ABSTRACT
We describe a 44-year-old man with end-stage renal disease who underwent insertion of a stent graft to repair a hemodialysis graft pseudoaneurysm. The indication for stent graft placement was an acute and rapidly enlarging intragraft pseudoaneurysm. The patient experienced no complications following the procedure, but he presented with two graft occlusions within the 2 months following the procedure.
Keywords: Hemodialysis access, pseudoaneurysm, stent graft
A pseudoaneurysm is a complication that can develop in arteriovenous (AV) hemodialysis grafts in patients with end-stage renal disease (ESRD) on chronic hemodialysis. The development of a pseudoaneurysm is multifactorial. Repeated graft cannulations cause disruption and fragmentation of the graft material, leading to an increased risk of pseudoaneurysm formation. When outflow venous stenosis occurs, the intragraft pressure increases and further disrupts the defects in the graft, leading to the development of a pseudoaneurysm or large area of graft degeneration.1,2 In general, the disruption of the graft material is an indolent process that may have a chronic evolution. This then evolves into large “soft spots” in the dialysis graft that may be repeatedly cannulated by dialysis nurses because of the ease of access. These areas of graft degeneration usually have a wide mouth and do not present a major threat for perforation. The most common complication associated with these lesions is the development of mural thrombus and subsequent hemodialysis graft thrombosis. But a true hemodialysis graft pseudoaneurysm represents a small focal orifice in the graft material that causes a massive enlargement of the overlying skin. In our experience, these lesions have a very high risk of perforation. This complication must be therefore be addressed immediately because if perforation occurs, uncontrollable bleeding and, eventually, patient death may result.
The treatment for intragraft pseudoaneurysms has classically been surgical revision of the graft. However, in the past 5 to 10 years, the endovascular management of these lesions has gained increasing importance. We present a case of endovascular management of a large acute intragraft pseudoaneurysm with the placement of a stent graft.
CASE REPORT
Our patient is a 44-year-old man with a history of ESRD secondary to thrombotic microangiopathy, antiphospholipid antibody syndrome, hypertension, deep venous thrombosis, and schizoaffective disorder. The patient was initially diagnosed with ESRD in July 2004, and he subsequently underwent the creation of a C-shaped loop permanent synthetic AV graft in his left arm between the brachial artery and basilic vein for hemodialysis.
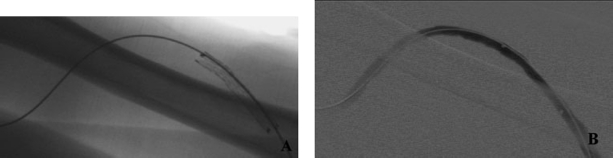
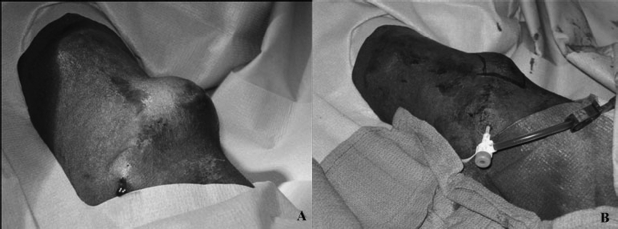
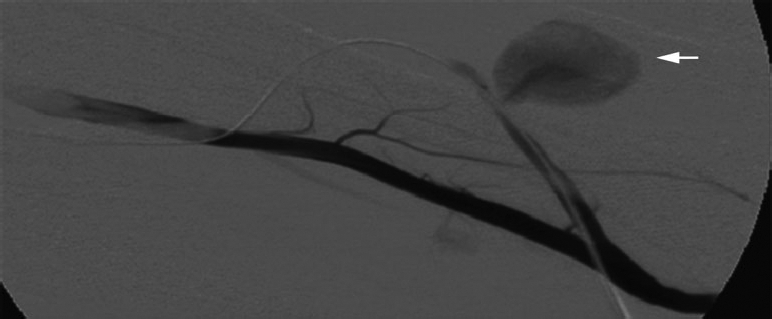
The patient was seen again in March 2006 when he arrived with complaints of a quickly enlarging arm mass. An arterial duplex scan identified a 3.4 × 3.5 × 2.8 cm pseudoaneurysm with partial peripheral thrombosis. A hemodialysis fistulogram demonstrated a 70% stenosis within the venous outflow anastomosis. The pseudoaneurysm was identified in the arterial limb of the graft (Fig. 1). The case was discussed with the transplant surgeon, and it was decided to treat the venous anastomotic stenosis with balloon angioplasty and the pseudoaneurysm with stent graft placement. A 4-cm-long × 9-mm-wide self-expandable polytetrafluoroethylene (ePTFE) covered Fluency Plus stent graft (BARD, Tempe, AZ) was employed to occlude the pseudoaneurysm. The stent graft was deployed across the neck of the pseudoaneurysm and expanded with a 7-mm-wide angioplasty balloon (Fig. 2). Poststent angiogram showed excellent results, with complete occlusion of the pseudoaneurysm. The pseudoaneurysm sac was then percutaneously drained with a One Step needle (Merit Medical, South Jordan, UT) (Fig. 3).
