can be created using a standard approach via the right hepatic vein. However, in some cases, if there is concern for tumor seeding or if the existing veins are not usable for shunt creation, alternative approaches may be attempted. The use of a transcaval TIPS creation is an acceptable technical modification (Fig. 6D to 6G). A transcaval TIPS is technically challenging.15,16 The procedure requires careful planning with evaluation of the axial images of the CT scan. An optimal level for inferior vena cava puncture is selected and anatomic correlation is established based on the CT findings. From the technical standpoint, probably the most important maneuver is to bend the transhepatic access needle to obtain almost a 90-degree angle. The access needle is then gently advanced to the anterior wall of the cava at the level selected for the puncture and the transcaval puncture is then performed.16 With this maneuver, the portal vein can be entered usually after the second or third pass. Once the access into the portal vein is obtained, the procedure is completed in the usual fashion. Soares and Murphy described three patients in whom a transcaval TIPS was required including: absent jugular or superior vena caval access to the hepatic veins, Budd-Chiari syndrome, and difficult access into the portal system in patients with preexisting occluded TIPS.16 A transcaval approach may pose a higher risk of vessel injury and bleeding complications; however, if performed carefully, it is an effective way to create a TIPS. The use of direct intravascular ultrasound guidance may be a safer approach; Petersen and Binkert have performed over 40 direct intrahepatic portosystemic shunts (DIPS), using direct intravascular ultrasound guidance. Their results have been excellent with this technique, with no reports of major complications.17
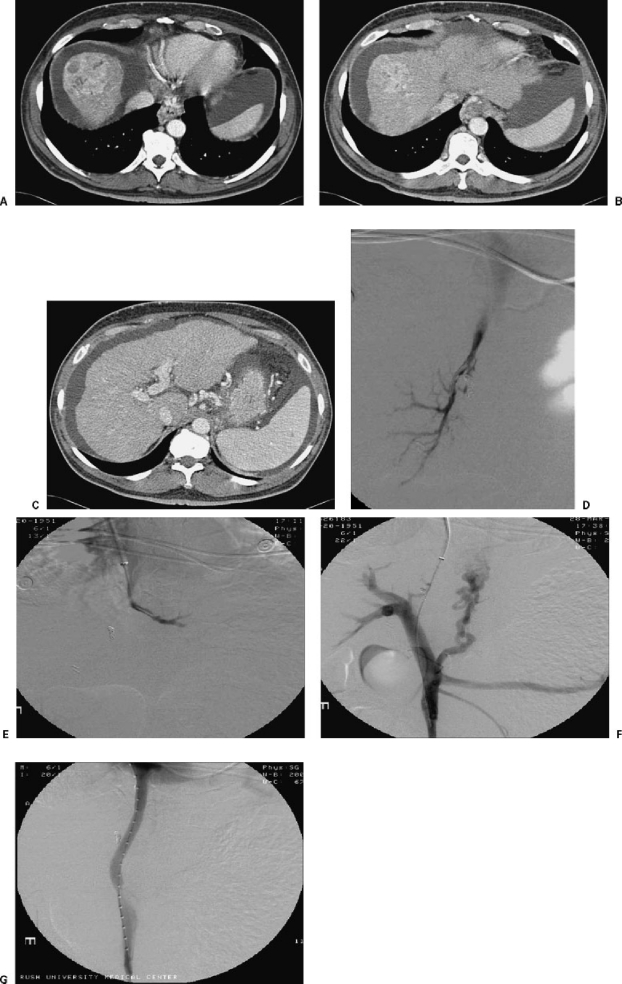
Figure 6.
