ABSTRACT
Despite the clinical complexity of patients with severe liver disease and the technical demands associated with the creation of a transjugular intrahepatic portosystemic shunt (TIPS), the major complication rate of this procedure is less than 5%. Delayed recognition and treatment of complications related to TIPS can have life-threatening consequences. This article provides an overview of the spectrum of periprocedural and delayed complications related to the performance of TIPS and offers the reader pearls for both avoiding and managing those complications.
Keywords: Hypertension—portal, complications—transjugular portosystemic shunts, portal vein perforation, metallic stents—complications
The creation of a transjugular intrahepatic portosystemic shunt (TIPS) is one of the most challenging procedures performed by interventional radiologists. With increased experience, the technical success rate of the procedure should be greater than 95% with a major complication rate of less than 5%.1,2 This article will focus on the most common complications related to the TIPS procedure and some practical solutions to avoid or solve these complications.
PATIENT'S INDIVIDUAL RISK FOR COMPLICATIONS
Earlier studies have evaluated independent predictors of 30-day mortality after TIPS placement in attempts to identify patients at risk. Several risk factors have been identified including sex, age, preexisting encephalopathy, elevated liver enzymes, hyperbilirubinemia, high creatinine, low albumin levels, presence of ascites, and emergent versus elective TIPS procedure.3,4,5,6,7 It has also been well described that patients undergoing an emergency TIPS have a higher postprocedural mortality when compared with patients undergoing elective TIPS.8,9 The utility of clinical and biochemical scoring systems such as the Child-Pugh score, the prognotic index (PI) score, and the Acute Physiology and Chronic Health Evaluation (APACHE) II score have also been evaluated.6,10 In general, it has been described that patients undergoing emergent TIPS and have a Child-Pugh score > 12, a PI score > 18.52, or an APACHE II score > 18 have a poor prognosis.6,10,11 Recently, the model of end-stage liver disease (MELD) score was developed to predict the 3-month mortality of patients undergoing elective TIPS.12 In this scoring system, the serum bilirubin levels, serum creatinine levels, and international normalized ratio are plotted in a formula and a score is calculated.13 A MELD score greater than 18 has been described to be associated with a poor prognosis.14,15,16 The first step to a successful TIPS is careful patient selection.
PROCEDURAL COMPLICATIONS
Vascular Access
CAROTID ARTERY INJURIES
Puncture of the carotid artery may occur while attempting an internal jugular vein approach for the TIPS procedure, especially if the landmark technique to access the jugular vein is employed. Venous access should be obtained using real-time sonographic guidance. This maneuver is very safe and expedites the venous access step of the procedure.
RIGHT ATRIAL PERFORATION
Perforation of the right atrium caused by the 10-F access sheath has been described.17 This complication has occurred after the TIPS procedure in patients in whom the sheath was left in place for intravenous fluids, medications, or a 24-hour post-TIPS follow-up.17 The long, rigid sheath may perforate the wall of the right atrium, with the risk exacerbated by trauma to the atrial wall resulting from the heart's pulsations. To avoid this problem, the long 10-F sheath must be exchanged for a short 10-F sheath if the access must be preserved for further medical management.
Complications during Portal Vein Localization
BLEEDING AFTER PERCUTANEOUS PORTOGRAPHY
The key step during the TIPS procedure is obtaining a safe access into the portal vein. Many authors have emphasized the importance of portal vein localization before attempting the transhepatic puncture.18,19,20,21 If the precise position of the portal vein is known, the operator has a target to aim toward and in theory, the number of transhepatic punctures can be reduced. When the TIPS procedure was in its early stages of development, one of the first maneuvers described for localization of the portal vein was the percutaneous placement of a retrieval basket into the main portal vein.22 The retrieval basket was used as a target for the transhepatic punctures.18 Investigators soon found that there was a high incidence of bleeding through the transhepatic tract with a high potential for a fatal outcome, and this technique was rapidly abandoned.22
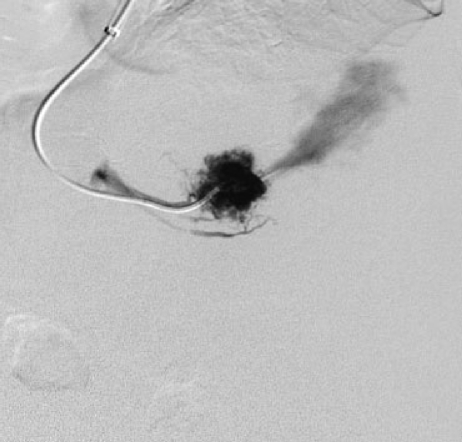
CAPSULAR LACERATION DURING WEDGED HEPATIC VENOGRAM
In current practice, the wedged hepatic venogram is probably the most commonly employed method for portal vein localization during a TIPS procedure.20 An angiographic catheter or a balloon-occlusion catheter is placed in a wedged position in one of the hepatic veins. Next, either iodinated contrast or CO2 is injected through the catheter to obtain retrograde opacification of the portal vein. With this technique, successful opacification of the portal vein is achieved in over 90% of cases.20 Liver laceration with capsular perforation can occur during a wedged hepatic venogram23 (Fig. 1) and is probably related to either forceful injection of the iodinated contrast or explosive delivery of CO2. This complication may have a fatal outcome23; however, in our experience, three patients have survived this event. We think that the most appropriate action when this complication is identified is to stay calm and try to create the shunt as soon and safely as possible. This complication is best avoided by performing a careful wedged hepatic venogram using CO2 delivery through a closed-bag system. We recommend gentle pressure during CO2 injection at a rate of 15 mL/s × 2 seconds. Excellent images of the portal vein can be obtained with this technique.
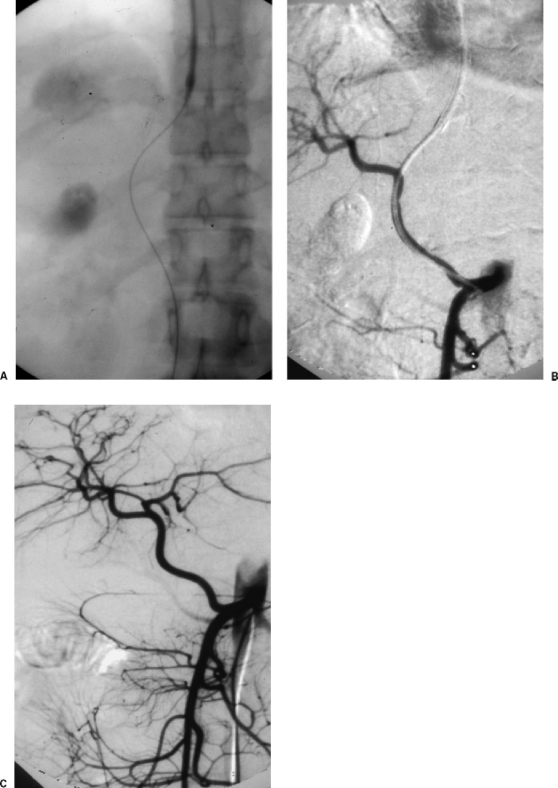
Figure 1.