Figure 1.
Fistulogram of synthetic arteriovenous graft reveals enlarging pseudoaneurysm (arrow).
Figure 2.
(A) Postprocedure digital image shows stent in final position. (B) Digital subtraction fistulogram shows patent graft and patent stent graft with successful occlusion of pseudoaneurysm.
Figure 3.
(A) Photograph illustrates pseudoaneurysm before stent placement. (B) Note decrease in size of pseudoaneurysm after stent placement.
DISCUSSION
Synthetic AV grafts are one of the most commonly used options to create a permanent vascular access conduit and they are usually composed of ePTFE. Grafts are not as desirable when compared with natural AV fistulas due to the higher failure rates and the lower patency. With recurrent intervention with procedures such as angioplasty or thrombectomy, a synthetic graft can reach a patency close to that of the natural AV fistula.3,4 The advantage of using a synthetic graft is that it is easier to create surgically, has a shorter maturation time, and is easier to canulate.3
Repeated cannulation of the ePTFE grafts leads to disruption and fragmentation of the ePTFE graft material, causing an increase in the rate of stenotic events and associated complications, such as formation of pseudoaneurysms or areas of graft degeneration.1 Pseudoaneurysm formation can create many difficulties for the patient, aside from the visual disfiguration. The pseudoaneurysm can predispose the patient to turbulent flow and thrombosis. It can create difficulties in accessing the graft during dialysis sessions, predispose the patient to spontaneous bleeding, become infected, or threaten the overlying skin.5,6 Pseudoaneurysm perforation may be a fatal complication due to exsanguination.
Indications for therapeutic intervention for pseudoaneurysm formation, as defined by the National Kidney Foundation's Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines,7 include rapidly expanding size, diameter twice greater than the graft diameter, infection, or threat to the overlying skin. Current therapeutic options are chosen based on the size of the pseudoaneurysm. Small pseudoaneurysms may be monitored if they are not clinically significant, can be occluded with direct compression under sonographic guidance, or thrombosed with the use of thrombotic agents.8 An alternative is to intervene surgically with excision and ligation of the affected graft area. More recent reports have illustrated the use of stent grafts to occlude the pseudoaneurysm.1,5,6,9,10,11,12
Vesely et al reported the use of Viabahn stent grafts (W.L. Gore, Flagstaff, AZ) to repair pseudoaneurysms of hemodialysis grafts in 11 patients.1 The Viabahn stent graft is a self-expandable nitinol stent with an ePTFE cover. Results yielded continued patency in 5 of the 11 patients; the rest had required interventions at varying intervals. Complications requiring interventions in the other patients included continuous issues with the previous pseudoaneurysm or issues from the continued cannulation of the graft. The author asserts that utilizing a stent graft to repair a pseudoaneurysm may be an effective method for treating clinically significant pseudoaneurysms.
A previous study by Ryan et al examined the use of a WALLGRAFT Dacron-covered stent (Boston Scientific, Natick, MA) to treat pseudoaneurysms in four patients.5 None of the patients suffered recurrent complications associated with the original pseudoaneurysm, but two had undergone treatment later on for elevated venous pressures and a new pseudoaneurysm formation. The authors indicate that using a WALLGRAFT device is a viable option, and puncturing the stent graft device did not cause any recurrence of the treated pseudoaneurysm.
