Abstract
Background
Melatonin appears to play a role in breast cancer etiology, but data addressing the association between melatonin levels and breast cancer risk in postmenopausal women is sparse.
Methods
We conducted a nested case-control study in the Nurses’ Health Study cohort. First spot morning urine was collected from 18,643 cancer-free women from March 2000 through December 2002. The concentration of melatonin’s major metabolite, 6-sulfatoxymelatonin (aMT6s), was available for 357 postmenopausal women who developed incident breast cancer through May 31, 2006, along with 533 matched control subjects. We used multivariable conditional logistic regression models to investigate associations. All statistical tests were two-sided.
Results
An increased concentration of urinary aMT6s was statistically significantly associated with a lower risk of breast cancer (odds ratio [OR] for the highest versus lowest quartile of morning urinary 6-sulfatoxymelatonin = 0.62, 95% confidence interval [CI] = 0.41 to 0.95; P[trend] = .004). There was no apparent modification of risk by hormone receptor status of breast tumors, age, body-mass index, or smoking status.
Conclusion
Results from this prospective study add substantially to the growing literature that supports an inverse association between melatonin levels and breast cancer risk.
Keywords: melatonin, aMT6s, breast cancer
INTRODUCTION
The indoleamine hormone melatonin (N-acetyl-5-methoxytrptamine) is produced primarily by the pineal gland in humans, in a circadian fashion: Throughout the day, melatonin production remains very low, until it increases in the evening and peaks between 2 and 4 a.m., then gradually declines. Melatonin is metabolized by the liver (90% at first pass) and mainly excreted in the urine. Melatonin’s major urinary metabolite, 6-sulfatoxymelatonin (aMT6s), as measured in the first morning urine specimen, is closely correlated with peak plasma melatonin levels measured during the previous night (1, 2). In contrast to single plasma or saliva melatonin measures, a single measure of aMT6s in morning urine allows determination of nightly peak levels of melatonin (2).
Substantial laboratory evidence lends support to an important role of melatonin in cancer etiology (3). Recently, Blask et al. demonstrated that melatonin-depleted blood of healthy premenopausal women enhanced breast tumor growth in rodent models, in contrast to melatonin-rich blood, which reduced proliferative activity (4). While the exact mechanism of the oncostatic properties of melatonin is still being examined, studies suggest antiestrogenic actions of melatonin, both through down-regulation of the hypothalamic-pituitary reproductive axis, resulting in a reduction of circulating estrogen levels (5), and through direct actions of melatonin at the tumor cell level, by interfering at different levels with the estrogen signaling pathway (6). Because melatonin appears to act antiestrogenically not via binding to the estrogen receptor, but rather by binding to its own membrane receptors, it is able to interact with the estrogen receptor signaling pathway (7, 8). It is currently thought that melatonin decreases the expression of ERα and hinders the binding of the estradiol-Erα complex to the estrogen response element on DNA (9–11), effects that have been shown to be dependent on melatonin binding to specific melatonin (MT1) membrane receptors (which have also been found in breast tissue) (6).
Indirect evidence from observational studies (12, 13) also suggests an association between melatonin suppression, using surrogates for light exposure at night, and breast cancer risk. However, to date, only three prospective studies (14–16) have directly examined the association between melatonin levels and breast cancer risk in humans and results were inconsistent. One study reported no evidence for an association (17); however, that study used 24-hour urine samples, which may not reflect average nightly melatonin levels (the peak of physiologic melatonin production). The other two studies used first morning urine (14) and 12 hour overnight urine (16), and both found that melatonin levels were inversely associated with the risk of breast cancer.
We used a nested case–control design to conduct a prospective study of the association between melatonin levels in the first morning urine specimen and breast cancer risk among postmenopausal women enrolled in the Nurses’ Health Study cohort. We evaluated the associations in postmenopausal women between creatinine-adjusted 6-sulfatoxymelatonin level and breast cancer risk.
STUDY POPULATION AND METHODS
Study Population
In 1976, 121,700 female registered nurses from 11 large U.S. states, ages 30 to 55 and of primarily Caucasian descent, were enrolled in the Nurses’ Health Study (NHS). Since baseline they have completed biennial mailed questionnaires that comprise items about their health status, medical history, and known or suspected risk factors for cancer (18) and heart disease (19). Every two years, follow-up questionnaires have been sent to cohort members to update the information on potential risk factors and to identify new diagnoses of cancer and other major medical events. Between 1989 and 1990, blood samples were collected from 32,826 women. Further details of the NHS blood collection methods have been previously published (20, 21). Following identical procedures, from March 2000 through December 2002 a second blood collection was conducted among 18,706 women, 18,643 (99.7%) of whom also provided a first spot morning urine sample along with their blood.
Cases in this analysis are women with no cancer diagnosis (with the exception of non-melanoma skin cancer) prior to urine collection and for whom breast cancer was reported anytime after urine collection up to May 31, 2006. Further details of the case identification procedures have been provided elsewhere (22). To each case, we matched 1 (for each postmenopausal case with postmenopausal hormone use) to 2 (all other cases) controls on their year of birth, menopausal status (postmenopausal versus not), recent postmenopausal hormone (PMH) use defined as use within 3 months of urine collection versus not, month and time of day of urine collection, and fasting status at urine draw (≥ 10 hrs since a meal versus not). A woman was defined as postmenopausal if she reported a natural menopause or bilateral oophorectomy or if she was at least 56 years old (if a non-smoker) or 54 years old (if a current smoker) after hysterectomy without bilateral oophorectomy – by these ages natural menopause had occurred in 90% of the cohort. The study was approved by the Committee on the Use of Human Subjects in Research at the Brigham and Women’s Hospital.