Capsular perforation during wedged hepatic venogram. Digital subtraction angiogram demonstrates active extravasation of contrast into the peritoneal cavity during a wedged hepatic venogram in a patient with situs inversus. This finding is indicative of laceration of the liver capsule.
Complications during Portal Vein Access
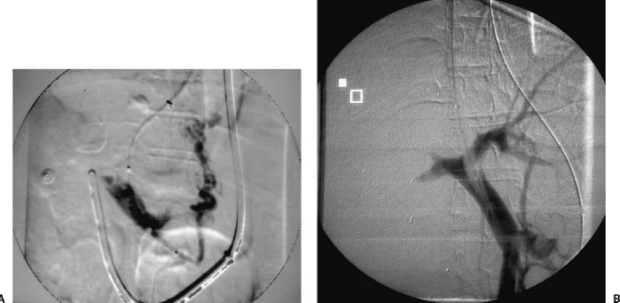
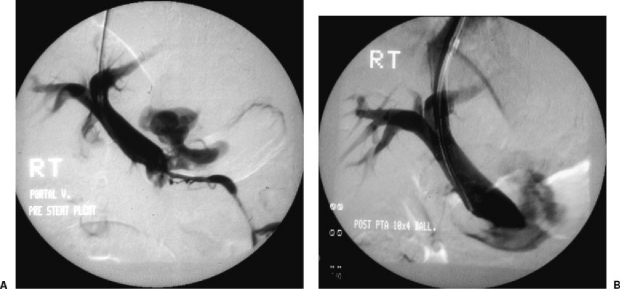
PORTAL VEIN PERFORATION
Obtaining access into the portal vein is the most challenging step during the TIPS procedure. Several techniques have been described to facilitate portal vein puncture and make it safer, including real-time ultrasonographic guidance,21 placement of a guide wire in the portal vein, and recently, using a sectorial intravascular ultrasound to perform the puncture.24 A puncture directly into the main portal vein with subsequent portal vein perforation may result in massive bleeding. The main portal vein is extrahepatic in ~47% of patients and thus a direct puncture into the main portal vein may result in massive extravasation when angioplasty of the tract is performed.19,20 This is probably the most feared complication during TIPS. Fortunately, this is an uncommon complication, reported to occur in ~0.5% of cases,25 but if it occurs, it may result in a fatal outcome.26,27 The first sign of portal vein perforation is a sudden increase in the patient's heart rate. Angiographically, the portogram demonstrates massive extravasation of contrast into the peritoneal cavity (Fig. 2A). If this complication is encountered, the operator should act rapidly and effectively. The first step is to stabilize the patient by rapidly placing an angioplasty balloon (usually a 10-mm balloon) and inflating it at the perforation site26 (Fig. 2B). The next step is the deployment of a stent, making sure that the perforation site is covered. In some cases, the extravasation is sealed after placement of a bare stent20,27; however, with the current availability of stent grafts, we would recommend primary placement of a stent graft as this maneuver will solve the problem in most cases (Figs. 3A and 3B and Figs. 4A and 4B).28
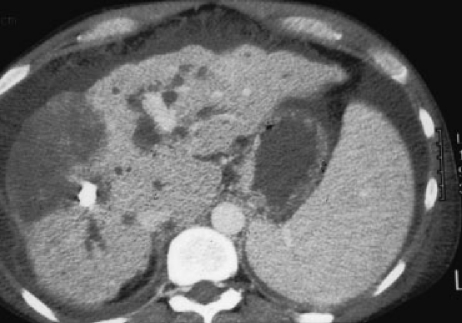
Figure 2.
(A) Portal vein perforation. Direct portogram performed via an angioplasty balloon placed through a transhepatic tract. There is opacification of small esophageal varices. There is a large, irregular area of contrast extravasation consistent with perforation of the portal vein. (B) Control of portal vein perforation. The angioplasty balloon has been inflated at the perforation site to control the periportal extravasation. This maneuver will control the bleeding most of the time. The next step would be the placement of a stent graft. Note the central location of the puncture at the portal bifurcation.
Figure 3.
(A) Portal vein perforation. Direct portogram using a measuring catheter demonstrates opacification of the main portal vein and intrahepatic branches. Small varices are identified. There is an irregular linear image inferior to the border of the liver consistent with free spillage of contrast. Note the central location of the puncture, directly into the main portal vein. (B) Portogram post–stent graft. Direct portogram after placement of a 10 mm × 7 cm VIATORR stent-graft (W.L. Gore, Flagstaff, AZ) demonstrates a patent TIPS and no further extravasation is observed.
Figure 4.
Portal vein perforation. (A) Direct portogram performed through the Rosch-Uchida TIPS sheath (Cook, Bloomington, IN) demonstrates a large area of extravasation in close proximity to the lower aspect of the main portal vein. A very small inferior mesenteric vein is identified. Note the central puncture site within the main portal vein. (B) Portogram after Wallstent placement still demonstrates the site of extravasation. In this case, placement of a bare stent did not control the portal vein leak and the patient required surgical repair of the portal perforation.
