Abstract
Objectives. We examined the impact of Arizona's May 2007 comprehensive statewide smoking ban on hospital admissions for diagnoses for which there is evidence of a causal relationship with secondhand smoke (SHS) exposure (acute myocardial infarction [AMI], angina, stroke, and asthma).
Methods. We compared monthly hospital admissions from January 2004 through May 2008 for these primary diagnoses and 4 diagnoses not associated with SHS (appendicitis, kidney stones, acute cholecystitis, and ulcers) for Arizona counties with preexisting county or municipal smoking bans and counties with no previous bans. We attributed reductions in admissions to the statewide ban if they occurred only in diagnoses associated with SHS and if they were larger in counties with no previous bans. We analyzed the data with Poisson regressions, controlling for seasonality and admissions trends. We also estimated cost savings.
Results. Statistically significant reductions in hospital admissions were seen for AMI, angina, stroke, and asthma in counties with no previous bans over what was seen in counties with previous bans. No ban variable coefficients were statistically significant for diagnoses not associated with SHS.
Conclusions. Arizona's statewide smoking ban decreased hospital admissions for AMI, stroke, asthma, and angina.
Evidence for a direct association between exposure to secondhand smoke (SHS) and a range of health conditions is growing. A number of studies in the United States and other countries1–10 and 2 meta-analyses11,12 have shown a decrease in the incidence of acute myocardial infarction (AMI) after the implementation of comprehensive smoking bans. Although the early studies have been criticized for methodological flaws (see, for example, Kabat13), later larger and more rigorous studies also have shown this reduction.1,6,7,10
Several studies have now also examined the effect of smoking bans on other health conditions. For example, Khuder et al.8 focused on coronary heart disease, which included angina, heart failure, atherosclerosis, and AMI. Juster et al.7 examined impacts on both AMI and stroke, and Pell et al.10 considered acute coronary syndrome, which includes AMI and unstable angina. A recent study of New Zealand's national smoking ban14 examined the effect on both cardiovascular and pulmonary diagnoses. The conditions included were those with “sufficient” (AMI and angina), “suggestive” (stroke and asthma), and “inadequate” (exacerbations of chronic obstructive pulmonary disease [COPD]) evidence of a causal relationship with SHS according to the 2006 US Department of Health and Human Services Surgeon General's report.15 Although this is the only published study that did not show a reduction in AMIs, possibly because there was a nationwide partial smoking ban in place for 14 years beforehand, it did demonstrate a reduction in the numbers of asthma, stroke, unstable angina, and COPD cases compared with the year before the ban. These reductions did not, however, survive a more rigorous Poisson regression.
All studies mentioned previously utilized data on hospital admissions for the conditions of interest. Two other studies used survey methods to obtain data from individuals regarding their respiratory symptoms before and after smoking bans. A study by Menzies et al.16 used interviews, spirometry, and blood tests of nonsmoking bar workers 1 month before and 2 months after Scotland's national smoking ban to show significant reductions in respiratory (i.e., wheeze, shortness of breath, cough, phlegm) and sensory (i.e., red or irritated eyes, painful throat and nasal itch, runny nose, and sneeze) symptoms, serum cotinine levels, total white blood cell and neutrophil counts, and increases in forced expiratory volume in 1 second. Another study17 used telephone interviews of hospitality employees immediately before and 5 months after Norway's total ban on smoking in indoor hospitality venues. This study showed a significant reduction in all 5 respiratory symptoms measured (morning cough, daytime cough, phlegm cough, dyspnea, and wheezing). The reductions were largest in former smokers.