Specimen and Questionnaire Data Collection
Blood draw and a spot morning urine sample were collected on the same day. Collections were not timed within the menstrual cycle (random samples), since over 99% of the cohort were postmenopausal at the time of collection. Each woman was sent a questionnaire on which to record the date and time of urine collection (i.e., whether samples were first spot morning urine or not). In addition, information was gathered on participant’s current weight, current smoking status, and other life-style variables. Information on more detailed life-style factors associated with health, including reproductive history, were available for each participant from the biennial NHS questionnaires completed in 2000. In addition, we queried the women on difficulty sleeping (all the time, most of the time or good bit of difficulties; some or a little difficulty; none) and total hours slept/day, along with information on how often a women snored (every night, most nights, few nights, to almost never) on the 2000 questionnaire.
Urine specimens from women with breast cancer and matched control subjects were handled identically and assayed together on the same day and in the same run. All samples were taken out of the freezer simultaneously and sent to the laboratory in the same parcel on dry ice. Until then, all specimens had been stored in the vapor phase of nitrogen freezers (at – 130 °C or colder). Laboratory personnel were blinded to case–control status of all specimens. Analytic error was assessed by including masked quality controls in each assay batch.
Urinary aMT6s was assayed by the Endocrine Core Laboratory of Dr. M. Wilson (Yerkes National Primate Research Center, Emory University, Atlanta, GA), using the Bühlmann enzyme-linked immunosorbent assay (ALPCO, Windham, NH) with a lower detection limit of 0.8 ng/mL for aMT6s. Creatinine levels were also measured for each sample by the same laboratory, using creatinine reagents purchased from Sigma Diagnostics, and aMT6s levels were normalized to the creatinine level of the sample to account for differences arising from variations in urine concentrations. The average within-batch coefficient of variation was 9.5% and 10.3% (first and second batch, respectively) for urinary aMT6s, and 8.5% and 3.1% (first and second batch, respectively) for creatinine.
Statistical Analyses
Samples were not available for one case and eight controls because of low urine volume, thus, there were 372 incident breast cancer cases and 598 matched controls available for these analyses and sent to the laboratory. Of these, melatonin values were missing for 11 women and creatinine level was missing for one woman due to assay problems. Further, we identified the melatonin values of six women as statistical outliers based on the generalized extreme studentized deviate many-outlier detection approach (23). This resulted in 366 women with breast cancer and their 586 matched controls. We based our primary analyses on women who were postmenopausal at the time of urine collection, excluding the small proportion (9 cases subjects and 53 control subjects) of women who were still premenopausal or of uncertain menopause status at urine collection. Pathology records were obtained for all remaining 357 cases. In total, 276 were pathologically confirmed invasive breast cancers and 79 were in situ cancers. Although pathology reports had not yet been obtained for 2 of the 276 women, we included them in our analyses because the accuracy of self-reported breast cancer in this cohort is extremely high (99%) (24). Thus, after all exclusions, 357 postmenopausal women with breast cancer and their 533 matched controls with valid melatonin values remained in our final data set. Of these, 27 women had 6-sulfatoxymelatonin levels that were below the limit of detection for the assay (i.e., <0.8 ng/mL); they were retained in the analyses, with their values conservatively set to 0.8ng/mL. 6-sulfatoxymelatonin levels were normalized to the creatinine level of the sample to account for differences arising from variations in urine concentrations (expressed as ng of 6-sulfatoxymelatonin per mg of creatinine).
In sub-analyses, we excluded women with in situ cancers or current smokers (at the time of urine collection) and stratified by tumor receptor status. To test for differences in hormone levels between case patient and control subjects, we used mixed-effects regression models for clustered data to adjust for possible confounding due to the matching factors and for any residual correlation between case patients and control subjects within the matched set (25). We used conditional regression models to estimate the relative risks of breast cancer (reported as odds ratios [ORs] with 95% confidence intervals [CIs]) by quartiles of urinary 6-sulfatoxymelatonin concentrations, which were derived from urinary 6-sulfatoxymelatonin values for all control subjects. In our primary analyses, these quartiles were based on cut points based on all controls. Since melatonin was assayed in two different batches (sent in 2007 and 2008) and levels varied slightly between them, we also created batch-specific cut points in secondary analyses; however, results were essentially unchanged when using this approach and we therefore based our main analyses on overall cut points. Multivariable models were adjusted for known or possible breast cancer risk factors, including body mass index (≤23, 23–24.9, 25–28.9, or ≥ 29 kg/m2), history of benign breast disease (yes or no), family history (mother or sister) of breast cancer (yes or no), smoking history (current smoker, yes or no), age at menarche (<12, 13, 14, or >14 years), age at menopause (≤45, 46–50, 51–55, or >55 years), alcohol consumption (none or less than one drink/day, or 1+ drinks/day), current hormone replacement therapy use (yes or no), parity (nulliparous or 1–2 or 3–4 or ≥ 5 children), first spot morning urine (yes or no), and current use of antidepressants (yes or no). We tested for trends by modeling natural 6-sulfatoxymelatonin concentrations continuously and calculating the Wald statistic. We examined the possibly non-linear relationship between aMT6s and breast cancer risk non-parametrically with restricted cubic splines (26). Tests for non-linearity used the likelihood ratio test, comparing the model with only the linear term to the model with the linear and the cubic spline terms. We used SAS version 9.1.3 (Cary, NC) for all analyses. We tested for heterogeneity by tumor invasiveness using polytomous unconditional logistic regression methods. All P values were two-sided.