The key to preventing this complication is to have a clear understanding of the vascular anatomy of the liver.19,20,29 The best way to avoid this complication is to attempt entry into the right portal vein ~3 cm lateral to the portal bifurcation.30 This segment of the portal vein is intrahepatic over 95% of the time, thereby minimizing the risk of this complication.19,20,29
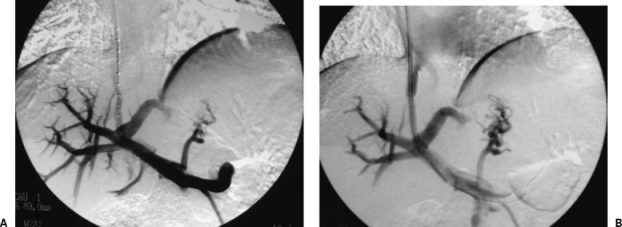
LACERATION OF THE INFERIOR VENA CAVA DURING TRANSCAVAL PUNCTURE
When the hepatic veins cannot be used to create a TIPS, alternative methods can be employed including direct puncture through a hepatic vein stump such as in Budd-Chiari patients31 (Figs. 5A to 5C), direct puncture from the inferior vena cava to portal vein,32 methods such as the “gun-sight” approach,33 or even the use of mesenteric vein access assisted with a minilaparotomy followed by retrograde puncture from portal vein to hepatic veins or inferior vena cava, as described by Rozenblit and colleagues.34 These approaches increase the risk of vena cava laceration or injury and should be performed with extreme caution and careful preprocedural planning, always keeping in mind the anatomic relationship between the inferior vena cava, portal vein, and arterial structures and “free” zones of the liver.19
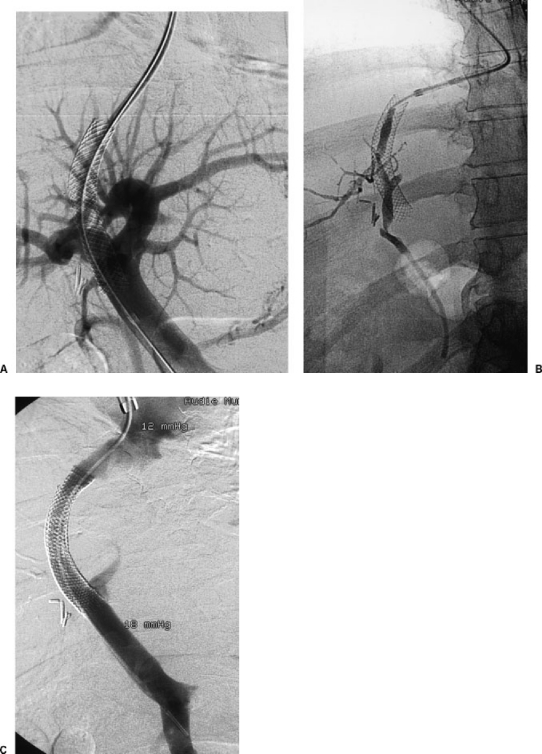
Figure 5.
(A) Inferior vena cavagram in a patient with Budd-Chiari demonstrates compression of the intrahepatic inferior vena cava. There is a small stump in the anticipated anatomic position of the right hepatic vein. (B) A Rosch-Uchida needle has been advanced directly from the hepatic vein stump into the liver parenchyma. Contrast injection demonstrates the spiderweb appearance classic of hepatic vein occlusion in Budd-Chiari. (C) Portogram after creation of the TIPS shows a widely patent shunt. In this case, the direct transhepatic puncture was uneventful and the shunt was created successfully.
HEPATIC ARTERY INJURY
Injuries to the hepatic artery during a TIPS procedure are reported to occur in less than 1% of all TIPS cases.25 Severe hepatic artery injuries may have a fatal outcome.35 It is very important that the operator is aware of the catheter position at all times during a TIPS procedure to identify this complication in a timely fashion to prevent a major mistake with a fatal consequence. First of all, we must be aware that it is not uncommon to puncture the hepatic artery during a TIPS procedure. This is usually an insignificant event during the procedure and usually the operator may ignore it, continue on, and complete the TIPS.20 Significant problems may occur when a catheter is fully advanced into the hepatic artery (Figs. 6A to 6C)35 and may be much worse if a communication is inadvertently created between the hepatic artery and an hepatic vein.36 If the hepatic artery is entered with a catheter or the large TIPS sheath, the recommended maneuver is to slowly withdraw the catheter/sheath combination until the hepatic artery is disengaged and then proceed with tract embolization.37 It is important not to embolize the hepatic artery as this maneuver may cause a large liver infarction (Fig. 7) as the patient is already at risk of developing ischemic liver failure after TIPS.35 Hepatic artery injury may also result in pseudoaneurysm formation, hepatobiliary fistula with consequent hemobilia, or hepatic infarction.
Figure 6.
Hepatic artery injury during TIPS. (A) Radiograph obtained after transhepatic puncture. Advancement of the guide wire shows the guide wire with a course consistent with location within the portal vein. (B) Digital subtraction arteriogram demonstrates the angiographic catheter within the hepatic artery. At this point, the catheter was withdrawn and the tract was embolized. (C) Digital subtraction arteriogram in the same patient demonstrates anatomic variant with complete replacement of the hepatic artery, originating from the superior mesenteric artery.
Figure 7.
Liver infarction post–hepatic artery embolization. A contrast-enhanced computed tomography scan demonstrates a low-density, wedge-shaped area in the right lobe of the liver, consistent with a large liver infarction after hepatic artery embolization. Note moderate dilation of the intrahepatic biliary ducts, irregular liver surface, and moderate amount of ascites.
BILIARY DUCT INJURY
Puncture and opacification of the biliary ducts is common during a TIPS procedure (Fig. 8), but severe bile duct injury is uncommon and reported to be present in less than 1% of cases.25 A large communication between the shunt tract and the biliary system can be associated with fever, sepsis, and shunt stenosis or occlusion.38,39,40 A fistulous communication with the biliary system must be suspected in cases of subacute TIPS occlusion or in cases with midshunt stenosis that do not respond well to repeat angioplasty, requiring frequent revisions. It is relatively difficult to demonstrate a TIPS to biliary fistula, angiographically; however, if the complication is demonstrated, the best approach is to manage the problem with the placement of a stent graft41,42 (Figs. 9A to 9C). The incidence of this complication may decrease significantly now that TIPS are more often created using stent grafts.43 In some cases a biloma may form as a consequence of bile duct injury during TIPS. This may be managed with either percutaneous drainage of the fluid cavity or endoscopic placement of a biliary stent to drain the biliary system.
Figure 8.
Opacification of the common bile duct during a TIPS procedure.
Figure 9.
TIPS to biliary fistula. (A) Direct portogram demonstrates opacification of the main portal vein and intrahepatic portal branches. The shunt is completely occluded. (B) Injection within the occluded stent demonstrates opacification of the common biliary duct and partial opacification of intrahepatic biliary system. (C) Portogram after TIPS revision and placement of a stent graft demonstrates patent shunt with no further demonstration of the biliary fistula.
