Abstract
Objectives. We compared estimated population-based health outcomes for New York City (NYC) homeless families with NYC residents overall and in low-income neighborhoods.
Methods. We matched a NYC family shelter user registry to mortality, tuberculosis, HIV/AIDS, and blood lead test registries maintained by the NYC Department of Health and Mental Hygiene (2001–2003).
Results. Overall adult age-adjusted death rates were similar among the 3 populations. HIV/AIDS and substance-use deaths were 3 and 5 times higher for homeless adults than for the general population; only substance-use deaths were higher than for low-income adults. Children who experienced homelessness appeared to be at an elevated risk of mortality (41.3 vs 22.5 per 100 000; P < .05). Seven in 10 adult and child deaths occurred outside shelter. Adult HIV/AIDS diagnosis rates were more than twice citywide rates but comparable with low-income rates, whereas tuberculosis rates were 3 times higher than in both populations. Homeless children had lower blood lead testing rates and a higher proportion of lead levels over 10 micrograms per deciliter than did both comparison populations.
Conclusions. Morbidity and mortality levels were comparable between homeless and low-income adults; homeless children's slightly higher risk on some measures possibly reflects the impact of poverty and poor-quality, unstable housing.
Most studies examining the health of homeless populations have involved single adults and have identified higher rates of death, tuberculosis (TB), HIV/AIDS, mental health disorders, substance use, poor birth outcomes, and cardiovascular disease than in the general population.1–7 Whether these findings can be generalized to homeless families is not known, as the 2 populations differ greatly. Nationally, homeless families overwhelmingly consist of a young female head of household with children, whereas single homeless adults are mostly men aged 31 to 50 years.8 Homeless families are also distinct in their reasons for becoming homeless, citing poverty more often and substance use and mental illness less often than is the case for their single adult counterparts.9 Based on their demographic and socioeconomic profiles, the health of homeless families may be more like that of other low-income families than that of homeless single adults.
Recent economic conditions have led to a rise in the number of homeless families nationwide. Although overall US homelessness held fairly constant from 2007 to 2008, the number of homeless families increased by 9%. According to the latest available national data, an estimated 516 700 adults and children were sheltered as families over a 1-year period in 2008, constituting roughly a third of the overall sheltered homeless population during that time.8 More recent data from a sampling of localities found that, as of September 2009, the count of sheltered families had increased 10% from the previous quarter, as foreclosure and unemployment rates continued to rise.10
In New York City (NYC), the Department of Homeless Services (DHS) supplies apartment-style shelters and support services such as childcare, housing assistance, and health care referral to homeless families. Because the city provides emergency shelter to eligible families, virtually all homeless families use shelter facilities. In 7 years of an annual count of street homeless, a family has never been found on the street.11 A small share of homeless families is sheltered by city agencies other than DHS. However, analyses based on DHS shelter registry likely include the vast majority of the NYC homeless family population.
Our objective was to systematically characterize the health of adults and children who used the NYC family shelter system. We matched the DHS family shelter registry with 4 health registries managed by the NYC Department of Health and Mental Hygiene, and we compared estimates of morbidity and mortality in the homeless family population with those of the NYC general and lowest-income neighborhood populations.
METHODS
The DHS provides emergency shelter to NYC resident families that have no permanent or temporary place to live. From 2001 through 2003, the system included parents (predominantly single mothers) with children, pregnant women, and 2 or more related adults (married or domestically partnered couples, parents with adult children, and adult siblings). The analytic population for this study included adults with children, their children (aged 1–17 years), and pregnant women who spent at least 1 night in a DHS family shelter from January 1, 2001, through December 31, 2003. Infants (aged < 1 year) were excluded because the DHS registry does not have a mechanism for documenting the death of infants who die before leaving the hospital. At shelter intake, name, date of birth, Social Security number, and sex were collected on all residents and their children. Race and ethnicity were only collected for the head of household.
Data Sources and Matching Procedures
We matched the family shelter registry to 4 legally mandated city health registries (vital statistics, HIV/AIDS, TB, and lead). The NYC Bureau of Vital Statistics maintains information on cause and manner of deaths within NYC. The HIV/AIDS Reporting System monitors information on HIV-related events in NYC. For suspected and confirmed TB, demographic, clinical, laboratory, and risk-factor information is reported to the TB registry. The NYC blood lead registry maintains information on all laboratory blood lead tests, including mandated tests for NYC children.
We retrospectively matched the DHS registry to death, TB, and HIV/AIDS registries using name, date of birth, and Social Security number for the period January 1, 2001, through December 31, 2003. Variations of names and birthdates were also identified as potential matches by using a hierarchical match key algorithm. We matched children in the DHS registry to the lead registry data via name, date of birth, sex, mother's name and date of birth, and most recent address reported. Social Security numbers were not available in the lead registry.
For the death, HIV/AIDS, and TB registry matches, records that matched on all fields were included in the data set without further review. Incompletely matched records were assessed by 2 reviewers, and discordance was settled by a third reviewer. In the lead registry match, we used probability thresholds based on variations in the match to determine whether a pair of records matched.