Finally, all but 1 of the previously discussed studies measured changes in health impacts (hospital admissions or reported symptoms) before and after the implementation of a single smoking ban. By contrast, Juster et al.7 tracked monthly hospital admissions in New York State for AMI and stroke over a 10-year period by county, and captured the impact of the statewide ban as well as the impacts of the various county-level smoking bans that were in place previously. The authors classified the county bans as either comprehensive (smoking is prohibited in all worksites, including bars, restaurants, and other hospitality venues) or moderate (smoking is restricted in most worksites, but not in hospitality venues). They found an increased rate of reduction in hospital admissions for AMI after the various bans were implemented, but no immediate reduction—i.e., the interaction between time and ban implementation was statistically significant, but the main effect of ban implementation was not. They also found that the effect of the comprehensive county bans was twice that of the moderate bans, and that the statewide ban resulted in an 8% reduction in AMI admissions in the year after implementation over what had already been accomplished by the county bans. The authors hypothesized that they saw a smaller reduction in AMIs than that seen in earlier studies (40% in Helena, Montana,4 and 27% in Pueblo, Colorado1) because of the incremental enactment of smoking bans and restrictions in New York over time.
We used hospital admission data and data on previous county bans to determine whether Arizona's statewide smoking ban reduced the incidence of hospitalizations for AMI, unstable angina, acute stroke, and acute asthma in the state.
METHODS
In this study, we used hospital discharge data gathered by the 87 hospitals in Arizona for the purpose of routine reporting to the Arizona Department of Health Services. We included all records of Arizona residents admitted from January 1, 2004, through May 31, 2008, with primary diagnoses coded with the following International Classification of Diseases, Ninth Revision (ICD-9) codes18: AMI (410.x0 and 410.x1), unstable angina (411.1x), acute stroke (430–434.xx, 436.xx, and 437.1x), and acute asthma (493.xx). June 2008 data were available but excluded from the analyses because they did not include patients admitted in June who were discharged in July.
Causality
Because causality is difficult to infer from observational data, these data were subjected to several tests following Hill's guidelines for causality.19 The statewide smoking ban was assumed to be a causal factor in the reduction in hospital admissions if (1) there was a reduction in admissions after the statewide ban was implemented (temporality), (2) the reduction was statistically significant (strength), (3) the reduction in admissions in the counties with no previous smoking bans in place was larger than it was in counties with previous bans (dose–response), and (4) there was only a reduction in health conditions with sufficient or suggestive evidence of a causal relationship with SHS exposure (biologic plausibility). Hill's guideline of consistency among studies has already been shown by the results of the studies reviewed in the Introduction.
A number of cities and counties in Arizona had various smoking bans in place before May 1, 2007 (the date the statewide smoking ban took effect). To test for Hill's dose–response guideline for causality, cases were separated between those in hospitals in counties that had these bans and those in counties that did not. The Arizona counties with no official county or city smoking bans in place (other than bans in municipal buildings, or, in 1 case—Mohave County—other than a partial ban in a city making up less than 0.5% of the county's population) were Apache, Cochise, Gila, Graham, Greenlee, La Paz, Mohave, Navajo, Pinal, and Yuma. They will be referred to as “nonban counties” and their combined populations make up slightly more than 17% of the state's total population. The remaining counties (Coconino, Maricopa, Pima, Santa Cruz, and Yavapai—i.e., “ban counties”) had at least 1 major municipality with a complete smoking ban in at least indoor worksites (other than hospitality venues) that was continuous over the 2004 to 2007 time period. The strongest effect of the statewide ban should be seen in the nonban counties.
To test for Hill's biologic plausibility guideline for causality, we also obtained hospital admissions data for 4 acute diagnoses that each account for a substantial portion of hospital admissions and that are not known to be associated with SHS exposure: acute appendicitis, kidney stones, acute cholecystitis, and ulcers. Records of Arizona residents admitted in 2004 through May 2008 with primary diagnoses coded with the following ICD-9 codes were included in this analysis: acute appendicitis (540.x and 541), kidney stones (592.x), acute cholecystitis (574.0x, 574.3x, 574.6x, and 575.0), and ulcer (531–533.xx except for 531.7x, 532.7x, and 533.7x). No change in admissions was expected to be seen in these diagnoses in the period after the implementation of the statewide ban.