Complications during Stent Placement
STENT MISPLACEMENT
Early shunt dysfunction is usually related to an underlying technical problem, such as incomplete stent coverage of the parenchymal tract or the presence of a kink along the shunt tract.44,45 Incomplete stent coverage of the transhepatic tract may be related to stent misplacement, stent migration, or stent recoil. Ideally, the stent should have a smooth curve with the portal vein end placed 2 to 4 cm into the portal vein20 and the hepatic vein end extending to the hepatocaval junction,46 being careful not to extend the stent into the right atrium. Until recently, the most common stent used for TIPS creation has been the Wallstent (Boston Scientific, Natick, MA). An advantage with the use of the Wallstent is that the operator has the ability to recapture and reposition it if the initial deployment is inadequate, reducing the risk of misplacement. If stent misplacement occurs such as excessive protrusion of the stent into the portal vein or insufficient stent covering of the transhepatic tract, the key issue is to avoid losing wire access and to place a second stent in tandem to cover the entire tract. Misplacement with stent protrusion into the right atrium may cause atrial perforation and development of an aortoatrial fistula with devastating consequences.47 Probably the best maneuver here is prevention, insisting on very careful stent deployment technique during TIPS. If for any reason the stent ends up protruding into the right atrium, it may be necessary to remove the stent with a loop snare before perforation occurs.48
Early shunt thrombosis caused by stent misplacement resulting in a short or insufficiently stented tract needs to be addressed with an expedited shunt revision.49,50 Stent revision usually requires removal of thrombus with either a mechanical thrombectomy device or pulse-spray thrombolysis. Once the thrombus is removed, the revision is usually completed with placement of an additional stent.49
STENT RECOIL
A disadvantage of the use of the Wallstent for TIPS is that the stent has a tendency to recoil. Stent recoil may make the length of the stent insufficient to maintain shunt patency (Fig. 10). This phenomenon tends to occur more often at the hepatic vein end of the shunt and is very uncommon at the portal vein end of the shunt. When this complication occurs, shunt revision is necessary. Revision requires shunt catheterization, thrombectomy of the occluded stent, and usually, additional stent placement. If access into the shunt cannot be obtained, an option is the creation of a new parallel shunt.49,50
Figure 10.
Stent recoil. Ultrasound image demonstrates stent retraction into the liver parenchyma with insufficient extension into the portal vein. The shunt was occluded and required a TIPS revision with extension of the stent further out into the portal vein.
STENT MIGRATION
Stent migration is a problematic situation. If the stent migrates forward into the portal vein, it is very important not to lose wire access and to attempt placing a second stent in tandem to cover the entire tract with stent material. The real problem comes when the stent migrates centrally. If a guide wire is kept through the stent at all times, the problem is relatively minor, the stent will migrate centrally into the right atrium, and it may be retrieved with a loop snare with relative ease.50,51 However, if for any reason the wire is not kept through the stent at all times, there is a possibility of stent migration into the right ventricle and even into the pulmonary artery, and this is really a distressing complication that needs to be solved immediately as severe hemodynamic complications or perforation of the cardiac chambers may occur.52,53 Several authors have described techniques for Wallstent retrieval during TIPS procedures. The use of snares and large-bore access sheaths is key to the success of migrated stent retrieval.51,54,55,56
Stent migration can also occur if an angioplasty balloon is accidentally caught within the struts of the stent.57 The most dangerous aspect of this complication is that the stent may be dragged back into the right atrium, causing perforation of the right atrium and fistulization to the aorta. This complication may have a fatal outcome.57 The best way to prevent this complication is to make sure that the angioplasty balloon used to dilate a recently placed stent is completely deflated before removal. Continuous extranegative pressure can be applied with a 20- or 30-mL syringe if the operator considers that the angioplasty balloon may have large wings.
Complications after a Successful TIPS
HEMODYNAMIC CHANGES AFTER TIPS
The creation of TIPS causes diversion of the portal flow with preferential flow through the shunt, redirecting blood from the portal circulation to the systemic circulation, and thereby exacerbating the hyperdynamic circulatory state of the cirrhotic.58 Changes that occur after a successful TIPS include significant elevation of the pulmonary artery pressure, right atrial pressure, cardiac index, and pulmonary vascular resistance.58,59 These changes may lead to an acute decompensation post-TIPS in patients with limited cardiac reserve. If this complication occurs, the management is medical with diuretics, high-pressure O2 via a nonrebreather mask, and sedation with morphine at a dose of 4 to 6 mg intravenously. The best way to prevent this complication is to perform a careful patient evaluation before TIPS. If there is a clinical suspicion of right heart failure, a full workup with echocardiography and indirect pressure measurements may be necessary. If right ventricular failure is diagnosed, the patient should not undergo a TIPS procedure.60
LIVER FAILURE AFTER TIPS
The total portal flow diversion caused by a functioning shunt may also result in fulminant liver failure after TIPS.61,62 Most of the flow to the liver is supplied by the portal vein and ~20 to 25% is supplied by the hepatic artery. The hepatic artery buffer response is the physiological response of the hepatic artery to a sudden decrease in portal flow.63 In a normal hepatic artery buffer response, the flow in the hepatic artery increases enough to compensate for the loss of portal flow.63 If the response is insufficient, the patient may develop fulminant liver failure post-TIPS.61 Patients who develop liver failure after TIPS usually present with a significant sudden elevation of the total bilirubin along with a moderate elevation of liver enzymes. If this phenomenon progresses rapidly within the next few days, the outcome may be fatal. In some cases, the derangement in liver function reaches a peak and then slowly drifts down. If severe, this complication may be treated by placing a reducing stent in an effort to decrease the flow through the shunt, and thus, diminish the total portal flow diversion (Figs. 11A and 11B). If placement of a reducing stent is not successful in decreasing the flow through the shunt, it may be necessary to occlude the shunt completely.
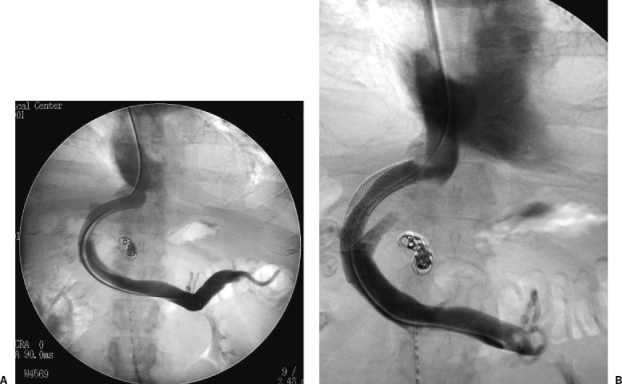
Figure 11.