Analyses
We performed all statistical analyses with SAS 9.1 (SAS Institute Inc, Cary, NC). We calculated death rates (by cause), HIV/AIDS prevalence, new HIV/AIDS diagnoses, and TB diagnoses for homeless adults who used the family shelter system, the general NYC adult population, and adults in NYC's 3 poorest neighborhoods. These neighborhoods were determined by median neighborhood income according to the US Census and United Hospital Fund neighborhood groupings, consisting of aggregated zip codes,12,13 and were found to be contiguous within the South Bronx borough of NYC. However, these low-income groups are not necessarily reflective of all NYC low-income neighborhoods on all indices.
We calculated rates of death, HIV, TB, lead testing, and elevated blood lead levels (BLLs) among children who used the shelter system and compared these with rates in NYC children and those in the lowest-income neighborhoods. We presented causes of death among children as proportions rather than rates, because of small numbers.
We calculated rates among homeless adults, NYC residents, and the lowest-income neighborhoods by dividing the number of events during the study period by the DHS registry, NYC, and lowest-income neighborhood populations, respectively (the latter 2 from the 2000 census12). Rates of death and illness among adults were age adjusted to the 2000 projected US population, and, except for HIV/AIDS prevalence, the adults and child rates were annualized. Analyses of HIV/AIDS prevalence were not annualized because of disease chronicity.
New York State Public Health law mandates universal blood lead testing by health care providers of all children aged 1 and 2 years.14 Our lead analyses were limited to children aged 36 months to 47 months at the time of shelter stay during 2001 through 2003. For the general and low-income populations, analyses were conducted among children turning 3 years in 2001; children who received a lead test before then were considered tested. Analyses of high BLLs (≥ 10 μg/dL) were done only among children who had been tested before their 48th month.
We calculated rate ratios to compare rates across groups. To test differences in percentages and rates, we calculated odds ratios and 95% confidence intervals (CIs).
RESULTS
From 2001 to 2003, 102 771 family members were housed by the DHS family shelter system for at least 1 night, including 45 756 adults (0.8% of NYC adult residents) and 57 015 children (3% of NYC child residents). Among families with children in shelter, 45% had only 1 child, 40% had 2 or 3 children, 10% had more than 3 children, and 5% were pregnant with no other children with them. Adults in the family system were mostly female (69%), and 33% were aged 18 to 24 years. By contrast, only 54% of the general NYC population and 56% of the low-income adult population were female, and 13% and 17%, respectively, were aged 18 to 24 years. About two thirds of adults in shelter with known race/ethnicity were Black (64%) and one third was Hispanic (34%), compared with 23% and 25%, respectively, of NYC adults, and 33% and 62%, respectively, of those in low-income neighborhoods. The age distribution of children in shelter was younger than that of children citywide. Three in 10 children in shelter (31%) were aged 5 years or younger compared with 24% citywide and 23% among those in low-income neighborhoods, and teenagers (aged 12–17 years) constituted only 26% of children in shelter, compared with 34% citywide and 32% in low-income neighborhoods.12
During the study, the average cumulative length of stay for families was 307 days (range: 1–1082). Length of stay was more than 30 days for almost all adults (91%) and children (92%).
Mortality
There were 178 deaths among adults who stayed in shelter from 2001 through 2003. Their age-adjusted death rate was 1195 per 100 000, similar to adult rates in the general population (1043 per 100 000) and in low-income neighborhoods (1258 per 100 000). However, death rates among adults aged 25 to 49 years were significantly elevated compared with the NYC overall rate and marginally higher than that in low-income neighborhoods (Table 1). The death rate among adults who used shelter increased with age, as in general and low-income populations. Less than one third (31%) of adult deaths occurred while in shelter. Among those who died after leaving shelter, the average interval between shelter exit and death was 351 days (range: 1–953).
TABLE 1.
