ABSTRACT
The arterial and venous circulation of the bowel is complex and is characterized by marked redundancy of multiple interconnecting branches, which provides a rich blood supply to aid in the digestive process and also serves to protect the bowel from potential ischemia or infarction. As a result of this circulatory pattern, anatomic variants and extensive collateral pathways are common. A thorough knowledge of both the arterial and venous mesenteric circulation, including normal, variant, and collateral anatomy, is necessary for the appropriate evaluation and management of the various disease processes that may affect the vascular supply of the gastrointestinal system.
Keywords: Mesenteric circulation, mesenteric collateral pathways, variant arterial anatomy
NORMAL ANATOMY
Developmental
The primitive fetal blood supply is initially a dual one, with double aortas and both a dorsal and a ventral arterial supply to the abdominal viscera. During subsequent differentiation, much of this dual vascular supply regresses. Varying degrees of persistence of certain portions of the dual blood supply account for the many variations that are seen in the mesenteric circulation.1
A series of vitelline arteries arise from the paired, fused dorsal aortas in the fetus, and are initially connected through a ventral anastomotic channel. During fetal development, three of these vitelline segments (10th, 13th, and 21st) persist to individually form the celiac, superior mesenteric (SMA), and inferior mesenteric (IMA) arteries; the remaining segments regress before birth. If a portion of the ventral anastomosis fails to regress, or there is abnormal persistence of vitelline segments during development, anatomic variants result (e.g., arc of Buhler, hepatic artery “replaced” to the SMA) (Fig. 1).1,2,3,4,5,6
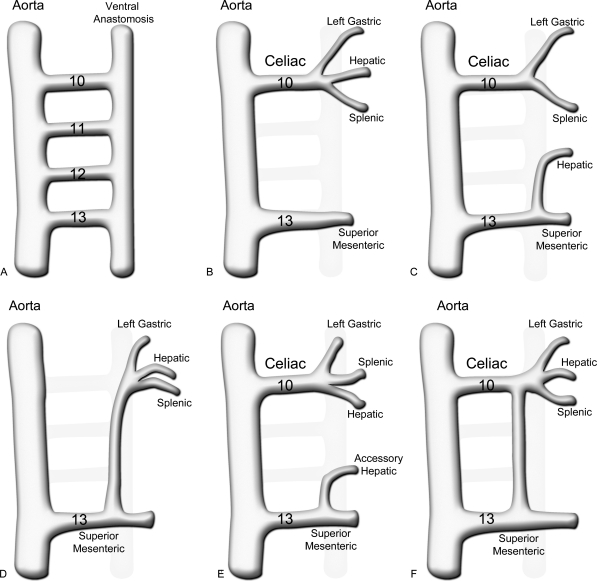
Figure 1.
Embryology of normal and variant mesenteric vascular anatomy. (A) In the primitive vasculature, the 10th to 13th vitelline arteries communicate between the aorta and a primitive ventral anastomotic artery. (B) Normally the ventral anastomosis and the 11th and 12th vitelline arteries regress, leaving the 10th root as the celiac trunk and the 13th as the superior mesenteric artery (SMA). (C) With replacement of the hepatic artery to the SMA, there is incomplete regression of the ventral anastomosis, forming a hepatomesenteric trunk. (D) A celiacomesenteric trunk occurs when the 10th to 12th vitelline arteries regress and a large portion of the ventral anastomosis persists to connect the celiac artery and branches to the SMA. (E) A partially replaced or accessory hepatic artery occurs in similar fashion to a completely replaced hepatic artery, through failure of a portion of the ventral anastomosis to regress. (F) The arc of Buhler results from persistence of the ventral anastomosis, connecting the celiac and SMA, despite regression of the 11th and 12th vitelline arteries.