Liver failure after TIPS. (A) Direct portogram in a patient who underwent a TIPS procedure for the management of refractory ascites. Shortly after TIPS he had a significant elevation of total serum bilirubin and liver enzymes. The patient was not a transplant candidate. Reducing stent placement was requested. (B) A reducing stent was created with a Wallgraft and placed within the patent shunt. The portogram shows successful shunt reduction after reducing stent placement.
ENCEPHALOPATHY
The development of encephalopathy after TIPS is probably the most frequent complication related to the procedure, its incidence ranging between 5 and 35%.64 Most of the time, encephalopathy can be managed medically with a protein-restricted diet, branched-chain amino acids, and the administration of oral lactulose.64 This approach controls 95% of cases of encephalopathy; however, 3 to 7% of these patients show encephalopathy that is refractory to therapy and a more aggressive approach is required.64,65 The options include shunt occlusion,66,67 creation of a reducing stent with a bare stent,68,69 and the creation of a reducing stent using a stent graft.70
Intentional permanent TIPS occlusion with coils or other permanent occluding material has been associated with immediate severe hemodynamic changes such as elevation of portal vein pressure and decrease in cardiac output resulting in hypotension. These hemodynamic changes may result in a fatal outcome and for this reason, this maneuver is preferably avoided.66 Temporary shunt occlusion67 has the advantage of enabling the operator to recanalize the shunt if required. It appears that the placement of a reducing stent is a much more reasonable approach. Forauer and McLean created a reducing stent by deploying a 10 × 42 mm Wallstent within a P-154 Palmaz stent (Johnson & Johnson, Warren, NJ). The constraining stent is then loaded into a 10-F sheath and it is advanced to its final position by using a pusher from a Vena-Tech inferior vena cava filter system (Braun, Evanston, IL). The creation of a reducing stent by using a stent graft was described by Madoff et al and is probably a better option because the regulation of blood flow through the stent graft is slightly more predictable than the regulation of blood flow achieved by the use of a reducing stent created with bare stents.64 These authors deploy the Wallgraft on the back table. A dilator is then used as a template to predetermine the diameter of the reducing stent. A purse-string suture is then woven through the mesh and graft material to create the “waist” in the reducing stent. The trailing two thirds of the graft material are removed to prevent hepatic vein occlusion. The stent graft is then loaded on a new 9-F sheath and deployed within the existing patent shunt. With this technique, Madoff and colleagues reported a 100% technical success and clinical benefit in four out of five patients.64
RADIATION INJURIES
Radiation injuries are uncommon but may occur after a lengthy TIPS.71 The technical difficulties associated with this procedure have been overcome by most operators and now, a standard TIPS takes only ~2 hours with a total of 20 to 35 minutes of total fluoroscopy time employed. Probably the best way to avoid radiation injuries is to follow the basic rules to decrease excessive radiation exposure (i.e., avoiding unnecessary fluoroscopy, not using largely magnified fields for long periods of time, trying to avoid continuous fluoroscopy over the same region, and restricting the area exposed to radiation by using field collimation).
CONCLUSION
The TIPS procedure is considered safe. Major complications may occur but they are uncommon, presenting in ~3 to 5% of patients undergoing the procedure. Operators performing TIPS should be aware of all the potential major complications during this technically difficult interventional procedure.
REFERENCES
- Haskal Z J, Rees C R, Ring E J, Saxon R, Sacks D. Reporting standards for transjugular intrahepatic portosystemic shunts. Technology Assessment Committee of the SCVIR. J Vasc Interv Radiol. 1997;8:289–297. doi: 10.1016/s1051-0443(97)70558-x. [DOI] [PubMed] [Google Scholar]
- Freedman A M, Sanyal A J, Tisnado J, et al. Complications of transjugular intrahepatic portosystemic shunt: a comprehensive review. Radiographics. 1993;13:1185–1210. doi: 10.1148/radiographics.13.6.8290720. [DOI] [PubMed] [Google Scholar]
- Coldwell D M, Ring E J, Rees C R, et al. Multicenter investigation of the role of transjugular intrahepatic portosystemic shunt in management of portal hypertension. Radiology. 1995;196:335–340. doi: 10.1148/radiology.196.2.7617842. [DOI] [PubMed] [Google Scholar]
- Encarnacion C E, Palmaz J C, Rivera F J, et al. Transjugular intrahepatic portosystemic shunt placement for variceal bleeding: predictors of mortality. J Vasc Interv Radiol. 1995;6:687–694. doi: 10.1016/s1051-0443(95)71165-4. [DOI] [PubMed] [Google Scholar]
- Tyburski J G, Noorily M J, Wilson R F. Prognostic factors with the use of the transjugular intrahepatic portosystemic shunt for bleeding varices. Arch Surg. 1997;132:626–630;. doi: 10.1001/archsurg.1997.01430300068014. discussion 630–622. [DOI] [PubMed] [Google Scholar]
- Patch D, Nikolopoulou V, McCormick A, et al. Factors related to early mortality after transjugular intrahepatic portosystemic shunt for failed endoscopic therapy in acute variceal bleeding. J Hepatol. 1998;28:454–460. doi: 10.1016/s0168-8278(98)80320-6. [DOI] [PubMed] [Google Scholar]
