The algorithm for patients with renal insufficiency who require vascular imaging has recently changed in my hospital. Previously, the majority of these patients underwent magnetic resonance angiography (MRA) or occasionally computed tomographic angiography after prescan hydration and sodium bicarbonate infusion. Although we have used carbon dioxide (CO2) for many years, with the advent of nephrogenic systemic sclerosis and its unclear relationship to MRA contrast agents, we are increasingly using CO2 as a contrast agent for both diagnosis and to guide therapy. CO2 has been used for > 30 years. It is not nephrotoxic or hepatotoxic and is nonallergenic. It is also quite inexpensive compared with other contrast agents.
PROCEDURE
Equipment
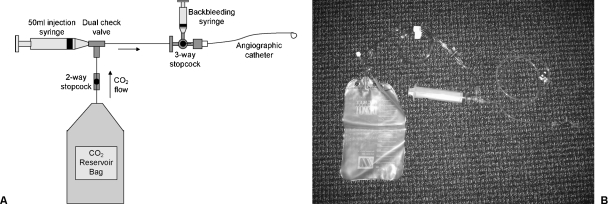
I use a modified plastic bag system with an O-ring first described by Hawkins and associates. A prepackaged carbon dioxide kit (called a “custom waste management kit” from Merit Medical, South Jordan, UT) is available. A similar kit is manufactured by AngioDynamics (Queensbury, NY). Because CO2 angiography is “off-label,” neither can be marketed as a “CO2 angiography” kit, and both cost approximately $50 to 100. Although very straightforward, it is important to understand the connections of this system thoroughly (Fig. 1). The kit includes the following:
Figure 1.
Carbon dioxide delivery system. (A) Illustration depicts connections in closed bag system. (B) Photograph of closed bag system.
1500-mL CO2 bag
50-mL syringe
Multiple stopcocks and connectors
Medical-grade CO2 cylinder
Filling Reservoir Bag
The bag is purged three times using an O-ring filter with medical grade CO2 to eliminate room air. On the final filling, the bag should not be overdistended.
Connection to Catheter
The filled bag is connected to the remaining manifold and the two-way stopcock is opened. The 50-mL syringe is filled with CO2 via a dual check valve and expelled to purge air out of the tubing, which is then connected to the angiographic catheter. The three-way stopcock can be turned off to CO2 to allow backbleeding into a small syringe to eliminate all air from the system. The stopcock is then closed to the backbleeding syringe, and the blood is gently purged from the catheter by slowly injecting CO2 via the syringe. When injecting CO2, resistance is initially felt as blood is purged from the catheter followed by a “give” when CO2 completely fills the catheter. Blood is purged from the catheter to prevent “explosive” delivery of CO2 during angiography.
Angiography
Angiographic runs are then performed at two to six frames per second using digital subtraction software with angiographic inversion and image summation, or “stacking.” Typically 30 to 50 mL of CO2 are injected into the aorta or inferior vena cava via a pigtail catheter. Less volume is used for selective injections, and it is helpful to use catheters with one side hole. Injections are performed 2 to 3 minutes apart; occasionally slightly longer delays are used when performing mesenteric angiography. Patients should be supine, and injections must be made below the level of the diaphragm. For evaluation of the calves and feet, the legs can be elevated slightly on pillows to allow the gas to “rise” to fill the arteries in this region. Nitroglycerine in 100- to 200-μg aliquots can be administered intra-arterially as necessary.
Interpretation
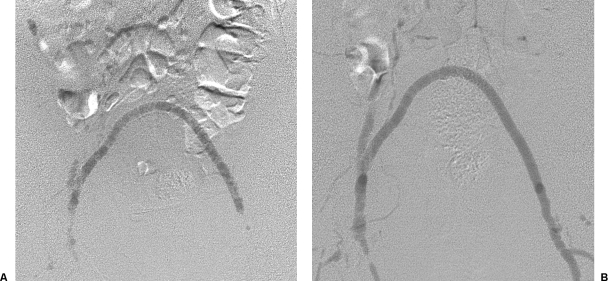
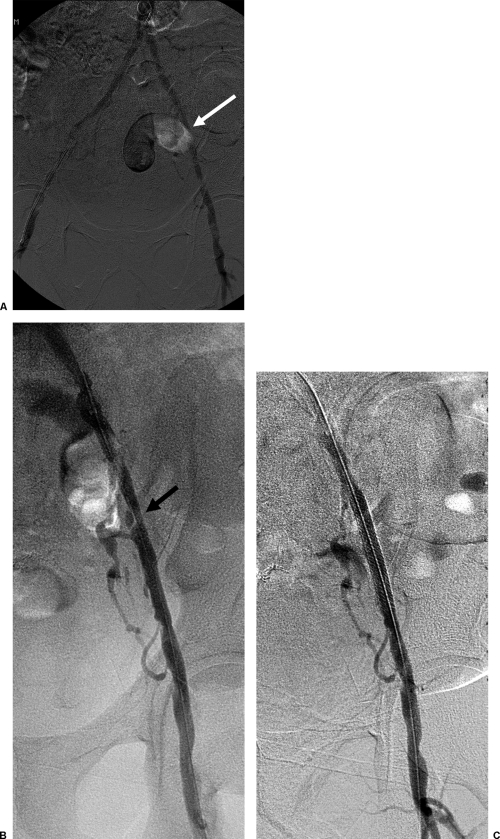
It is important to recognize that CO2 “floats” on the top of blood; therefore abnormalities in the dependent portions of blood vessels (e.g., posterior plaques in iliac arteries) may not be demonstrated to full advantage. In practical terms, this is only a problem in larger (i.e., > 1-cm diameter) vessels because CO2 fills smaller caliber arteries more completely. Arteries that assume a posterior course, such as dependent coursing renal arteries, may be difficult to fill, particularly from a nonselective injection. As CO2 passes through bifurcations, the bolus dissipates into smaller bubbles that can create a “pseudostenosis” (Fig. 2). Overlying bowel gas can obscure vessels and presents a potential pitfall to interpretation (Fig. 3).
