Abstract
Objectives. We explored whether a successful randomized controlled trial of early education, the Carolina Abecedarian Project (ABC), which enrolled infants from 1972 to 1977 at the Frank Porter Graham Child Development Institute in Chapel Hill, North Carolina, improved health outcomes and behaviors by 21 years of age.
Methods. ABC randomized 111 infants to receive an intensive early education program or nutritional supplements and parental counseling alone; participants have been followed to the present day. We examined the effect of ABC on health outcomes and behavioral risk factors when participants were aged 21 years, and then explored the mediators of this relationship.
Results. Relative to the control group, the ABC treatment group was previously found to have improved cognition and educational attainment. We found that the intervention also improved heath (P = .05) and health behaviors (P = .03) when participants were aged 21 years. These improvements in behaviors were not mediated by IQ, math and reading scores at 15 years of age, educational attainment, or health insurance.
Conclusions. Effective early education programs may improve health and reduce risky health behaviors in adulthood.
Enhancements to schooling have the potential to improve a wide range of socioeconomic outcomes, including cognitive development, educational attainment, and occupational status, which may, in turn, increase health and longevity.1–8 The considerable disadvantages faced by children from low-income families can be mitigated by high-quality early education programs that provide cognitive enrichment.9–14 Such programs may therefore serve as an effective and efficient way to simultaneously improve population health and reduce health disparities.15
The adult health benefits of early childhood education have only been studied in a randomized controlled trial once before.16 That study, the Perry Preschool Program (PPP), found that a moderately intensive parental and prekindergarten program reduced risky health behaviors in former participants (relative to the control group) by 40 years of age.
The Carolina Abecedarian Project (ABC), a small, intensive program designed to enhance cognition and language development starting in infancy, afforded another opportunity to explore this relationship through young adulthood, with randomized data.17 ABC produced large improvements among treated children (relative to control participants) in IQ by 3 years of age, higher reading and math achievement by 15 years of age, lower rates of teen pregnancy and depression, and greater likelihood of college enrollment at 21 years of age.18,19 We investigated whether ABC also improved adult behavioral risk factors and health.
METHODS
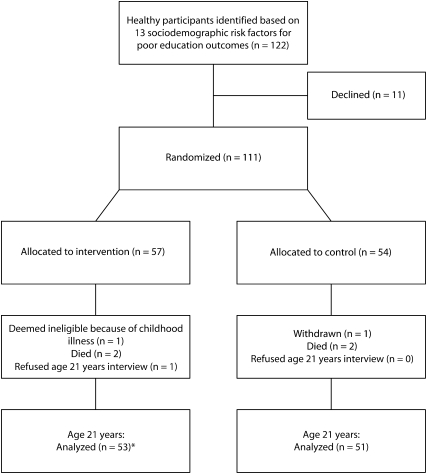
Participants were identified with the help of local service agencies and prenatal clinics and were included if they (1) were healthy and (2) were scored as high risk for poor educational outcomes according to a weighted, 13-item sociodemographic risk index.20 Four cohorts of infants (n = 111; mean age = 4.4 months) were enrolled in ABC beginning in 1972 and ending in 1977 (Figure 1). When they were aged 21 years, 105 participants were alive and eligible for follow-up. In that and subsequent follow-up studies, all participants, regardless of whether their data was complete across the entire intervention period (infancy to 8 years of age), were recruited and surveyed. One individual declined to participate at 21 years of age, leaving 104 participants: 53 who had received the preschool intervention and 51 who had not.
FIGURE 1.
Randomization flow diagram of infant participants in an early childhood education intervention: Carolina Abecedarian Project, Chapel Hill, NC 1972–1977.
Note. The asterisk refers to the 5 subjects who left the intervention, but were nevertheless followed through age 21 years.
Intervention and Control Groups
The first phase of the intervention included an age-appropriate curriculum designed to enhance cognition and language development starting in infancy. In addition, parents received social services and support as needed. Treated children received their primary pediatric care at the child care center; control group children had access to well-baby care at low-cost clinics in the area.
