Abstract
Accumulating evidence indicates that cannabis use may be a risk factor for schizophrenia (SZ), and chronic cannabis users score higher than non-users on measures of schizotypal personality traits. The purpose of the present study was to investigate the relations between normal personality, schizotypy, and cannabis use. Sixty-two chronic cannabis users and 45 cannabis-naïve controls completed a measure of normal personality, the NEO-Five Factor Inventory (NEO-FFI), and two measures of schizotypy, the Schizotypal Personality Questionnaire (SPQ) and Perceptual Aberration Scale (PAS). Substance use was assessed using the SCID I alcohol/drug module and a locally developed drug use questionnaire. On the NEO-FFI, users scored higher than controls on Openness, but lower on Agreeableness and Conscientiousness, and endorsed greater schizotypy on the SPQ and PAS. Higher Neuroticism predicted greater schizotypy in both groups, and, higher Extraversion predicted lower negative-syndrome schizotypy among users. Finally, duration of cannabis use was positively correlated with scores on the SPQ and PAS among users, suggesting a relation between overall cannabis use chronicity and schizotypy. These data show that cannabis users differ from non-users on dimensions of normal personality and schizotypy, and provide further evidence that cannabis use is associated with increased levels of psychosis-related personality traits.
Keywords: Five-factor model, marijuana, Schizotypal Personality Questionnaire, Perceptual Aberration Scale, schizophrenia
1. Introduction
Cannabis is the most popular illicit substance of abuse in the United States (SAMHSA, 2007), and previous research has linked chronic use of this drug to personality traits associated with increased psychosis-proneness, or schizotypy (Compton et al., 2007). However, relatively little research has investigated relations between chronic cannabis use and facets of normal personality, such as the “Big Five” dimensions specified by the Five Factor Model (Digman, 1990). Variations in normal personality dimensions have been linked previously to increased schizotypy in community samples (Costa and McCrae, 1990; Coolidge et al., 1994; Dyce and O'Connor, 1998; Ross et al., 2002), but no previous research has investigated relations among scores on measures of normal personality, schizotypy, and the use of cannabis. A more thorough understanding of such associations may identify risk factors and inform intervention strategies by characterizing personality traits associated with psychosis-proneness in cannabis users.
1.1. The Five Factor Model and cannabis use
The Five Factor Model (FFM) is a well-validated taxonomy of normal personality derived from factor-analytic studies of lexical descriptors and questionnaire measures of personality traits (McCrae and Costa, 1987; Digman, 1990; McCrae and John, 1992). This model has been used to study personality in healthy individuals (e.g., Costa and McCrae, 1992a; McCrae and John, 1992) as well as in persons with diverse forms of Axis I (for a recent meta-analysis, see Malouff et al., 2005) and Axis II (for a recent meta-analysis, see Saulsman and Page, 2004) psychopathology. The five personality dimensions specified by the FFM are Neuroticism (i.e., the tendency to experience negative affect or distress), Extraversion (i.e., the tendency to be sociable, outgoing, and experience positive affect), Openness (i.e., the tendency to be imaginative, intellectually curious, and seek out new experiences), Agreeableness (i.e., the tendency to sympathetic, cooperative, and nurturing), and Conscientiousness (i.e., the tendency to be well-organized, self-disciplined, and deliberate).
Although cannabis is more widely used than any other illicit substance, few studies have attempted to characterize the personalities of chronic cannabis users according to the FFM. One study found that symptoms of cannabis abuse/dependence were positively related to Openness, but negatively related to Agreeableness and Conscientiousness (Flory et al., 2002). However, after controlling for alcohol abuse/dependence, antisocial personality disorder, and internalizing symptoms, cannabis abuse/dependence symptoms were negatively related to Extraversion and positively related to Openness in that sample. A separate study using a large (n = 1,102) epidemiologic sample found that current cannabis users were lower in Agreeableness and Conscientiousness, but higher in Openness, relative to never-users (Terracciano et al., 2008). However, the effects of non-cannabis substances were not controlled for in that study, making it difficult to disentangle those personality dimensions which may be associated specifically with cannabis use from those associated with the use of other drugs. Regardless, the studies by Flory and colleagues (2002) and Terracciano and colleagues (2008) suggest that chronic cannabis use appears related to normal levels of Neuroticism, high Openness, and low Agreeableness and Conscientiousness.
1.2. Schizotypy and cannabis use
Schizotypy is a constellation of personality characteristics reflecting “psychosis proneness” (Chapman et al., 1976; Raine, 1991, 2006). Schizotypy may be conceptualized as tri-dimensional, incorporating positive-syndrome (e.g., cognitive-perceptual distortions such as odd perceptual experiences, magical thinking, and paranoia), negative-syndrome or negative-syndrome (e.g., interpersonal deficits such as constricted affect, few close friends, and social anxiety), and disorganized-syndrome (e.g. odd or eccentric speech or behavior) traits (Raine, 2006). Other studies have identified a fourth SPQ factor (paranoia) in addition to those described above (Stefanis et al., 2004; Compton et al., 2009b); however, we interpreted the data presented in this report in terms of the traditional three-factor model since most previous research has used this structure (Raine, 2006). Individuals with schizotypal personality disorder (SPD) exhibit a pervasive pattern of interpersonal deficits characterized by a lack of close relationships, as well as cognitive or perceptual distortions and eccentric behavior (APA, 2000).
Several studies have reported that cannabis users score higher than non-users on measures of positive-syndrome schizotypy (Mass et al., 2001; Skosnik et al., 2001; Verdoux et al., 2002; Earleywine, 2006; Skosnik et al., 2008; Compton et al., 2009a). The relation between cannabis use and negative-syndrome schizotypy is less clear. Some studies have found that users reported significantly more negative-syndrome schizotypy symptoms than non-users (Mass, et al., 2001; Bailey and Swallow, 2004; Compton, et al., 2009a), while another study reported no such differences (Skosnik, et al., 2001). Most recently, Skosnik and colleagues (2008) reported that cannabis use was associated with lower scores on a measure of negative-syndrome schizotypy. Lastly, several studies have noted a relation between cannabis use and increased disorganized-syndrome schizotypy (Mass, et al., 2001; Skosnik, et al., 2001; Dumas et al., 2002; Bailey and Swallow, 2004; Barkus and Lewis, 2008; Esterberg et al., 2009). It is unclear whether elevated schizotypy is a causal influence or consequence of heavy cannabis use. Elevations on schizotypal personality traits may predispose individuals to use cannabis; alternatively, usage of that drug may elicit positive (i.e., perceptual disturbances) or negative (i.e., the “amotivational syndrome”) psychotic symptoms in heavy users (Verdoux, et al., 2002).
