ABSTRACT
Successful transcatheter arterial embolization of symptomatic adrenal aldosteronoma in a 56-year-old woman with hypertension and hypokalemia is described. The presentation, diagnosis, and treatment of aldosterone-producing tumors are subsequently discussed.
Keywords: Aldosteronoma, embolization, ethanol
Primary aldosteronism, also termed Conn's syndrome, is clinically characterized by intractable hypertension and hypokalemia. When due to a solitary aldosterone-producing tumor, this condition is typically curable, with surgical resection the established treatment method. Alternative therapies for management of symptomatic aldosteronomas have been investigated for patients who cannot tolerate surgery, however. In this article, a case of endovascular aldosteronoma embolization is presented, and the presentation, diagnosis, and treatment of aldosterone-producing tumors are discussed.
CASE REPORT
A 56-year-old African American woman with a past medical history significant for amyotrophic lateral sclerosis presented with refractory hypertension, despite treatment with multiple combinations of antihypertensive medications, as well as severe persistent hypokalemia requiring daily supplementation. Measured blood pressure was 160/120 mm Hg, and laboratory analysis showed a potassium level of 2.6.
Clinical workup included computed tomography (CT) of the abdomen, which revealed a left adrenal nodule measuring ~1.8 cm. The lesion was described as “very vascular” in early arterial phase imaging and showed contrast washout characteristics consistent with a lipid-poor adenoma. Functioning adrenal adenoma was suspected, and subsequent adrenal vein sampling performed at an outside hospital confirmed left-sided lateralization compatible with a functioning aldosteronoma.
The patient was deemed a poor surgical candidate due to poor condition. Interventional radiology was therefore consulted for a minimally invasive alternative treatment of the patient's aldosteronoma.
After consent was obtained and documented, the patient was brought to the interventional radiology suite and the groins were prepped and draped in the usual sterile manner. The right common femoral artery was accessed using an 18-gauge single-wall needle, and after advancing a 0.035-inch Bentson guidewire (Cook, Bloomington, IN) into the abdominal aorta, a 5F vascular sheath was placed. Next, a 5F Omni Flush catheter (AngioDynamics, Queensbury, NY) was advanced over the Bentson wire and formed in the abdominal aorta. Aortogram was performed and revealed a hypervascular blush in the region of the left adrenal gland (Fig. 1), localizing the tumor. The left adrenal artery was then selected using a 5F SOS catheter. Using a Renegade Hi-Flo microcatheter (Boston Scientific, Natick, MA) and a 0.014-inch Luge guidewire (Boston Scientific, Natick, MA), the left adrenal branch supplying the adenoma was superselected, and an arteriogram was performed (Fig. 2). From here, this vessel was embolized using a 3:1 mixture of alcohol to lipiodol. Postembolization angiography was performed (Fig. 3). The catheters and sheath were removed. The patient tolerated the procedure well and was instructed to discontinue all of her antihypertensive medications after the procedure.
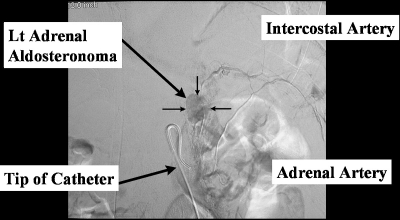
Figure 1.
Aortogram hypervascular blush of left adrenal adenoma (arrows).
Figure 2.
Superselective angiogram better delineates left adrenal adenoma (arrows). Catheter, intercostals artery, and adrenal artery labeled.
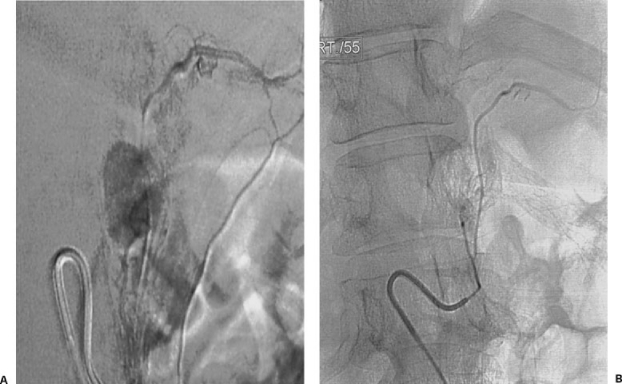
Figure 3.
(A) Infusion of alcohol and lipiodol into adrenal adenoma. (B) Postembolization image shows loss of hypervascular tumor blush.
Up to 4 months postprocedure follow-up showed that the patient was no longer hypertensive and was able to abandon all antihypertensive medications. Serum potassium levels improved; they did not return to normal range, however.
DISCUSSION
Dr. Jerome W. Conn was the first to characterize primary aldosteronism in 1956, and he specifically referred to a functioning adrenal aldosteronoma causing hypertension and hypokalemia. Although primary aldosteronism accounts for only 0.05 to 2% of cases of hypertension in the general population, recognition of the disease is important because symptoms almost always resolve after adrenalectomy.1
The cause of primary aldosteronism is an adrenal adenoma in 80% of patients and adrenal gland hyperplasia in 20%. Adrenal carcinoma is an extremely rare cause of primary aldosteronism. In 75 to 90% of patients with a solitary aldosterone-producing tumor, surgical adrenalectomy corrects the hypertension and hypokalemia. However, alternatives to surgical adrenalectomy have been investigated for patients who are not able to withstand surgery or are reluctant to undergo surgery.1
Clinical manifestations of primary hyperaldosteronism occur as the result of aldosterone excess in the renal tubules. Aldosterone causes sodium retention and, as a result, potassium loss. Sodium retention promotes water retention, an increase in the extracellular volume, and a decrease of renin production. The combination of these factors usually results in medically uncontrollable hypertension. Potassium loss can lead to hypokalemic alkalosis, which results in muscular weakness, cramping, tetany, palpitations, and abnormal electrocardiogram findings.