Data Analysis
We analyzed the data with Poisson regression. The number of cases for each diagnosis category, for either all counties with no previous smoking bans or all counties with previous bans, was the dependent variable. The estimated adult population (or total population for asthma and appendicitis) for each group of counties each year was used as the offset variable. A dummy variable with the value of “1” indicated cases from nonban (i.e., no previous ban) counties and, used alone, this variable captured any difference in the prevalence rate of each condition between the groups of counties. A dummy variable that had the value of “1” in the months including and after May 2007 and “0” otherwise was used to capture the effect of the time period after the implementation of the statewide smoking ban. An interaction between these dummy variables allowed the effect of the statewide ban to be different in ban and nonban counties, and measured the change in admissions in the nonban counties over and above that seen in the ban counties during the post–statewide ban period. Seasonality was constrained to be the same for each year and for all counties, but was allowed to be defined by the data through the inclusion of variables for month, month-squared, and month-cubed. An annual linear trend was included to capture any general trend in the incidence of each diagnosis. An interaction term with the nonban counties variable captured any difference in this trend between the groups of counties.
No age- or sex-adjustment was made in the hospital admission data for 2 reasons. First, no adequate estimate of Arizona's population by age, sex, and county for these years was available, and, second, an analysis of the population's components by age and sex from statewide estimates for this period differed by less than one half of 1% year to year.
The hospital discharge data set also contains information on the total charges incurred for each patient's stay and on the expected source of payment for the majority of those charges. We used this information for hospital stays by Arizona residents for each of the diagnoses to calculate an estimate of the average cost savings attributable to the statewide smoking ban. We ran the analyses with the GENLIN procedure in SPSS 16.0 for Windows (SPSS Inc, Chicago, IL).
RESULTS
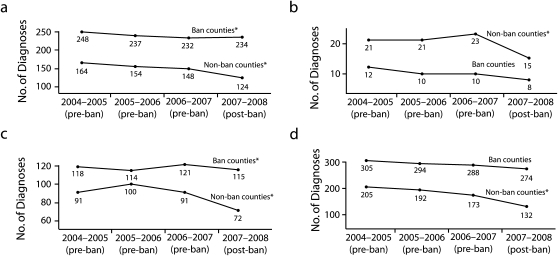
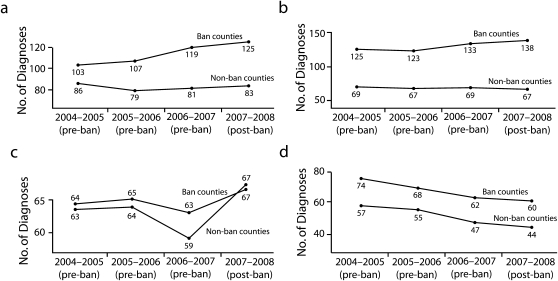
Figure 1 and Figure 2 show the rate of hospital admissions (per 100 000) by diagnosis for 3 full years prior to and 1 full year after the statewide smoking ban for counties with no significant smoking bans in place prior to the statewide ban (nonban counties) and for counties with some smoking bans in place (ban counties). (A table showing the number of cases and rates by year for each diagnosis [Table A.1], and a table showing the average age and percentage of cases who were female [Table A.2] are available as a supplement to the online version of this article at http://www.ajph.org.)
FIGURE 1.
Rate of hospital admissions (per 100 000 adult population) for secondhand smoke–associated diagnoses, by county smoking ban status and year, for (a) AMI, (b) angina, (c) asthma,a and (d) stroke: May 2004–April 2008.
Note. AMI = acute myocardial infarction. For ease of interpretation, this figure only shows data for 3 full years prior to the implementation of the ban although 40 months of pre-ban data were included in the analysis, and it only shows data for 1 full year after the ban although 13 months of post-ban data were included in the analysis.
aPer 100 000 of the total population.
*P < .05, for the estimated change in the number of hospital admissions for each diagnosis after the implementation of the statewide ban.
FIGURE 2.
Rate of hospital admissions (per 100 000 adult population) for diagnoses not associated with secondhand smoke, by county smoking ban status and year for (a) acute cholecystitis, (b) appendicitis,a (c) kidney stones, and (d) ulcers: May 2004–April 2008.
Note. For ease of interpretation, this figure only shows data for 3 full years prior to the implementation of the ban although 40 months of pre-ban data were included in the analysis, and it only shows data for 1 full year after the ban although 13 months of post-ban data were included in the analysis.
aPer 100 000 of the total population.