1.3. The relation between the FFM and schizotypy in non-clinical samples
Previous studies of personality in non-clinical or community samples have noted associations between the personality dimensions specified by the FFM and scores on measures of schizotypal personality traits, although such associations have not been explored previously in cannabis users (for meta-analyses, see Saulsman and Page, 2004; Samuel and Widiger, 2008). High schizotypy has been most frequently associated with high Neuroticism, but low Extraversion (Costa and McCrae, 1990; Coolidge, et al., 1994; Trull et al., 2001; Bagby et al., 2005; Mullins-Sweatt et al., 2006), low Agreeableness (Costa and McCrae, 1990; Coolidge, et al., 1994; Trull, et al., 2001; Mullins-Sweatt, et al., 2006), and low Conscientiousness (Coolidge, et al., 1994; Trull, et al., 2001; Bagby, et al., 2005; Mullins-Sweatt, et al., 2006). Less frequently, high schizotypy has been associated with increased Openness as well (Coolidge, et al., 1994; Trull, et al., 2001; Mullins-Sweatt, et al., 2006).
Prior research with non-clinical samples has identified relations between specific syndrome dimensions of schizotypy and FFM personality traits among these individuals as well. Scores on measures of positive-syndrome schizotypy have been associated with increased Neuroticism and Openness (Ross, et al., 2002), but decreased Agreeableness (Ross, et al., 2002; Camisa et al., 2005). In contrast, scores on measures of negative-syndrome schizotypy have been associated with increased Neuroticism (Ross, et al., 2002; Camisa, et al., 2005), decreased Extraversion and Agreeableness (Ross, et al., 2002; Camisa, et al., 2005), and decreased Openness (Ross, et al., 2002). We know of no previous investigations of relations between FFM personality dimensions and disorganized-syndrome schizotypy specifically, although one study considered disorganized symptoms (i.e., odd thinking and speech) as part of the positive schizotypy syndrome (Gurrera et al., 2005).
1.4. Objectives of the present study
The primary objective of this study was to compare current cannabis users with cannabis naïve controls on measures of FFM personality dimensions and schizotypy, and to examine the relations among those measures within each group. To our knowledge, this is the first study to investigate these relations in cannabis users, thereby bridging the gap between measures of normal and abnormal personality in these individuals. We predicted that cannabis users would exhibit higher Openness, but lower Agreeableness and Conscientiousness, than would cannabis-naïve controls. We also predicted that chronic cannabis users would exhibit higher scores on the SPQ and PAS, suggesting greater psychosis-proneness among those individuals relative to never-users. In addition, we explored potential dose-response relations between cannabis use and personality (Skosnik et al., 2006) by correlating personality traits with cannabis usage variables (total years of cannabis use, age of first use, and frequency of use).
2. Methods
2.1. Participants
Sixty-two current cannabis users and 45 healthy drug-naive controls participated in the present study. Participants were recruited from the local university community and were paid for their participation. The study protocol was approved by the Indiana University Human Subjects Committee, and written informed consent was obtained from all participants. Participant data was de-identified to protect confidentiality, and all participants were compensated $10/hour for their participation. Cannabis users who reported past use of three or more non-cannabis illicit substances, reported use of an illicit substance other than cannabis within three months prior to their study participation, or who met criteria for a non- cannabis-related DSM-IV psychopathology were excluded from the study to minimize the influence of those variables on the results. The control group was composed entirely of cannabis-naïve individuals to minimize the influence of previous cannabis exposure on the present results.
Formal inclusion criteria were as follows: 1) For the cannabis group: current cannabis consumption at the rate of at least once per week during the past month, no other illicit substance use during the past three months, and no DSM-IV diagnosis of Axis I or II disorders except cannabis abuse or dependence; 2) For the control group: no history of illicit substance use and no history of psychiatric illness (Axis I or II); 3) For all participants: age 18 years or older, completion of high school education, no history of cardiovascular disease, hearing problems, neurological disease, learning disability, or head injury resulting in loss of consciousness. Participants in the cannabis group were required to abstain from cannabis use for at least 24 hours prior to their participation in the study to eliminate possible acute cannabis effects during data collection.
2.2. Clinical Interviews and Drug Use Assessment
The Structured Clinical Interview for DSM-IV Axis I and II Disorders (SCID-I and SCID-II; First et al., 1997; First et al., 2002) were used to rule out previous psychiatric conditions and assess drug use histories. The Picture completion, Digit Symbol, Similarities, and Digit Span subscales of the Wechsler Adult Intelligence Scale III (WAIS-III; Wechsler, 1997), were used to examine general neuropsychological functioning.
The SCID-I and a locally developed drug-use questionnaire were used to ascertain current and past diagnoses for substance abuse and dependence, as well as current and past cannabis consumption patterns. Measures of frequency, quantity, and density of cannabis consumption were determined via the SCID-I and questionnaire for the past three months, then for one month prior to the test session. Total lifetime cannabis use was also estimated (age of first use and total years of use). Participants were instructed to consider each day of the week and indicate, for an average week, how much they consumed per drug-use occasion over the past three months, and then for the month prior to testing. Recency and density of last use was assessed using the past month section of the interview. Lifetime use was estimated by calculating total months of active use since the onset of initial cannabis use, which accounts for different periods of non-use, and a measure of overall density of use (total amount ever used/total months active use).
Self-reported recent drug use was corroborated using urine drug screens (Q10-1, Proxam) for a portion of subjects (32 control and 45 cannabis-using participants). The Q10-1 kit screens for cannabis, opiates, amphetamines, cocaine, MDMA (ecstasy), tricyclic antidepressants, phencyclidine, benzodiazepines, methamphetamines, and barbiturates. Participants included in the control group tested negative for all drugs, whereas those included in the cannabis-using group tested positive for cannabis only.
Demographic data for both participant groups are shown in Table 1. There was a small, but significant, difference between the groups for years of education. The groups differed significantly for average number of alcoholic drinks consumed per week and proportion who were current tobacco users, but did not differ on sex, age, or WAIS subtest performance (data on tobacco use were unavailable for one control participant and two cannabis-using participants).
Table 1.