- Rajan D K, Haskal Z J, Clark T WI. Serum bilirubin and early mortality after transjugular intrahepatic portosystemic shunts: results of a multivariate analysis. J Vasc Interv Radiol. 2002;13:155–161. doi: 10.1016/s1051-0443(07)61932-0. [DOI] [PubMed] [Google Scholar]
- Helton W S, Belshaw A, Althaus S, Park S, Coldwell D, Johansen K. Critical appraisal of the angiographic portacaval shunt (TIPS) Am J Surg. 1993;165:566–571. doi: 10.1016/s0002-9610(05)80436-2. [DOI] [PubMed] [Google Scholar]
- Banares R, Casado M, Rodriguez-Laiz J M, et al. Urgent transjugular intrahepatic portosystemic shunt for control of acute variceal bleeding. Am J Gastroenterol. 1998;93:75–79. doi: 10.1111/j.1572-0241.1998.075_c.x. [DOI] [PubMed] [Google Scholar]
- Rubin R A, Haskal Z J, O'Brien C, Cope C, Brass C. Transjugular intrahepatic portosystemic shunting: decreased survival for patients with high APACHE II scores. Am J Gastroenterol. 1995;90:556–563. [PubMed] [Google Scholar]
- Chalasani N, Clark W S, Martin L G, et al. Determinants of mortality in patients with advanced cirrhosis after transjugular intrahepatic portosystemic shunting. Gastroenterology. 2000;118:138–144. doi: 10.1016/s0016-5085(00)70422-7. [DOI] [PubMed] [Google Scholar]
- Malinchoc M, Kamath P S, Gordon F D, Peine C J, Rank J, ter Borg P C. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864–871. doi: 10.1053/he.2000.5852. [DOI] [PubMed] [Google Scholar]
- Kamath P S, Wiesner R H, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease [see comments] Hepatology. 2001;33:464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- Angermayr B, Cejna M, Karnel F, et al. Child-Pugh versus MELD score in predicting survival in patients undergoing transjugular intrahepatic portosystemic shunt. Gut. 2003;52:879–885. doi: 10.1136/gut.52.6.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno F, Merli M, Cazzaniga M, et al. MELD score is better than Child-Pugh score in predicting 3-month survival of patients undergoing transjugular intrahepatic portosystemic shunt. J Hepatol. 2002;36:494–500. doi: 10.1016/s0168-8278(01)00309-9. [DOI] [PubMed] [Google Scholar]
- Ferral H, Gamboa P, Postoak D W, et al. Survival after elective transjugular intrahepatic portosystemic shunt creation: prediction with model for end-stage liver disease score. Radiology. 2004;231:231–236. doi: 10.1148/radiol.2311030967. [DOI] [PubMed] [Google Scholar]
- Fitt G, Thomson K, Hennessy O. Delayed fatal cardiac perforation by an indwelling long introducer sheath following transjugular intrahepatic portocaval stents (TIPS) Cardiovasc Intervent Radiol. 1993;16:109–110. doi: 10.1007/BF02602990. [DOI] [PubMed] [Google Scholar]
- Richter G M, Noeldge G, Palmaz J C, et al. Transjugular intrahepatic portacaval stent shunt: preliminary clinical results. Radiology. 1990;174:1027–1030. doi: 10.1148/radiology.174.3.174-3-1027. [DOI] [PubMed] [Google Scholar]
- Uflacker R, Reichert P, D'Albuquerque L C, de Oliveira e Silva A. Liver anatomy applied to the placement of transjugular intrahepatic portosystemic shunts. Radiology. 1994;191:705–712. doi: 10.1148/radiology.191.3.8184050. [DOI] [PubMed] [Google Scholar]
- Saxon R R, Keller F S. Technical aspects of accessing the portal vein during the TIPS procedure. J Vasc Interv Radiol. 1997;8:733–744. doi: 10.1016/s1051-0443(97)70655-9. [DOI] [PubMed] [Google Scholar]
- Rose S C, Behling C, Roberts A C, et al. Main portal vein access in transjugular intrahepatic portosystemic shunt procedures: use of three-dimensional ultrasound to ensure safety. J Vasc Interv Radiol. 2002;13:267–273. doi: 10.1016/s1051-0443(07)61719-9. [DOI] [PubMed] [Google Scholar]
- Richter G M, Noeldge G, Palmaz J C, Roessle M. The transjugular intrahepatic portosystemic stent-shunt (TIPSS): results of a pilot study. Cardiovasc Intervent Radiol. 1990;13:200–207. doi: 10.1007/BF02575474. [DOI] [PubMed] [Google Scholar]
- Semba C P, Saperstein L, Nyman U, Dake M D. Hepatic laceration from wedged venography performed before transjugular intrahepatic portosystemic shunt placement. J Vasc Interv Radiol. 1996;7:143–146. doi: 10.1016/s1051-0443(96)70751-0. [DOI] [PubMed] [Google Scholar]
- Petersen B. Intravascular ultrasound-guided direct intrahepatic portacaval shunt: description of technique and technical refinements. J Vasc Interv Radiol. 2003;14:21–32. [PubMed] [Google Scholar]
- Haskal Z J, Martin L, Cardella J F, et al. Quality improvement guidelines for transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 2001;12:131–136. doi: 10.1016/s1051-0443(07)61817-x. [DOI] [PubMed] [Google Scholar]
- Kim J K, Yun W, Kim J W, Joo Y U, Park J G. Extrahepatic portal vein tear with intraperitoneal hemorrhage during TIPS. Cardiovasc Intervent Radiol. 2001;24:436–437. doi: 10.1007/s00270-001-0051-5. [DOI] [PubMed] [Google Scholar]
- Davis A G, Haskal Z J. Extrahepatic portal vein puncture and intra-abdominal hemorrhage during transjugular intrahepatic portosystemic shunt creation. J Vasc Interv Radiol. 1996;7:863–866. doi: 10.1016/s1051-0443(96)70863-1. [DOI] [PubMed] [Google Scholar]
- Owen R J, Rose J D. Endovascular treatment of a portal vein tear during TIPSS. Cardiovasc Intervent Radiol. 2000;23:230–232. doi: 10.1007/s002700010050. [DOI] [PubMed] [Google Scholar]
- Schultz S R, LaBerge J M, Gordon R L, Warren R S. Anatomy of the portal vein bifurcation: intra- versus extrahepatic location: implications for transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 1994;5:457–459. doi: 10.1016/s1051-0443(94)71529-3. [DOI] [PubMed] [Google Scholar]