Deaths, Death Rates, and Mortality Rate Ratios Among Adults With Children and Children Who Used the New York City Department of Homeless Services Family Shelter: New York City, 2001–2003
| Deaths Among NYC Residents |
Deaths in NYC Low-Income Neighborhoods,a |
||||
| Deaths Among Family Shelter Users, No. (Deaths per 100 000) | No. (per 100 000) | Mortality Rate Ratiob (95% CI) | No. (per 100 000) | Mortality Rate Ratioc (95% CI) | |
| Adults | |||||
| Overalld | 178 (1195.2) | 175 505 (1042.6) | 1.2 (0.7, 1.6) | 9255 (1257.9) | 0.95 (0.6, 1.3) |
| Age, y | |||||
| 18–24 | 18 (118.8) | 1700 (70.6) | 1.7 (1.0, 2.4) | 169 (97.9) | 1.2 (0.8, 1.6) |
| 25–49 | 124 (431.0) | 19 500 (205.5) | 2.1 (1.8, 2.4) | 2040 (373.9) | 1.2 (1.0, 1.3) |
| ≥50 | 36 (1964.0) | 154 305 (2446.3) | 0.8 (0.6,1.1) | 7046 (2521.3) | 0.8 (0.6, 1.0) |
| Sexd | |||||
| Male | 66 (1209.8) | 84 223 (1216.5) | 1.0 (0.4, 1.61) | 4765 (1587.0) | 0.76 (0.3, 1.2) |
| Female | 112 (1196.1) | 91 282 (912.3) | 1.3 (0.7, 1.9) | 4490 (1034.6) | 1.16 (0.7, 1.7) |
| Children | |||||
| Overall | 23 (41.3) | 1231 (22.5) | 1.8 (1.2, 2.5) | 98 (19.2) | 2.1 (1.6, 2.5) |
| Age, y | |||||
| 1–4 | 9 (51.8) | 354 (27.4) | 1.9 (1.0, 3.0) | 24 (20.2) | 2.6 (2.0, 3.2) |
| 5–11 | 4 (16.6) | 372 (15.8) | 1.0 (0.0, 1.9) | 34 (14.9) | 1.1 (0.0, 1.7) |
| 12–17 | 10 (70.2) | 505 (27.4) | 2.6 (1.3, 4.0) | 40 (24.6) | 2.9 (2.0, 3.7) |
| Sex | |||||
| Male | 12 (42.2) | 714 (25.7) | 1.6 (0.9, 2.5) | 56 (22.2) | 2.0 (1.6, 2.5) |
| Female | 11 (40.3) | 517 (19.2) | 2.1 (0.9, 3.1) | 42 (16.8) | 2.4 (1.4, 2.9) |
Notes. CI = confidence interval; DHS = New York City Department of Homeless Services; NYC = New York City.
United Hospital Fund areas 105, 106, and 107 in the South Bronx.
Deaths among family shelter users compared with NYC residents.
Deaths among family shelter users compared with those in NYC low-income neighborhoods.
Deaths per 100 000 are age-adjusted, except for analyses stratified by age; analysis limited to adults with children.
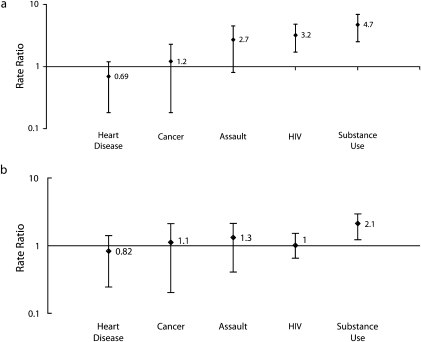
The leading causes of death among adults who used the family shelter system were heart disease (300.2 per 100 000) and cancer (296.6 per 100 000), comparable to adult rates citywide. Deaths attributable to substance use and HIV/AIDS were elevated; substance use deaths were twice as high as those for adults in the lowest-income neighborhoods and 4.7 times higher than for those in the general population (Figure 1). The HIV/AIDS death rate was 3 times higher among those who had been sheltered than among adults citywide, but was comparable with the rate in low-income neighborhoods.
FIGURE 1.
Cause-specific death rate ratios of (a) adults with children who used the New York City (NYC) Department of Homeless Services (DHS) family shelters, and NYC adults, 2001–2003, and (b) adults with children who used the DHS family shelters, and NYC low-income adults, 2001–2003.
Note. New York City (NYC) low-income adults are not limited to single adults. Source. Data on low-income adults were obtained from the 2000 US Census.12
During 2001 through 2003, there were 23 deaths among homeless children. As with homeless adults, 70% of child deaths occurred while the family was not using the shelter; the average interval between shelter exit and death was 326 days (range: 52–846). This interval was longer among those aged 1 to 4 years (353 days; range: 210–485) than among those aged 12 to 17 years (223 days; range: 52–325). Although the number of observations was low, evidence suggests that the death rate among homeless children was potentially higher than that of children citywide and in low-income neighborhoods (Table 1). The difference was most prominent among children aged 1 to 4 years and 12 to 17 years, although this variance represented only 9 and 10 child deaths, respectively. Young children who had a shelter stay of 1 or more days had a marginally higher mortality rate than did children in NYC overall and 2.6 times higher than did those in the low-income neighborhoods selected for this comparison; adolescents who used the shelter system were at nearly 3 times the mortality risk than were adolescents from both comparison populations.
The small number of child deaths precluded detailed cause-specific comparisons with citywide and low-income child populations. Proportionately, the most frequent causes of death among children using the shelter system were external injuries. Of the 23 deaths, 6 (26.1%) were caused by assaults, and 4 (17.4%) by unintentional injuries. Cancer (n = 3 or 13.0%), suicide, and chronic respiratory disease (n = 2 or 8.7% each) made up 30% of deaths. Of the 10 deaths among adolescents aged 12 to 17 years, 3 were caused by assault, 2 by cancer, and 2 resulted from suicide.
Tuberculosis
Fifteen cases of TB were diagnosed among adults who used the family shelters. Of the 14 cases for whom TB information was available, 4 (28.6%) were diagnosed while the family was in shelter, including 1 who had acid-fast bacilli smear-positive sputum, suggesting increased infectiousness.