Demographic information
| Group |
|||
|---|---|---|---|
| CON Mean (S.D.) |
THC Mean (S.D.) |
p |
|
| Sex (Males: Females) | 21 : 24 | 40 : 22 | NSa |
| Age | 21.53 (3.27) | 21.11 (3.55) | NSb |
| Education | 14.93 (1.60) | 14.23 (1.36) | < 0.05b |
| Picture Completion (WAIS) | 13.04 (3.57) | 12.05 (2.46) | NSb |
| Digit Symbol Coding (WAIS) | 11.93 (2.96) | 10.98 (2.56) | NSb |
| Similarities (WAIS) | 12.38 (2.86) | 12.53 (2.73) | NSb |
| Digit Span (WAIS) | 11.76 (2.72) | 11.87 (3.10) | NSb |
| Drinks/week | 0.89 (1.51) | 5.53 (4.67) | < 0.001b |
| Tobacco use (Users:Non-users) | 1 : 43 | 24 : 35 | < 0.001a |
| Age at First Cannabis Use (Yrs) | 15.38 (2.17) | ||
| Total Years of Use | 5.59 (3.33) | ||
| Frequency of Cannabis Use (previous month) | 40.94 (41.10) | ||
Note: N.S. = non-significant.
Chi-square,
t-test.
2.3. NEO Five-Factor Inventory
Participants completed the NEO Five-Factor Inventory (NEO-FFI, Form S; Costa and McCrae, 1992b), a 60-item assessment of the “Big Five” personality traits. Participants rated how much each NEO-FFI item applied to them on a five-point scale ranging from “strongly agree” to “strongly disagree”. Total scores for each of the Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness factors were derived from each participant's responses to the test items and converted to T scores based upon adult gender-combined normative data (Costa and McCrae, 1992b). Internal consistency estimates (coefficient alpha) for the NEO-FFI subscales were estimated to range from 0.81 to 0.93 in the present study, based upon data from 20 random participants (10, control, 10 user). Six-month test-retest reliability for this measure has been shown to range from 0.80 (Agreeableness) to 0.87 (Openness) (Murray et al., 2003).
2.4. Schizotypal Personality Questionnaire
All subjects were given the schizotypal personality questionnaire (SPQ) developed by Raine (1991). The SPQ is composed of 74 yes/no questions organized into nine subscales based upon the diagnostic features of schizotypal personality disorder (SPD) in the DSM-IV. The SPQ has been used previously to investigate schizotypy in cannabis users (e.g., Skosnik, et al., 2001; Skosnik, et al., 2006; Skosnik, et al., 2008) and non-clinical samples (Raine, 1991; Noguchi et al., 2008). Factor analysis of the SPQ (Raine et al., 1994) revealed that its 9 symptom subscales load onto three factors corresponding to broader symptom dimensions of SPD and schizophrenia-spectrum disorders: Cognitive-Perceptual distortions (i.e., positive symptoms), composed of the Ideas of Reference, Odd beliefs/Magical Thinking, Unusual Perceptual Experiences, and Suspiciousness/Paranoid Ideation subscales; Interpersonal deficits (i.e., negative symptoms), composed of the Social Anxiety, No Close Friends, Constricted Affect, and Suspiciousness/Paranoid Ideation subscales; and Disorganized symptoms, composed of the Odd Behavior and Odd Speech subscales. Dependent measures included the total number of affirmative answers to all items (SPQ Total) as well as the number of affirmative answers to the individual subscale and factor items. Thus, higher scores indicate an increased tendency toward schizotypy. Estimated internal reliability for the SPQ was high in the present sample (coefficient alpha = 0.92).
2.5. Perceptual Aberration Scale
The Perceptual Aberration Scale (PAS; Chapman et al., 1978) a 35-item, true/false assessment of unusual perceptual or body-image experiences sometimes reported by patients with psychotic disorders. In contrast to the broader scope of the SPQ, the main focus of the PAS is on individuals' prior experiences with unusual body sensations (e.g., “I have sometimes felt that some part of my body no longer belongs to me”). Estimated internal reliability for the PAS was good in the present sample (coefficient alpha = 0.83).
2.6. Statistical Analysis
Demographic and questionnaire measures were compared between groups. Chi-square was used for qualitative between-group comparisons, and MANOVA was used for quantitative comparisons. Follow-up one-way ANOVAs clarified the sources of significant group main effects. Hierarchical multiple regression was used to explore potential relations between NEO-FFI scores and schizotypy measures (SPQ, PAS) after adjusting for demographic variables (age, sex) and alcohol use (drinks/week). For the cannabis group, Pearson correlations were used to investigate the relation between cannabis usage variables (total years of cannabis use, age at first cannabis use, and frequency of use over the past month) and personality scores. Significance level was set to α ≤ 0.05 for all statistical analyses.
3. Results
3.1. NEO-FFI scores
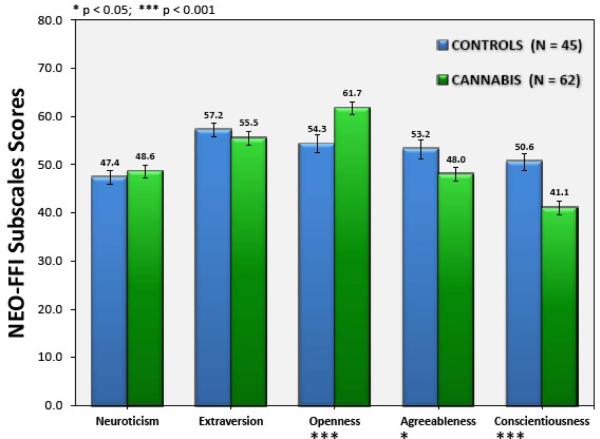
Figure 1 shows the mean scores of the cannabis and control groups for each of the five NEOFFI traits. There was a significant effect of group [Wilks's Lambda = 0.76, F(5, 101) = 6.37, p < 0.001; multivariate partial η2 = 0.24]. Follow-up ANOVAs revealed that the cannabis group scored higher than the control group on the Openness scale [F(1, 105] = 11.57, p < 0.001; Cohen's d = 0.67], but lower on the Agreeableness [F(1, 105) = 5.02, p < 0.05, d = 0.44] and Conscientiousness [F(1, 105) = 18.71, p < 0.001, d = 0.85] scales.
Figure 1.
Mean (±SEM) scores of the control and cannabis groups for each of the five NEO-FFI personality dimensions.
3.2. SPQ and PAS scores
Table 2 shows the mean (S.D.) total score on the SPQ for the cannabis and control groups, as well as each group's score on the three SPQ schizotypy factors and individual subscales of that measure. The cannabis group scored higher than the control group on the SPQ overall, F(1, 105) = 5.79, p < 0.05, d = 0.48. Cannabis users scored higher than controls on the Cognitive-Perceptual [F(1, 105) = 4.31, p < 0.05, d = 0.41] and Disorganized [F(1, 105) = 9.77, p < 0.01, d = 0.62] factors of the SPQ. The groups did not differ significantly in terms of their scores on the Interpersonal factor [F(1, 105) = 2.06, p =0.15].
Table 2.