Documentation of decreased renin levels is essential to the diagnosis. A sodium chloride suppression test can be used to demonstrate the inability to suppress aldosterone secretion. This suppression test involves the administration of large amounts of sodium chloride over 3 to 5 days, which causes hypokalemia in 80 to 90% of patients with primary aldosteronism. This response is associated with muscle weakness, cardiac arrhythmia, carbohydrate intolerance, and nephrogenic diabetes insipidus. Hypertension associated with primary aldosteronism is usually benign, but in rare cases, malignant hypertension may develop.1
Adrenal vein sampling also aids in diagnosis of aldosteronoma. Cortisol and aldosterone samples are obtained from both the right and left adrenal veins and from the infra-adrenal and supra-adrenal inferior vena cava both before and after intravenous administration of cosyntropin. Aldosteronomas have an average size of 1.7 cm (range, 0.5 to 3.5 cm), the left adrenal gland is affected more often, and the tumors are bilateral in 6% of patients.1
Transcatheter arterial embolization with ethanol has been described in cases of renal cell carcinoma,2 adrenal pheochromocytoma,3 and liver metastases.4 Little has been written about nonsurgical treatment of aldosteronomas. Perhaps the most extensive study to date involved adrenal arterial ethanol embolization in 33 cases.5 Blood pressure decreased in 27 of the 33 patients. Decrease in blood pressure was not influenced by sex, age, hypertension duration, family history of hypertension, adenoma site, type of ethanol used, or number of arteries embolized.
Due to the recent development and improvement in laparoscopic adrenalectomy, many patients still opt for surgery. However, transcatheter arterial embolization still has several advantages over surgery. First, the procedure time of embolization is significantly less. Embolization can also be performed with moderate sedation and local anesthesia, whereas surgery requires general anesthesia. The success rate of aldosteronoma embolization has been reported at 82%.3 The success rate of surgical adrenalectomy, open or laparoscopic, has been reported as > 90%.6,7
Other minimally invasive treatments of aldosteronoma have been described, including CT-guided percutaneous injection of alcohol and acetic acid. However, complications such as adrenal hemorrhage have been encountered with this method. No study has reported hemorrhage as a significant complication of transarterial embolization of aldosteronoma.8,9 Radiofrequency ablation of aldosteronoma has also been described.10
CONCLUSION
In summary, our experience with transarterial embolization of an aldosteronoma proved to be safe and effective. Overall, ethanol embolization of aldosteronomas is an effective alternative for patients who are poor surgical candidates or for those who do not desire open surgery. Therefore, transarterial embolization of aldosteronoma should be considered as a viable therapy for these lesions.
REFERENCES
- Khan A N. Hyperaldosteronism. Available at: www.emedicine.com/radio/topic354.htm Available at: www.emedicine.com/radio/topic354.htm
- Ellman B A, Parkhill B J, Curry T S, III, Marcus P B, Peters P C. Ablation of renal tumors with absolute ethanol: a new technique. Radiology. 1981;141:619–626. doi: 10.1148/radiology.141.3.7302214. [DOI] [PubMed] [Google Scholar]
- Onohara S, Kobayashi H, Uchiyama N, Sonoda T, Oyama T, Shinohara S. A successfully treated case of malignant pheochromocytoma by arterial embolization using absolute ethanol. Nippon Igaku Hoshasen Gakkai Zasshi. 1983;43:1–8. [PubMed] [Google Scholar]
- Shibata T, Maetani Y, Ametani F, Itoh K, Konishi J. Percutaneous ethanol injection for treatment of adrenal metastasis from hepatocellular carcinoma. AJR Am J Roentgenol. 2000;174:333–335. doi: 10.2214/ajr.174.2.1740333. [DOI] [PubMed] [Google Scholar]
- Hokotate H, Inoue H, Baba Y, Tsuchimochi S, Nakajo M. Aldosternomas: experience with superselective adrenal arterial embolization in 33 cases. Radiology. 2003;227:401–406. doi: 10.1148/radiol.2272011798. [DOI] [PubMed] [Google Scholar]
- Weigel R J, Wells S A, Gunnells J C, Leight G S. Surgical treatment of primary hyperaldosteronism. Ann Surg. 1994;219:347–352. doi: 10.1097/00000658-199404000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granberg P O, Adamsson U, Hamberger B, Lins P E. Surgical treatment of primary aldosteronism. Ann Chir Gynaecol. 1983;72:171–176. [PubMed] [Google Scholar]
- Rossi R, Savastano S, Tommaselli A P, et al. Percutaneous computed tomography-guided ethanol injection in aldosterone-producing adrenocortical adenoma. Eur J Endocrinol. 1995;132:302–305. doi: 10.1530/eje.0.1320302. [DOI] [PubMed] [Google Scholar]
- Liang H L, Pan H B, Lee Y H, et al. Small functional adrenal adenoma: treatment with CT-guided percutaneous acetic acid injection—report of three cases. Radiology. 1999;213:612–615. doi: 10.1148/radiology.213.2.r99nv10612. [DOI] [PubMed] [Google Scholar]
- Mayo-Smith W W, Dupuy D E. Adrenal neoplasms: CT-guided radiofrequency ablation—preliminary results. Radiology. 2004;231:225–230. doi: 10.1148/radiol.2311031007. [DOI] [PubMed] [Google Scholar]