ABSTRACT
Chronic mesenteric ischemia is a rare condition, generally characterized by postprandial abdominal pain. Although chronic mesenteric ischemia accounts for only a small percentage of all mesenteric ischemic events, it can have significant clinical consequences. There are multiple etiologies; however, the most common cause is atherosclerosis. The diagnosis of chronic mesenteric ischemia requires a high clinical index of suspicion. An imaging study can confirm the presence of a stenosis or occlusion involving the mesenteric vessels in patients who are suspected of having chronic mesenteric ischemia. The diagnosis is usually late in its course due to the slow progression of disease and the abundance of mesenteric collaterals. Because of the extensive collateral network, usually at least two of the three visceral vessels need to be affected before patients develop symptoms. Treatment is necessary to avoid progression to bowel ischemia and infarction. Once a diagnosis of chronic mesenteric ischemia is made, treatment options include open surgical revascularization and endovascular revascularization.
Keywords: Ischemia, mesenteric, atherosclerosis
Chronic mesenteric ischemia is a rare condition that was first described in 1918 as “abdominal angina” by Goodman.1 Its onset is gradual and it is often diagnosed late in its course. Treatment of the underlying lesion(s) is necessary to prevent the development of acute mesenteric ischemia, which may result in bowel infarction and death. Shaw performed the first successful open repair for chronic mesenteric ischemia in 1958.2 Since then, surgical repair has been the standard treatment for chronic mesenteric ischemia. However, angioplasty and stenting of the mesenteric arteries for treatment of chronic mesenteric ischemia has gained popularity because of its effectiveness and relatively low rates of morbidity and mortality compared with open surgical repair.
PATHOGENESIS AND CLINICAL PRESENTATION
The etiology of chronic mesenteric ischemia is often multifactorial. The most common cause is atherosclerosis involving the proximal portions of the celiac, superior mesenteric, or inferior mesenteric artery.3 Less common etiologies include dissection, vasculitis, fibromuscular dysplasia, radiation, and cocaine abuse. Factors that predispose patients to atherosclerosis are associated with increased risk for chronic mesenteric ischemia. These include smoking, hypertension, diabetes mellitus, and hypercholesterolemia. Chronic symptoms are caused by the gradual decrease in blood flow to the intestines. Because total blood flow to the intestine can vary from 25% when fasting to 35% after eating, symptoms are more prevalent after eating.4 The normal circulation to the bowel includes blood supply from the celiac artery, the superior mesenteric artery, and the inferior mesenteric artery. There is, however, the potential for collateralization between the vascular territories of these vessels.5 The abundant mesenteric blood supply and slow progression of atherosclerosis allows these collateral pathways to develop.6 Because of this collateral circulation within the mesenteric vasculature, patients may not experience symptoms until two or three major mesenteric vessels are involved. Classic symptoms of chronic mesenteric ischemia include postprandial abdominal pain associated with significant weight loss, food fear, nausea, vomiting, or diarrhea. The abdominal pain classically starts 15 to 30 minutes after a meal and typically lasts for ∼30 minutes.7 As the obstructive process progresses, chronic, dull abdominal pain ensues. Chronic mesenteric ischemia generally presents in patients older than 60 years of age and is 3 times more frequent in women.8
WORKUP
Physical exam findings include signs of weight loss, malnutrition, ± epigastric bruit, and evidence of diffuse atherosclerotic disease, including coronary artery disease and peripheral vascular disease.
Laboratory Studies
Complete blood count may demonstrate anemia, leukopenia, or lymphopenia secondary to chronic malnutrition.
Chemistry studies may show electrolyte abnormalities as a result of malnutrition.
Liver function tests (LFT) may show hypoalbuminemia from malnutrition.
Preprocedural laboratories should also include a prothrombin time/international normalized ratio and activated partial thromboplastin time.
IMAGING
The history and physical exam as well as a high index of suspicion are important factors in diagnosing chronic mesenteric ischemia. Once the diagnosis of chronic mesenteric ischemia is suspected, imaging options for confirmation include ultrasound (US), computed tomography angiography (CTA), magnetic resonance angiography (MRA), and conventional angiography.