Precision in subgroup rate estimation was limited because of the small number of cases. Nonetheless, the age-adjusted rate of TB diagnoses among adults in shelter was significantly higher (more than 3 times the rate) than among adults citywide and more than twice that in low-income neighborhoods. The TB rates among homeless men and women were 5 and 3 times higher, respectively, than in the general population. The largest disparity between shelter users and the general population was in adults aged 45 to 64 years, for whom the rate of TB was nearly 10 times higher. No cases of TB were reported among homeless adults aged 65 years or older (vs 15% of cases citywide). Tuberculosis rates among Black and Hispanic homeless adults were 5.0 and 2.3 times higher than in the general population, and 3.8 and 2.5 times higher than in low-income neighborhoods, respectively, though estimates are imprecise because of small numbers (Table 2).
TABLE 2.
Tuberculosis Cases, Rates, and Rate Ratios Among Adults With Children Who Used the New York City Department of Homeless Services Family Shelter System: New York City, 2001–2003
| TB Among NYC Total Population |
TB Among NYC Low-Income Neighborhoodsa |
||||
| TB Among Adult Family Shelter Users, No. (per 100 000 Adults)b | No. (per 100 000 Adults)b | Rate Ratioc (95% CI) | No. (per 100 000 Adults)b | Rate Ratiod (95% CI) | |
| Tuberculosis total | 15 (65.1) | 3280 (18.0) | 3.6 (2.2, 6.0) | 241 (24.4) | 2.7 (1.6, 4.5) |
| Sex | |||||
| Female | 7 (33.9) | 1236 (12.6) | 2.7 (1.3, 5.7) | 102 (18.3) | 1.9 (0.9, 4.0) |
| Male | 8 (121.9) | 2044 (24.7) | 4.9 (2.5, 9.9) | 139 (32.5) | 3.2 (1.8, 7.6) |
| Age, y | |||||
| 18–24 | 2 (13.2) | 338 (14.0) | 0.9 (0.2, 3.8) | 25 (14.5) | 0.9 (0.2, 3.9) |
| 25–44 | 6 (22.6) | 1492 (18.9) | 1.2 (0.5, 2.7) | 121 (26.2) | 0.9 (0.4, 2.0) |
| 45–64 | 7 (181.6) | 944 (18.6) | 9.8 (4.6, 20.5) | 73 (27.9) | 6.5 (3.0, 14.0) |
| ≥65 | 0 (0) | 506 (18.0) | NA | 22 (21.5) | NA |
| Race/ethnicity | |||||
| White | 0 (0) | 274 (3.5) | NA | 2 (13.2) | NA |
| Black | 12 (130.0) | 1089 (26.1) | 5.0 (2.8, 8.8) | 115 (34.4) | 3.8 (2.1, 6.8) |
| Hispanic | 3 (50.5) | 960 (21.6) | 2.3 (0.8, 7.3) | 120 (20.5) | 2.5 (0.8, 7.8) |
| Other | 0 (0) | 957 (55.6) | NA | 4 (10.7) | NA |
Notes. CI = confidence interval; NA = not applicable; NYC = New York City; TB = tuberculosis.
United Hospital Fund areas 105, 106, and 107 in the South Bronx.
Age-adjusted, except for analyses stratified by age.
TB among family shelter users compared with NYC residents.
TB among family shelter users compared with those in NYC low-income neighborhoods.
Only 2 TB cases were diagnosed during 2001 through 2003 among children who used the shelter system, for a rate similar to that in NYC's child population (3.4 per 100 000), and 1 was diagnosed while in shelter. The mother of 1 child with TB was also infected. Neither child was smear-positive.
HIV/AIDS Cases
During the study, 659 adults who used the shelter system were identified with HIV or AIDS, for an age-adjusted prevalence of 18.1 per 1000; about half (53%) had been diagnosed before 2001. Overall, the main routes of transmission for homeless adults were heterosexual sexual intercourse (35%) and intravenous drug use (17%), compared with men who have sexual intercourse with men (MSM; 27%) and intravenous drug use (37%) among the general city population. HIV-positive men who used shelter were less likely to have had sexual intercourse with men than were HIV-positive men in NYC overall (12.2% vs 38.4%; P < .001), and HIV-positive women who used shelter were less likely than were HIV-positive women in NYC to have injected drugs (13.5% vs 25.3%; P < .001).
HIV/AIDS prevalence among adults who used the shelter system was 31% higher than in the general adult population (Table 3) but lower than in low-income neighborhoods. This pattern was largely driven by homeless women, whereas prevalence among homeless men was lower than that in the other 2 populations. By age, HIV/AIDS rates were highest among those aged 45 to 64 years.
TABLE 3.