The hepatic, splenic, and portal venous systems originate through the development of a liver bud that forms between the pericardial cavity and the primitive yolk sac stalk. Hepatic sinusoids are formed when liver cords insinuate between vitelline and umbilical vein tributaries. Branches of the right vitelline vein around the duodenum ultimately become the central portal vein, while the right umbilical vein involutes and the left umbilical vein becomes the primary venous inflow vessel to the liver. This left umbilical vein inflow (portal venous inflow) is connected via the ductus venosus to the hepatic venous outflow. The hepatic venous outflow consists of the hepatic veins and the intrahepatic portion of the inferior vena cava (IVC) formed by the right vitelline vein. Shortly after birth, the ductus venosus and the left umbilical vein close and form the ligamentum venosum and the ligamentum teres, respectively.1,2
Celiac Artery and Branches
The celiac artery (celiac axis or trunk) arises from the anterior aspect of the abdominal aorta at approximately the T-12 level, with either a cephalad, caudad, or straightforward course of variable length. Classically, this vessel then divides into three arterial branches: the left gastric, splenic, and common hepatic (Fig. 2). Most commonly, the initial branch of the celiac trunk is the left gastric artery, followed by a division into the splenic and the common hepatic arteries; this pattern is seen in 65 to 75% of individuals, whereas a true trifurcation is seen in only 25% of patients. As a relatively common anatomic variant, either the inferior phrenic arteries (35% incidence) or the dorsal pancreatic artery (22% incidence) may originate from the celiac trunk.3,4,7,8 The latter variant may further give rise to either the entire middle colic artery or to the left branch of the middle colic artery (Fig. 3).
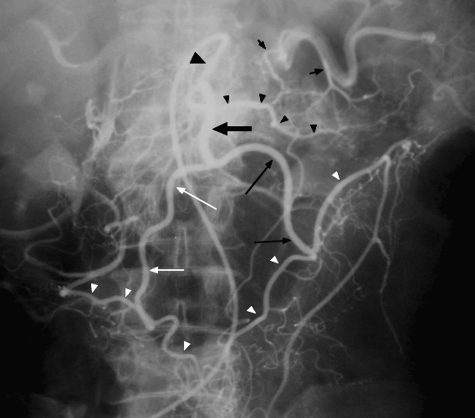
Figure 2.
Digital subtraction angiography arteriogram shows the common hepatic (medium white arrow), splenic (large white arrow) and left gastric (small black arrow) arteries as the three divisions of the celiac trunk. After the origin of the gastroduodenal artery (GDA; medium black arrow) the proper hepatic artery (large black arrow) courses and divides into the right (small white arrow) and left (white arrowhead) hepatic arteries. The GDA terminates as the right gastroepiploic artery (medium black arrowheads). Note that there are accessory left gastric artery branches (small black arrow-heads).
Figure 3.
Selective arteriogram shows variant anatomy in which the entire middle colic artery (large black arrow) arises from the dorsal pancreatic artery (large black arrowhead) and then divides into the right (small white arrows) and left (small black arrows) branches to supply the entire transverse colon (small white arrowheads). The transverse pancreatic artery (small black arrowheads) also arises from the dorsal pancreatic artery and has multiple anastomoses with small branches (short black arrows) that arise from the splenic artery.
The common hepatic artery gives off the gastroduodenal artery (GDA) and then continues as the proper hepatic artery, which divides into the right and left hepatic arteries, with an occasional middle hepatic artery, that supplies the hepatic quadrate. The small right gastric artery usually arises from either the common or the left hepatic artery, to supply the pylorus and the lesser gastric curvature, ultimately anastomosing with the distal left gastric artery (Fig. 4). The gallbladder is supplied by the cystic artery, arising from the right hepatic artery.
Figure 4.
Selective common hepatic arteriogram shows the gastroduodenal (GDA) artery (small white arrow) and its terminal branch, the gastroepiploic artery (small white arrowheads). After yielding the GDA, the common hepatic becomes the proper hepatic artery (large black arrowhead), which then divides into the right (small black arrows) and left (small black arrowheads) hepatic arteries. The right gastric artery (large white arrows) arises from the proper hepatic artery, but may also arise from the left hepatic artery.
The gastroduodenal artery courses between the pancreas and the duodenum, yielding as its first branches the superior pancreaticoduodenal arteries. This superior pancreaticoduodenal arterial arcade supplies the pancreatic head through extensive anastomoses with the inferior pancreaticoduodenal arteries that originate from the SMA (Fig. 4).1,2 Typically, the posterior superior pancreaticoduodenal artery arises first, to supply both the pancreas and the pylorus, and the anterior superior pancreaticoduodenal artery follows. The terminal branch of the GDA, the right gastroepiploic artery supplies the greater gastric curvature and ultimately anastomoses with the left gastroepiploic artery that arises from the splenic artery.