RESULTS
Baseline Characteristics
Baseline characteristics of the 357 postmenopausal case patients and 533 control subjects are shown in Table 1. The mean time between urine collection and diagnosis was 30 months (±18 months, SD) with a range of 1–73 months. Women were 54 to 80 years old at urine collection (mean age, 67 years). Most baseline characteristics did not differ by case–control status (Table 1). However, the creatinine-adjusted mean urinary 6-sulfatoxymelatonin levels for the case patients with breast cancer was slightly lower than that for control subjects (24.5 ng of 6-sulfatoxymelatonin per mg of creatinine versus 28.8 ng of 6-sulfatoxymelatonin per mg of creatinine).
Table 1.
Baseline characteristicsof 357 postmenopausal† breast cancer case patients and 533 matched control subjects (in 2000) *
| Characteristic | Case patients (n = 357) | Control subjects (n = 533) |
|---|---|---|
| Mean age, y (SD) | 67.2 (6.7) | 67.2 (6.7) |
| Mean age at menarche, y (SD) | 12.6 (1.4) | 12.6 (1.4) |
| Mean age at menopause†, y (SD) | 48.4 (6.0) | 47.5 (6.5) |
| Mean No. of births‡ (SD) | 3.2 (1.4) | 3.2 (1.6) |
| Family history of breast cancer, % | 23.8 | 16.1 |
| Mean BMI, kg/m2 (SD) | 26.9 (5.0) | 26.4 (5.0) |
| Mean amount of alcohol consumed/day, gm (SD) | 6.3 (9.8) | 5.4 (9.1) |
| Current smoker, % | 5.6 | 4.1 |
| History of benign breast disease, % | 64.2 | 60.6 |
| Current antidepressant use, % | 12.4 | 13.1 |
| Postmenopausal hormones ever used, % | 67.2 | 58.9 |
| First morning urine, % | 95.8 | 94.6 |
| Frequently difficulty sleeping, % | 10.8 | 11.3 |
| Frequently snores, % | 21.1 | 18.5 |
| Avg. hours of sleep/day 5 or less hours, % | 6.8 | 3.0 |
| Mean aMT6s level, ng/mg creatinine (SD) | 24.5 (29) | 28.8 (39) |
| Mean creatinine level, mmol/L (SD) | 6.1 (3.8) | 5.5 (3.4) |
SD = standard deviation; BMI = body mass index.
Natural menopause or menopause due to bilateral oophorectomy.
Among parous women only.
Urinary 6-sulfatoxymelatonin Levels and Breast Cancer Risk
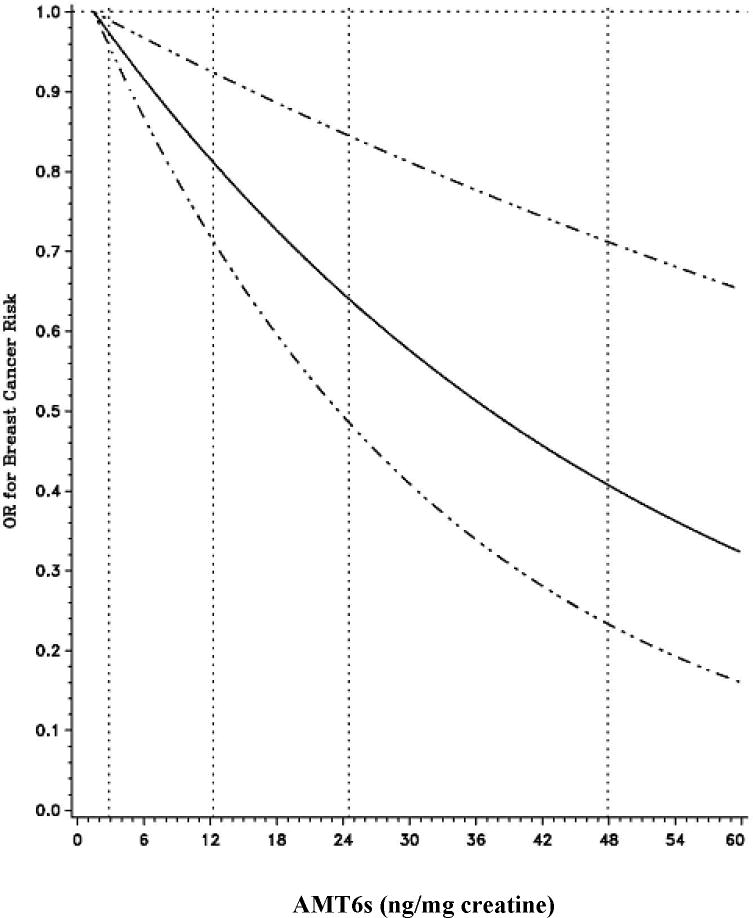
We observed an inverse association between urinary 6-sulfatoxymelatonin levels and breast cancer risk (for highest versus lowest quartile of urinary 6-sulfatoxymelatonin concentration, OR = 0.81, 95% CI = 0.60 to 1.09; Ptrend = 0.07; Table 2), a finding which became statistically significant after additional adjustment for breast cancer risk factors (OR = 0.62, 95% CI = 0.41–0.95; Ptrend = 0.004). The main confounders in these analyses were age at menopause, a family history of breast cancer, and smoking status. We fitted restricted cubic splines to our conditional logistic regression model to examine non-parametrically the possibly non-linear relationship between aMT6s and breast cancer risk. However, the test for curvature (i.e., non-linear relationship) from these analyses was 0.59, whereas the test for a linear relationship was 0.002, suggesting that the association between aMT6s and breast cancer risk follows a linear relationship (Figure 1).