HIV/AIDS Cases, New Diagnosis Rates, and Rate Ratios Among Adults With Children Who Used the New York City Department of Homeless Services Family Shelter System: New York City, 2001–2003
| HIV/AIDS Among Adults in NYC |
HIV/AIDS Among Adults in NYC Low-Income Neighborhoodsa |
||||
| HIV/AIDS Among Adult Family Shelter Users, No. (per 1000 Adults)b | No. (per 1000 Adults)b | Rate Ratioc (95% CI) | No. (per 1000 Adults)b | Rate Ratiod (95% CI) | |
| HIV/AIDS cases | |||||
| Total | 659 (18.1) | 85 235 (13.8) | 1.31 (1.15, 1.47) | 10 211 (29.8) | 0.61 (0.54, 0.67) |
| Sex | |||||
| Female | 470 (18.0) | 25 062 (7.7) | 2.35 (1.98, 2.71) | 4109 (20.9) | 0.86 (0.73, 0.98) |
| Male | 189 (18.1) | 58 864 (20.3) | 0.89 (0.74, 1.03) | 6102 (41.3) | 0.44 (0.37, 0.50) |
| Age, y | |||||
| 18–24 | 74 (4.9) | 2825 (3.5) | 1.39 (1.11, 1.64) | 409 (7.1) | 0.69 (0.59, 0.77) |
| 25–44 | 458 (17.3) | 50 622 (19.2) | 0.90 (0.82, 0.97) | 6115 (39.8) | 0.43 (0.40, 0.46) |
| 45–64 | 126 (32.7) | 29 989 (17.7) | 1.85 (1.54, 2.15) | 3514 (40.3) | 0.81 (0.69, 0.92) |
| ≥65 | 1 (4.4) | 1799 (1.9) | 2.32 (-2.33, 6.56) | 173 (5.1) | 0.88 (-0.99, 2.26) |
| Race/ethnicity | |||||
| White | 3 (4.3) | 18 464 (8.2) | 0.52 (-0.07, 1.10) | 314 (59.6) | 0.07 (-0.01, 0.14) |
| Black | 330 (24.1) | 37 570 (26.1) | 0.93 (0.74, 1.10) | 4578 (40.3) | 0.60 (0.49, 0.70) |
| Hispanic | 136 (18.4) | 27 127 (17.4) | 1.06 (0.82, 1.29) | 5257 (25.0) | 0.74 (0.58, 0.89) |
| HIV/AIDS new diagnoses | |||||
| Total | 251 (1.8) | 13 829 (0.75) | 2.46 (2.07, 2.83) | 1897 (1.8) | 0.99 (0.86, 1.11) |
| Sex | |||||
| Female | 182 (1.9) | 4650 (0.48) | 3.91 (3.17, 4.61) | 798 (1.4) | 1.37 (1.16, 1.55) |
| Male | 69 (1.8) | 9179 (1.1) | 1.68 (1.20, 2.14) | 1099 (2.5) | 0.71 (0.53, 0.88) |
| Age, y | |||||
| 18–24 | 44 (1.0) | 1232 (0.5) | 1.89 (1.41, 2.32) | 189 (1.1) | 0.88 (0.72, 1.00) |
| 25–44 | 175 (2.2) | 8751 (1.1) | 1.95 (1.70, 2.20) | 1186 (2.7) | 0.83 (0.75, 0.90) |
| 45–64 | 32 (2.8) | 3578 (0.7) | 3.88 (2.62, 5.06) | 482 (1.9) | 1.45 (1.04, 1.79) |
| ≥65 | 0 (0) | 268 (0.10) | 0.00 | 40 (0.04) | 0.00 |
| Race/ethnicity | |||||
| White | 2 (1.0) | 2096 (0.3) | 3.00 (-1.20, 6.86) | 66 (4.5) | 0.21 (-0.11, 0.41) |
| Black | 119 (2.1) | 7417 (1.7) | 1.23 (0.95, 1.49) | 1061 (3.2) | 0.68 (0.55, 0.79) |
| Hispanic | 42 (1.7) | 4016 (0.85) | 1.95 (1.14, 2.71) | 755 (1.2) | 1.40 (0.85, 1.87) |
Notes. CI = confidence interval; NYC = New York City.
United Hospital Fund areas 105, 106, and 107 in the South Bronx.
Age-adjusted, except for analyses stratified by age.
HIV/AIDS among family shelter users compared with NYC residents.
HIV/AIDS among family shelter users compared with those in NYC low-income neighborhoods.
Although about one third of adults who were diagnosed with HIV, both citywide and in low-income neighborhoods, were diagnosed with HIV and AIDS concurrently (34.4% and 31.1%), only 16.4% of homeless adults with children were concurrently diagnosed. Among young women (aged 18–24 years), only 3.1% had a concurrent diagnosis, compared with 16.8% and 19.2% among the general and low-income populations.
We found 22 cases of HIV/AIDS among children using shelter, for a prevalence of 0.40 per 1000, much lower than the prevalence citywide (1.3 per 1000; n = 2298) and among children from low-income neighborhoods (2.4 per 1000; n = 403). One child with HIV/AIDS among homeless youths was aged younger than 5 years, 12 (55%) were aged 5 to 12 years, and 9 (41%) were aged 13 to 17 years. Most (n = 19) were infected perinatally (86%); the remaining 3 had no risk factor recorded, but were diagnosed after age 13 years, suggesting possible sexual transmission. Similarly, almost all pediatric cases citywide (95%) and among those in low-income neighborhoods (96%) were perinatally transmitted.