Mean (S.D.) scores on SPQ subscales for the control (CON) and cannabis-using (THC) groups.
| Group |
|||
|---|---|---|---|
| CON Mean (SD) |
THC Mean (SD) |
pa |
|
| SPQ Total | 12.82 (9.26) | 18.24 (12.88) | < 0.05 |
| SPQ subscale scores | |||
| Ideas of reference | 1.89 (2.13) | 2.32 (2.38) | NS |
| Social anxiety | 1.62 (1.48) | 1.95 (2.19) | NS |
| Magical thinking/odd beliefs | 0.87 (1.24) | 1.35 (1.94) | NS |
| Unusual perceptual experiences | 1.04 (1.24) | 1.90 (2.19) | < 0.05 |
| Eccentric/odd behavior | 1.04 (1.58) | 2.50 (2.36) | < 0.001 |
| No close friends | 1.36 (1.67) | 1.40 (1.74) | NS |
| Odd speech | 2.20 (2.16) | 2.97 (2.37) | NS |
| Constricted affect | 1.84 (1.30) | 2.21 (1.34) | NS |
| Suspiciousness/paranoia |
0.96 (1.48) |
1.63 (1.86) |
< 0.05 |
| SPQ syndrome (factor) scores | |||
| Cognitive-Perceptual | 4.76 (4.95) | 7.21 (6.71) | < 0.05 |
| Interpersonal | 5.78 (4.07) | 7.19 (5.64) | NS |
| Disorganized |
3.24 (3.16) |
5.47 (3.94) |
< 0.01 |
| PAS Total | 1.33 (1.65) | 3.49 (4.89) | < 0.01 |
Note: N.S = non-significant.
ANOVA.
The scores of each group on the individual subscales of the SPQ were compared using MANOVA. There was an overall main effect of Group [Wilks's Lambda = 0.83, F(9, 97) =2.25, p < 0.05, multivariate partial η2 = 0.17]. Cannabis users scored higher than controls on the Unusual Perceptual Experiences [F(1, 105) = 5.59, p < 0.05, d = 0.48], Odd Behavior/Appearance [F(1, 105) = 12.91, p < 0.001, d = 0.72], and Suspiciousness/Paranoid Ideation [F(1, 105) = 4.05, p < 0.05,d = 0.39] subscales.
Between-group differences on the PAS were investigated via ANOVA. PAS data were missing for two members of the cannabis group. Mean (S.D.) scores for each group on that measure were 1.33 (1.65) for controls and 3.49 (4.89) for cannabis users, which were significantly different, [F(1, 102) = 8.06, p < 0.01, d = 0.62].
3.3. Relations between SPQ/PAS and NEO-FFI scores
We conducted hierarchical multiple regression analyses to examine the relation between NEO-FFI personality dimensions and scores on the SPQ and PAS for each group separately. Participant sex, age, and average number of drinks per week were entered in the first step of the model, and scores on all five NEO-FFI dimensions were entered in the second step. Thus, the model tested the association between normal personality dimensions (NEO scores) and schizotypy after accounting for the effects of sex, age, and alcohol consumption. We did not include education in step 1 of our model because education were highly correlated with age (r = 0.54, p < 0.001) within our sample. The results of this analysis are summarized in Table 3.
Table 3.
Hierarchical multiple regression predicting SPQ factor and total score and PAS total score with NEO-FFI dimension scores.
| Dependent variable |
Step |
Significant Predictors |
β
|
Total R2 |
R2change (step) |
F for R2 change |
|
|---|---|---|---|---|---|---|---|
| CON | SPQ Cognitive-Perceptual | 2 | Neuroticism | 0.56** | 0.28 | 0.25 | 2.39† |
| SPQ Interpersonal | 2 | Neuroticism | 0.45** | 0.31 | 0.27 | 2.78* | |
| SPQ Disorganized | Drinks/week | −0.33* | |||||
| 2 | Neuroticism | 0.51** | 0.50 | 0.40 | 5.68*** | ||
| Openness | 0.28* | ||||||
| SPQ Total Score | 2 | Neuroticism | 0.61*** | 0.41 | 0.35 | 4.20** | |
| PAS Total Score | 2 | Neuroticism | 0.58** | 0.35 | 0.33 | 3.57* | |
| THC | SPQ Cognitive-Perceptual | 2 | Age | 0.23* | 0.55 | 0.46 | 10.27*** |
| Neuroticism | 0.60*** | ||||||
| SPQ Interpersonal | 2 | Neuroticism | 0.63*** | 0.66 | 0.61 | 17.98*** | |
| Extraversion | −0.29** | ||||||
| SPQ Disorganized | 1 | Age | 0.34** | 0.14 | 0.14 | 2.93* | |
| Age | 0.26* | ||||||
| 2 | Neuroticism | 0.30* | 0.49 | 0.35 | 7.04*** | ||
| Openness | 0.31** | ||||||
| SPQ Total Score | 2 | Age | 0.25** | 0.62 | 0.51 | 13.69*** | |
| Neuroticism | 0.59*** | ||||||
| PAS Total Score | 2 | Neuroticism | 0.40** | 0.27 | 0.22 | 3.00* |
Note: Sex, age, and alcohol use (drinks/week) were entered simultaneously in Step 1. Only significant coefficients (β values) are shown.
p < 0.10;
p < 0.05;
p < 0.01;
p < 0.001.
Among controls, NEO-FFI variables significantly improved the ability of the model to predict SPQ Interpersonal syndrome, SPQ Disorganized syndrome, SPQ total, and PAS total scores after accounting for the demographic variables identified above (all R2 change ≥ 0.27, all p < 0.05, see Table 3). The improvement in the ability of the model to predict SPQ Cognitive-Perceptual factor scores after including NEO scores was significant at the trend level (R2 change = 0.25, p = 0.06) among controls. Among users, NEO-FFI variables significantly improved the ability of the model to predict all schizotypy variables among users (all R2 change ≥ 0.27 all ps < 0.05).
Neuroticism scores significantly predicted all schizotypy variables among both controls (all βs ≥ 0.43, all p-values < 0.05) and users (all βs ≥ 0.30, all p-values < 0.05). In addition, Openness significantly predicted SPQ Disorganized factor scores for both groups (control β = 0.29, p < 0.05; user β = 0.35, p < 0.01). In contrast, Extraversion scores improved the ability of the model to predict SPQ Interpersonal factor scores among users (β = −0.29, p < 0.01) but not controls (β = −0.19, n.s.). Age significantly predicted SPQ Cognitive-Perceptual syndrome (β = 0.23, p < 0.05), SPQ Disorganized (β = 0.26, p < 0.05), and SPQ total (β = 0.25, p < 0.01) scores among users but not controls (all βs n.s.).