Both the intervention and control participants received nutritional supplements and social work services. These measures were intended to ensure that any cognitive enhancement could be more definitively attributed to early educational intervention rather than to enhanced nutrition (treated children in the intervention received 2 meals and a snack as nutritional supplements at the child care center) or to parental intervention. Some of the control children were enrolled in other programs within the community that also provided early child care and preschool services.
Statistical Analyses
We conducted an intent-to-treat analysis, comparing the cohort originally assigned to receive treatment with the cohort originally assigned to the control group. We did not have adequate information on participant exposure to conduct a treatment-on-treated analysis.
The sample size was small. As a result, we did not have adequate statistical power to detect a clinically meaningful effect size for any 1 health outcome measured within ABC. In addition, many outcomes were measured, requiring correction for multiple comparisons. We therefore needed to ascertain whether effects were generally beneficial or detrimental across broader categories of health outcomes. We combined outcomes into 2 larger groupings (health and healthy behaviors) and employed joint testing.
The data encompassed 3 health measures and 11 measures of behavioral risk factors. The health measures were the number of self-reported health problems since 15 years of age, a depression index score, and the number of hospitalizations in the past year. The depression index score was determined with the Brief Symptom Inventory, a 53-item questionnaire that measures various dimensions of affect and psychopathology.21
The 11 measures of behavioral risk factors concerned traffic safety, drug use, and access to primary care. The traffic safety measures recorded seat belt use, drunk driving, and riding as a passenger with a drunk driver, all coded as always, sometimes, rarely, or never. The drug use measures were number of binge-drinking episodes per month, defined as more than 5 drinks on any occasion, age when respondent started drinking, tobacco use (both the number of cigarettes smoked per day and the age when the respondent began smoking regularly), both the frequency and the age of initiation of marijuana use, and an indicator for whether cocaine was ever used. A final measure asked whether the respondent had a primary care doctor.
We first estimated regression models for each outcome measure under study, with controls for mother's age at program entry, whether a father was in the household at childbirth, child's gender, and mother's years of education at program entry. We added covariates to reduce noise in the dependent variable, thus improving the precision of our estimates. We estimated linear regression models for all continuous variables, order logit regression models for all ordinal variables, and logit regression models for all binary variables.
Because our dependent variables came from the same participants, reporting estimates based on these series of regressions would ignore the correlation of error terms, thus leading to invalid statistical inference. To account for this correlation, we estimated these models via seemingly unrelated regression (SUR) to obtain a single variance–covariance matrix for all regression equations, enabling us to account for the joint determination of outcomes.22,23 By estimating equations as a set, we detected whether effects were generally beneficial (or adverse) over a broader health category with multiple outcomes. Because estimates from our SUR model assessed statistical significance for only 2 broadly defined categories, we did not have to correct for multiple comparisons.
With prospective data, we were able to investigate not only whether early education interventions affect health, but also how.24 However, limited variables were available in our data set: IQ, achievement in math and reading by 15 years of age, educational attainment, and health insurance. We tested for mediation by adding these variables to our regression models and assessing the degree to which estimates of the treatment effect changed. We examined each separately and also tested mediation after grouping the first 3 into a combined category: cognitive achievement.
RESULTS
We noted no statistically significant differences in sociodemographic characteristics by group assignment, verifying that random assignment was successful (Table 1).
TABLE 1.