The splenic artery arises from the celiac artery distal to the left gastric artery origin and is closely associated with the dorsal aspect of the pancreatic body and tail. With age, the artery elongates and becomes more tortuous, and is one of the initial visceral vessels to demonstrate atherosclerotic disease. The splenic artery gives off several variable branches to the spleen, pancreas, and stomach. The artery divides near the splenic hilum into superior and inferior branches that supply the spleen, while the dorsal pancreatic artery, multiple small pancreatic branches, and the pancreatica magna artery arise from the splenic artery throughout its course, to supply the pancreatic body and tail. The dorsal pancreatic artery usually gives off the transverse pancreatic artery, which courses through the body and tail and has extensive anastomoses with the other multiple pancreatic branches. The splenic arterial supply to the stomach is through the short gastric arteries and the inferior polar artery that gives rise to the left gastroepiploic artery that supplies the lesser gastric curvature. Both the right and left gastroepiploic arteries yield epiploic or omental arteries that supply the mesentery and greater omentum.
The gastric cardia is supplied by the left gastric artery through branches to the distal esophagus and gastric fundus (Fig. 5). There are extensive connections with the short gastric branches, the right gastric and the left inferior phrenic arteries. Accessory left gastric arteries occur relatively frequently and may arise from the splenic, common hepatic, celiac, and left hepatic arteries. Additionally, an accessory left hepatic (incidence: 8 to 13%) or the entire left hepatic artery (incidence: 10 to 12%) may originate from the left gastric artery as an anatomic variant and thus partially or entirely supply the left hepatic lobe.8,9
Figure 5.
Selective arteriogram shows the left gastric artery (large white arrow) supplying the gastric cardia and retrograde filling of the right gastric artery (large white arrowheads) and opacification of a portion of the left hepatic artery (small white arrow) from which the right gastric artery arises. There is also retrograde filling of the gastroepiploic artery (small white arrowheads) and opacification of a short segment of the gastroduodenal artery (small black arrow), from which the right gastroepiploic artery originates.
Superior Mesenteric Artery and Branches
The SMA arises from the anterior aorta 1 to 2 cm below the celiac artery, near the L1–2 level. It courses behind the pancreatic body where it enters the mesentery, and supplies the distal duodenum, the entire small bowel, and the colon from the cecum to the midtransverse portion.
The first SMA branch is the inferior pancreaticoduodenal artery, which occasionally arises with the first jejunal branch as a common trunk. As previously noted, this is part of a rich collateral arcade supplying the pancreatic head. The middle colic artery arises proximally from the right side of the SMA either as a separate trunk or in common with the right colic artery (Fig. 6). Typically, the middle colic artery divides into right and left branches, which supply the ascending and transverse colon, respectively. The right branch of the middle colic artery anastomoses with the ascending branch of the right colic artery, while the left branch connects with the ascending branch of the left colic artery in the splenic flexure region to form an important SMA–IMA collateral pathway, the marginal artery of Drummond, that courses along the colonic mesenteric border.
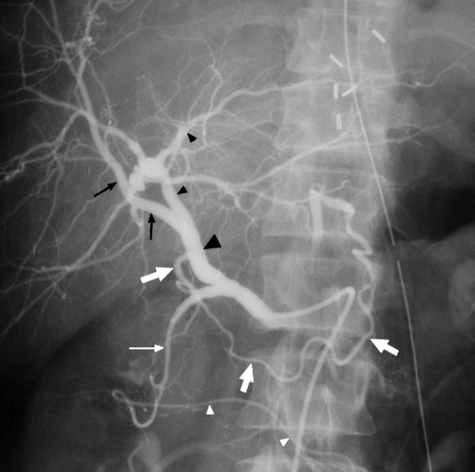
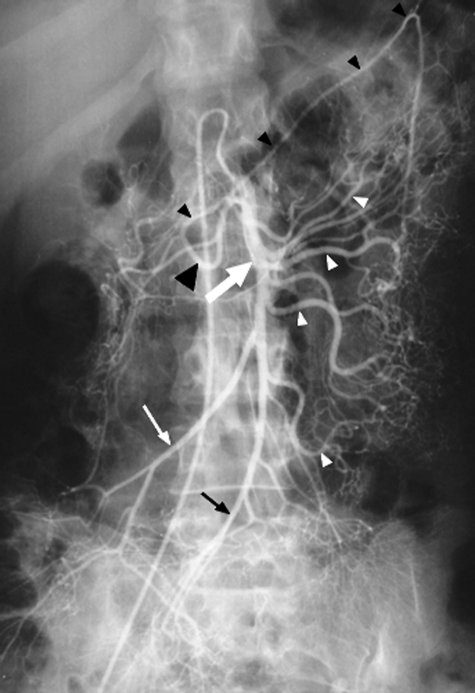
Figure 6.