US
Duplex US (Fig. 1) has shown promising results in the diagnosis of chronic mesenteric ischemia. The study can be limited in quality by patient body habitus, overlying bowel gas, and operator dependence. In addition, the velocity criteria for determining a significant stenosis vary according to the postprandial state of the patient. Fasting duplex criteria for mesenteric stenosis suggest that a superior mesenteric artery peak systolic velocity of 275 cm/s or greater and a celiac artery peak systolic velocity of 200 cm/s or greater are reliable indicators of a 70% or greater stenosis.9
Figure 1.
(A,B) Fasting duplex ultrasound demonstrating peak systolic velocities of ∼300 cm/s in the superior mesenteric artery indicating a stenosis of 70% or greater.
CT
Multidetector helical CT (Fig. 2) can be used to evaluate for stenosis or occlusion within the mesenteric vasculature. In addition, sequelae of ischemia such as bowel wall thickening, pneumatosis, or peritoneal fluid can be identified. Because of its fast scanning speeds (0.5 seconds) and narrow collimation (1 mm), multidetector CT scanners can image the entire abdomen in much shorter times than single-detector CT scanners. The scan can be timed to acquire images in both the arterial and venous phases, which improves detection of an underlying abnormality in the vasculature. In addition, the fast scanning and 1-mm collimation improves the quality of 3-D reconstruction images. 3-D imaging allows one to evaluate the collateral pathways, which may be present in cases of chronic mesenteric ischemia.
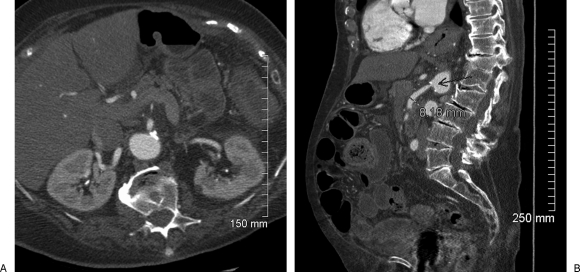
Figure 2.
(A) Postcontrast axial computed tomography scan demonstrating a stenosis at the origin of the superior mesenteric artery. (B) Saggital reformat maximum intensity projection (MIP) image confirming the stenosis.
Magnetic Resonance Imaging/MRA
Similar to CT, the multiplanar imaging capability of magnetic resonance imaging (MRI)/MRA makes this another good, noninvasive imaging technique to evaluate for stenoses within the mesenteric vessels. Another advantage to MRI is the ability to image without radiation. One disadvantage, however, is the potential inability to accurately evaluate the inferior mesenteric artery.
Angiography
Catheter angiography (Fig. 3) has been the gold standard for diagnosing mesenteric vascular disease for many years.7 If chronic mesenteric ischemia is suspected, an US, CT, or MRI/MRA may be performed to assist with treatment planning, including angioplasty or stent placement. In addition to visual inspection of the mesenteric vasculature, angiography allows for selective catheterization and pressure measurement across a stenosis to determine the hemodynamic significance of questionable lesions.
Figure 3.
(A) Lateral aortogram demonstrating a celiac artery stenosis. (B,C) Selective inferior mesenteric arteriogram demonstrating retrograde filling of the superior mesenteric artery through an arc of Riolan, which is secondary evidence of a superior mesenteric arterial stenosis or occlusion.
TREATMENT
After the diagnosis of chronic mesenteric ischemia is made, patients should undergo definitive treatment because of the risk of continued weight loss, acute infarction, perforation, sepsis, and death.
Medical treatment is usually reserved for patients who are not healthy enough to be treated, either surgically or endovascularly. This would consist of long-term anticoagulation, such as warfarin. In addition, some patients may find short-term relief with nitrate therapy; however, this is not curative.
