Abstract
No single HIV prevention strategy will be sufficient to control the HIV pandemic. However, a growing number of interventions have shown promise in partially protecting against HIV transmission and acquisition, including knowledge of HIV serostatus, behavioral risk reduction, condoms, male circumcision, needle exchange, treatment of curable sexually transmitted infections, and use of systemic and topical antiretroviral medications by both HIV-infected and uninfected persons. Designing the optimal package of interventions that matches the epidemiologic profile of a target population, delivering that package at the population level, and evaluating safety, acceptability, coverage, and effectiveness, all involve methodological challenges. Nonetheless, there is an unprecedented opportunity to develop “prevention packages” that combine various arrays of evidence-based strategies, tailored to the needs of diverse subgroups and targeted to achieve high coverage for a measurable reduction in population-level HIV transmission. HIV prevention strategies that combine partially effective interventions should be scaled up and evaluated.
Keywords: Combination HIV prevention, HIV prevention methods, HIV prevention packages, Antiretroviral therapy, Test and treat
Introduction
Thirty years into the global HIV pandemic, there is a critical need for effective prevention strategies that can be implemented with high levels of coverage in populations with high incidence of new infections. Worldwide, nearly 3 million new HIV infections were estimated to have occurred in 2008 [1]. No single, stand-alone HIV prevention intervention offers a “magic bullet.” It is unlikely that a single deployed intervention, even a vaccine [2], will halt the pandemic. However, a growing number of behavioral [3–8] and biomedical [9–16] HIV prevention strategies appear promising in providing some protection against infection, and the efficacy of several is supported by randomized controlled trials (RCTs) [17]. Indeed, combining several partially protective strategies might have additive or synergistic effects in reducing HIV incidence on a population level. Analogous to the need for combination antiretroviral therapy (ART) for treatment, there is growing recognition that combination HIV prevention strategies might optimize HIV prevention impact [18••], potentially enough to reduce transmission below the reproductive rate necessary to sustain HIV epidemics around the globe [19].
UNAIDS (2010) provides the following definition of combination HIV prevention:
“The strategic, simultaneous use of different classes of prevention activities (biomedical, behavioral, social/structural) that operate on multiple levels (individual, relationship, community, societal), to respond to the specific needs of particular audiences and modes of HIV transmission, and to make efficient use of resources through prioritizing, partnership, and engagement of affected communities” [20].
Multicomponent packages of evidence-based biomedical, behavioral, and structural interventions must be assembled to be appropriate, acceptable, and deliverable to populations with high levels of coverage and adherence. These prevention packages must address risk factors at the individual, dyadic, sexual or needle sharing network, and community levels, while taking into account the epidemiologic context (Table 1). Determining what constitutes a sufficient level of evidence for inclusion in any given combination package is a critical step. Levels of intervention efficacy (often demonstrated in single studies in only one subpopulation or setting) vary. Since some HIV prevention interventions cannot pragmatically or ethically be randomized, decisions about evidence may need to be drawn from quasi-experimental and programmatic data, in addition to RCTs. Methodologic challenges include deciding what level of experimental or observational evidence is sufficient to warrant inclusion of an intervention in a prevention “package.” Guidelines developed by the US Preventive Services Task Force, the Centers for Disease Control and Prevention, and others often include ratings of the strength of evidence to address this dilemma (see http://www.ahrq.gov/clinic/uspstf07/ratingsv2.htm). However, it is important to anticipate and recognize that interventions found to be efficacious in one setting may not readily transfer and may require cultural adaptation. Standardized approaches for translating interventions have been developed including the ADAPT-ITT [21] and RE-AIM models [22], among others.
Table 1.
HIV risk target levels to consider for combination HIV prevention packages
| Individual | Dyad/network | ||
Host factors
|
|
||
Sexual behaviors
|
|||
Substance use behaviors
|
Structural | ||
HIV serostatus knowledge
|
Economic
|
||
Epidemiologic context
|
Legal
|
||
Public health & health care infrastructure
|
|||
 | |||
ART antiretroviral therapy; STI sexually transmitted infection
(Adapted from Kurth and Spielberg [73])
To our knowledge, no major multicomponent package of interventions has been launched in a full-scale, community-level randomized trial to assess impact on HIV seroincidence. The challenges inherent in assembling the optimal HIV prevention package, scaling it up for delivery, and empirically assessing the combined, rather than single-intervention effect are considerable. Recognizing this, in 2009, the National Institutes of Health (NIH) launched a research initiative called the Methods of Prevention Package Program (MP3) to fund combination HIV prevention studies. The purpose of these grants is to devise optimal HIV prevention packages for specific populations, and to design evaluation strategies to rigorously examine the acceptability, safety, and efficacy of those packages. The research teams for these studies have brought together multidisciplinary collaborators with expertise in behavioral and biomedical methods of HIV prevention, epidemiology, mathematical modeling, and clinical trial design and implementation [23]. The resulting MP3 grants illustrate a range of potential prevention approaches that may be required for heterogeneous HIV epidemics in different geographic regions and populations (Table 2). A second round of awards focused on populations other than those targeted in the first MP3 studies will begin in 2011. Previously completed and ongoing clinical trials of novel HIV prevention strategies, such as those conducted by the NIH’s HIV Prevention Trials Network (HPTN), the Microbicide Trials Network (MTN), the HIV Vaccine Trials Network (HVTN), the Medical Research Council Clinical Trials Network (MRC), and other organizations, have tended to focus on testing single interventions. Such RCTs provide a critical foundation for the development and rigorous evaluation of evidence-based combination prevention packages.