Selective superior mesenteric artery (SMA; large white arrow) arteriogram shows the middle colic artery (large black arrowhead) divides into left (small black arrowheads) and right branches. Multiple jejunal and ileal branches (small white arrowheads) and the right colic artery (small white arrow) arise before the ileocolic artery (small black arrow), which is the terminal branch of the SMA.
Multiple jejunal and ileal branches arise from the main SMA trunk, extending from the left upper to the left and right lower quadrants. Numerous interconnecting arterial arcades between the branches terminate in vasa recta that supply the small bowel wall. The SMA terminates as the ileocolic artery, with branches to the terminal ileum, appendix, cecum, and proximal ascending colon.
Inferior Mesenteric Artery and Branches
The IMA originates anterolaterally from the left aspect of the abdominal aorta around the L3–4 level and supplies the colon from the midtransverse portion to the rectum. Initially, the vessel has an inferior course of several centimeters and then yields to the left colic artery. The ascending branch of this latter vessel anastomoses with the left branch of the middle colic artery in the splenic flexure region (Fig. 7). The IMA and left colic arteries also yield descending colic and sigmoid branches to the lower descending and sigmoid colon segments. The IMA then terminates as the superior rectal (hemorrhoidal) artery, which bifurcates into right and left branches to supply the upper rectum. Middle and inferior rectal branches to the remainder of the rectum arise from the anterior division of the internal iliac arteries.
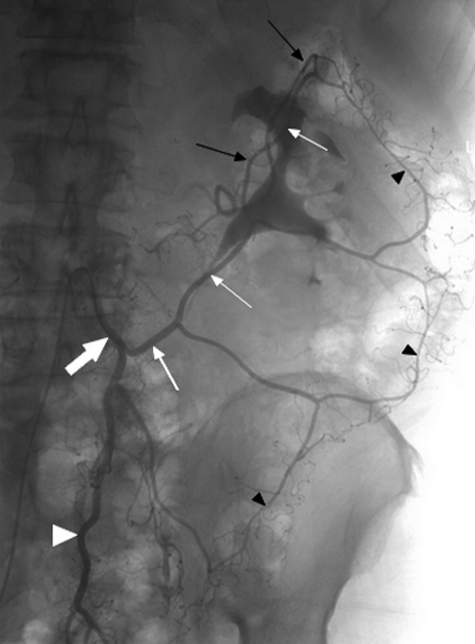
Figure 7.
Selective arteriogram shows the IMA (large white arrow) yields the left colic artery (small white arrows) which has an ascending division that anastomoses with the left branch of the middle colic artery (small black arrows) in the splenic flexure region. The terminal branch of the IMA is the superior rectal (hemorrhoidal) artery (white arrowhead). Note the marginal artery of Drummond (small black arrowheads) that courses along the mesenteric border of the colon.
Hepatic, Splenic, and Portal Venous System
The splenic vein courses behind the pancreas below the splenic artery and receives inflow from the short gastric, left gastroepiploic, pancreatic, and inferior mesenteric veins. The superior mesenteric vein (SMV) receives venous blood from the jejunum, ileum, and proximal colon via venous tributaries. The splenic and the superior mesenteric veins join to form the portal vein, which courses anterior to the IVC and behind the pancreatic head prior to entering the hilum of the liver. The portal vein bifurcates into the right and left portal veins; this may occur outside of the liver in ~50% of individuals.10,11 The right and left portal veins and their branches course with the hepatic arteries into the hepatic substance, supplying the various hepatic segments (Fig. 8).
Figure 8.
Computed tomography angiogram shows the splenic vein (small white arrows) joining the superior mesenteric vein (large white arrow) to form the portal vein (white arrowhead), which bifurcates into the right (black arrowhead) and left (large black arrow) portal veins. Note that the right (small black arrowhead) and left (small black arrows) hepatic arteries course with the portal vein divisions into the liver to supply their respective anatomic territories.