3.4. Correlations between personality measures and cannabis use
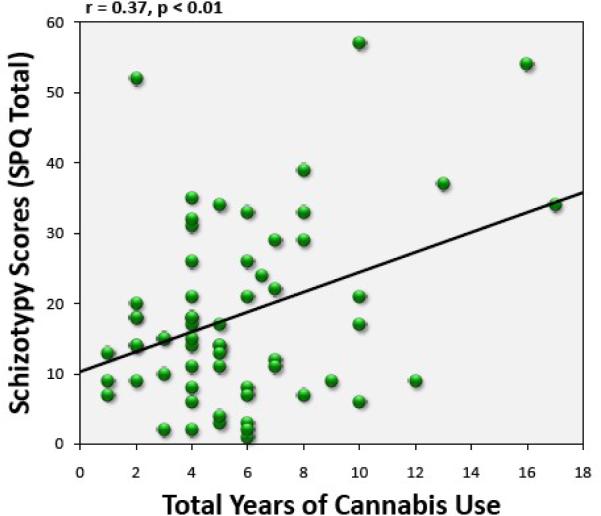
We calculated Pearson correlations between cannabis/alcohol use variables (age of first cannabis use, total years of use, and frequency of use during the previous month, average number of alcoholic drinks per week) and personality scores (NEO-FFI dimension, SPQ factor, and PAS) for the cannabis-using group. Total years of cannabis use correlated significantly with SPQ total score (r = 0.37, p < 0.01, see Figure 2), SPQ Cognitive-Perceptual (r = 0.34, p < 0.01) and SPQ Disorganized (r = 0.36, p < 0.01) factor scores, and PAS total score (r = 0.30, p < 0.05). There was a trend toward correlations between total years of use and SPQ Interpersonal syndrome schizotypy (r = 0.24, p = 0.06) and between total years of use and Neuroticism (r = 0.22, p = 0.08). Age of first cannabis use, frequency of cannabis use during the previous month, and average number of alcoholic drinks consumed per week did not correlate significantly with any personality measure (all coefficients ≤ 0.22, all p values n.s.).
Figure 2.
Total years of cannabis use (x-axis) versus total SPQ score (y-axis) for the cannabis group.
4. Discussion
Our results indicate that chronic cannabis users differ from cannabis-naive controls on measures of normal personality and schizotypy. On the NEO-FFI, cannabis users reported higher Openness, lower Agreeableness and Conscientiousness, and equivalent Neuroticism and Extraversion relative to controls, consistent with previous studies of personality and cannabis use (Flory, et al., 2002; Terracciano, et al., 2008). Users' scores on the NEO-FFI suggest that these individuals are non-conformists who prefer novel experiences (high Openness), but may be somewhat impulsive (low Conscientiousness) and uncooperative or suspicious of others as well (low Agreeableness) (Costa and McCrae, 1992b; McCrae and John, 1992; Flory, et al., 2002). A tendency to be open to new experiences may lead people to try cannabis (Grossman et al., 1974). Low Agreeableness and Conscientiousness characterize chronic users of other drugs as well (Trull and Sher, 1994; McCormick et al., 1998; Reno, 2004; Walton and Roberts, 2004), and low levels of these traits may predispose individuals to abuse substances or may account for some problems commonly associated with frequent drug use, such as impulsivity and problems with interpersonal relationships (Ball, 2005). Importantly, cannabis users in the present study did not differ from controls in terms of their scores on the Neuroticism or Extraversion dimensions. High Neuroticism is associated with a tendency toward negative affect and psychological distress (Costa and McCrae, 1992b; McCrae and John, 1992), and individuals suffering from mood or anxiety disorders (Trull and Sher, 1994) or substance use disorders (Trull and Sher, 1994; Fisher et al., 1998; McCormick, et al., 1998; Walton and Roberts, 2004) are elevated on this trait. However, our results suggest that “pure” chronic cannabis users who do not suffer from mood, anxiety, or non-cannabis substance use disorders are not elevated on this dimension. These results are consistent with those of a recent meta-analytic study of cannabis use and mental health outcomes which reported that evidence linking cannabis use to increased risk for affective or anxiety disorders is generally weak, and may reflect confounding factors, such as the presence of symptoms at baseline (Moore et al., 2007).
Chronic cannabis-using participants in the present study scored higher than controls on the PAS and Cognitive-Perceptual and Disorganized factors of the SPQ, in line with previous reports of a relation between cannabis use and increased psychosis-proneness (Mass, et al., 2001; Skosnik, et al., 2001; Dumas, et al., 2002; Verdoux, et al., 2002; Bailey and Swallow, 2004; Earleywine, 2006; Barkus and Lewis, 2008; Skosnik, et al., 2008; Compton, et al., 2009a; Esterberg, et al., 2009). Chronic cannabis users in the present study endorsed more symptoms of positive (e.g., perceptual disturbances, paranoia) and disorganized (e.g., odd behavior) schizotypy than did controls. Elevated schizotypy and cannabis use are associated with increased risk for psychosis (Chapman et al., 1994; Moore, et al., 2007). We found no significant differences between users and controls on the Interpersonal (i.e., negative symptom) schizotypy dimension, in contrast to previous reports (Mass, et al., 2001; Bailey and Swallow, 2004; Skosnik, et al., 2008). Since social interactions and relationships with others are the main emphases of the interpersonal deficits factor of the SPQ, this result is congruent with the lack of difference between users' and controls' scores on NEO-FFI Extraversion. An “amotivational syndrome”, which includes social withdrawal, has been identified as a potential negative consequence of chronic cannabis use (Sewell et al., 2009). However, previous research has failed to support an association between chronic use of this drug and impaired motivation (Comitas, 1976; Barnwell et al., 2006), and motivational deficits in cannabis users may be a consequence of other factors, such as depression (Kupfer et al., 1973; Musty and Kaback, 1995). Our data suggest that social withdrawal is not a trait-like characteristic of chronic cannabis users who do not meet criteria for a current or past mood disturbance.