- Saxon R S, Ross P L, Mendel-Hartvig J, et al. Transjugular intrahepatic portosystemic shunt patency and the importance of stenosis location in the development of recurrent symptoms. Radiology. 1998;207:683–693. doi: 10.1148/radiology.207.3.9609891. [DOI] [PubMed] [Google Scholar]
- Peltzer M Y, Ring E J, LaBerge J M, Haskal Z J, Radosevich P M, Gordon R L. Treatment of Budd-Chiari syndrome with a transjugular intrahepatic portosystemic shunt. J Vasc Interv Radiol. 1993;4:263–267. doi: 10.1016/s1051-0443(93)71849-7. [DOI] [PubMed] [Google Scholar]
- Soares G M, Murphy T P. Transcaval TIPS: indications and anatomic considerations. J Vasc Interv Radiol. 1999;10:1233–1238. doi: 10.1016/s1051-0443(99)70224-1. [DOI] [PubMed] [Google Scholar]
- Haskal Z J, Duszak R, Jr, Furth E E. Transjugular intrahepatic transcaval portosystemic shunt: the gun-sight approach. J Vasc Interv Radiol. 1996;7:139–142. doi: 10.1016/s1051-0443(96)70750-9. [DOI] [PubMed] [Google Scholar]
- Rozenblit G, DelGuercio L R, Savino J A, et al. Transmesenteric-transfemoral method of intrahepatic portosystemic shunt placement with minilaparotomy. J Vasc Interv Radiol. 1996;7:499–506. doi: 10.1016/s1051-0443(96)70790-x. [DOI] [PubMed] [Google Scholar]
- Haskal Z J, Pentecost M J, Rubin R A. Hepatic arterial injury after transjugular intrahepatic portosystemic shunt placement: report of two cases. Radiology. 1993;188:85–88. doi: 10.1148/radiology.188.1.8511322. [DOI] [PubMed] [Google Scholar]
- Pattynama P M, Hoek B van, Kool L J. Inadvertent arteriovenous stenting during transjugular intrahepatic portosystemic shunt procedure and the importance of hepatic artery perfusion. Cardiovasc Intervent Radiol. 1995;18:192–195. doi: 10.1007/BF00204150. [DOI] [PubMed] [Google Scholar]
- Kerlan R K, Jr, LaBerge J M, Gordon R L, Ring E J. Inadvertent catheterization of the hepatic artery during placement of transjugular intrahepatic portosystemic shunts. Radiology. 1994;193:273–276. doi: 10.1148/radiology.193.1.8090907. [DOI] [PubMed] [Google Scholar]
- Mallery S, Freeman M L, Peine C J, Miller R P, Stanchfield W R. Biliary-shunt fistula following transjugular intrahepatic portosystemic shunt placement. Gastroenterology. 1996;111:1353–1357. doi: 10.1053/gast.1996.v111.pm8898650. [DOI] [PubMed] [Google Scholar]
- Jawaid Q, Saeed Z A, Di Bisceglie A M, et al. Biliary-venous fistula complicating transjugular intrahepatic portosystemic shunt presenting with recurrent bacteremia, jaundice, anemia and fever. Am J Transplant. 2003;3:1604–1607. doi: 10.1046/j.1600-6135.2003.00267.x. [DOI] [PubMed] [Google Scholar]
- Saxon R R, Mendel-Hartvig J, Corless C L, et al. Bile duct injury as a major cause of stenosis and occlusion in transjugular intrahepatic portosystemic shunts: comparative histopathologic analysis in humans and swine. J Vasc Interv Radiol. 1996;7:487–497. doi: 10.1016/s1051-0443(96)70789-3. [DOI] [PubMed] [Google Scholar]
- Cohen G S, Young H Y, Ball D S. Stent-graft as treatment for TIPS-biliary fistula. J Vasc Interv Radiol. 1996;7:665–668. doi: 10.1016/s1051-0443(96)70825-4. [DOI] [PubMed] [Google Scholar]
- Boyvat F, Cekirge S, Balkanci F, Besim A. Treatment of a TIPS-biliary fistula by stent-graft in a 9-year-old boy. Cardiovasc Intervent Radiol. 1999;22:67–68. doi: 10.1007/s002709900331. [DOI] [PubMed] [Google Scholar]
- Saxon R R. A new era for transjugular intrahepatic portosystemic shunts? J Vasc Interv Radiol. 2004;15:217–219. doi: 10.1097/01.rvi.0000116862.34422.a5. [DOI] [PubMed] [Google Scholar]
- Darcy M D, Vesely T M, Picus D, Middleton W D, Hicks M E. Percutaneous revision of an acutely thrombosed transjugular intrahepatic portosystemic shunt. J Vasc Interv Radiol. 1992;3:77–80. doi: 10.1016/s1051-0443(92)72191-5. discussion 81–72. [DOI] [PubMed] [Google Scholar]
- Hausegger K A, Sternthal H M, Klein G E, Karaic R, Stauber R, Zenker G. Transjugular intrahepatic portosystemic shunt: angiographic follow-up and secondary interventions. Radiology. 1994;191:177–181. doi: 10.1148/radiology.191.1.8134566. [DOI] [PubMed] [Google Scholar]
- Clark T W, Agarwal R, Haskal Z J, Stavropoulos S W. The effect of initial shunt outflow position on patency of transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 2004;15:147–152. doi: 10.1097/01.rvi.0000109401.52762.56. [DOI] [PubMed] [Google Scholar]
- Sehgal M, Brown D B, Picus D. Aortoatrial fistula complicating transjugular intrahepatic portosystemic shunt by protrusion of a stent into the right atrium: radiologic/pathologic correlation. J Vasc Interv Radiol. 2002;13:409–412. doi: 10.1016/s1051-0443(07)61745-x. [DOI] [PubMed] [Google Scholar]
- Slonim S M, Dake M D, Razavi M K, et al. Management of misplaced or migrated endovascular stents. J Vasc Interv Radiol. 1999;10:851–859. doi: 10.1016/s1051-0443(99)70127-2. [DOI] [PubMed] [Google Scholar]
- Ferral H, Banks B, Wholey M, Nazarian G K, Bjarnason H, Castaneda-Zuniga W R. Techniques for transjugular intrahepatic portosystemic shunt revision. AJR Am J Roentgenol. 1998;171:1041–1047. doi: 10.2214/ajr.171.4.9762993. [DOI] [PubMed] [Google Scholar]
- Sterling K M, Darcy M D. Stenosis of transjugular intrahepatic portosystemic shunts: presentation and management. AJR Am J Roentgenol. 1997;168:239–244. doi: 10.2214/ajr.168.1.8976952. [DOI] [PubMed] [Google Scholar]