Hepatocarcinoma of the right lobe of the liver requiring transcaval TIPS. (A) Selected axial cut from a three-phase contrast-enhanced CT demonstrates an irregular, hypervascular mass at the dome of the liver. (B) Axial cut at the level of the origin of the hepatic vein demonstrates that the area of irregularity extends to an area very close to the anticipated origin of the hepatic vein. (C) Axial cut at the level of the portal bifurcation shows a very discrete area of irregularity anterior to the right portal vein. (D) Right hepatic venogram demonstrates a small, irregular right hepatic vein. (E) Left hepatic venogram demonstrates a very small, irregular left hepatic vein. (F) Direct portogram after direct transcaval puncture demonstrating successful entry into the portal system. There is fugal flow into large gastric and esophageal varices. (G) Direct portogram after completion of TIPS procedure. The portogram shows flow within the shunt. No opacification of intrahepatic portal branches and no further opacification of esophageal or gastric varices. The shunt was created with a 10 × 8 cm VIATORR® stent-graft (W.L. Gore, Flagstaff, AZ).
PROBLEM: PORTAL VEIN THROMBOSIS; SOLUTION: PORTAL VEIN RECANALIZATION
Portal vein thrombosis is uncommon condition that may occur in cirrhotic and noncirrhotic patients. This condition may be related to a variety of factors including hypercoagulable states, trauma, neonatal portal vein catheterization, infections, tumors, pancreatitis, and postsurgical conditions.18,19,20,21,22 Recanalization of the thrombosed portal vein has been described by several authors, and these cases are usually approached using a variety of techniques, including percutaneous transhepatic, transjugular, transmesenteric using a combined surgical approach, and even trans-splenic.18 The creation of a TIPS can be technically complex in patients with a thrombosed portal vein, especially if the thrombosis is chronic and associated with cavernomatous transformation.19,23
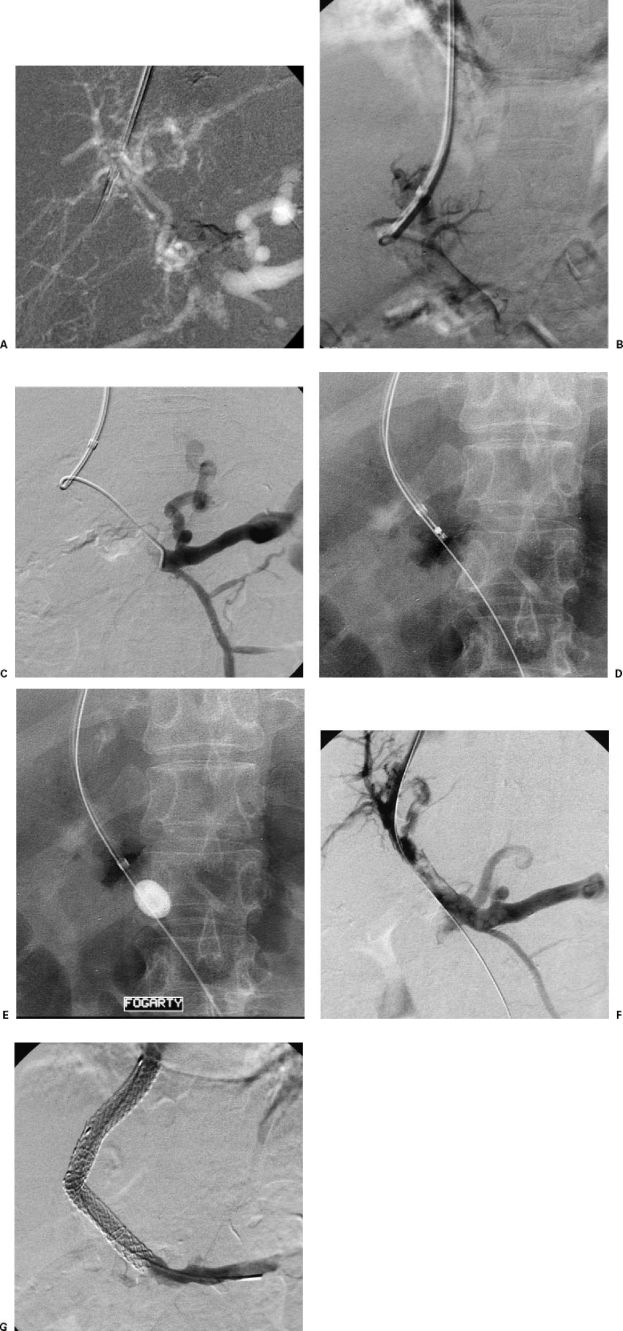
The use of an intraparenchymal injection of CO2 is extremely useful in cases of portal vein thrombosis. Even if the picture is somewhat confusing at first, it may guide the operator toward the correct anatomic position of the portal vessels (Fig. 7A). Once the operator has the correct orientation and a rough idea of where to aim the transparenchymal needle, a pass can be performed. The next step is to probe with a guide wire (Stiff angled glidewire, Terumo, Japan) and attempt to guide the wire toward the expected position of the main portal vein (Fig. 7B). If the guide wire does advance to the expected location of the portal vein, then an angiographic catheter may be used to follow the wire and a portogram may then be performed (Fig. 7B and 7C) . If the portogram confirms correct catheter position within the portal venous system, then the access is secured and further intervention can then be undertaken (Fig. 7D and 7E), including mechanical thrombectomy, reverse Fogarty maneuver, pulse-spray thrombolysis, or stent placement. The TIPS can then be completed in the usual fashion. For cases of portal vein thrombosis, we recommend shunt creation employing stent-grafts because the use of bare stents may be associated with a high risk of rethrombosis (Fig. 7F and 7G).21,24
Figure 7.