Higher Neuroticism predicted greater schizotypy among both groups in the present study, which is consistent with previous reports linking the tendency to experience negative affect with increased risk for psychosis (Van Os and Jones, 2001; Krabbendam et al., 2002). Openness also significantly predicted disorganized-syndrome schizotypy among both groups. This is unsurprising given that individuals high in Openness have been described as “unconventional” (McCrae and John, 1992; Gurrera, et al., 2005), and the disorganized-syndrome factor of the SPQ consists of items sensitive to odd or idiosyncratic behavior and speech (Raine, 1991). In addition, Extraversion significantly predicted interpersonal deficits (i.e., negative-syndrome schizotypy) among members of the cannabis-using group. Higher Extraversion was associated with lower SPQ Interpersonal factor scores within that group, which is consistent with previous research in non-psychiatric samples (Dyce and O'Connor, 1998; Ross, et al., 2002; Camisa, et al., 2005). Psychosis-prone individuals who are more extraverted may tend to seek out and participate in social networks, which may lead to better overall functioning and reduced likelihood of psychosis (e.g., Van Os and Jones, 2001;Camisa, et al., 2005). Indeed, social withdrawal is a prodromal sign of schizophrenia (Lieberman et al., 2001; Miller et al., 2002). In addition, the regression analysis indicated that age positively predicted SPQ Cognitive-Perceptual and Disorganized factor scores and SPQ total score among users but not controls as well. While this appears to contradict the results of a recent study which reported a negative correlation between schizotypy scores and age in a non-clinical sample (Mata et al., 2005), age was highly correlated with years of use (r = 0.79, p < 0.001) among users in the present study. Thus, the relations between age and schizotypy indicated in Table 3 may reflect the contribution of cumulative years of use to schizotypy scores, rather than the effects of age per se. Collectively, the present results suggest that older cannabis users who are high in Neuroticism and Openness, but low in Extraversion, may be at greatest risk for psychosis, although the cross-sectional design of the present study prevented us from testing that possibility directly.
The present data should be interpreted in light of some potential caveats. First, the cross-sectional design of our study precludes us from inferring any causal relations between participants' cannabis use and their scores on the personality measures. Although there is strong evidence implicating cannabis use as a risk factor for the development of psychosis (Moore, et al., 2007), this association may be influenced by additional factors, such as genetic risk for psychosis. Second, participants were self-referred for the study which may have introduced a selection bias into our sample. For instance, cannabis users high in negative-syndrome schizotypy may be socially withdrawn and may not wish to participate in a research study. The status of cannabis as an illegal substance may have discouraged potential participants as well, especially those who tend to be suspicious or distrustful of others. Third, our cannabis-using sample reported minimal use of other drugs and did not meet abuse/dependence criteria for any other substance. Polysubstance use is common among cannabis users (Gledhill-Hoyt et al., 2000), so participants in our sample may not reflect the “typical” cannabis user. Lastly, participants in the present study were relatively young and well-educated, and it is unclear whether the present results would generalize to older, less educated samples.
The present study provides further support for an association between chronic cannabis use and greater self-reported schizotypy. Users exhibited elevated positive- and disorganized-syndrome schizotypy relative to controls, and we found a positive correlation between years of cannabis use and those symptom dimensions. Our data also suggest that chronic users differ from non-users in terms of normal personality dimensions. Users exhibited higher Openness, but lower Agreeableness and Conscientiousness, relative to controls. Importantly, cannabis users in the present study did not show elevated Neuroticism relative to controls, suggesting that chronic cannabis use is not associated with a tendency to experience negative affect, as has been observed previously among chronic users of other substances (Trull and Sher, 1994; Fisher, et al., 1998; McCormick, et al., 1998; Walton and Roberts, 2004). While chronic cannabis use has been associated with the development of psychosis (Moore, et al., 2007), the psychobiological mechanisms behind this relation are unclear. Our data indicate that individual differences in the Neuroticism, Extraversion, and Openness to experience dimensions specified by the FFM predict schizotypy scores among cannabis users. Thus, individual variation in normal personality may be related to differences in psychosis-proneness among chronic users.
Acknowledgements
This work was supported in part by grants from NIDA (1 R03 DA019630-01; 1 R21 DA023097-01A1) and a NARSAD Young Investigator Award (PDS). We wish to thank William Hetrick, Peter Finn, Chad Edwards, and Adam Steinmetz for their help throughout the project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- APA . Diagnostic and Statistical Manual of Mental Disorders. 4th, Text Revision ed. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Bagby RM, Marshall MB, Georgiades S. Dimensional personality traits and the prediction of DSM-IV personality disorder symptom counts in a nonclinical sample. Journal of Personality Disorders. 2005;19:53–67. doi: 10.1521/pedi.19.1.53.62180. [DOI] [PubMed] [Google Scholar]
- Bailey EL, Swallow BL. The relationship between cannabis use and schizotypal symptoms. European Psychiatry. 2004;19:113–114. doi: 10.1016/j.eurpsy.2003.12.001. [DOI] [PubMed] [Google Scholar]
- Ball SA. Personality traits, problems, and disorders: Clinical applications to substance use disorders. Journal of Research in Personality. 2005;39:84–102. [Google Scholar]
- Barkus E, Lewis S. Schizotypy and psychosis-like experiences from recreational cannabis in a non-clinical sample. Psychological Medicine. 2008;38:1267–1276. doi: 10.1017/S0033291707002619. [DOI] [PubMed] [Google Scholar]