It is possible that the difference in rates between the nonban and ban counties was influenced by the effects of the smoking bans in place before the implementation of the statewide ban. However, it is more likely that the differences in rates reflect the more urban (ban counties) versus more rural (nonban counties) incidence of these diagnoses. If the statewide smoking ban reduced the incidence of hospital admissions for a diagnosis, the rate for that condition for May 2007 through April 2008 should be lower than that expected with any trend seen across the previous 3 years, especially for nonban counties.
Table 1 gives the estimated change in hospital admissions for each diagnosis expected to be affected by SHS. These estimates are based on the Poisson regression results and the P values shown are those of the coefficients estimated for the 2 ban effects variables. As expected, all estimates for the nonban counties are negative and statistically significant at the α < 0.05 level. For example, there are estimated to be 159 fewer cases of hospital admission for AMI in nonban counties in the 13 months after the ban than what would have been expected from the rates seen in ban counties during the same period.
TABLE 1.
Estimated Change in the Number of Hospital Admissions After Implementation of the Arizona Statewide Smoking Ban, by Diagnosis: May 1, 2007–May 31, 2008
| Ban County Effects |
Additional Effects in Nonban Counties Over Those Seen in Ban Counties |
|||||
| Change in Number of Cases | Percentage Change in Number of Cases | P | Change in Number of Cases | Percentage Change in Number of Cases | P | |
| Acute myocardial infarction | 375 | 4 | .027 | −159 | −13 | .01 |
| Unstable angina | −3 | −1 | .934 | −63 | −33 | .014 |
| Acute stroke | −266 | −2 | .155 | −198 | −14 | .001 |
| Acute asthma | −306 | −4 | .035 | −249 | −22 | <.001 |
Because they lack a dose–response comparison group according to Hill's guidelines for causality, the estimates for the ban counties are not as easy to interpret. The only claim that can be made regarding these estimates is that they indicate a change in the number of cases in counties with previous bans after the implementation of the statewide ban. The estimated change in admissions for AMI in ban counties is positive and statistically significant; it is negative and statistically significant for asthma, and negative but not statistically significant for stroke and angina. It is unclear whether these changes are attributable to the statewide smoking ban or to some other factor that may have had an influence on hospital admissions for these diagnoses in the May 1, 2007, to May 31, 2008, period.
Under the guideline of biologic plausibility, none of the estimates of ban effects for the diagnoses not expected to be affected by SHS (acute appendicitis, kidney stones, acute cholecystitis, and ulcers) should be statistically different than zero. This criterion was met.
Table 2 contains an estimate of the cost savings attributable to the statewide smoking ban in nonban counties over the first 13 months after its implementation: $16.8 million. Approximately $2.3 million of this would have been paid by Medicaid. Because hospital charges generally overstate actual economic costs because some insurers pay lower-than-average cost,20 this figure may be an overestimate. However, as noted earlier, these estimates are based on a reduction in the number of cases in nonban counties over what could be expected in ban counties, thus, this figure could also be an underestimate of the actual savings in hospital costs because of the ban.
TABLE 2.
Estimated Impact of the Arizona Statewide Smoking Ban on Hospital Charges: May 1, 2007–May 31, 2008
| Number of Cases Reduced | Average Total Charge per Case | Estimated Savings (Millions of Dollars) | |
| Acute myocardial infarction | 159 | $45 033 | $7.2 |
| Unstable angina | 63 | $13 866 | $0.9 |
| Acute stroke | 198 | $24 836 | $4.9 |
| Acute asthma | 249 | $15 330 | $3.8 |
| Total savings | $16.8 |
DISCUSSION
Within the context of the growing body of consistent evidence from studies in other states and regions, the results of this study support the case for substantial health benefits from Arizona's comprehensive statewide smoking ban in areas with no previous bans. According to this analysis there was a statistically significant decrease in the number of AMI, angina, stroke, and asthma cases admitted to hospitals in counties with no previous smoking bans, compared with counties with previous bans, during the months following the implementation of the statewide comprehensive ban. In addition, these decreases were seen in those counties during the post–statewide ban period only in diagnoses with “sufficient” or “suggestive” evidence of a causal relationship with SHS exposure according to the US Department of Health and Human Services Surgeon General's 2006 report.15 None of the relevant coefficients for 4 diagnoses unrelated to SHS exposure (acute appendicitis, kidney stones, acute cholecystitis, and ulcers) were statistically different than zero.
