ABSTRACT
The current trend among interventional radiologists is to be actively involved in the pre- and post-procedure care that surrounds many of our procedures. For this to occur, defined office space that is set up in such a way that is conducive to outpatient consultation and post-procedure visits is required. In addition, appropriate support staff such as midlevel providers (including nurse practitioners and physician assistants) and a receptionist are needed to make the entire system work. Finally, dedicated time to focus on direct patient care is mandatory. Equally important is understanding the processes that occur in the background of a typical procedural encounter, including generating referrals, obtaining insurance pre-authorization, managing medical records, and communicating with referring physicians, all of which are expected to take place when managing patients in an outpatient setting. When these components are in place, it becomes possible for an interventionalist to successfully develop an outpatient office and to meet the expectation that patients will be seen before and after procedures by the practitioner performing that procedure.
Keywords: Outpatient medical practice, interventional radiology, midlevel providers
For all procedural specialists, the preprocedural and postprocedural outpatient office visit is a mandatory component any episode of care. It would be difficult for us to imagine a surgeon meeting a patient for the first time as they were being wheeled into the operating room for an elective procedure. For today's interventional radiologist, it has become equally difficult to imagine meeting a patient for the first time as they are being prepared for a procedure in the angio suite.
Preprocedural consultations are, of course, an integral part of the relationship between a procedural specialist and his or her patient. Having the opportunity to speak to a patient to understand their presenting complaints, their past medical and surgical history, the results of all prior diagnostic testing, and their expectations of a procedure you can offer them cannot be replaced by reviewing paperwork or with a quick conversation on the day of a procedure. It is normal for a patient to be nervous on the day of a procedure and, in general, most patients are more relaxed and levelheaded during a consultation taking place days or weeks before a planned procedure. This gives the physician the opportunity to learn about the patient and the opportunity for the patient to learn about the physician and the procedure(s) being offered by the physician. This two-way dialogue has the potential to put everybody at ease and to allow appropriate recommendations to be made and appropriate expectations to be developed.
Postprocedural office visits are equally important after an interventional procedure. These visits clearly demonstrate to both patients and referring physicians that a procedural specialist is assuming complete responsibility for a patient following an invasive procedure. It is simply unacceptable for an interventional radiologist to expect another physician to have the same degree of knowledge about procedures they perform and what is and is not normally expected after these procedures. Nobody is better suited to evaluate a patient after an interventional procedure than an interventionalist, and the trend of interventional radiologists seeing patients after their procedures is good for both patients and physicians.
THE OUTPATIENT OFFICE
A clinic or dedicated office space is the most important component of any effort to see patients in an outpatient setting before and after they undergo an interventional procedure. Unfortunately, this type of dedicated physical space is not always readily available in the context of a freestanding radiology practice or in-hospital radiology department. Therefore, interventionalists either need to find space that already has or can accommodate individual consultation and examination rooms and a reception area (with a waiting room and space to check in and check out patients). Sometimes this space may be available within an existing imaging center or radiology department and other times, separate space may need to be shared with another medical practice or rented as a stand-alone interventional outpatient clinic.
An outpatient office goes beyond the physical space that it occupies. The support staff employed within the context of an outpatient office is critical to its overall success.1 Nurse practitioners (NPs) and physician's assistants (PAs) have been growing in popularity as they become hired by many interventional practices to support a clinical practice. These providers practice under a collaborating or supervising physician, and although the physical presence of that physician is not always necessary, a means of consulting with the physician must be in place.2 Ultimately, the clinical privileges for these providers are determined by the supervising physician, the institution, state law, and Medicare regulations, all of which may, in fact, contain differences in what the different types of providers are able to do.3 It is therefore important to fully understand these regulations and the rules of third-party payers to know how an NP or PA can benefit and participate in a clinical interventional radiology practice. Our own experience and the experience of others makes it clear that their background makes them extremely well suited for both establishing and participating in a clinic designed to follow patients before and after interventional procedures.