- Barnwell S, Earleywine M, Wilcox R. Cannabis, motivation, and life satisfaction in an internet sample. Substance Abuse Treatment, Prevention, and Policy. 2006;1:2. doi: 10.1186/1747-597X-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camisa KM, Bockbrader MA, Lysaker P, Rae LL, Brenner CA, O'Donnell BF. Personality traits in schizophrenia and related personality disorders. Psychiatry Research. 2005;133:23–33. doi: 10.1016/j.psychres.2004.09.002. [DOI] [PubMed] [Google Scholar]
- Chapman LJ, Chapman JP, Kwapil TR, Eckblad M, Zinser MC. Putatively psychosis-prone subjects 10 years later. Journal of Abnormal Psychology. 1994;103:171–183. doi: 10.1037//0021-843x.103.2.171. [DOI] [PubMed] [Google Scholar]
- Chapman LJ, Chapman JP, Raulin ML. Scales for physical and social anhedonia. Journal of Abnormal Psychology. 1976;85:374–382. doi: 10.1037//0021-843x.85.4.374. [DOI] [PubMed] [Google Scholar]
- Chapman LJ, Chapman JP, Raulin ML. Body-Image Aberration in Schizophrenia. Journal of Abnormal Psychology. 1978;87:399–407. doi: 10.1037//0021-843x.87.4.399. [DOI] [PubMed] [Google Scholar]
- Comitas L. Cannabis and work in Jamaica: A refutation of the amotivational syndrome. Annals of the New York Academy of Sciences. 1976;282:24–32. doi: 10.1111/j.1749-6632.1976.tb49881.x. [DOI] [PubMed] [Google Scholar]
- Compton MT, Chien VH, Bollini AM. Associations between past alcohol, cannabis, and cocaine use and current schizotypy among first-degree relatives of patients with schizophrenia and non-psychiatric controls. Psychiatric Quarterly. 2009a;80 doi: 10.1007/s11126-009-9102-x. [DOI] [PubMed] [Google Scholar]
- Compton MT, Goulding SM, Bakeman R, McClure-Tone EB. Confirmation of a four-factor structure of the Schizotypal Personality Questionnaire among undergraduate students. Schizophrenia Research. 2009b;111:46–52. doi: 10.1016/j.schres.2009.02.012. doi: DOI: 10.1016/j.schres.2009.02.012. [DOI] [PubMed] [Google Scholar]
- Compton MT, Goulding SM, Walker EF. Cannabis Use, first-episode psychosis, and schizotypy: A summary and synthesis of recent literature. Current Psychiatry Reviews. 2007;3:161–171. [Google Scholar]
- Coolidge FL, Becker LA, DiRito DC, Durham RL, Kinlaw MM, Philbrick PB. On the relationship of the five-factor personality model to personality disorders: Four reservations. Psychological Reports. 1994;75:11–21. doi: 10.2466/pr0.1994.75.1.11. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Personality disorders and the five-factor model of personality. Journal of Personality Disorders. 1990;4:362–371. [Google Scholar]
- Costa PT, McCrae RR. Normal personality assessment in clinical practice: The NEO Personality Inventory. Psychological Assessment. 1992a;4:5–13. [Google Scholar]
- Costa PT, McCrae RR. Revised NEO personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Psychological Assessment Resources; Odessa, FL: 1992b. [Google Scholar]
- Digman JM. Personality Structure: Emergence of the Five-Factor Model. Annual Review of Psychology. 1990;41:417–440. [Google Scholar]
- Dumas P, Saoud M, Bouafia S, Gutknecht C, Ecochard R, Daléry J, Rochet T, d'Amato T. Cannabis use correlates with schizotypal personality traits in healthy students. Psychiatry Research. 2002;109:27–35. doi: 10.1016/s0165-1781(01)00358-4. [DOI] [PubMed] [Google Scholar]
- Dyce JA, O'Connor BP. Personality disorders and the five-factor model: a test of facet-level predictions. Journal of Personality Disorders. 1998;12:31–45. doi: 10.1521/pedi.1998.12.1.31. [DOI] [PubMed] [Google Scholar]
- Earleywine M. Schizotypy, marijuana, and differential item functioning. Human Psychopharmacology: Clinical and Experimental. 2006;21:455–461. doi: 10.1002/hup.802. [DOI] [PubMed] [Google Scholar]
- Esterberg ML, Goulding SM, McClure-Tone EB, Compton MT. Schizotypy and nicotine, alcohol, and cannabis use in a non-psychiatric sample. Addictive Behaviors. 2009;34:374–379. doi: 10.1016/j.addbeh.2008.11.007. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) American Psychiatric Press, Inc.; Washington, DC: 1997. [Google Scholar]
- First MB, Spitzer RL, Miriam G, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/ PSY SCREEN) Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Fisher LA, Elias JW, Ritz K. Predicting relapse to substance abuse as a function of personality dimensions. Alcoholism: Clinical and Experimental Research. 1998;22:1041–1047. doi: 10.1111/j.1530-0277.1998.tb03696.x. [DOI] [PubMed] [Google Scholar]
- Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. The relations among personality, symptoms of alcohol and marijuana abuse, and symptoms of comorbid psychopathology: Results from a community sample. Experimental and Clinical Psychopharmacology. 2002;10:425–434. doi: 10.1037//1064-1297.10.4.425. [DOI] [PubMed] [Google Scholar]
- Gledhill-Hoyt J, Lee H, Strote J, Wechsler H. Increased use of marijuana and other illicit drugs at US colleges in the 1990s: results of three national surveys. Addiction. 2000;95:1655–1667. doi: 10.1046/j.1360-0443.2000.951116556.x. [DOI] [PubMed] [Google Scholar]
- Grossman JC, Goldstein R, Eisenman R. Undergraduate marijuana and drug use as related to openness to experience. Psychiatric Quarterly. 1974;48:86–92. doi: 10.1007/BF01574313. [DOI] [PubMed] [Google Scholar]
- Gurrera RJ, Dickey CC, Niznikiewicz MA, Voglmaier MM, Shenton ME, McCarley RW. The five-factor model in schizotypal personality disorder. Schizophrenia Research. 2005;80:243–251. doi: 10.1016/j.schres.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krabbendam L, Janssen I, Bak M, Bijl RV, de Graaf R, van Os J. Neuroticism and low self-esteem as risk factors for psychosis. Social Psychiatry & Psychiatric Epidemiology. 2002;37:1. doi: 10.1007/s127-002-8207-y. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Detre T, Koral J, Fajans P. A comment on the “amotivational syndrome” in marijuana smokers. Am J Psychiatry. 1973;130:1319–1322. doi: 10.1176/ajp.130.12.1319. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Perkins D, Belger A, Chakos M, Jarskog F, Boteva K, Gilmore J. The early stages of schizophrenia: Speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biological Psychiatry. 2001;50:884–897. doi: 10.1016/s0006-3223(01)01303-8. [DOI] [PubMed] [Google Scholar]
- Malouff JM, Thorsteinsson EB, Schutte NS. The relationship between the five-factor model of personality and symptoms of clinical disorders: A meta-analysis. Journal of Psychopathology and Behavioral Assessment. 2005;27:101–114. [Google Scholar]
- Mass R, Bardong C, Kindl K, Dahme B. Relationship between Cannabis Use, Schizotypal Traits, and Cognitive Function in Healthy Subjects. Psychopathology. 2001;34:209–214. doi: 10.1159/000049309. [DOI] [PubMed] [Google Scholar]
- Mata I, Mataix-Cols D, Peralta V. Schizotypal Personality Questionnaire-Brief: Factor structure and influence of sex and age in a nonclinical population. Personality and Individual Differences. 2005;38:1183–1192. [Google Scholar]