Therefore, according to Hill's guidelines for causality, there is evidence that the following reductions (and percentage reductions) in hospital admission cases in the nonban counties from May 1, 2007, to May 31, 2008, are attributable to the statewide ban: 159 (13%) fewer AMI cases, 63 (33%) fewer angina cases, 198 (14%) fewer stroke cases, and 249 (22%) fewer asthma cases. The estimated savings in hospital costs from these reductions is $16.8 million. These estimates may underestimate the impact of the statewide ban in these counties because they are estimates of reductions in admissions in addition to what could have been expected in ban counties. Note also that the reductions for AMI, stroke, and asthma come despite the lower rates of incidence for these diagnoses in nonban versus ban counties (Figure 1). Juster et al.7 also found larger reductions in hospital admissions in counties that went from no ban to a comprehensive ban than in those going from a moderate to a comprehensive ban.
Impacts in Countries With Previous Smoking Bans
The relationship between the changes seen in admissions in the ban counties and the statewide ban is less clear. It would have been ideal to have had hospital admission data from nearby counties in other states with levels of previous smoking bans in place similar to what was seen in the ban counties over the same time period, but with no statewide smoking ban. A comparison between the changes seen in these counties and the ban counties would have more clearly separated the impact of the statewide ban from the influence of other causal factors on admissions for the counties with previous bans. Unfortunately, no such data were available. California has had a statewide smoking ban since January 1995; New Mexico instituted its statewide smoking ban in June 2007; Utah instituted its statewide ban in January 2007; and Nevada has had a statewide partial ban (enclosed workplaces and restaurants, but not casinos) since November 2006.
Therefore, although it is tempting to claim that the statistically significant reduction in asthma in ban counties is because of the statewide ban, it could also be attributable to a reduction during that period in some other causal factor for asthma itself or for its diagnosis. The statistically significant increase seen in AMI would be even harder to explain as being caused by the statewide ban. It lacks both the dose–response and biologic plausibility arguments for causality. These changes are likely because of an increase in causal factors for AMI or for its diagnosis other than the statewide ban.
Comparisons With Other Studies
A number of previous studies have demonstrated reductions in hospital admissions for AMI1–10 after the implementation of smoking bans. The most recent of 2 meta-analyses12 yielded a pooled estimate of a 19% reduction in hospital admission rates for AMI, which is consistent with an estimate put forth by Pechacek and Babb21 of 18% to 19% as being the maximum impact that could be expected to be associated with a ban. Juster et al.7 estimated a 19% reduction in AMI admissions had there been no local bans in existence before New York's statewide ban was implemented, and an 8% reduction with the local bans. Our study showed a 13% reduction in AMI hospital admissions in counties with no previous bans compared with counties with previously existing municipal or county bans. This 13% reduction is comparable to the 11% difference (19% minus 8%) between the Juster et al. study's 2 estimates. However, instead of an 8% reduction in AMI admissions after implementation of the statewide ban for counties with previous bans (which would have been consistent with Juster et al.), our study showed an unexplained 4% increase in AMI admissions in the post–statewide ban period.
To our knowledge, our study is the first to demonstrate reductions in hospital admissions for angina, stroke, and asthma after the implementation of a smoking ban. Edwards et al.14 examined the impact of New Zealand's comprehensive smoking ban on these diagnoses, and on AMI and exacerbations of COPD. However, although post-ban reductions were seen in admission rates for angina, stroke, asthma, and COPD, these reductions disappeared when Poisson regression was applied. When one considers our results, it is possible that the Edwards et al. study suffered from the lack of a dose–response comparison group. New Zealand's comprehensive smoking ban was implemented 14 years after an earlier national law banned smoking
in public facilities (including retail areas), most shared offices, and [imposed] partial restrictions (≥ half of the area designated as nonsmoking) for work cafeterias, restaurants and meal serving areas of pubs and other licensed venues.14(p1)
It is possible that statistically significant reductions in hospital admissions would have been seen if a comparison had been available to hospital data from an otherwise similar region with either no previous ban (as was available for this study) or with a similar previous ban and no new comprehensive ban.