The inferior mesenteric vein (IMV), which drains the same colonic territory supplied by the IMA, may join either the splenic or the superior mesenteric vein. Other venous tributaries that ultimately drain into the portal system include the right gastroepiploic, pancreaticoduodenal, and right colonic veins; these often form a common gastrocolic trunk that enters the SMA, while the right and left gastric or coronary veins join the main portal or the splenic vein.
The right, middle, and left hepatic veins drain the liver into the IVC near the diaphragm, while the caudate lobe is drained separately into the intrahepatic IVC.
VARIANT ANATOMY
Anomalous branching patterns of the mesenteric arteries occur frequently, whereas anomalies involving the central origins from the aorta are much less common. The hepatic arteries frequently exhibit variant anatomy; by convention when an entire hepatic lobe is supplied by a vessel with an aberrant origin, this is termed a “replaced” hepatic artery, whereas an “accessory” hepatic artery denotes a vessel with an aberrant origin that only partially supplies a hepatic lobe (Fig. 9).1,7,8,9 Additionally, an accessory hepatic artery supplies an isolated area of a particular hepatic segment and is not merely a redundant vessel. As a general rule, a replaced or accessory hepatic artery arises from the left gastric artery in 20% of individuals and from the SMA with an equal frequency of ~20%.1
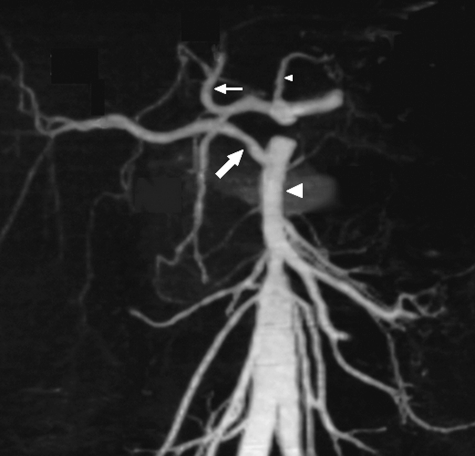
Figure 9.
Magnetic resonance angiogram shows a replaced right hepatic artery (large white arrow) arising from the superior mesenteric artery (large arrowhead). The left hepatic artery (small white arrow) arises normally from the celiac trunk, as does the left gastric artery (small arrowhead).
The celiac and superior mesenteric arteries have a common origin (celiacomesenteric trunk) in less than 1% of patients (Fig. 10).1,3 This is also the incidence of separate aortic origins of the left gastric, splenic, or hepatic arteries. Table 1 details the reported frequencies of the more important variants of the mesenteric arterial vasculature.
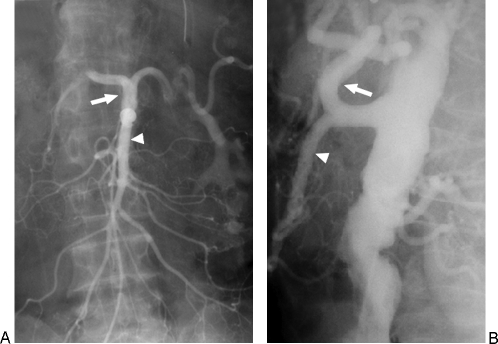
Figure 10.
Angiogram of a combined celiacomesenteric trunk is seen in both frontal (A) and lateral (B) projections. The celiac vessel courses cephalad (white arrow) and the superior mesenteric artery courses caudally (white arrowhead). This anatomic variant occurs in <1% of individuals.
Table 1.