Baseline Characteristics of Participants and Outcomes at Age 21 Years: Carolina Abecedarian Project, Chapel Hill, NC, 1972–1998
| Intervention Group (n = 55),Mean (SE) or % | Control Group (n = 54),Mean (SE) or % | Total (n = 109),Mean (SE) or % | |
| Sociodemographic profile at randomization | |||
| Maternal age, y | 19.6 (3.9) | 20.3 (5.8) | 19.9 (4.9) |
| Maternal education, y | 10.4 (1.8) | 10.0 (1.9) | 10.2 (1.8) |
| Maternal IQa | 85.5 (12.4) | 84.2 (10.8) | 84.8 (11.6) |
| Two-parent family | 23 | 26 | 24 |
| African American | 96 | 100 | 98 |
| Maleb | 51* | 43* | 47* |
| Outcomes at age 21 y | |||
| Has a regular doctor | 51.6 | 48.4 | 59.6 |
| Always wears seat belt | 53.6 | 46.4 | 53.9 |
| Never drinks and drives | 49.3 | 50.7 | 66.4 |
| Never rides with a drinker | 51.0 | 49.0 | 49.0 |
| No health problems since age 15 y | 51.3 | 48.7 | 73.1 |
| Age began regular smoking, y | |||
| 11–12 | 0.0 | 3.9 | 1.9 |
| 13–14 | 3.8 | 7.8 | 5.77 |
| 15–16 | 11.3 | 17.7 | 14.4 |
| Never or ≥ 17 | 81.1 | 70.6 | 76.0 |
| Cigarettes per d | |||
| ≥ 20 | 5.7 | 7.8 | 6.7 |
| 6–19 | 9.4 | 23.5 | 16.4 |
| 2–5 | 17.0 | 11.8 | 14.4 |
| > 0–1 | 7.6 | 5.9 | 6.7 |
| 0 | 56.6 | 51.0 | 53.9 |
| Age began drinking, y | |||
| 11–12 | 15.1 | 5.9 | 10.6 |
| 13–14 | 7.6 | 13.7 | 10.6 |
| 15–16 | 17.0 | 39.2 | 27.9 |
| Never or ≥ 17 | 56.6 | 41.2 | 49.0 |
| Binge drinking,c d/mo | |||
| ≥ 20 | 7.6 | 7.8 | 7.7 |
| 10–19 | 5.7 | 5.9 | 5.7 |
| 6–9 | 11.3 | 9.8 | 10.6 |
| 3–5 | 11.3 | 3.9 | 7.7 |
| 0–2 | 60.4 | 72.6 | 66.4 |
| Age first tried marijuana, y | |||
| 9–10 | 3.8 | 9.8 | 6.7 |
| 11–14 | 5.7 | 7.8 | 6.7 |
| 15–16 | 13.2 | 23.5 | 18.3 |
| Never or ≥ 17 | 73.6 | 58.8 | 66.4 |
| No. of marijuana uses in past mo | |||
| ≥ 40 | 3.8 | 7.8 | 5.7 |
| 20–39 | 0.0 | 7.8 | 3.9 |
| 10–19 | 3.8 | 9.8 | 6.7 |
| 3–9 | 5.7 | 5.9 | 4.8 |
| 1–2 | 5.7 | 7.8 | 6.7 |
| 0 | 79.3 | 60.8 | 70.2 |
| Never used cocaine | 90.6 | 96.1 | 93.3 |
| Average depression score at age 21 yd | 54.1** | 58.6** | 56.3** |
Note. Percentages may not total 100% due to rounding.
According to the Wechsler Adult Intelligence Scale. The national mean is 100, and the standard deviation is 15.
One mother randomized to the treatment group gave birth to twins.
Defined as 5 or more drinks in one sitting.
The depression index score was measured with the Brief Symptom Inventory, a 53-item questionnaire that measures various dimensions of affect and psychopathology.21 Comparison was made to a control group.
*P < .1; **P < .05.
Our results are shown in Table 2. Although scanning the individual coefficients broadly indicates effects, the effect size of any 1 outcome measure was not meaningful because of insufficient power and because inference was not corrected for multiple comparisons. The joint test of significance for all factors within any 1 category revealed meaningful effects.
TABLE 2.
Coefficients for the Difference Between Intervention and Control Groups Aged 21 Years at Follow-Up: Carolina Abecedarian Project, Chapel Hill, NC, 1972–1998
| Measure | No. of Participants (n = 104) | Coefficienta | P |
| Health outcomes | .05 | ||
| Depression index score | 102 | −3.12 | .18 |
| No health problems since age 15 y | 102 | 0.62 | .22 |
| No hospitalizations in past y | 100 | 1.1 | .57 |
| Behavioral risk factors | .03 | ||
| Always wears seatbelt | 100 | 0.38 | .37 |
| Never drinks and drives | 99 | −0.08 | .88 |
| Never rides with a drinker | 99 | 0.01 | .99 |
| Has a primary care doctor | 102 | 0.21 | .63 |
| Never used cocaine | 71 | −0.8 | .44 |
| Age began drinking | 100 | 1.48 | .17 |
| Binge drinking | 100 | 0.13 | .73 |
| Age began regular smoking | 100 | 5.47 | .02 |
| Cigarettes smoked in past wk | 100 | −0.96 | .26 |
| Age first tried marijuana | 100 | 3.73 | .04 |
| Marijuana use in past mo | 100 | −4.24 | .06 |
Note. The intervention group was the baseline comparator. Variables were grouped into health outcomes and health behaviors. The outcome of interest was the joint test across each category. Coefficients were adjusted for mother's age at program entry, whether a father was in the household at childbirth, child's gender, and mother's years of education.