(A) Intraparenchymal CO2 injection demonstrating multiple small vascular structures in the liver parenchyma. The splenic vein and small gastric varices can be identified. (B) Direct portogram demonstrates the angiographic catheter within a thrombosed portal vein; no extravasation is noted. (C) Direct portogam now demonstrates the catheter within the splenic vein. There is retrograde flow into the inferior mesenteric vein and into small gastric varices. Note the correlation of images with the transparenchymal CO2 injection. (D) The image demonstrates a mechanical thrombectomy device within the thrombosed portal vein. (E) Image demonstrates additional thrombectomy with a retrograde Fogarty maneuver. (F) Portogram after mechanical thrombectomy shows partially patent portal vein with a moderate amount of residual thrombus. (G) Portogram after completion of TIPS. Two overlapping VIATORR® stent-grafts were placed. The shunt appears widely patent.
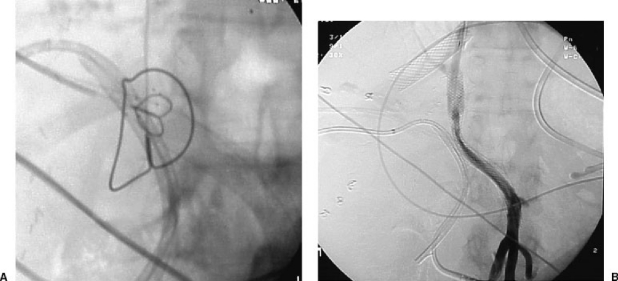
PROBLEM: DIFFICULT ACCESS FROM HEPATIC VEIN TO PORTAL VEIN AFTER MULTIPLE ATTEMPTS; SOLUTION: GUN-SIGHT TECHNIQUE
The gun-sight technique was described by Haskal et al.25 The technique was described to achieve a successful portosystemic shunt in patients with very small, angulated, or occluded hepatic veins.25 This technique involves the placement of a snare within the portal vein and a second snare within the inferior vena cava (Fig. 8A). The connection is then created by performing a puncture through both snares on the same plane (usually in the lateral plane). A wire is then retrieved from the vena cava and the communication is created by advancing a needle or a catheter from the transjugular approach into the portal system. The TIPS can then be completed using the usual maneuvers (Fig. 8B). This is an interesting technique that may be used in a desperate situation when all other maneuvers to create a TIPS have failed.
Figure 8.
(A) Lateral spot film demonstrating the gun-sight technique. The small snare is within the portal vein and the large snare within the inferior vena cava. The next step is to perform a puncture with a needle traversing both snares. (B) Portogram after completion of TIPS procedure after using the gun-sight technique. Note that there is a stent within the right hepatic vein. This stent was thrombosed and precluded an optimal hepatic vein access in this case.