In addition to NPs and PAs, the receptionist is also an important part of the team of people running an outpatient clinical office. This is because the receptionist is often the point of contact between patients and the physicians within an office. A successful receptionist is efficient and professional and shows concern to the patients seen within that office. In addition, they should not be viewed as a barrier between the patient and physician, which is why a receptionist must have a strategy as to how to handle family member questions, test result requests, and so on with compassion and respect.1 The office receptionist is also responsible for scheduling appointments for patients in a manner that works for both the patients and the physicians. Although it is virtually impossible to eliminate patient waiting (because the exact amount of time each patient will require during the course of their individual visit is never known with certainty), sensitivity to the issue of patient waiting time can ultimately benefit a practice as patients experiencing reasonable wait times that are handled well have a positive perception of and often return to that practice.4 Therefore, working with a receptionist who understands this can go a long way to optimizing patient satisfaction as it concerns the operation of an outpatient office.3
THE OUTPATIENT OFFICE VISIT
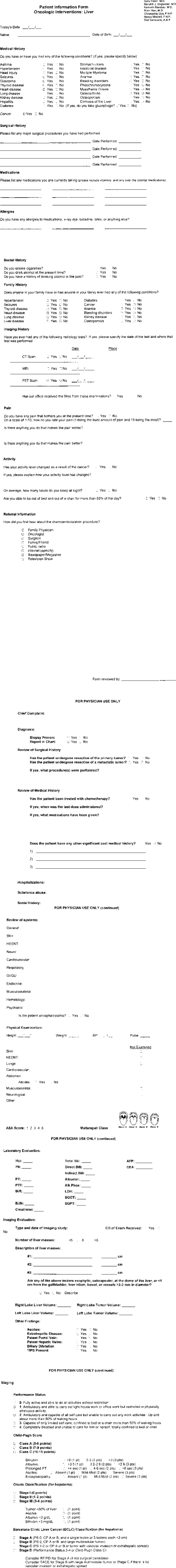
When a patient is initially seen in our office, the visit is not dissimilar to a visit to any procedural specialist. A history is obtained that, although thorough, is clearly directed toward the patient's presenting problem and other issues that may have an impact on that presenting problem. Patients visiting our office fill out a detailed history sheet that has been designed with particular procedures in mind (e.g., uterine artery embolization, saphenous vein ablation, chemoembolization/radiofrequency ablation, and so on) (Fig. 1). Once the patient has completed that form, a physician or NP reviews it with them, elaborating on the historical issues raised by the patient. A directed physical examination is performed as well, with particular attention paid to those components of the physical examination that relate to the patient's primary problem.
Figure 1.
Example of a standard form used by patients and physicians.
There is no doubt that the vast majority of the time we spend with most of our patients is spent counseling them on their treatment options and on the relative risks and benefits of the procedure(s) that we and others can potentially perform to address their presenting complaint. It is important that a patient leaves your office with their questions answered. It is no secret that the complaints that most patients have about the care offered by today's physicians revolve around the lack of time and apparent lack of attention by the physician during their initial and subsequent visits. Time constraints often limit the ability of any physician to fully answer every question raised by a patient in a manner that most patients would find acceptable. Interventional radiologists are, of course, under similar time constraints. The difference is that this type of clinical care is new to many interventional radiologists, and as a result, many interventionalists approach these office visits and their time spent in clinics enthusiastically. If perceived by the patient, this enthusiasm can lead to a very successful office visit and improve the perception that a patient will have regarding their time spent with you. Whether or not you actually have the time to spend answering a patient's questions, it is critical that you make an attempt to answer these questions at the time of consultation or at least provide another means of having them answered, such as an informative website or direct e-mail to you or your office staff.
REFERRALS
It is important to be familiar with and to understand the route that a particular patient came from to make an appointment to see you in your outpatient office. In today's managed care environment, most patients have to be referred for consultations if they wish for it to be a covered service under their personal health insurance. That said, the manner in which that referral is obtained is often information that is worth knowing. A patient who is referred to a specialist by their primary care provider and is then subsequently referred to your office by that specialist is different than patients who learns about your services on their own and then actively seeks a referral to see you from their primary care provider. Still different is the patient who is referred directly from their primary care provider for a service that you offer. It is this path taken by an individual patient that often sets the tone for the conversations that take place during the consultation.
Patients who have sought out an interventional radiologist to learn more about procedures that may or may not relate to their presenting problem often come to a consultation enthusiastically seeking information and/or to clarify information they have obtained on their own from the Internet or other sources. As a result, these are well-informed patients who arrive at your office expecting to leave educated as they prepare to be treated. These consultations are oftentimes demanding as these patients and their families often have many questions. However, it has always been our opinion that well-thought-out questions coming from an informed patient leads to the opportunity to have good two-way dialogue that allows our physicians and NPs to learn more about the patient. This type of discussion almost universally leads to satisfying experiences for both patients and providers. It has been our experience that these patients commonly arrive for their consultation with the expectation that they will pursue the therapy that you may offer, and therefore, the consultations frequently translate into both procedures and continuing care.
As both interventional radiologists and the procedures offered by interventional radiologists become better known in the medical community, patients are getting referred for our services without necessarily knowing anything about them prior to their consultation. These patients are very different from the previously described patients. Either their primary care physician or a specialist has evaluated these patients, and these physicians have determined that the services offered by interventional radiology may have a role in the care of this patient. These patients were seeking care from one physician who has subsequently referred them to another physician. In general, these patients are less informed about interventional radiology procedures and have made an appointment with you because “their doctor told them to.” These patients are both easier and harder to talk to. They are easier because they have fewer questions and fewer expectations regarding the information they expect to hear. They are harder because they oftentimes require more education about their care and about the procedures you can potentially offer them. Because this is often the first time that these patients are hearing about the treatment options we can offer them, they need time to think about the information provided to them. This ultimately requires a mechanism within your outpatient office to follow up with these patients if they do not call back themselves to arrange further care with you.