Open surgical repair includes transaortic endarterectomy, direct reimplantation on the aorta, and antegrade or retrograde bypass grafting. Several series evaluating surgical repair for chronic mesenteric ischemia have reported high technical success rates and symptom improvement in 90 to 100% of patients.10,11,12,13,14 However, they have also demonstrated that open surgical repair has also been associated with significant morbidity (5 to 30%) and mortality (5 to 12%).10 This is at least in part related to the weight loss and malnutrition, including low albumin, in this patient group, which are all predictors of increased morbidity and mortality after major surgery.15 Symptom recurrence rates following open surgical repair for chronic mesenteric ischemia ranged between 9% and 35% in these studies. Recurrent symptoms and thus the reintervention rate were higher in patients treated endovascularly when compared with those treated with open surgery.10
Endovascular repair includes angioplasty and/or stent placement of lesions within the mesenteric vasculature (Fig. 4). The technique of mesenteric angioplasty as an alternative to surgery was first described in 1980.16 Kougias et al performed a meta-analysis of several published series evaluating endovascular treatment of mesenteric stenosis in patients diagnosed with chronic mesenteric ischemia. The data from 16 series were evaluated and a total of 328 patients were studied. These studies demonstrated high technical (90 to 100%) and high clinical (80 to 100%) success rates. The complication rate was 9% and the 30-day mortality was 3%, which is favorable compared with the published rates in patients treated with open surgery.8 In this meta-analysis, repeat angioplasty was performed in 27% of the patients. However, the low morbidity and mortality associated with endovascular treatment, especially in this patient subset, has led to the widespread use of this treatment modality as first-line treatment for patients diagnosed with chronic mesenteric ischemia. In addition, a few studies have compared stent placement to angioplasty alone. Landis et al hypothesize that stenting of the mesenteric arteries provides more structural support to the arterial wall against elastic recoil when compared with angioplasty alone and thus provides better long-term patency and lower rates of reintervention.17 A review of the literature demonstrates a better patency rate with mesenteric artery stenting when compared with angioplasty alone.17,18 Figure 5 demonstrates a case of elastic recoil following conventional angioplasty and complete resolution of the stenosis following stent placement.
Figure 4.
(A) Lateral aortogram demonstrating a stenosis in the superior mesenteric artery. (B) Selective superior mesenteric arteriogram. (C) Stent placement. (D) Poststent arteriogram demonstrating no residual stenosis.
Figure 5.
(A) Selective superior mesenteric arteriogram demonstrating a proximal stenosis. Note the replaced hepatic artery. (B) Angioplasty of the stenosis with wire protection in the replaced hepatic artery. (C) Postangioplasty arteriogram demonstrating a significant residual stenosis. (D) Balloon expandable stent placement. (E) Poststent arteriogram demonstrating resolution of the stenosis.
FOLLOW-UP
Patients should be seen in clinic at routine intervals following treatment. With the follow-up clinic visit, a dedicated history and physical should be performed. If symptoms recur, a noninvasive imaging study (US, CT, MRI/MRA) can be performed to evaluate for restenosis or progression of disease. At our institution, we recommend routine duplex evaluation at 1, 3, and 6 months initially, and every 6 to 12 months thereafter. We also recommend anticoagulation with clopidogrel in patients in whom a stent was placed, if there is no contraindication. The usual course is a loading dose with 300 mg at the time of treatment and a once-daily dose of 75 mg for at least 3 months. In addition, the associated risk factors for atherosclerosis (smoking, hypercholesterolemia, diabetes mellitus) should be managed.
CONCLUSION
Chronic mesenteric ischemia is a rare, but potentially life-threatening condition. A high index of suspicion is necessary for diagnosis. In the vast majority of cases, the cause is atherosclerotic stenosis or occlusion involving the mesenteric arteries. Because there is significant mesenteric collateral circulation, at least two of the three visceral arteries are involved in symptomatic patients. Once a patient with classic symptoms is diagnosed with a lesion within the mesenteric vasculature and the diagnosis of chronic mesenteric ischemia is made, treatment options consist of open surgical repair and endovascular revascularization techniques. Traditionally, open surgical repair has been the standard method of treatment. However, the published success rates and lower morbidity and mortality associated with endovascular revascularization techniques have led to increased popularity of this technique as a first-line treatment for patients with chronic mesenteric ischemia.