Normal and Variant Mesenteric Arterial Anatomy
| Artery | Anomalous Origin | Frequency (%) |
|---|---|---|
| Celiac Trunk | ||
| Classic three vessel | 65–75 | |
| Classic plus dorsal pancreatic | 22 | |
| Celiacomesenteric trunk | Aorta | <1 |
| Inferior phrenic | Celiac | 35 |
| Hepatic Artery | ||
| Common hepatic from celiac | 75 | |
| Replaced common hepatic | SMA | 2.5 |
| Replaced right hepatic | SMA | 10–17 |
| Accessory right hepatic | SMA | 6–8 |
| Replaced left hepatic | Left gastric | 10–12 |
| Accessory left hepatic | Left gastric | 8–13 |
| Gastric Arteries | ||
| Left gastric artery from celiac | 90 | |
| Left gastric, splenic, or hepatic | Aorta | <1 |
| Gastroduodenal | Right or left hepatic | 18 |
| Right gastric artery | Proper hepatic | 40 |
| Right gastric artery | Left or middle hepatic | 40 |
| Right gastric artery | Right hepatic artery | 10 |
| Right gastric artery | Gastroduodenal artery | 8 |
| Middle Colic Artery | ||
| Middle colic artery | Dorsal pancreatic, splenic, hepatic | <1 |
COLLATERAL PATHWAYS
The mesenteric arterial circulation is characterized by multiple redundant interconnecting branches, allowing for a rich blood supply to the bowel through these numerous collateral pathways.12,13 This redundancy protects the bowel from potential ischemia or infarction in situations in which the arterial supply is compromised, as in segmental arterial occlusions.12,13
The primary collateral pathways are relatively constant ones that connect the main mesenteric arteries. The celiac and superior mesenteric arteries are connected through the pancreaticoduodenal arcade formed by the superior and inferior pancreaticoduodenal arteries; these pancreatic arcades become extremely important anastomotic channels in patients with either celiac or SMA occlusion.12,14 Additionally, there are inconstant collateral pathways of persistent embryologic origin that connect the celiac and the SMA (arc of Buhler and the arc of Barkow).5,6
The SMA and IMA are linked through the marginal artery of Drummond and may also be connected through the arc of Riolan (Fig. 11).15 The marginal artery of Drummond represents the major collateral arcade between the two mesenteric vessels. Located within the mesentery of the colon and lying adjacent to the colonic wall, it runs the entire length of the colon, and is composed of branches from the right, middle, and left colic arteries. The arc of Riolan is situated medial to the mesenteric border of the colon, where it courses radially through the midportion of the mesenteric arcade, near the inferior mesenteric vein.15 Some authors suggest that this is an enlargement of a normally existing collateral vessel, which dilates in the presence of a significant arterial occlusion of either the SMA or IMA.15,16,17 The IMA and the internal iliac artery collateral arcades involve the superior and middle rectal arteries.
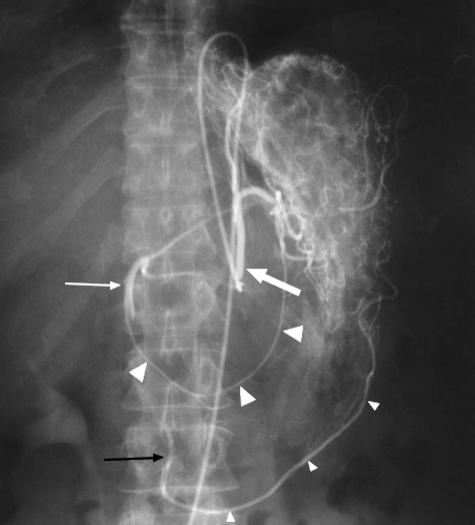
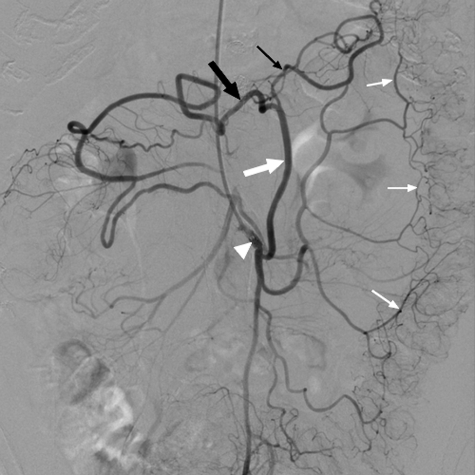
Figure 11.
Selective inferior mesenteric artery (IMA) arteriogram shows the arc of Riolan (large white arrow) arising from the IMA (white arrowhead) and coursing medially in the mesentery to anastomose with the right (large black arrow) and left (small black arrow) branches of the middle colic artery. The marginal artery of Drummond (small white arrows) courses along the mesenteric border of the colon. It is somewhat inconstant and less developed in this patient.
REFERENCES
- Reuter S R, Redman H C, Cho K J. Gastrointestinal Angiography. 3rd ed. Philadelphia, PA: WB Saunders; 1986.
- Kaufman J A, Lee M J. Vascular and Interventional Radiology: The Requisites. St. Louis, MO: Mosby; 2004.