PHYSICIAN-TO-PHYSICIAN COMMUNICATION
Whether or not a patient arrives in your office after obtaining a referral from a physician (primary care or specialist) or at their own insistence from their primary care provider, it is still critical for you as a treating specialist to identify the patient's primary care provider. Our practice has enthusiastically taken on the responsibilities inherent in managing the preprocedural, intraprocedural, and postprocedural care associated with the treatment options we offer our patients. That said, we still want to identify the physician who is responsible for the overall care of the patient for communication purposes. Our role as a procedural specialist is to manage the entire episode of care surrounding performance of our procedures while still working under the overall plan of care established by the patient's primary care physician (or the physician referring the patient to the interventionalist). Therefore, it is the responsibility of the interventionalist in this setting to communicate with the patient's primary care physician to convey the results of the assessment and treatment plan developed based on that assessment. In addition, a primary care provider needs to know when their patient undergoes the procedure and should be informed about the outcome of that procedure. Finally, your assessment at the time of each postprocedural visit must be conveyed to the primary care provider as well so he or she can participate in the follow-up process because at some point, patients will no longer need to be seen by your office.
Communication most commonly consists of a letter sent to the physician who was actually responsible for referring the patient to your office for the consultation. In addition, copies of this letter should be sent to the patient's primary care provider and consideration should be given to sending a copy to the patient themselves if appropriate. These letters become part of the patient's record at each physician's office, and when the patient sees any of these physicians in the future, that physician will be aware of the care he or she received by your practice. Although there is no replacement for an actual letter that can become part of the patient's chart at that physician's office, it is also valuable to speak directly with the referring physician so he or she can have the opportunity to have their questions about our service answered.
Physician-to-physician communication can potentially have more of a role than just serving the needs of the patients you treat. It can also serve both directly and indirectly as a marketing tool for an interventional practice. Physicians who are successful in marketing their services understand the need to take advantage of every opportunity they have to let other physicians know about the services they offer and how these services can potentially play a role in the care of their patients. Every time a referring physician receives a letter from you or your practice, the knowledge that you perform that particular service gets reinforced, which can only help when another patient sees that physician for a similar problem. In addition, as a referring physician gains more of an understanding of your practice, opportunities to either place brochures in that office or give a lunch-and-learn presentation to that physician and his or her staff will become available.
ORDERING TESTS AND ARRANGING PROCEDURES
Once a patient has been seen in your office and a decision has been made regarding the appropriateness of a particular procedure to address that patient's presenting complaint, the procedure and appropriate preoperative testing need to be arranged. Your practice staff should arrange this. One question frequently raised by radiologists is whether or not they are able to actually order diagnostic tests or therapeutic procedures. This responsibility typically lies with a “treating” physician, who is a physician, as defined by §1861(r) of the Social Security Act, who furnishes a consultation or treats a beneficiary for a specific medical problem and who uses the results of a diagnostic test in the management of the beneficiary's specific medical problem. This rule specifically states that a radiologist performing a therapeutic interventional procedure is considered a treating physician. Therefore, an interventional radiologist seeing a patient in consultation is able to order the appropriate testing required in association with a procedure they are to perform if they will be using the results of the diagnostic test in the management of the patient's specific medical problem.
With that in mind, it is important to recognize that radiologists do not typically assume this responsibility. Historically, the burden of ordering diagnostic tests and arranging therapeutic procedures has fallen upon the physicians referring these patients to an interventional radiologist. If interventionalists are going to continue assuming more a role in direct patient care, then they must be prepared to evaluate the patients they are seeing and determine if additional diagnostic testing is required prior to performance of a procedure (Table 1). In addition, it isn't enough to simply order these tests. By taking on the title of “ordering physician,” interventionalists are now taking on the responsibility of evaluating the results of these tests. In fact, this involves more than just evaluating the results. The ordering physician is equally responsible for acting upon the results of these tests, especially if these tests reveal something unanticipated. All of these responsibilities create a large amount of work that must be managed by a competent office staff devoted to the outpatient office. Staff skilled in arranging laboratory work, ordering diagnostic tests, arranging admissions to an inpatient or observation service, and scheduling interventional procedures is often not found in typical radiology practices but must be part of an outpatient office supporting the work of an interventional radiologist.
Table 1.