Compared with the control group.
Table 2 lists mean differences in health and behavioral outcomes between the treatment and control groups. The joint tests for overall health outcomes and for health behaviors were both significant (P = .05 and P = .03, respectively), suggesting that ABC produced an overall improvement in health and health behaviors by 21 years of age.
Participants randomized to ABC treatment were significantly older when they first became regular smokers of cigarettes (5.5 years; P = .02) and marijuana (3.7 years; P = .04). They also showed a tendency to smoke marijuana 4.2 fewer times in the past month than did control participants (P = .06). Because these measures were not corrected for multiple comparisons (e.g., via Bonferroni), they should not be interpreted as meaningful by themselves. We found no mediating influence of IQ, reading or math scores at 15 years of age, educational attainment, or health insurance (not shown).
DISCUSSION
We found that ABC treatment significantly improved health and reduced behavioral risk factors by 21 years of age. PPP was the only other randomized controlled trial to explore the impact of early education enhancements and adult health behaviors.16 Cohort sizes were similar in PPP and ABC, but the PPP intervention was less intensive than was the ABC intervention. Our data characterized ABC participants at 21 years of age; PPP followed participants until they were 40 years of age. Although some of the behavioral risk factor survey questions in ABC were the same as those in PPP, many were not. However, both studies grouped individual outcomes into broader categories via the same analytical approach, SUR, to test for whether effects generally occurred for health and health behaviors.
By the time the treated PPP participants were aged 40 years, they had significantly fewer behavioral risk factors than did the control group (P = .01).16 Moreover, scores in the subcategory measures pertaining to health status (self-rated health, stopped working because of poor health, and mortality) were also significantly better in the intervention group (P = .01). However, the treated group was more likely than was the control group to have self-reported or medically diagnosed conditions, an effect that persisted after control for health insurance. The net health effects were not better for the intervention than for the control group in the SUR analysis across all health outcome categories. In contrast to the PPP study, the combined health measures in ABC were statistically significant.
Although our results were largely consistent with those of PPP, we found a major difference in the mediation results. Educational attainment and health insurance proved to mediate some of the positive health behaviors in PPP, but the relationships we observed in ABC were not mediated by IQ, math or reading performance, educational attainment, or health insurance. Lack of mediation by cognitive variables is inconsistent not only with findings in PPP but also with a large body of literature linking IQ and educational attainment to improved health.1–3,5–8
Our study had several limitations. Although derived from a randomized controlled trial, our data were limited by our inability to conduct a treatment-on-treated analysis. Our intent-to-treat analysis produced conservative estimates of treatment effects because some experimental participants received little treatment, and some control group participants received early education elsewhere. Although our findings were likely conservative and internally valid, the intervention we tested was highly localized, so its generalizability is less certain. Finally, our approach, SUR, weights all outcome variables within a category equally. Thus, outcomes such as cocaine use, seat belt use, and binge drinking were all given equal weighting as behavioral risk factors, although some may have been more important than others.
Because they may improve income, reduce crime, and enhance the global competitiveness of the American workforce, early education enhancements are hypothesized to be more cost effective than many traditional medical and public health approaches to improving population health.15 Our study provides causal evidence in support of this hypothesis, but much remains to be learned about both the pathways linking education to health and the overall effect sizes of education on health.
Acknowledgments
We thank the Carolina Abecedarian Project for assistance.
Human Participant Protection
No protocol approval was needed for this study because we worked exclusively with de-identified data.