Juster et al.7 found no impact on hospital admissions for stroke for either previous partial bans or for the comprehensive statewide ban. The authors used a broader range of ICD-9 codes to identify stroke (ICD-9 codes 430–438.xx) than was used in the present study; it is possible that the inclusion of nonacute stroke diagnoses such as cerebral atherosclerosis (ICD-9 code 437.0) and the late effects of cerebrovascular disease (ICD-9 code 438.xx) diminished the expected effect. In the case of unstable angina, it is unfortunate that neither the Khuder et al. study,8 which looked at coronary heart disease (AMI, angina, heart failure, and atherosclerosis), nor the Pell et al. study,10 which looked at acute coronary syndrome (AMI and unstable angina), separated the impacts found across the various underlying diagnoses.
Juster et al.7 is the only other study that found estimated cost savings from a smoking ban. They used an estimate of the average in-hospital cost per AMI of $14 772, which was substantially lower than the average charge of $45 033 per AMI found in our data. There are 2 reasons for this difference. First, as mentioned previously, hospital charges regularly overestimate actual costs.20 Second, the $14 772 figure used in Juster et al. is based on 1992 to 1993 data.22 Adjusting this 1992 to 1993 estimate to 2008 dollars by using the consumer price index for medical care gives an average cost of $26 208 per AMI, which is closer to but still substantially lower than the $45 033 estimate used in this study. However, the study that was the source of the $14 772 cost estimate also contained an average charge estimate of $24 794. When this figure is adjusted to 2008 dollars, it becomes $43 989 per AMI, a figure comparable to the average charge estimate of $45 033 per AMI that we used in our study.
Limitations and Conclusions
We have attempted to be conservative in interpreting our findings by using Hill's guidelines for causality. Even so, as with any study that relies on observational rather than experimental data, there are limitations to these data. We used a census of hospital admissions data available in Arizona for the 53 months of the study; however, the generalizability of the size of the effects to other regions is limited by the demographics of the state's population and its distribution across the state. Although the ban counties provided a comparison group to study the effects for the nonban counties, as noted previously, we had no similar comparison group for the ban counties (i.e., ban counties with no statewide ban). Therefore, the inconsistent findings for SHS-related diagnoses in ban counties (some decreases, some increases) are difficult to interpret.
We provide evidence that Arizona's statewide smoking ban reduced the incidence of hospital admissions for AMI, stroke, asthma, and angina in the 13 months after its implementation, at least in counties with no previous bans. We also illustrated the cost savings of these drops in admissions. Taken with the growing number of other studies showing substantial health benefits from comprehensive bans on smoking, and the recent Institute of Medicine conclusion that bans reduce coronary heart disease risk,23 there is now little room to doubt their effectiveness. If one considers the fact that only about 40% of the US population is presently covered by a comprehensive smoke-free law,24 and the need for effective and cost-saving options in health care, comprehensive smoking bans should be considered by any governmental agency, employer, or other organization seeking to advocate or implement policies that improve health and reduce health care costs.
Acknowledgments
This work was completed with the financial support of the Arizona Department of Health Services Bureau of Tobacco and Chronic Disease.
Special thanks are also offered to Sue Voelker who extracted the hospital admission data.
Human Participant Protection
This study was deemed exempt from institutional review board review because only deidentified publicly available data were used.