Table 2.
Odds ratios (ORs) and 95% confidence intervals of breast cancer by quartile of urinary 6-sulphatoxymelatonin (aMT6s) level among 890 postmenopausal women
| Group and parameter | Quartile |
||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Ptrend† | |
| Urinary aMT6s, ng/mg creatinine | <10.2 | 10.2–21.4 | 21.5–34.2 | ≥34.3 | |
| Invasive and in situ cancers combined | |||||
| No. of case patients/No. of control subjects | 107/136 | 109/128 | 66/134 | 75/135 | |
| Simple OR‡ | 1.0 | 1.04 (0.80–1.36) | 0.75 (0.55–1.02) | 0.81 (0.60–1.09) | 0.07 |
| Multivariable OR§ | 1.0 | 1.08 (0.73–1.59) | 0.58 (0.38–0.88) | 0.62 (0.41–0.95) | 0.004 |
| Invasive cancers only | |||||
| No. of case patients/No. of control subjects | 82/110 | 85/100 | 52/101 | 59/103 | |
| Simple OR‡ | 1.0 | 1.08 (0.79–1.46) | 0.80 (0.56–1.13) | 0.85 (0.61–1.19) | 0.11 |
| Multivariable OR§ | 1.0 | 1.17 (0.75–1.83) | 0.70 (0.43–1.12) | 0.74 (0.46–1.21) | 0.03 |
| In situ cancers only | |||||
| No. of case patients/No. of control subjects | 25/26 | 24/28 | 14/33 | 16/32 | |
| Simple OR‡ | 1.0 | 0.94 (0.54–1.65) | 0.61 (0.32–1.17) | 0.68 (0.36–1.27) | 0.36 |
| Multivariable OR§ | 1.0 | 1.00 (0.36–2.79) | 0.24 (0.08–0.71) | 0.23 (0.08–0.69) | 0.03 |
We tested for trends by modeling log-transformed aMT6s concentrations continuously and calculating the Wald statistic.
Simple conditional logistic regression model.
Multivariable conditional logistic regression models adjusted for the following breast cancer risk factors: body mass index in four categories (≤23, 23–24.9, 25–28.9, or ≥ 29 kg/m2), history of benign breast disease (yes or no), family history (mother or sister) of breast cancer (yes or no), smoking history (current smoker, yes or no), age at menarche in four categories (<12, 13, 14, or >14 years), age at menopause in four categories (≤45, 46–50, 51–53, or >53 years), alcohol consumption (none or less than one drink/day, or 1+ drinks/day), current hormone replacement therapy use (yes or no), parity (nulliparous or 1–2 or 3–4 or ≥ 5 children), first spot morning urine (yes or no), and current use of antidepressants (yes or no).
Figure 1.
Smoothing spline plot for aMT6s level (ng/mg creatinine) in relation to breast cancer risk among postmenopausal women. 95% confidence intervals (CI) are indicated by dotted lines.
Night work and melatonin have been more strongly related to invasive than in situ breast cancer risk (14, 27–29). Thus, in secondary analyses, we excluded 79 case patients who were diagnosed with in situ breast cancer and their matched control subjects. Among women with invasive breast cancer, the inverse association was slightly weaker, although overall very similar (for highest versus lowest quartile of urinary 6-sulfatoxymelatonin concentration, multivariable OR = 0.74, 95% CI = 0.46 to 1.21; Ptrend = 0.03). In the small subset of women with in situ cancers, the effect of higher aMT6s levels appeared more pronounced though based on only 16 cases in the top quartile (for highest versus lowest quartile of urinary 6-sulfatoxymelatonin concentration, multivariable OR = 0.23, 95% CI = 0.08 to 0.69; Ptrend = 0.03; Table 2; Pheterogeneity = 0.92).