There were 251 new HIV/AIDS diagnoses among adults from 2001 through 2003, for an annualized rate of 1.8 per 1000. The new HIV diagnosis rate among homeless adults using shelter was more than twice as high as the citywide rate, but the same as in the lowest-income neighborhoods (Table 3). However, compared with both the general population and low-income neighborhoods, higher new diagnosis rates were found among women who used the shelter system. By age, biggest disparity between the general, low-income, and homeless populations was among adults aged 45 to 64 years.
No difference in new HIV diagnoses was observed among the 3 populations of children; there were 6 new HIV/AIDS diagnoses in homeless children during 2001 through 2003 (0.11 per 1000) compared with 238 new diagnoses in the general child population (0.04 per 1000) and 35 in low-income neighborhoods (0.07 per 1000).
Blood Lead Levels
Among children who were aged 3 years during a shelter stay from 2001 through 2003, 70.8% (95% CI = 69.8, 71.8) had BLLs tested before their third birthday, compared with rates of 90.8% (95% CI = 90.7, 91.0) for those aged 3 years living in NYC in 2001 and 96.3% (95% CI = 95.9, 96.7) for those aged 3 years in low-income neighborhoods. A larger proportion of children who had a shelter stay of at least 1 day had BLLs of 10 micrograms per deciliter or higher than did children in the other 2 groups: 59.4 per 1000 children tested (95% CI = 53.9, 65.4) had BLLs 10 micrograms per deciliter or higher (n = 381), compared with 41.7 per 1000 children tested (95% CI = 40.5, 42.9) in NYC (n = 4429) and 35.6 per 1000 children tested (95% CI = 32.2, 39.3) in the low-income neighborhoods (n = 381). We did not explore where the lead exposures occurred.
DISCUSSION
We used a novel record linkage approach to characterize patterns of illness and death among adults and children who use family shelters, a homeless subpopulation for which health information is limited. We found that rates of death and disease among adults in homeless family shelters were mostly similar to those of adults in low-income neighborhoods, but rates were elevated compared with the general population. Among children experiencing homelessness, the number of deaths was small and, thus, plausibly affected by sporadic events. However, the evidence suggests that children experiencing homelessness may be at higher risk of mortality, particularly among children aged younger than 4 years and those aged 12 to 17 years, compared with both NYC general population children and those living in low-income neighborhoods.
Most previous studies examining homeless children's health have focused on access to care and preventive health services among adolescents rather than health status. We looked at select health outcomes of children who used shelter. We found that they had a higher mortality rate than did children citywide or in low-income neighborhoods, and relative mortality among children in the youngest and oldest age groups accounted for most of this difference. As in low-income neighborhoods, more than 4 in 10 deaths were identified as amenable to prevention (unintentional injuries and assaults). Seven in 10 deaths among children occurred out of shelter, occurring, on average, nearly a year after the shelter episode, thus not necessarily reflecting increased risk while in shelter per se, but potentially broader risks faced by families who use shelter care.
HIV and TB were not elevated among homeless children, but a high proportion had elevated BLLs and a lower likelihood of having received a lead test than did children citywide or in low-income neighborhoods. Homeless children often come from poor-quality, unstable housing, and are potentially exposed to lead in various environments and at different points in their lives. Families with children in shelter would benefit from enhanced efforts to link them to lead screening and education on preventing lead poisoning from lead-based paint hazards and nonpaint lead sources (such as contaminated imported consumer products). Because of the small number of observations in this study, larger studies focusing on childhood mortality would better characterize the potential risks preliminarily identified in this study.
The overall mortality rate among adults in family shelters was similar to that of the general NYC and low-income adult populations; the rate was substantially lower than were mortality estimates documented among single homeless adults in NYC during the same period11 or from other studies examining single homeless adults.3,15 The leading causes of death among adults who used shelters were heart disease and cancer, similar to general and low-income populations in NYC, confirming that these conditions and related high-risk behaviors, such as poor diet, lack of exercise, and smoking, should be addressed not only in the general population, but also among homeless individuals. Although the risk of death from HIV/AIDS and substance use was higher among adults in shelters than in the general public, only deaths from substance use were higher among homeless adults than in low-income neighborhoods. This finding suggests that issues of poverty may be the root cause of poor health among this population, requiring a focus on prevention, quality of care, and linkages to primary care professionals in broader low-income populations from which most homeless individuals come. However, the population in need of shelter may require extra measures to combat substance use and prevent overdose.
We found no previous studies of TB among homeless families; research on single homeless adults, mostly in congregate settings, has identified higher TB prevalence estimates than ours (32% to 79%).11,16,17 This risk differential may partially reflect the fact that single homeless adults may come in contact with higher-risk individuals. In addition, previous research has shown that homeless individuals living in more crowded situations have a higher likelihood of TB infection,17 and family shelters in NYC are typically apartment-based housing, not group or congregate settings. We documented an elevation in TB case rates, most of which were diagnosed when not in shelter. This elevated risk among homeless individuals compared with both general population and low-income adults is not well understood. For TB diagnoses and substance use mortality, which was also elevated, it is possible that poor health status related to substance abuse or congregate settings (e.g., previous incarceration) may predispose some families in low-income neighborhoods to becoming homeless. Irrespective of potential unmeasured selection factors, the suggested elevated burden of TB and substance-use deaths warrants additional study.