- Petscavage J M, Maldjian P. Celiomesenteric trunk: two variants of a rare anomaly. Australas Radiol. 2007;51(Suppl):B306–B309. doi: 10.1111/j.1440-1673.2007.01824.x. [DOI] [PubMed] [Google Scholar]
- Iezzi R, Cotroneo A R, Giancristofaro D, Santoro M, Storto M L. Multidetector-row CT angiographic imaging of the celiac trunk: anatomy and normal variants. Surg Radiol Anat. 2008;30(4):303–310. doi: 10.1007/s00276-008-0324-7. [DOI] [PubMed] [Google Scholar]
- McNulty J G, Hickey N, Khosa F, O'Brien P, O'Callaghan J P. Surgical and radiological significance of variants of Bühler's anastomotic artery: a report of three cases. Surg Radiol Anat. 2001;23(4):277–280. doi: 10.1007/s00276-001-0277-6. [DOI] [PubMed] [Google Scholar]
- Saad W E, Davies M G, Sahler L, et al. Arc of Buhler: incidence and diameter in asymptomatic individuals. Vasc Endovascular Surg. 2005;39(4):347–349. doi: 10.1177/153857440503900407. [DOI] [PubMed] [Google Scholar]
- Winston C B, Lee N A, Jarnagin W R, et al. CT angiography for delineation of celiac and superior mesenteric artery variants in patients undergoing hepatobiliary and pancreatic surgery. AJR Am J Roentgenol. 2007;189(1):W13–W19. doi: 10.2214/AJR.04.1374. [DOI] [PubMed] [Google Scholar]
- Koops A, Wojciechowski B, Broering D C, Adam G, Krupski-Berdien G. Anatomic variations of the hepatic arteries in 604 selective celiac and superior mesenteric angiographies. Surg Radiol Anat. 2004;26(3):239–244. doi: 10.1007/s00276-004-0229-z. [DOI] [PubMed] [Google Scholar]
- Covey A M, Brody L A, Maluccio M A, Getrajdman G I, Brown K T. Variant hepatic arterial anatomy revisited: digital subtraction angiography performed in 600 patients. Radiology. 2002;224(2):542–547. doi: 10.1148/radiol.2242011283. [DOI] [PubMed] [Google Scholar]
- Koç Z, Oğuzkurt L, Ulusan S. Portal vein variations: clinical implications and frequencies in routine abdominal multidetector CT. Diagn Interv Radiol. 2007;13(2):75–80. [PubMed] [Google Scholar]
- Gallego C, Velasco M, Marcuello P, Tejedor D, De Campo L, Friera A. Congenital and acquired anomalies of the portal venous system. Radiographics. 2002;22(1):141–159. doi: 10.1148/radiographics.22.1.g02ja08141. [DOI] [PubMed] [Google Scholar]
- Song S Y, Chung J W, Kwon J W, et al. Collateral pathways in patients with celiac axis stenosis: angiographic-spiral CT correlation. Radiographics. 2002;22(4):881–893. doi: 10.1148/radiographics.22.4.g02jl13881. [DOI] [PubMed] [Google Scholar]
- Fisher D F, Jr, Fry W J. Collateral mesenteric circulation. Surg Gynecol Obstet. 1987;164(5):487–492. [PubMed] [Google Scholar]
- Horton K M, Fishman E K. Volume-rendered 3D CT of the mesenteric vasculature: normal anatomy, anatomic variants, and pathologic conditions. Radiographics. 2002;22(1):161–172. doi: 10.1148/radiographics.22.1.g02ja30161. [DOI] [PubMed] [Google Scholar]
- Gourley E J, Gering S A. The meandering mesenteric artery: a historic review and surgical implications. Dis Colon Rectum. 2005;48(5):996–1000. doi: 10.1007/s10350-004-0890-7. [DOI] [PubMed] [Google Scholar]
- Lin P H, Chaikof E L. Embryology, anatomy, and surgical exposure of the great abdominal vessels. Surg Clin North Am. 2000;80(1):417–433, xiv. doi: 10.1016/s0039-6109(05)70413-8. [DOI] [PubMed] [Google Scholar]
- Rosenblum J D, Boyle C M, Schwartz L B. The mesenteric circulation. Anatomy and physiology. Surg Clin North Am. 1997;77(2):289–306. doi: 10.1016/s0039-6109(05)70549-1. [DOI] [PubMed] [Google Scholar]