On the basis of a previous study (30) indicating that an increased level of nocturnal plasma melatonin was inversely associated with tumor estrogen receptor concentration, we conducted analyses stratified on estrogen receptor status. Hormone receptor status was available for 76% of all case patients with breast cancer; 226 (83%) of the 273 tumors for which estrogen receptor status was available were estrogen receptor-positive (only 43 women had estrogen receptor-negative breast tumors). When we restricted analysis to women with estrogen receptor-positive breast tumors, the significant inverse association between 6-sulfatoxymelatonin and breast cancer risk remained by and large unchanged (for highest versus lowest quartile of urinary 6-sulfatoxymelatonin, multivariable OR = 0.62, 95% CI = 0.36 to 1.09, P for trend 0.01). Although there were only ten case patients in the upper quartile, the risk of estrogen receptor-negative breast cancer appeared lowest among women in the highest quartile of 6-sulfatoxymelatonin concentration (for highest versus lowest quartile of urinary 6-sulfatoxymelatonin, multivariable OR = 0.64, 95% CI = 0.31 to 1.32). For a subgroup of women (71%), information on HER2 receptor status was also available. Of these, only 39 women had HER2 positive breast tumors. Although with limited power, in stratified analyses, results appeared similar regardless of HER2 receptor status (data not shown).
Because sleep duration may influence absolute melatonin production, we also examined associations between sleep-related variables and urinary aMT6s levels. While we did not observe substantial differences in aMT6s concentration by level of difficulty sleeping or frequency of snoring, women who slept on average longer appeared to have somewhat lower aMT6s levels than those with fewer hours of sleep reported (aMT6s concentration, geometric mean adjusted for age, 9+ hours of sleep, 14.6 ng/mg creatinine versus 6 or less hours of sleep, 18.0 ng/mg creatinine). However, adjusting for sleep duration, difficulty sleeping, and snoring did not alter our estimates materially. Moreover, the association between melatonin and breast cancer risk did not vary by hours slept (7 or less vs. 8 or more), age (<67 vs. ≥ 67 years old), body mass index (stratified along the median, 25.5 kg/m2), or smoking status. To exclude the possibility of preclinical tumors influencing our 6-sulfatoxymelatonin levels, in subset analyses we excluded case patients diagnosed with breast cancer within one or two years of urine collection. In these subset analyses, the strength of the association between urinary 6-sulfatoxymelatonin level and breast cancer risk remained similar (for highest versus lowest quartile of urinary 6-sulfatoxymelatonin concentration and risk of breast cancer, excluding cases diagnosed within one year, OR = 0.72, 95% CI = 0.45 to 1.17; Ptrend .03; or two years after urine collection, OR = 0.76, 95% CI = 0.44 to 1.31; Ptrend .05) after urine collection.
Urinary creatinine concentration is influenced by a number of factors, including sex, ethnicity, age, and body mass index (31). Although our study was composed of white women exclusively, differences in age and body mass index may have biased our creatinine-adjusted 6-sulfatoxymelatonin measure. We found a modest correlation between the creatinine-adjusted 6-sulfatoxymelatonin level and creatinine level (Spearman r = − 0.19 and P < 0.001) in our data, indicating that adjusting our aMT6s levels for creatinine may not appropriately have corrected for urine concentration. We, therefore, repeated our analyses using aMT6s concentration unadjusted for creatinine with urinary creatinine added as a separate independent variable to our multiple regression models, as suggested by Barr et al. (31), but results were unchanged (data not shown).
DISCUSSION
We found a statistically significant inverse association between first morning urinary 6-sulfatoxymelatonin level and breast cancer risk in this large group of postmenopausal women. Among the 4,661 (25% of 18,643) women in the highest 6-sulfatoxymelatonin quartile, 75 developed breast cancer during follow-up (average follow-up = 2.4 years), compared with 107 of the 4,661 (25%) women in the lowest 6-sulfatoxymelatonin quartile.
While several prior studies evaluated the association between circulating melatonin levels and breast cancer risk in women, their results have been inconsistent; however, these studies are severely hampered by their retrospective design and their small case numbers, making interpretation difficult (30, 32–42). Three prospective studies, to date, have been conducted and they also produced inconsistent results. The first study (17), which used 24-hour urine specimens and comprised 127 cases and 353 control subjects, reported no association between the circulating level of 6-sulfatoxymelatonin and breast cancer risk (OR = 0.99, 95% CI = 0.58 to 1.70, comparing the highest tertile with the lowest tertile of aMT6s concentration). Whether 24-hour urine samples are the right sample to capture the nocturnal melatonin peak has been questioned subsequently (43). In the Nurses’ Health Study II (14), first spot morning urine specimens were used. A strong inverse association between levels of 6-sulfatoxymelatonin in first morning urine specimens and breast cancer risk was reported in the 147 premenopausal women with invasive breast cancer and their 291 matched controls (OR = 0.59, 95% CI = 0.36 to 0.97, comparing the highest quartile with the lowest quartile of aMT6s concentration). Most recently, in the Hormones and Diet in the Etiology of Breast Cancer Risk (ORDET) cohort, a similarly strong inverse association between 6-sulfatoxymelatonin output as measured in 12 hour overnight urine specimen and breast cancer risk was observed in their postmenopausal women (OR = 0.56, 95% CI = 0.33 to 0.97 for women in the highest quartile of total overnight 6-sulfatoxymelatonin output vs. the lowest quartile) (16).
Our results are in complete agreement with the two more recently published studies using either first morning or overnight urine (14, 16). Moreover, while based on few cases, our study suggests that circulating melatonin level might be more strongly related to in situ than invasive breast tumors. However, it is not entirely clear how frequently in situ tumors progress to invasive tumors (44, 45). No prior study has been able to address the association between melatonin and in situ breast tumors. Thus, while plausible, our finding of a stronger effect of endogenous melatonin on in situ tumors, requires replication in a larger data set to rule out a chance finding.