CONCLUSION
TIPS procedures are usually straightforward and should be completed within 1 to 2 hours, using 20 to 30 minutes of fluoroscopic time. The present article describes and illustrates a collection of unusual maneuvers that the authors have found useful in difficult or challenging cases. The employment of these maneuvers may make the difference between an “impossible” TIPS and a successfully created shunt.
REFERENCES
- Richter G M, Noeldge G, Palmaz J C, Roessle M. The transjugular intrahepatic portosystemic stent-shunt (TIPSS): results of a pilot study. Cardiovasc Intervent Radiol. 1990;13:200–207. doi: 10.1007/BF02575474. [DOI] [PubMed] [Google Scholar]
- Saxon R R, Keller F S. Technical aspects of accessing the portal vein during the TIPS procedure. J Vasc Interv Radiol. 1997;8:733–744. doi: 10.1016/s1051-0443(97)70655-9. [DOI] [PubMed] [Google Scholar]
- Richter G M, Noeldge G, Palmaz J C, et al. Transjugular intrahepatic portacaval stent shunt: preliminary clinical results. Radiology. 1990;174:1027–1030. doi: 10.1148/radiology.174.3.174-3-1027. [DOI] [PubMed] [Google Scholar]
- Teitelbaum G P, Van Allan R J, Reed R A, Hanks S, Katz M D. Portal venous branch targeting with a platinum-tipped wire to facilitate transjugular intrahepatic portosystemic shunt (TIPS) procedures. Cardiovasc Intervent Radiol. 1993;16:198–200. doi: 10.1007/BF02641894. [DOI] [PubMed] [Google Scholar]
- Muller M F, Siewert B, Stokes K R, et al. MR angiographic guidance for transjugular intrahepatic portosystemic shunt procedures. J Magn Reson Imaging. 1994;4:145–150. doi: 10.1002/jmri.1880040208. [DOI] [PubMed] [Google Scholar]
- Warner D L, Owens C A, Hibbeln J F, Ray C E., Jr Indirect localization of the portal vein during a transjugular intrahepatic portosystemic shunt procedure: placement of a radiopaque marker in the hepatic artery. J Vasc Interv Radiol. 1995;6:87–89. doi: 10.1016/s1051-0443(95)71065-x. discussion 89–90. [DOI] [PubMed] [Google Scholar]
- Sheppard D G, Moss J, Miller M. Imaging of the portal vein during transjugular intrahepatic portosystemic shunt procedures: a comparison of carbon dioxide and iodinated contrast. Clin Radiol. 1998;53:448–450. doi: 10.1016/s0009-9260(98)80275-4. [DOI] [PubMed] [Google Scholar]
- Petersen B, Uchida B T, Timmermans H, Keller F S, Rosch J. Intravascular US-guided direct intrahepatic portacaval shunt with a PTFE-covered stent-graft: feasibility study in swine and initial clinical results. J Vasc Interv Radiol. 2001;12:475–486. doi: 10.1016/s1051-0443(07)61887-9. [DOI] [PubMed] [Google Scholar]
- Rose S C, Pretorius D H, Nelson T R, et al. Adjunctive 3D US for achieving portal vein access during transjugular intrahepatic portosystemic shunt procedures. J Vasc Interv Radiol. 2000;11:611–621. doi: 10.1016/s1051-0443(07)61614-5. [DOI] [PubMed] [Google Scholar]
- Haskal Z J, Martin L, Cardella J F, et al. Quality improvement guidelines for transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 2001;12:131–136. doi: 10.1016/s1051-0443(07)61817-x. [DOI] [PubMed] [Google Scholar]
- Bilbao J I, Pueyo J C, Longo J M, et al. Interventional therapeutic techniques in Budd-Chiari syndrome. Cardiovasc Intervent Radiol. 1997;20:112–119. doi: 10.1007/s002709900117. [DOI] [PubMed] [Google Scholar]