- Cekirge S, Foster R G, Weiss J P, McLean G K. Percutaneous removal of an embolized Wallstent during a transjugular intrahepatic portosystemic shunt procedure. J Vasc Interv Radiol. 1993;4:559–560. doi: 10.1016/s1051-0443(93)71921-1. [DOI] [PubMed] [Google Scholar]
- Linka A Z, Jenni R. Migration of intrahepatic portosystemic stent into right ventricle: an unusual cause of tricuspid regurgitation. Circulation. 2001;103:161–162. doi: 10.1161/01.cir.103.1.161. [DOI] [PubMed] [Google Scholar]
- Rumi M N, Schumann R, Freeman R B, Rohrer R J, Fairchild R B. Acute transjugular intrahepatic portosystemic shunt migration into pulmonary artery during liver transplantation. Transplantation. 1999;67:1492–1494. doi: 10.1097/00007890-199906150-00020. [DOI] [PubMed] [Google Scholar]
- Cohen G S, Ball D S. Delayed Wallstent migration after a transjugular intrahepatic portosystemic shunt procedure: relocation with a loop snare. J Vasc Interv Radiol. 1993;4:561–563. doi: 10.1016/s1051-0443(93)71922-3. [DOI] [PubMed] [Google Scholar]
- Hartnell G G, Crenshaw W B, Burger A J, Hamer A W. Percutaneous removal of a fully expanded Wallstent from the right ventricle with transesophageal echocardiography guidance. J Vasc Interv Radiol. 1996;7:371–374. doi: 10.1016/s1051-0443(96)72869-5. [DOI] [PubMed] [Google Scholar]
- Lipton M, Cynamon J, Bakal C W, Sprayregen S. Percutaneous retrieval of two Wallstent endoprostheses from the heart through a single jugular sheath. J Vasc Interv Radiol. 1995;6:469–472. doi: 10.1016/s1051-0443(95)72844-5. [DOI] [PubMed] [Google Scholar]
- Prahlow J A, O'Bryant T J, Barnard J J. Cardiac perforation due to Wallstent embolization: a fatal complication of the transjugular intrahepatic portosystemic shunt procedure. Radiology. 1997;205:170–172. doi: 10.1148/radiology.205.1.9314980. [DOI] [PubMed] [Google Scholar]
- Azoulay D, Castaing D, Dennison A, Martino W, Eyraud D, Bismuth H. Transjugular intrahepatic portosystemic shunt worsens the hyperdynamic circulatory state of the cirrhotic patient: preliminary report of a prospective study. Hepatology. 1994;19:129–132. [PubMed] [Google Scholar]
- der Linden P Van, Le Moine O, Ghysels M, Ortinez M, Deviere J. Pulmonary hypertension after transjugular intrahepatic portosystemic shunt: effects on right ventricular function. Hepatology. 1996;23:982–987. doi: 10.1053/jhep.1996.v23.pm0008621179. [DOI] [PubMed] [Google Scholar]
- Kerlan R K, Jr, LaBerge J M, Gordon R L, Ring E J. Transjugular intrahepatic portosystemic shunts: current status. AJR Am J Roentgenol. 1995;164:1059–1066. doi: 10.2214/ajr.164.5.7717204. [DOI] [PubMed] [Google Scholar]
- Walser E, Ozkan O S, Raza S, Soloway R, Gajula L. Hepatic perfusion as a predictor of mortality after transjugular intrahepatic portosystemic shunt creation in patients with refractory ascites. J Vasc Interv Radiol. 2003;14:1251–1257. doi: 10.1097/01.rvi.0000092665.72261.b0. [DOI] [PubMed] [Google Scholar]
- Walser E M, DeLa Pena R, Villanueva-Meyer J, Ozkan O, Soloway R. Hepatic perfusion before and after the transjugular intrahepatic portosystemic shunt procedure: impact on survival. J Vasc Interv Radiol. 2000;11:913–918. doi: 10.1016/s1051-0443(07)61811-9. [DOI] [PubMed] [Google Scholar]
- Zipprich A, Steudel N, Behrmann C, et al. Functional significance of hepatic arterial flow reserve in patients with cirrhosis. Hepatology. 2003;37:385–392. doi: 10.1053/jhep.2003.50065. [DOI] [PubMed] [Google Scholar]
- Madoff D C, Wallace M J, Ahrar K, Saxon R R. TIPS-related hepatic encephalopathy: management options with novel endovascular techniques. Radiographics. 2004;24:21–36. doi: 10.1148/rg.241035028. discussion 36–37. [DOI] [PubMed] [Google Scholar]
- Forauer A R, McLean G K. Transjugular intrahepatic portosystemic shunt constraining stent for the treatment of refractory postprocedural encephalopathy: a simple design utilizing a Palmaz stent and Wallstent. J Vasc Interv Radiol. 1998;9:443–446. doi: 10.1016/s1051-0443(98)70296-9. [DOI] [PubMed] [Google Scholar]
- Paz-Fumagalli R, Crain M R, Mewissen M W, Varma R R. Fatal hemodynamic consequences of therapeutic closure of a transjugular intrahepatic portosystemic shunt. J Vasc Interv Radiol. 1994;5:831–834. doi: 10.1016/s1051-0443(94)71616-x. [DOI] [PubMed] [Google Scholar]
- Kerlan R K, Jr, LaBerge J M, Baker E L, et al. Successful reversal of hepatic encephalopathy with intentional occlusion of transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 1995;6:917–921. doi: 10.1016/s1051-0443(95)71212-x. [DOI] [PubMed] [Google Scholar]
- Haskal Z J, Middlebrook M R. Creation of a stenotic stent to reduce flow through a transjugular intrahepatic portosystemic shunt. J Vasc Interv Radiol. 1994;5:827–829. doi: 10.1016/s1051-0443(94)71614-6. discussion 829–830. [DOI] [PubMed] [Google Scholar]
- Hauenstein K H, Haag K, Ochs A, Langer M, Rossle M. The reducing stent: treatment for transjugular intrahepatic portosystemic shunt-induced refractory hepatic encephalopathy and liver failure. Radiology. 1995;194:175–179. doi: 10.1148/radiology.194.1.7997547. [DOI] [PubMed] [Google Scholar]
- Madoff D C, Perez-Young I V, Wallace M J, Skolkin M D, Toombs B D. Management of TIPS-related refractory hepatic encephalopathy with reduced Wallgraft endoprostheses. J Vasc Interv Radiol. 2003;14:369–374. doi: 10.1097/01.rvi.0000058418.01661.48. [DOI] [PubMed] [Google Scholar]
- Knautz M A, Abele D C, Reynolds T L. Radiodermatitis after transjugular intrahepatic portosystemic shunt. South Med J. 1997;90:352–356. doi: 10.1097/00007611-199703000-00020. [DOI] [PubMed] [Google Scholar]