At our institution we have performed stent graft placement for the treatment of hemodialysis access pseudoaneurysms or areas of graft degeneration in 16 patients. We have exclusively used the Fluency Plus stent graft. A total of 28 stents were deployed for indications of spontaneous bleeding, thrombus formation, and an enlarging pseudoaneurysm. Ten of the 16 patients presented with an enlarging pseudoaneurysm on either the arterial or venous limbs of the graft. Of the 16 patients, 4 exhibited complications after the stent was deployed. Three patients suffered from endoleak, and one patient had migration of the stent. Six patients required between two and five stents to exclude the lesion successfully. Follow-up was done at an average of 3 months after stent placement. In our short experience with this therapeutic alternative, we have found that true pseudoaneurysms respond better than areas of graft degeneration. Usually, true pseudoaneurysms require placement of a single stent, whereas graft degeneration areas with a wider mouth require two or more stents. We have also treated venous aneurysms in native fistulas, but our experience with the management of these lesions has not been encouraging. These lesions usually require more than one stent graft and are more prone to endoleaks after stent graft placement, which is probably related to vein distensibility. In general, the evidence accumulated at our institution demonstrates that utilizing a ePTFE stent graft provides an acceptable alternative in the treatment of true pseudoaneurysms arising in synthetic hemodialysis grafts. This correlates with other institutions' experience using different brands of stent grafts. The use of stent grafts to treat clinically significant pseudoaneurysms appears to be a viable option. It provides additional choices to patients who might not be capable of undergoing further surgery to create a new fistula or are unable to undergo further surgical revision of their grafts. This procedure allows these patients to maintain the patency in their graft and extend the life of the current AV graft.
REFERENCES
- Vesely T M. Use of stent grafts to repair hemodialysis graft-related pseudoaneurysms. J Vasc Interv Radiol. 2005;16:1301–1307. doi: 10.1097/01.RVI.0000175903.38810.13. [DOI] [PubMed] [Google Scholar]
- Hein A N, Vesely T M. Use of the percutaneous thrombolytic device for the treatment of thrombosed pseudoaneurysms during mechanical thrombectomy of hemodialysis grafts. J Vasc Interv Radiol. 2002;13:201–204. doi: 10.1016/s1051-0443(07)61939-3. [DOI] [PubMed] [Google Scholar]
- Roy-Chaudhury P, Kelly B S, Melhem M, et al. Vascular access in hemodialysis: issues, management, and emerging concepts. Cardiol Clin. 2005;23:249–273. doi: 10.1016/j.ccl.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Cinat M E, Hopkins J, Wilson S E. A prospective evaluation of PTFE graft patency and surveillance techniques in hemodialysis access. Ann Vasc Surg. 1999;13:191–198. doi: 10.1007/s100169900241. [DOI] [PubMed] [Google Scholar]
- Ryan J M, Dumbleton S A, Doherty J, Smith T P. Technical innovation: using a covered stent (wallgraft) to treat pseudoaneurysms of dialysis grafts and fistulas. AJR Am J Roentgenol. 2003;180:1067–1071. doi: 10.2214/ajr.180.4.1801067. [DOI] [PubMed] [Google Scholar]
- Silas A M, Bettmann M A. Utility of covered stents for revision of aging failing synthetic hemodialysis grafts: a report of three cases. Cardiovasc Intervent Radiol. 2003;26:550–553. doi: 10.1007/s00270-003-0013-1. [DOI] [PubMed] [Google Scholar]
- NKF-K/DOQI clinical practice guidelines for vascular access: update 2000. Am J Kidney Dis. 2001;37(suppl 1):S137–S181. doi: 10.1016/s0272-6386(01)70007-8. [DOI] [PubMed] [Google Scholar]
- Rodriguez H E, Leon L, Schalch P, Labropoulos N, Borge M, Kalman P G. Arteriovenous access: managing common problems. Perspect Vasc Surg Endovasc Ther. 2005;17:155–166. doi: 10.1177/153100350501700221. [DOI] [PubMed] [Google Scholar]
- Rhodes E S, Silas A M. Dialysis needle puncture of Wallgrafts placed in polytetrafluoroethylene hemodialysis grafts. J Vasc Interv Radiol. 2005;16:1129–1134. doi: 10.1097/01.RVI.0000167852.14245.05. [DOI] [PubMed] [Google Scholar]
- Najibi S, Bush R L, Terramani T T, et al. Covered stent exclusion of dialysis access pseudoaneurysms. J Surg Res. 2002;106:15–19. doi: 10.1006/jsre.2002.6389. [DOI] [PubMed] [Google Scholar]
- Rabindranauth P, Shindelman L. Transluminal stent-graft repair for pseudoaneurysm of PTFE hemodialysis grafts. J Endovasc Surg. 1998;5:138–141. doi: 10.1583/1074-6218(1998)005<0138:TSGRFP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Hausegger K A, Tiessenhausen K, Klimpfinger M, Raith J, Hauser H, Tauss J. Aneurysms of hemodialysis access grafts: treatment with covered stents—a report of three cases. Cardiovasc Intervent Radiol. 1998;21:334–337. doi: 10.1007/s002709900271. [DOI] [PubMed] [Google Scholar]