Strengths of our study are that we were able to consider most important breast cancer risk factors, including sleep duration and night work in our analyses. When we adjusted for life-time duration of night work, which was queried in 1988, results remained unchanged. Excluding case patients who were diagnosed within the first 2 years after urine collection did not alter our findings; however, the short follow-up (2.5 years average) in our study limited our ability to address this fully. Our study is further limited by the lack of information on circulating sex steroid levels. Finally, we were unable to correct for laboratory measurement error and within-person variability in our data set; however, because of the random nature of this error, we expect that this correction would have strengthened our observed risks. Moreover, the intra-class correlation over a 3 year period in premenopausal women from the Nurses’ Health Study II cohort was fairly high (0.72), suggesting that melatonin remains fairly stable over time (46).
In summary, our findings show that melatonin secretion, as assessed by first morning urinary 6-sulfatoxymelatonin concentration, is associated with the risk of developing breast cancer in postmenopausal women. Studies to confirm our findings should have longer follow-up and should also address the importance of interrelationships with sex steroids in these associations.
Acknowledgments
This research was supported by National Cancer Institute Grants CA/ES62984, CA87969, CA49449, and CA67262. We thank Susie Lacky and her colleagues at the Endocrine Core Laboratory, Yerkes Primate Research Center, Emory University, for collaboration on this project. We are also indebted to Helena Ellis for her technical assistance.
References
- 1.Baskett JJ, Cockrem JF, Antunovich TA. Sulphatoxymelatonin excretion in older people: relationship to plasma melatonin and renal function. J Pineal Res. 1998;24:58–61. doi: 10.1111/j.1600-079x.1998.tb00366.x. [DOI] [PubMed] [Google Scholar]
- 2.Graham C, Cook MR, Kavet R, Sastre A, Smith DK. Prediction of nocturnal plasma melatonin from morning urinary measures. J Pineal Res. 1998;24:230–238. doi: 10.1111/j.1600-079x.1998.tb00538.x. [DOI] [PubMed] [Google Scholar]
- 3.Vijayalaxmi, Thomas CR, Jr, Reiter RJ, Herman TS. Melatonin: from basic research to cancer treatment clinics. J Clin Oncol. 2002;20:2575–601. doi: 10.1200/JCO.2002.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Blask DE, Brainard GC, Dauchy RT, Hanifin JP, Davidson LK, Krause JA, Sauer LA, Rivera-Bermudez MA, Dubocovich ML, Jasser SA, Lynch DT, Rollag MD, Zalatan F. Melatonin-depleted blood from premenopausal women exposed to light at night stimulates growth of human breast cancer xenografts in nude rats. Cancer Res. 2005;65:11174–11184. doi: 10.1158/0008-5472.CAN-05-1945. [DOI] [PubMed] [Google Scholar]
- 5.Stevens RG. Electric power use and breast cancer: a hypothesis. Am J Epidemiol. 1987;125:556–561. doi: 10.1093/oxfordjournals.aje.a114569. [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez A, Martinez-Campa C, Mediavilla MD, Alonso-Gonzalez C, Sanchez-Mateos S, Hill SM, Sanchez-Barcelo EJ, Cos S. Effects of MT1 melatonin receptor overexpression on the aromatase-suppressive effect of melatonin in MCF-7 human breast cancer cells. Oncol Rep. 2007;17:947–53. doi: 10.3892/or.17.4.947. [DOI] [PubMed] [Google Scholar]
- 7.Ram PT, Dai J, Yuan L, Dong C, Kiefer TL, Lai L, Hill SM. Involvement of the mt1 melatonin receptor in human breast cancer. Cancer Lett. 2002;179:141–150. doi: 10.1016/s0304-3835(01)00873-4. [DOI] [PubMed] [Google Scholar]
- 8.Yuan L, Collins AR, Dai J, Dubocovich ML, Hill SM. MT(1) melatonin receptor overexpression enhances the growth suppressive effect of melatonin in human breast cancer cells. Mol Cell Endocrinol. 2002;192:147–156. doi: 10.1016/s0303-7207(02)00029-1. [DOI] [PubMed] [Google Scholar]
- 9.Molis TM, Spriggs LL, Hill SM. Modulation of estrogen receptor mRNA expression by melatonin in MCF-7 human breast cancer cells. Mol Endocrinol. 1994;8:1681–1690. doi: 10.1210/mend.8.12.7708056. [DOI] [PubMed] [Google Scholar]
- 10.Rato AG, Pedrero JG, Martinez MA, del Rio B, Lazo PS, Ramos S. Melatonin blocks the activation of estrogen receptor for DNA binding. FASEB Journal. 1999;13:857–868. doi: 10.1096/fasebj.13.8.857. [DOI] [PubMed] [Google Scholar]