Earlier studies have found a wide range of HIV/AIDS rates among single homeless adults (4%–62%).11,18 One previous study examined HIV in homeless families and found similar results to ours (1.1%).18 We documented higher HIV/AIDS prevalence and new diagnosis rates among homeless adults compared with the general population, but these rates were similar to or lower than those found in low-income communities. Half were diagnosed before the study, again pointing to the potential impact of poverty and social disadvantage. HIV/AIDS prevalence was higher among homeless women than men, potentially because of the lower prevalence of MSM in family shelters. Although less than 2% of homeless women were HIV positive during the study period, they were 4 times more likely to be newly diagnosed with HIV than were women in the general population and had a higher new disease rate than did women in low-income neighborhoods. This pattern may reflect improved diagnosis from increased screening, rather than a higher true incidence of disease.
Among those diagnosed with HIV, we observed a lower rate of concurrent AIDS diagnoses among those who used the shelter system, compared with similar individuals in the general NYC and the low-income populations. This may be a reflection of the demographic make-up of the population. Adults in our homeless family study population consisted of fewer MSM than in either comparison population, and were mostly young women; all had children. Since 1997, New York State has had mandatory newborn and optional prenatal HIV screening programs, which might account for the low rate of concurrent diagnosis in the homeless population.
Despite elevated risks of TB and HIV/AIDS, the attributable burden of homeless families on these citywide disease rates was relatively small. Previous estimates by the Centers for Disease Control and Prevention and NYC Department of Health and Mental Hygiene suggest that about 6% of reported TB cases in the United States and NYC are among homeless persons.19,20 Although these estimates may be true for the full homeless population, we found that adults utilizing family shelters constituted less than 1% of the TB and HIV/AIDS cases in NYC.
Limitations
Several limitations should be noted. First, this study focused on the health of adults and children who spent at least 1 night in a DHS family shelter during 2001 through 2003; as a result, data are not generalizable to families who use alternate homeless shelter systems.
Second, the low-income neighborhood comparison group does not represent all low-income New Yorkers on all indices. For example, BLLs have been shown to be higher in other low-income neighborhoods than in those utilized in these analyses.21 By selecting neighborhoods based on percentage of households living below a certain poverty level, we aimed to compare the health of homeless families to that of families living in poor neighborhoods. However, not all families in those neighborhoods are poor, and aspects of neighborhoods with high concentrations of poverty may influence health status in both positive and negative ways that are different from the influence of individual-level poverty. For example, high-poverty neighborhoods tend to have large concentrations of public housing, which may concentrate or facilitate certain social services as well as maintain a certain physical housing standard. This trend may explain why BLL test rates were higher among children from low-income families, but rates of elevated BLLs were lower, compared with those in the NYC general population or children in homeless families. The same trend may also partially explain the comparable death rates among children in low-income neighborhoods and NYC children overall.
Third, the matching process between registries was imperfect and may have missed cases, which would also underestimate the disease burden. Fourth, the data did not include deaths and illnesses of homeless persons who left NYC during the 3-year period; again, these data would have led to underestimation of morbidity and mortality in the homeless population. Fifth, in some analyses, the numbers of shelter residents were small and the cases rare, resulting in imprecise estimates of morbidity and mortality. Sixth, because this study was designed as a linkage study between administrative records and health registries (and did not involve medical chart reviews), we had limited information about the specific illness and mortality profiles or types of care that individuals received. This limitation hindered our ability to assess, for example, the accuracy of cause of death or the timeliness, consistency, or appropriateness of cardiovascular disease—, TB-, or HIV-related treatment. Seventh, we had limited access to data on homeless children's health; future research should identify additional reliable health indicators for this group. Childhood estimates of morbidity and mortality also did not include infants and may be an underestimate of disease burden in this population. Finally, our study was cross-sectional, so no inferences about causality or the effectiveness of interventions can be made.
Conclusions
Our findings demonstrate that the health outcomes of adults in families experiencing homelessness are mainly representative of outcomes for low-income adults in NYC, although homeless children are at higher risk on some measures. These results suggest that homeless children may differ from those living in low-income neighborhoods who are not homeless. Previous research indicates that families experiencing homelessness are likely to have lived in poorer quality housing and to have moved frequently before shelter entry.22,23 Efforts to improve the health of the homeless population should thus be centered on community-based prevention in low-income neighborhoods to improve the health and well-being of high-risk individuals. Targeted interventions should increase efforts to link families at risk for homelessness with substance-use treatment, lead poisoning prevention services, and primary health care in the community, and should renew and reinforce those linkages in shelter so families remain connected with health care providers as they exit shelter and return to permanent housing in the community.
Acknowledgments
We would like to acknowledge Jiehui Li, Benjamin Tsoi, Maryanne Schretzman, Wenhui Li, David Hanna, Lucia Torian, Alexander Gutkovich, Veronica Neville, Jennifer Chudy, and Joanna Weissman for their contributions to this article.