REFERENCES
- Goodman G H. Angina abdominus. Am J Med Sci. 1918;155:524–528. [Google Scholar]
- Shaw R S, Maynard E P., III Acute and chronic thrombosis of the mesenteric arteries associated with malabsorption; a report of two cases successfully treated by thromboendarterectomy. N Engl J Med. 1958;258:874–878. doi: 10.1056/NEJM195805012581803. [DOI] [PubMed] [Google Scholar]
- Sreenarasimhaiah J. Chronic mesenteric ischemia. Best Pract Res Clin Gastroenterol. 2005;19:283–295. doi: 10.1016/j.bpg.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Chang R W, Chang J B, Longo W E. Update in management of mesenteric ischemia. World J Gastroenterol. 2006;12:3243–3247. doi: 10.3748/wjg.v12.i20.3243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleveland T J, Nawaz S, Gaines P A. Mesenteric arterial ischaemia: diagnosis and therapeutic options. Vasc Med. 2002;7:311–321. doi: 10.1191/1358863x02vm454ra. [DOI] [PubMed] [Google Scholar]
- Biebl M, Oldenburg W A, Paz-Fumagalli R, McKinney J M, Hakaim A G. Surgical and interventional visceral revascularization for the treatment of chronic mesenteric ischemia—when to prefer which? World J Surg. 2007;31:562–568. doi: 10.1007/s00268-006-0434-5. [DOI] [PubMed] [Google Scholar]
- Ujiki M, Kibbe M R. Mesenteric ischemia. Perspect Vasc Surg Endovasc Ther. 2005;17:309–318. doi: 10.1177/153100350501700405. [DOI] [PubMed] [Google Scholar]
- Kougias P, El Sayed H F, Zhou W, Lin P H. Management of chronic mesenteric ischemia. The role of endovascular therapy. J Endovasc Ther. 2007;14:395–405. doi: 10.1583/07-2102.1. [DOI] [PubMed] [Google Scholar]
- Mitchell E L, Moneta G L. Mesenteric duplex scanning. Perspect Vasc Surg Endovasc Ther. 2006;18:175–183. doi: 10.1177/1531003506291885. [DOI] [PubMed] [Google Scholar]
- Atkins M D, Kwolek C J, LaMuraglia G M, Brewster D C, Chung T K, Cambria R P. Surgical revascularization versus endovascular therapy for chronic mesenteric ischemia: a comparative experience. J Vasc Surg. 2007;45:1162–1171. doi: 10.1016/j.jvs.2007.01.067. [DOI] [PubMed] [Google Scholar]
- Kihara T K, Blebea J, Anderson K M, Friedman D, Atnip R G. Risk factors and outcomes following revascularization for chronic mesenteric ischemia. Ann Vasc Surg. 1999;13:37–44. doi: 10.1007/s100169900218. [DOI] [PubMed] [Google Scholar]
- Jimenez J G, Huber T S, Ozaki C K, et al. Durability of antegrade synthetic aortomesenteric bypass for chronic mesenteric ischemia. J Vasc Surg. 2002;35:1078–1084. doi: 10.1067/mva.2002.124377. [DOI] [PubMed] [Google Scholar]
- Park W M, Cherry K J, Jr, Chua H K, et al. Current results of open revascularization for chronic mesenteric ischemia: a standard for comparison. J Vasc Surg. 2002;35:853–859. doi: 10.1067/mva.2002.123753. [DOI] [PubMed] [Google Scholar]
- Cho J S, Carr J A, Jacobsen G, Shepard A D, Nypaver T J, Reddy D J. Long-term outcome after mesenteric artery reconstruction: a 37-year experience. J Vasc Surg. 2002;35:453–460. doi: 10.1067/mva.2002.118593. [DOI] [PubMed] [Google Scholar]
- Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri S F. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg. 1999;134:36–42. doi: 10.1001/archsurg.134.1.36. [DOI] [PubMed] [Google Scholar]
- Furrer J, Grüntzig A, Kugelmeier J, Goebel N. Treatment of abdominal angina with percutaneous dilatation of an arteria mesenterica superior stenosis. Preliminary communication. Cardiovasc Intervent Radiol. 1980;3:43–44. doi: 10.1007/BF02551961. [DOI] [PubMed] [Google Scholar]
- Landis M S, Rajan D K, Simons M E, Hayeems E B, Kachura J R, Sniderman K W. Percutaneous management of chronic mesenteric ischemia: outcomes after intervention. J Vasc Interv Radiol. 2005;16:1319–1325. doi: 10.1097/01.RVI.0000171697.09811.0E. [DOI] [PubMed] [Google Scholar]
- Yazdi H R, Youness F, Laroia S, et al. Mesenteric artery stenting for chronic mesenteric ischemia. Vasc Dis Manage. 2007;4:180–184. [Google Scholar]