- 11.Lawson NO, Wee BE, Blask DE, Castles CG, Spriggs LL, Hill SM. Melatonin decreases estrogen receptor expression in the medial preoptic area of inbred (LSH/SsLak) golden hamsters. Biol Reprod. 1992;47:1082–1090. doi: 10.1095/biolreprod47.6.1082. [DOI] [PubMed] [Google Scholar]
- 12.Straif K, Baan R, Grosse Y, Secretan B, Ghissassi FE, Bouvard V, Altieri A, Benbrahim-Ballaa L, Cogliano V Group., O. b. o. t. W. I. A. f. R. o. C. M. W. Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol. 2007;8:1065–1066. doi: 10.1016/S1470-2045(07)70373-X. [DOI] [PubMed] [Google Scholar]
- 13.Stevens RG, Blask DE, Brainard GC, Hansen J, Lockley SW, Provencio I, Rea MS, Reinlib L. Meeting report: the role of environmental lighting and circadian disruption in cancer and other diseases. Environ Health Perspect. 2007;115:1357–62. doi: 10.1289/ehp.10200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schernhammer ES, Hankinson SE. Urinary melatonin levels and breast cancer risk. J Natl Cancer Inst. 2005;97:1084–1087. doi: 10.1093/jnci/dji190. [DOI] [PubMed] [Google Scholar]
- 15.Travis RC, Allen DS, Fentiman IS, Key TJ. Melatonin and breast cancer: a prospective study. J Natl Cancer Inst. 2004;96:475–82. doi: 10.1093/jnci/djh077. [DOI] [PubMed] [Google Scholar]
- 16.Schernhammer ES, Berrino F, Krogh V, Secreto G, Micheli A, Venturelli E, Sieri S, Sempos CT, Cavalleri A, Schunemann HJ, Strano S, Muti P. Urinary 6-Sulfatoxymelatonin Levels and Risk of Breast Cancer in Postmenopausal Women. J Natl Cancer Inst. 2008 doi: 10.1093/jnci/djn171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Travis RC, Allen DS, Fentiman IS, Key TJ. Melatonin and breast cancer: a prospective study. J Nat Cancer Inst. 2004;96:475–482. doi: 10.1093/jnci/djh077. [DOI] [PubMed] [Google Scholar]
- 18.Willett WC, Stampfer MJ, Colditz GA, Rosner BA, Hennekens CH, Speizer FE. Dietary fat and the risk of breast cancer. N Engl J Med. 1987;316:22–28. doi: 10.1056/NEJM198701013160105. [DOI] [PubMed] [Google Scholar]
- 19.Stampfer MJ, Willett WC, Colditz GA, Rosner B, Speizer FE, Hennekens CH. A prospective study of postmenopausal estrogen therapy and coronary heart disease. N Engl J Med. 1985;313:1044–1049. doi: 10.1056/NEJM198510243131703. [DOI] [PubMed] [Google Scholar]
- 20.Hankinson SE, Willett WC, Manson JE, Colditz GA, Hunter DJ, Spiegelman D, Barbieri RL, Speizer FE. Plasma sex steroid hormone levels and risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 1998;90:1292–1299. doi: 10.1093/jnci/90.17.1292. [DOI] [PubMed] [Google Scholar]
- 21.Hankinson SE, Willett WC, Colditz GA, Hunter DJ, Michaud DS, Deroo B, Rosner B, Speizer FE, Pollak M. Circulating concentrations of insulin-like growth factor-I and risk of breast cancer. Lancet. 1998;351:1393–1396. doi: 10.1016/S0140-6736(97)10384-1. [DOI] [PubMed] [Google Scholar]
- 22.Adebamowo CA, Cho E, Sampson L, Katan MB, Spiegelman D, Willett WC, Holmes MD. Dietary flavonols and flavonol-rich foods intake and the risk of breast cancer. Int J Cancer. 2005;114:628–633. doi: 10.1002/ijc.20741. [DOI] [PubMed] [Google Scholar]
- 23.Rosner B. Percentage points for a generalized ESD many-outlier procedure. Technometrics. 1983;25:165–172. [Google Scholar]
- 24.Willett WC, Browne ML, Bain C, Lipnick RJ, Stampfer MJ, Rosner B, Colditz GA, Hennekens CH, Speizer FE. Relative weight and risk of breast cancer among premenopausal women. Am J Epidemiol. 1985;122:731–740. doi: 10.1093/oxfordjournals.aje.a114156. [DOI] [PubMed] [Google Scholar]
- 25.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
- 26.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 27.Schernhammer ES, Laden F, Speizer FE, Willett WC, Hunter DJ, Kawachi I, Colditz GA. Rotating night shifts and risk of breast cancer in women participating in the Nurses’ Health Study. J Natl Cancer Inst. 2001;93:1563–1568. doi: 10.1093/jnci/93.20.1563. [DOI] [PubMed] [Google Scholar]
- 28.Davis S, Mirick DK, Stevens RG. Night shift work, light at night, and risk of breast cancer. J Natl Cancer Inst. 2001;93:1557–1562. doi: 10.1093/jnci/93.20.1557. [DOI] [PubMed] [Google Scholar]
- 29.Hansen J. Increased breast cancer risk among women who work predominantly at night. Epidemiology. 2001;12:74–77. doi: 10.1097/00001648-200101000-00013. [DOI] [PubMed] [Google Scholar]
- 30.Tamarkin L, Danforth D, Lichter A, DeMoss E, Cohen M, Chabner B, Lippman M. Decreased nocturnal plasma melatonin peak in patients with estrogen receptor positive breast cancer. Science. 1982;216:1003–1005. doi: 10.1126/science.7079745. [DOI] [PubMed] [Google Scholar]