Human Participant Protection
This study involved secondary analysis of administrative data; institutional review board approval was not required.
References
- 1.Haddad MB, Wilson TW, Ijaz K, Marks SM, Moore M. Tuberculosis and homelessness in the United States, 1994-2003. JAMA. 2005;293(22):2762–2766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338(24):1734–1740 [DOI] [PubMed] [Google Scholar]
- 3.Hwang SW. Mortality among men using homeless shelters in Toronto, Ontario. JAMA. 2000;283(16):2152–2157 [DOI] [PubMed] [Google Scholar]
- 4.Barrow SM, Herman DB, Córdova P, Struening EL. Mortality among homeless shelter residents in New York City. Am J Public Health. 1999;89(4):529–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee TC, Hanlon JG, Ben-David J, et al. Risk factors for cardiovascular disease in homeless adults. Circulation. 2005;111(20):2555–2556 [DOI] [PubMed] [Google Scholar]
- 6.Nyamathi A, Berg J, Jones T, Leake B. Predictors of perceived health status of tuberculosis-infected homeless. West J Nurs Res. 2005;27(7):896–910 [DOI] [PubMed] [Google Scholar]
- 7.Little M, Shah R, Vermeulen MJ, Gorman A, Dzendoletas D, Ray JG. Adverse perinatal outcomes associated with homelessness and substance use in pregnancy. CMAJ. 2005;173(6):615–618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Dept of Housing and Urban Development The Fourth Annual Homeless Assessment Report to Congress. July 2009. Available at: http://www.hudhre.info/documents/4thHomelessAssessmentReport.pdf. Accessed April 15, 2010
- 9.Burt M, Aron LY, Lee E, Valente J. Helping America's Homeless: Emergency Shelter or Affordable Housing? Washington, DC: The Urban Institute Press; 2001 [Google Scholar]
- 10.The Department of Housing and Urban Development (HUD) Third Homelessness Pulse Report. Washington, DC: US Dept of Housing and Urban Development; January 2010 [Google Scholar]
- 11.Kerker BD, Bainbridge J, Li W, et al. The health of homeless adults in New York City: a report from the New York City Departments of Health and Mental Hygiene and Homeless Services. New York, NY: New York City Departments of Health and Mental Hygiene and Homeless Services; December 2005 [Google Scholar]
- 12.US Census Bureau. Census 2000 Summary File 3. Available at: http://factfinder.census.gov/servlet/DatasetMainPageServlet?_program=DEC&_submenuId=datasets_1&_lang=en. Accessed August 15, 2008.
- 13.New York City Dept of Health and Mental Hygiene United Hospital Fund neighborhoods and zip code areas. Available at: http://www.nyc.gov/html/doh/downloads/pdf/survey/uhf_map_100604.pdf. Accessed August 15, 2008
- 14.NYS Regulations for lead poisoning prevention and control – NYCRR Title X, Part 67, subpart 67–1.2, lead screening and follow-up of children by health care providers. Available at: http://www.health.state.ny.us/regulations/nycrr/title_10/part_67/#sec67-1-2. Accessed April 16, 2009.
- 15.Hibbs JR, Benner L, Klugman L, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331(5):304–309 [DOI] [PubMed] [Google Scholar]
- 16.Zolopa AR, Hahn JA, Gorter R, et al. HIV and tuberculosis infection in San Francisco's homeless adults. JAMA. 1994;272(6):455–461 [PubMed] [Google Scholar]
- 17.Paul EA, Lebowitz SM, Moore RE, Hoven CW, Bennett BA, Chen A. Nemesis revisited: tuberculosis infection in a New York City men's shelter. Am J Public Health. 1993;83(12):1743–1745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Culhane DP, Gollub E, Kuhn R, Shpaner M. The co-occurrence of AIDS and homelessness: results from the integration of administrative databases for AIDS surveillance and public shelter utilisation in Philadelphia. J Epidemiol Community Health. 2001;55(7):515–520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention Tuberculosis transmission in a homeless shelter population—New York 2000-2003. MMWR Morb Mortal Wkly Rep. 2005;54(6):149–152 [PubMed] [Google Scholar]
- 20.New York City Dept of Health and Mental Hygiene 2004 TB Annual Summary. New York, NY: Bureau of Tuberculosis Control; 2005. Available at: http://www.nyc.gov/html/doh/downloads/pdf/tb/tb2004.pdf. Accessed April 20, 2009 [Google Scholar]
- 21.New York City Dept of Health and Mental Hygiene New York City Childhood Lead Poisoning Prevention Program, Annual Report 2002. New York, NY: Lead Poisoning Prevention Program; 2004. Available at: http://nyc.gov/html/doh/downloads/pdf/lead/lead-2002report.pdf. Accessed June 23, 2010 [Google Scholar]
- 22.Shinn M, Weitzman B, Stojanovic D, et al. Predictors of homelessness among families in New York City: from shelter request to housing stability. Am J Public Health. 1998;88(11):1651–1657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Markee P. Housing a Growing City: New York's Bust in Boom Times. New York, NY: Coalition for the Homeless; July 2002 [Google Scholar]