Figure 2.
Carbon dioxide (CO2) pelvic angiography in a patient with a femoral-to-femoral crossover graft. (A) Digital subtraction angiogram with insufficient CO2 injected, resulting in poor filling of graft. (B) Repeat digital subtraction angiogram with larger bolus showing widely patent graft.
Figure 3.
Bowel gas pitfall. (A) Digital subtraction angiogram using carbon dioxide in which bowel gas partially obscures left external iliac artery (white arrow). (B) Digital subtraction angiogram using iodinated contrast material shows ulcerated plaque and high-grade stenosis (black arrow). (C) Digital subtraction angiogram after stenting shows alleviation of lesion.
Complications and Contraindications
The following complications have been reported using CO2 for angiography: paresthesia, abdominal pain, tenesmus, vapor lock, and nausea. Abdominal pain is thought to be related to CO2 in the mesenteric vessels and is best handled by rotating the patient from side to side and gently massaging the abdomen to allow the CO2 to diffuse into the blood. It may be caused by vapor lock in mesenteric arteries and is reported to be more likely in patients with CO2 collecting in abdominal aortic aneurysms. Nausea is usually encountered only when high flow rates are used for angiography.
Vapor lock in the heart is a feared complication that occurs when CO2 is trapped there, increasing pulmonary artery pressure and preventing normal blood flow and venous return. This is essentially only a risk with venography and may reflect air contamination. Intravascular air injection may cause significant vapor lock in the heart with bradycardia and hypotension. If this occurs, the patient should be rotated into a left lateral decubitus position.
CO2 should not be combined with nitrous oxide sedation, and it should be used with discretion in patients with chronic obstructive pulmonary disease. CO2 is contraindicated in the cerebral vessels and should not be injected above the level of the diaphragm or used in patients with left-to-right shunts.
DISCUSSION
Hawkins, Caridi, and associates at the University of Florida have accrued the longest and largest experience with CO2, which can be used for a variety of procedures:
Transjugular intrahepatic portosystemic shunt (TIPS) insertion: CO2 is used to perform wedged portal venography; however, there have been several case reports of hepatic capsular rupture and death when using CO2 for this purpose. Personally, I do not routinely perform wedged venography during TIPS. I do not find it particularly helpful. If CO2 is used for this purpose, some investigators advocate gentle injection via an occlusion balloon inflated in the hepatic vein.
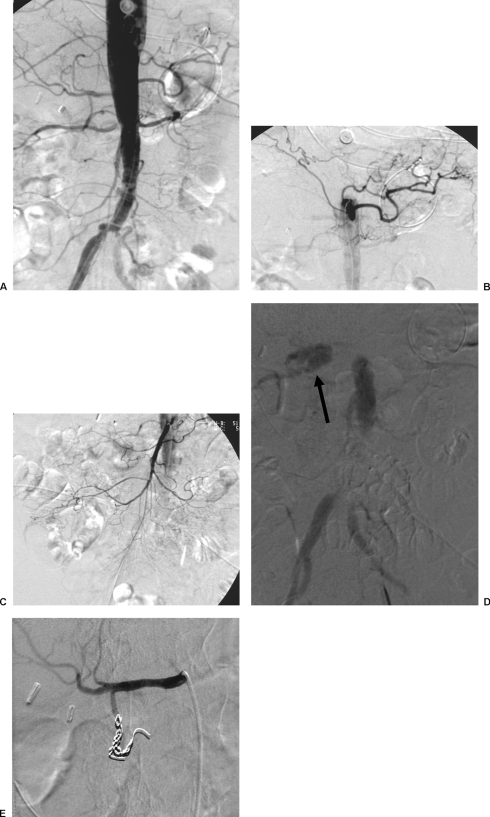
Gastrointestinal (GI) hemorrhage: CO2 is much less viscous compared with liquid contrast material and therefore may be more sensitive for the detection of GI bleeding. I have found it helpful in problematic cases (Fig. 4) but do not perform it routinely for all procedures.