References
- 1.Grossman M. Education and nonmarket outcomes. : Hanushek E, Welch F, Handbook of the Economics of Education. Amsterdam, Netherlands: Elsevier; 2006 [Google Scholar]
- 2.Belfield CR, Nores M, Barnett S, Schweinhart L. The High/Scope Perry Preschool Program: cost-benefit analysis using data from the age-40 follow-up. J Hum Resour. 2006;41(1):162–190 [Google Scholar]
- 3.Lleras-Muney A. The relationship between education and adult mortality in the United States. Rev Econ Stud. 2005;72(1):189–221 [Google Scholar]
- 4.Carneiro P, Heckman JJ. Human capital policy. : Heckman J, Krueger A, Inequality in America: What Role for Human Capital Policies? Cambridge, MA: MIT Press; 2003 [Google Scholar]
- 5.Levin H, Belfield C. The Price We Pay: Economic and Social Consequences of Inadequate Education. Washington, DC: Brookings Institution Press; 2007 [Google Scholar]
- 6.Muennig P. How education produces health: a hypothetical framework. Teach Coll Rec. Available at: http://www.tcrecord.org/Content.asp?ContentID=14606. Published September 12, 2007. Accessed November, 22, 2010
- 7.Haan M, Kaplan GA, Camacho T. Poverty and health. Prospective evidence from the Alameda County Study. Am J Epidemiol. 1987;125(6):989–998 [DOI] [PubMed] [Google Scholar]
- 8.Ross CE, Wu CL. The links between education and health. Am Sociol Rev. 1995;60(5):719–745 [Google Scholar]
- 9.Currie J. Early childhood education programs. J Econ Perspect. 2001;15(2):213–238 [Google Scholar]
- 10.Knudsen EI, Heckman JJ, Cameron JL, Shonkoff JP. Economic, neurobiological, and behavioral perspectives on building America's future workforce. Proc Natl Acad Sci USA. 2006;103(27):10155–10162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noble KG, McCandliss BD, Farah MJ. Socioeconomic gradients predict individual differences in neurocognitive abilities. Dev Sci. 2007;10(4):464–480 [DOI] [PubMed] [Google Scholar]
- 12.Hart B, Risley TR. Meaningful Differences in the Everyday Experience of Young American Children. Baltimore, MD: Paul H Brookes Pub Co; 1995 [Google Scholar]
- 13.Gormley WT, Jr., Gayer T, Phillips D, Dawson B. The effects of universal pre-K on cognitive development. Dev Psychol. 2005;41(6):872–884 [DOI] [PubMed] [Google Scholar]
- 14.Beddington J, Cooper CL, Field J, et al. The mental wealth of nations. Nature. 2008;455(7216):1057–1060 [DOI] [PubMed] [Google Scholar]
- 15.Muennig P, Woolf SH. Health and economic benefits of reducing the number of students per classroom in US primary schools. Am J Public Health. 2007;97(11):2020–2027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muennig P, Schweinhart L, Montie J, Neidell M. Effects of a prekindergarten educational intervention on adult health: 37-year follow-up results of a randomized controlled trial. Am J Public Health. 2009;99(8):1431–1437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramey CT, Campbell FA. Poverty, early childhood education, and academic competence: the Abecedarian experiment. : Huston A, Children in Poverty: Child Development and Public Policy. Melborne, Australia: Cambridge University Press; 1994:190–221 [Google Scholar]
- 18.Campbell FA, Ramey CT, Pungello E, Sparling J, Miller-Johnson S. Early childhood education: young adult outcomes from the Abecedarian Project. Appl Dev Sci. 2002;6(1):42–57 [Google Scholar]
- 19.McLaughlin AE, Campbell FA, Pungello EP, Skinner M. Depressive symptoms in young adults: the influences of the early home environment and early educational child care. Child Dev. 2007;78(3):746–756 [DOI] [PubMed] [Google Scholar]
- 20.Ramey CT, Smith B. Assessing the intellectual consequences of early intervention with high-risk infants. Am J Ment Defic. 1977;81(4):318–324 [PubMed] [Google Scholar]
- 21.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605 [PubMed] [Google Scholar]
- 22.O'Brien PC. Procedures for comparing samples with multiple endpoints. Biometrics. 1984;40(4):1079–1087 [PubMed] [Google Scholar]
- 23.Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75(1):83–119 [Google Scholar]
- 24.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182 [DOI] [PubMed] [Google Scholar]