Routine Preprocedural and Postprocedural Tests and Follow-up
| Procedure | Preprocedural Visit | Routine Postprocedural Visits |
|---|---|---|
| TIPS, transjugular intrahepatic portosystemic shunt; MRI, magnetic resonance imaging; CT, computed tomography; RFA, radiofrequency ablation; PVR, pulse volume recording; MRA, magnetic resonance angiography; CTA, computed tomography angiography. | ||
| Uterine fibroid embolization | Pre- and postcontrast MRI | 2 wk; 6 mo (pre- and postcontrast MRI) |
| Radiofrequency ablation, chemoembolization, and radioembolization (Y-90 microspheres) | Pre- and postcontrast CT scan with an ultrasound for RFA patients | 1 mo and then every 3 mo (pre- and postcontrast CT scan performed at each visit) |
| Kyphoplasty and vertebroplasty | Plain films, MRI spine | 1 mo |
| Saphenous vein ablation | Lower extremity ultrasound | 1 mo (lower extremity ultrasound) |
| Lower extremity arterial stents | PVR, MRA | 1 mo, 4 mo, and then every 6 mo (PVR at each visit) |
| Renal artery stents | CTA or MRA | 1 mo and then every 6 mo (ultrasound at each visit) |
| TIPS | Ultrasound and CT | 2 wk followed by every 3 mo for 1 y and then every 6 mo (ultrasound at each visit) |
Another critical responsibility of the staff supporting the work coming out of an interventional clinic is the obtaining of preauthorization or preapproval from medical insurance companies. Although referring physicians have always had this responsibility, it is simply not reasonable to expect another physician to do all of the paperwork that is necessary for an interventionalist to perform a procedure. As the treating physician ordering diagnostic tests and therapeutic procedures to treat a patient, these tasks must become the responsibility of the interventionalist. No other physician understands interventional procedures better than an interventionalist, and if questions come up during the preapproval process, nobody is more qualified to answer them then the interventionalist. Initially, this is an extremely time-consuming process for both the physicians and support staff, but in time, this does become more efficient as the steps involved are often repetitive and similar for most insurance companies.
FOLLOW-UP OFFICE VISITS
It is the responsibility of any procedural specialist to follow patients themselves after a procedure is performed. This is surely an expectation of the patient and is becoming an expectation of those physicians referring their patients to an interventional radiologist. There is a tangible amount of reassurance that patients receive from follow-up visits after a procedure is performed. It is normal for any patient to want to review the outcome of a procedure that is performed on them, and oftentimes, the immediate postprocedural period is not the best time to have these discussions due to the lingering effects of sedation and anxiety that often surrounds these procedures. That is why discussing the outcome of a procedure is often best accomplished in an outpatient office setting several days after the procedure has been performed. It is certainly possible for the referring physician to review the outcome with the patient. However, interventionalists understand the potential issues surrounding their procedures and are therefore in the best position to answer the questions that normally arise after our procedures and to assure the patient that there was a good outcome or to explain to the patient why the outcome did not meet expectations.
Communication is also an integral part of a follow-up office visit. Oftentimes, patients are referred to interventional radiologists by specialists and not necessarily by their primary care providers. Communication after a follow-up visit, either in the form of a letter, e-mail, or phone call, will serve to keep these physicians informed about the care of their patients but will also make them aware of your desire and ability to provide longitudinal follow-up care for your patients.
CONCLUSION
There is little doubt that longitudinal, outpatient care of patients undergoing endovascular and other minimally invasive procedures will be required for an interventional practice to consider themselves successful in the future. It is just as clear that significant time, staff, and resources are required to establish an outpatient office designed to provide effective patient care. In doing so, interventional radiologists will be sending a message out to the medical community at large that they are committed to providing the care that meets and quite possibly exceeds the standards that are in place within other procedural specialties. Ultimately, this will help gain the confidence of both patients and referring physicians and secure a place for interventional radiologists as experts in the field of minimally invasive, percutaneous therapy.
REFERENCES
- Nye L G. Office staff savvy: quality staff-patient communications as a loss prevention strategy. J Med Pract Manage. 2001;17:21–24. [PubMed] [Google Scholar]
- Davis A, Powe M L. Physician assistants: scope of practice, regulation and reimbursement. J Med Pract Manage. 2002;18:81–85. [PubMed] [Google Scholar]
- Siskin G P, Bagla S, Sansivero G E, Mitchell N L. The interventional radiology clinic: key ingredients for success. J Vasc Interv Radiol. 2004;15:681–688. doi: 10.1097/01.rvi.0000133504.70799.21. [DOI] [PubMed] [Google Scholar]
- Blender R, Maxey C. Are your patients patiently waiting? What to do about patient wait times. J Med Pract Manage. 2000;16:66–69. [PubMed] [Google Scholar]