- 31.Barr DB, Wilder LC, Caudill SP, Gonzalez AJ, Needham LL, Pirkle JL. Urinary creatinine concentrations in the U.S. population: implications for urinary biologic monitoring measurements. Environ Health Perspect. 2005;113:192–200. doi: 10.1289/ehp.7337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bartsch C, Bartsch H, Bellmann O, Lippert TH. Depression of serum melatonin in patients with primary breast cancer is not due to an increased peripheral metabolism. Cancer. 1991;67:1681–1684. doi: 10.1002/1097-0142(19910315)67:6<1681::aid-cncr2820670634>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 33.Bartsch C, Bartsch H, Fuchs U, Lippert TH, Bellmann O, Gupta D. Stage-dependent depression of melatonin in patients with primary breast cancer. Correlation with prolactin, thyroid stimulating hormone, and steroid receptors. Cancer. 1989;64:426–433. doi: 10.1002/1097-0142(19890715)64:2<426::aid-cncr2820640215>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 34.Bartsch C, Bartsch H, Jain AK, Laumas KR, Wetterberg L. Urinary melatonin levels in human breast cancer patients. J Neural Transm. 1981;52:281–294. doi: 10.1007/BF01256753. [DOI] [PubMed] [Google Scholar]
- 35.Bartsch C, Bartsch H, Karenovics A, Franz H, Peiker G, Mecke D. Nocturnal urinary 6-sulphatoxymelatonin excretion is decreased in primary breast cancer patients compared to age-matched controls and shows negative correlation with tumor-size. J Pineal Res. 1997;23:53–58. doi: 10.1111/j.1600-079x.1997.tb00335.x. [DOI] [PubMed] [Google Scholar]
- 36.Danforth DNJ, Tamarkin L, Mulvihill JJ, Bagley CS, Lippman ME. Plasma melatonin and the hormone-dependency of human breast cancer. J Clin Oncol. 1985;3:941–948. doi: 10.1200/JCO.1985.3.7.941. [DOI] [PubMed] [Google Scholar]
- 37.Falkson G, Falkson HC, Steyn ME, Rapoport BL, Meyer BJ. Plasma melatonin in patients with breast cancer. Oncology. 1990;47:401–405. doi: 10.1159/000226857. [DOI] [PubMed] [Google Scholar]
- 38.Lissoni P, Bastone A, Sala R, Mauri R, Rovelli F, Viviani S, Bajetta E, Esposti D, Esposti G, di Bella L, et al. The clinical significance of melatonin serum determination in oncological patients and its correlations with GH and PRL blood levels. Eur J Cancer Clin Oncol. 1987;23:949–957. doi: 10.1016/0277-5379(87)90340-3. [DOI] [PubMed] [Google Scholar]
- 39.Lissoni P, Crispino S, Barni S, Sormani A, Brivio F, Pelizzoni F, Brenna A, Bratina G, Tancini G. Pineal gland and tumor cell kinetics: serum levels of melatonin in relation to Ki-67 labeling rate in breast cancer. Oncology. 1990;47:275–277. doi: 10.1159/000226831. [DOI] [PubMed] [Google Scholar]
- 40.Skene DJ, Bojkowski CJ, Currie JE, Wright J, Boulter PS, Arendt J. 6-sulphatoxymelatonin production in breast cancer patients. J Pineal Res. 1990;8:269–276. doi: 10.1111/j.1600-079x.1990.tb00686.x. [DOI] [PubMed] [Google Scholar]
- 41.Kajdaniuk D, Marek B, Kos-Kudla B, Zwirska-Korczala K, Ostrowska Z, Buntner B, Szymszal J. Does the negative correlation found in breast cancer patients between plasma melatonin and insulin-like growth factor-I concentrations imply the existence of an additional mechanism of oncostatic melatonin influence involved in defense? Med Sci Monit. 2002;8:CR457–CR461. [PubMed] [Google Scholar]
- 42.Carlson LE, Campbell TS, Garland SN, Grossman P. Associations among salivary cortisol, melatonin, catecholamines, sleep quality and stress in women with breast cancer and healthy controls. J Behav Med. 2007;30:45–58. doi: 10.1007/s10865-006-9082-3. [DOI] [PubMed] [Google Scholar]
- 43.Hrushesky WJ, Blask DE. Re: Melatonin and breast cancer: a prospective study. J Nat Cancer Inst. 2004;96:888–889. doi: 10.1093/jnci/djh175. [DOI] [PubMed] [Google Scholar]
- 44.Fonseca R, Hartmann LC, Petersen IA, Donohue JH, Crotty TB, Gisvold JJ. Ductal carcinoma in situ of the breast. Ann Intern Med. 1997;127:1013–22. doi: 10.7326/0003-4819-127-11-199712010-00013. [DOI] [PubMed] [Google Scholar]
- 45.Lagios MD, Westdahl PR, Margolin FR, Rose MR. Duct carcinoma in situ. Relationship of extent of noninvasive disease to the frequency of occult invasion, multicentricity, lymph node metastases, and short-term treatment failures. Cancer. 1982;50:1309–14. doi: 10.1002/1097-0142(19821001)50:7<1309::aid-cncr2820500716>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 46.Schernhammer ES, Rosner B, Willett WC, Laden F, Colditz GA, Hankinson SE. Epidemiology of urinary melatonin in women and its relation to other hormones and night work. Cancer Epidemiol Biomarkers Prev. 2004;13:936–943. [PubMed] [Google Scholar]