- McCormick RA, Dowd ET, Quirk S, Zegarra JH. The relationship of NEO-PI performance to coping styles, patterns of use, and triggers for use among substance abusers. Addictive Behaviors. 1998;23:497–507. doi: 10.1016/s0306-4603(98)00005-7. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT. Validation of the five-factor model of personality across instruments and observers. Journal of Personality and Social Psychology. 1987;52:81–90. doi: 10.1037//0022-3514.52.1.81. [DOI] [PubMed] [Google Scholar]
- McCrae RR, John OP. An Introduction to the Five-Factor Model and its Applications. Journal of Personality. 1992;60:175–215. doi: 10.1111/j.1467-6494.1992.tb00970.x. [DOI] [PubMed] [Google Scholar]
- Miller P, Byrne M, Hodges A, Lawrie SM, Owens DG, Johnstone EC. Schizotypal components in people at high risk of developing schizophrenia: Early findings from the Edinburgh High-Risk Study. British Journal of Psychiatry. 2002;180:179–184. doi: 10.1192/bjp.180.2.179. [DOI] [PubMed] [Google Scholar]
- Moore THM, Zammit S, Lingford-Hughes A, Barnes TRE, Jones PB, Burke M, Lewis G. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. The Lancet. 2007;370:319–328. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- Mullins-Sweatt SN, Jamerson JE, Samuel DB, Olson DR, Widiger TA. Psychometric Properties of an Abbreviated Instrument of the Five-Factor Model. Assessment. 2006;13:119–137. doi: 10.1177/1073191106286748. [DOI] [PubMed] [Google Scholar]
- Murray G, Rawlings D, Allen NB, Trinder J. NEO Five-Factor Inventory Scores: Psychometric Properties in a Community Sample. Measurement & Evaluation in Counseling & Development. 2003;36:140–149. [Google Scholar]
- Musty RE, Kaback L. Relationships between motivation and depression in chronic marijuana users. Life Sciences. 1995;56:2151–2158. doi: 10.1016/0024-3205(95)00202-h. [DOI] [PubMed] [Google Scholar]
- Noguchi H, Hori H, Kunugi H. Schizotypal traits and cognitive function in healthy adults. Psychiatry Research. 2008;161:162–169. doi: 10.1016/j.psychres.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Raine A. The SPQ: A Scale for the Assessment of Schizotypal Personality Based on DSM-III-R Criteria. Schizophr Bull. 1991;17:555–564. doi: 10.1093/schbul/17.4.555. [DOI] [PubMed] [Google Scholar]
- Raine A. Schizotypal Personality: Neurodevelopmental and Psychosocial Trajectories. Annual Review of Clinical Psychology. 2006;2:291–326. doi: 10.1146/annurev.clinpsy.2.022305.095318. [DOI] [PubMed] [Google Scholar]
- Raine A, Reynolds C, Lencz T, Scerbo A, Triphon N, Kim D. Cognitive-perceptual, Interpersonal, and Disorganized Features of Schizotypal Personality. Schizophr Bull. 1994;20:191–201. doi: 10.1093/schbul/20.1.191. [DOI] [PubMed] [Google Scholar]
- Reno RM. Personality Characterizations of Outpatients With Schizophrenia, Schizophrenia With Substance Abuse, and Primary Substance Abuse. The Journal of Nervous and Mental Disease. 2004;192:672–681. doi: 10.1097/01.nmd.0000142030.44203.63. [DOI] [PubMed] [Google Scholar]
- Ross SR, Lutz CJ, Bailley SE. Positive and negative symptoms of schizotypy and the five-factor model: A domain and facet level analysis. Journal of Personality Assessment. 2002;79:53–72. doi: 10.1207/S15327752JPA7901_04. [DOI] [PubMed] [Google Scholar]
- SAMHSA . Results from the 2006 National Survey on Drug Use and Health: National findings (No. SMA 07-4293) Rockville, MD: 2007. [Google Scholar]
- Samuel DB, Widiger TA. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: A facet level analysis. Clinical Psychology Review. 2008;28:1326–1342. doi: 10.1016/j.cpr.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saulsman LM, Page AC. The five-factor model and personality disorder empirical literature: A meta-analytic review. Clinical Psychology Review. 2004;23:1055–1085. doi: 10.1016/j.cpr.2002.09.001. [DOI] [PubMed] [Google Scholar]
- Sewell RA, Ranganathan M, D'Souza DC. Cannabinoids and psychosis. International Review of Psychiatry. 2009;21:152–162. doi: 10.1080/09540260902782802. [DOI] [PubMed] [Google Scholar]
- Skosnik PD, Krishnan GP, Aydt EE, Kuhlenshmidt HA, O'Donnell BF. Psychophysiological Evidence of Altered Neural Synchronization in Cannabis Use: Relationship to Schizotypy. Am J Psychiatry. 2006;163:1798–1805. doi: 10.1176/ajp.2006.163.10.1798. [DOI] [PubMed] [Google Scholar]
- Skosnik PD, Park S, Dobbs L, Gardner WL. Affect processing and positive syndrome schizotypy in cannabis users. Psychiatry Research. 2008;157:279–282. doi: 10.1016/j.psychres.2007.02.010. [DOI] [PubMed] [Google Scholar]
- Skosnik PD, Spatz-Glenn L, Park S. Cannabis use is associated with schizotypy and attentional disinhibition. Schizophrenia Research. 2001;48:83–92. doi: 10.1016/s0920-9964(00)00132-8. [DOI] [PubMed] [Google Scholar]
- Stefanis NC, Smyrnis N, Avramopoulos D, Evdokimidis l., Ntzoufras l., Stefanis CN. Factorial Composition of Self-Rated Schizotypal Traits Among Young Males Undergoing Military Training. Schizophrenia Bulletin. 2004;30:335–350. doi: 10.1093/oxfordjournals.schbul.a007083. [DOI] [PubMed] [Google Scholar]
- Terracciano A, Lockenhoff C, Crum R, Bienvenu OJ, Costa PT. Five-Factor Model personality profiles of drug users. BMC Psychiatry. 2008;8:22. doi: 10.1186/1471-244X-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Sher KJ. Relationship between the five-factor model of personality and Axis I disorders in a nonclinical sample. Journal of Abnormal Psychology. 1994;103:350–360. doi: 10.1037//0021-843x.103.2.350. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Widiger TA, Burr R. A structured interview for the assessment of the Five-factor Model of personality: Facet-level relations to the Axis II personality disorders. Journal of Personality. 2001;69:175–198. doi: 10.1111/1467-6494.00141. [DOI] [PubMed] [Google Scholar]
- Van Os J, Jones PB. Neuroticism as a risk factor for schizophrenia. Psychological Medicine. 2001;31:1129–1134. doi: 10.1017/s0033291701004044. [DOI] [PubMed] [Google Scholar]
- Verdoux H, Sorbara F, Gindre C, Swendsen JD, van Os J. Cannabis use and dimensions of psychosis in a nonclinical population of female subjects. Schizophrenia Research. 2002;59:77–84. doi: 10.1016/s0920-9964(01)00401-7. [DOI] [PubMed] [Google Scholar]
- Walton KE, Roberts BW. On the relationship between substance use and personality traits: Abstainers are not maladjusted. Journal of Research in Personality. 2004;38:515–535. [Google Scholar]
- Wechsler D. WAIS-III administration and scoring manual. Psychological Corporation; San Antonio, TX: 1997. [Google Scholar]