Diagnostic angiography and intervention: I routinely use CO2 for diagnostic angiography in patients with renal insufficiency. In most cases, it can be used for both diagnosis and intervention (Fig. 5). Typically, I augment the study with a small volume of iso-osmolar contrast (10 to 20 mL) to show any pathology to best advantage or clarify any equivocal findings. I dilute the contrast 1:1 and use it for selective or subselective injections.
Renal intervention: Similar to diagnostic angiography, I often use CO2 for renal interventions. Occasionally, it is helpful to rotate the patient slightly to help fill the artery. Again, due to its relatively low viscosity, it is much easier to inject CO2 around a guidewire via a sidearm adaptor compared with liquid contrast. If necessary, I augment the study with small volumes of iso-osmolar contrast.
Venography: Can be done prior to inferior vena cava filter placement. It is more difficult to visualize posterior oriented renal veins (i.e., right renal vein) and caval thrombus compared with liquid contrast. CO2 can also be used for arm venography prior to dialysis access creation for patients with renal insufficiency who have not completely lost renal function or in patients with allergies to iodinated contrast material. In all these interventions, it is important to check the pulmonary arteries for accumulation of gas and subsequent dissipation within 30 to 45 seconds.
Figure 4.
Carbon dioxide (CO2) for gastrointestinal bleeding from obscure source. Tagged red blood cell scintigraphy showed bleeding in the right upper quadrant. (A) Aortogram using iodinated contrast material fails to show bleeding. (B) Celiac arteriogram fails to demonstrate bleeding. (C) Superior mesenteric angiogram fails to show bleeding. (D) CO2 aortogram showing bleeding in the right upper quadrant (arrow). (E) Digital subtraction angiogram after embolization. Active bleeding was found from a replaced gastroduodenal artery arising directly from the aorta, which was then embolized.
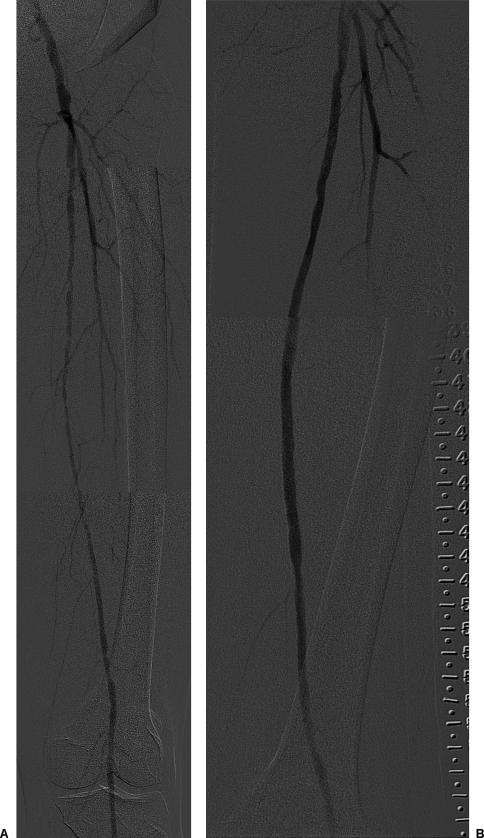
Figure 5.
Superficial femoral artery intervention. (A) Composite digital subtraction angiogram using carbon dioxide shows diffuse atherosclerotic disease of superficial femoral artery. (B) Composite digital subtraction angiogram after covered stent placement shows widely patent artery.
SUGGESTED READINGS
- Hawkins I F, Caridi J G. Carbon dioxide (CO2) digital subtraction angiography: 26-year experience at the University of Florida. Eur Radiol. 1998;8:391–402. doi: 10.1007/s003300050400. [DOI] [PubMed] [Google Scholar]
- Hawkins I F, Caridi J G, Klioze S D, Mladinich C R. Modified plastic bag system with O-ring fitting connection for carbon dioxide angiography. AJR Am J Roentgenol. 2001;176:229–232. doi: 10.2214/ajr.176.1.1760229. [DOI] [PubMed] [Google Scholar]
- Shaw D R, Kessel D O. The current status of the use of carbon dioxide in diagnostic and interventional angiographic procedures. Cardiovasc Intervent Radiol. 2006;29:323–331. doi: 10.1007/s00270-005-0092-2. [DOI] [PubMed] [Google Scholar]