- Fried M W, Connaghan D G, Sharma S, et al. Transjugular intrahepatic portosystemic shunt for the management of severe venoocclusive disease following bone marrow transplantation. Hepatology. 1996;24:588–591. doi: 10.1002/hep.510240321. [DOI] [PubMed] [Google Scholar]
- Hausegger K A, Tauss J, Karaic K, Klein G E, Uggowitzer M. Use of the left internal jugular vein approach for transjugular portosystemic shunt. AJR Am J Roentgenol. 1998;171:1637–1639. doi: 10.2214/ajr.171.6.9843303. [DOI] [PubMed] [Google Scholar]
- Wallace M, Swaim M. Transjugular intrahepatic portosystemic shunts through hepatic neoplasms. J Vasc Interv Radiol. 2003;14:501–507. doi: 10.1097/01.rvi.0000064846.87207.ab. [DOI] [PubMed] [Google Scholar]
- Gasparini D, Del Forno M, Sponza M, et al. Transjugular intrahepatic portosystemic shunt by direct transcaval approach in patients with acute and hyperacute Budd-Chiari syndrome. Eur J Gastroenterol Hepatol. 2002;14:567–571. doi: 10.1097/00042737-200205000-00017. [DOI] [PubMed] [Google Scholar]
- Soares G M, Murphy T P. Transcaval TIPS: indications and anatomic considerations. J Vasc Interv Radiol. 1999;10:1233–1238. doi: 10.1016/s1051-0443(99)70224-1. [DOI] [PubMed] [Google Scholar]
- Petersen B, Binkert C. Intravascular ultrasound-guided direct intrahepatic portacaval shunt: midterm follow-up. J Vasc Interv Radiol. 2004;15:927–938. doi: 10.1097/01.RVI.0000133703.35041.42. [DOI] [PubMed] [Google Scholar]
- Bilbao J I, Elorz M, Vivas I, Martinez-Cuesta A, Bastarrika G, Benito A. Transjugular intrahepatic portosystemic shunt (TIPS) in the treatment of venous symptomatic chronic portal thrombosis in non-cirrhotic patients. Cardiovasc Intervent Radiol. 2004;27:474–480. doi: 10.1007/s00270-004-0241-z. [DOI] [PubMed] [Google Scholar]
- Matsui O, Yoshikawa J, Kadoya M, et al. Transjugular intrahepatic portosystemic shunt after previous recanalization of a chronically thrombosed portal vein via a transmesenteric approach. Cardiovasc Intervent Radiol. 1996;19:352–355. doi: 10.1007/BF02570190. [DOI] [PubMed] [Google Scholar]
- Stein M, Link D P. Symptomatic spleno-mesenteric-portal venous thrombosis: recanalization and reconstruction with endovascular stents. J Vasc Interv Radiol. 1999;10:363–371. doi: 10.1016/s1051-0443(99)70044-8. [DOI] [PubMed] [Google Scholar]
- Uflacker R. Applications of percutaneous mechanical thrombectomy in transjugular intrahepatic portosystemic shunt and portal vein thrombosis. Tech Vasc Interv Radiol. 2003;6:59–69. doi: 10.1053/tvir.2003.36433. [DOI] [PubMed] [Google Scholar]
- Radovich P A. Portal vein thrombosis and liver disease. J Vasc Nurs. 2000;18:1–5. doi: 10.1016/s1062-0303(00)90052-9. [DOI] [PubMed] [Google Scholar]
- Blum U, Haag K, Rossle M, et al. Noncavernomatous portal vein thrombosis in hepatic cirrhosis: treatment with transjugular intrahepatic portosystemic shunt and local thrombolysis. Radiology. 1995;195:153–157. doi: 10.1148/radiology.195.1.7892458. [DOI] [PubMed] [Google Scholar]
- Bureau C, Garcia-Pagan J C, Otal P, et al. Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: results of a randomized study. Gastroenterology. 2004;126:469–475. doi: 10.1053/j.gastro.2003.11.016. [DOI] [PubMed] [Google Scholar]
- Haskal Z J, Duszak R, Jr ,Furth E E. Transjugular intrahepatic transcaval portosystemic shunt: the gun-sight approach. J Vasc Interv Radiol. 1996;7:139–142. doi: 10.1016/s1051-0443(96)70750-9. [DOI] [PubMed] [Google Scholar]