References
- 1.Bartecchi C, Alsever RN, Nevin-Woods C, et al. Reduction in the incidence of acute myocardial infarction associated with a citywide smoking ordinance. Circulation. 2006;114(14):1490–1496 [DOI] [PubMed] [Google Scholar]
- 2.Cesaroni G, Forastiere F, Agabiti N, Valente P, Zuccaro P, Perucci CA. Effect of the Italian smoking ban on population rates of acute coronary events. Circulation. 2008;117(9):1183–1188 [DOI] [PubMed] [Google Scholar]
- 3.Lemstra M, Neudorf C, Opondo J. Implications of a public smoking ban. Can J Public Health. 2008;99(1):62–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sargent RP, Shepard RM, Glantz SA. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study. BMJ. 2004;328(7446):977–980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seo DC, Torabi MR. Reduced admissions for acute myocardial infarction associated with a public smoking ban: matched controlled study. J Drug Educ. 2007;37(3):217–226 [DOI] [PubMed] [Google Scholar]
- 6.Barone-Adesi F, Vizzini L, Merletti F, Richiardi L. Short-term effects of Italian smoking regulation on rates of hospital admission for acute myocardial infarction. Eur Heart J. 2006;27(20):2468–2472 [DOI] [PubMed] [Google Scholar]
- 7.Juster HR, Loomis BR, Hinman TM, et al. Declines in hospital admissions for acute myocardial infarction in New York State after implementation of a comprehensive smoking ban. Am J Public Health. 2007;97(11):2035–2039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khuder SA, Milz S, Jordan T, Price J, Silvestri K, Butler P. The impact of a smoking ban on hospital admissions for coronary heart disease. Prev Med. 2007;45(1):3–8 [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention Reduced hospitalizations for acute myocardial infarction after implementation of a smoke-free ordinance—City of Pueblo, Colorado, 2002–2006. MMWR Morb Mortal Wkly Rep. 2009;57(51/52):1373–1377 [PubMed] [Google Scholar]
- 10.Pell JP, Haw S, Cobbe S, et al. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med. 2008;359(5):482–491 [DOI] [PubMed] [Google Scholar]
- 11.Dinno A, Glantz S. Clean indoor air laws immediately reduce heart attacks. Prev Med. 2007;45(1):9–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glantz SA. Meta-analysis of the effects of smokefree laws on acute myocardial infarction: an update. Prev Med. 2008;47(4):452–453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kabat G. Effect of public smoking ban in Helena, Montana: when results look too good to be true, they probably are. BMJ. 2004;328(7452):1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edwards R, Thomson G, Wilson N, et al. After the smoke has cleared: evaluation of the impact of a new national smoke-free law in New Zealand. Tob Control. 2008;17(1):e2. [DOI] [PubMed] [Google Scholar]
- 15.The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006 [PubMed] [Google Scholar]
- 16.Menzies D, Nair A, Williamson PA, et al. Respiratory symptoms, pulmonary function, and markers of inflammation among bar workers before and after a legislative ban on smoking in public places. JAMA. 2006;296(14):1742–1748 [DOI] [PubMed] [Google Scholar]
- 17.Eagan TML, Hetland J, Aaro LE. Decline in respiratory symptoms in service workers five months after a public smoking ban. Tob Control. 2006;15(3):242–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 19.Szklo M, Nieto FJ. Epidemiologic issues in the interface with public health policy. : Moyses S, Nieto FJ, Epidemiology: Beyond the Basics. 2nd ed Boston, MA: Jones and Bartlett Publishers; 2007:375–406 [Google Scholar]
- 20.Finkler SA. The distinction between cost and charges. Ann Intern Med. 1982;96(1):102–109 [DOI] [PubMed] [Google Scholar]
- 21.Pechacek TF, Babb S. How acute and reversible are the cardiovascular risks of secondhand smoke? BMJ. 2004;328(7446):980–983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krumholz HM, Chen J, Murillo JE, Cohen DJ, Radford MJ. Clinical correlates of in-hospital costs for acute myocardial infarction in patients 65 years of age and older. Am Heart J. 1998;135:523–531 [DOI] [PubMed] [Google Scholar]
- 23.Institute of Medicine Secondhand Smoke Exposure and Cardiovascular Effects: Making Sense of the Evidence. Washington, DC: The National Academies Press; 2009 [PubMed] [Google Scholar]
- 24.Summary of 100% smokefree state laws and population protected by 100% US smokefree laws. Berkeley, CA: The American Nonsmokers' Rights Foundation; 2009. Available at: http://www.no-smoke.org/pdf/SummaryUSPopList.pdf. Accessed September 15, 2009 [Google Scholar]