Table 2.
First round of NIH-funded combination HIV prevention studies
| Principal investigator | Study population | Setting | Package elements |
|---|---|---|---|
| Susan Buchbinder (San Francisco Department of Health) |
Men who have sex with men | North and South America | Potentially PrEP, VCT/disclosure/serosorting, addressing adherence, substance use, and risk compensation |
| Connie Celum (University of Washington) |
Rural heterosexual populations, including discordant couples | Uganda | Home-based HIV testing and targeted prevention referrals for MMC, ART, STI treatment, couples counseling, and topical and systemic PrEP (if efficacious) (PreventionRx) |
| Don Des Jarlais (Beth Israel Medical Center) |
Injection drug users | Estonia | Likely syringe exchange, pharmacy sales, methadone, STI screening/treatment, PrEP (if efficacious) |
| Wafaa El-Sadr (Columbia University) |
HIV-discordant heterosexual couples | Lesotho | Behavioral counseling, ART for prevention (CD4<500) plus couples counseling, MMC |
| Max Essex and Victor deGruttola (Harvard University) |
All reproductive-age persons in a single village | Botswana | Behavioral interventions: VCT, partner notification, concurrency reduction, MMC, condoms, and ART for those with high viral load |
| William Miller and Audrey Pettifor (UNC Chapel Hill) |
Persons with acute HIV infection | Malawi | Standard vs enhanced counseling vs behavioral intervention plus 12-week ART to reduce viral load |
ART antiretroviral therapy; MMC medical male circumcision; NIH National Institutes of Health; PrEP pre-exposure prophylaxis; STI sexually transmitted infection; VCT voluntary counseling and testing
A core tenet of the MP3 program is that understanding the patterns and risks for HIV transmission at a population level (be that national or local) guides the compilation of an optimal package of prevention interventions. This “know your epidemic” approach [24] involves understanding determinants of local HIV prevalence (and ideally incidence) to identify population targets with the highest rate of recent HIV infections, and to maximize the prevention benefits achieved. However, the need to know one’s epidemic should not be taken as an imperative that impedes action, when local epidemiologic data are not available at finest levels of completeness, granularity, or timeliness.
Combination ART reduces HIV replication by attacking the virus at multiple points of its life cycle, leading to multiple therapeutic targets for treatment, and yielding dramatic clinical benefits. Similarly, combination HIV prevention is likely to be most effective when different points in the “transmission cycle” are impeded [25], combining strategies to reduce infectiousness of HIV-positive persons with strategies that reduce HIV susceptibility in the uninfected. Most early HIV prevention policies focused heavily on HIV-negative, at-risk persons (eg, using behavior change communication campaigns). However, seronegative persons represent a very large pool to target for high coverage. In 30 years, only such nations as Uganda and Thailand have actually managed to reverse HIV epidemics using prevention strategies focused on HIV-seronegative persons [26]. Strategies to reduce the infectiousness of HIV-positive individuals by reducing secondary HIV transmission are now being assessed (eg, HPTN 052 and HPTN 065) [22]. Theoretically, if a high proportion of people living with HIV/AIDS (PLWHA) learned their HIV serostatus and adopted interventions such as ART to reduce their infectiousness coupled with behavioral risk reduction, this could have a significant impact on HIV transmission [27, 28••]. Optimizing HIV prevention for PLWHA in a community also targets significantly more people who may be motivated to seek care for their own health needs, than risk-reduction programs aimed at healthy, HIV-negative persons. Given the need to minimize both infectiousness (ART, condoms, STI treatment for positives) and susceptibility (multiple interventions for negatives), combination prevention incorporating complementary strategies aimed at both infected and uninfected persons offers the most promising way forward.
Designing Combination HIV Prevention Packages
Potential components of a combination HIV prevention package should focus on those interventions with demonstrated or promising potential efficacy to reduce HIV transmission (infectiousness) or acquisition (susceptibility), and will differ depending on target population, epidemiologic context [29], and varying levels of evidence (Table 3). Those with demonstrated efficacy—ie, impact on HIV incidence—include prevention of maternal-to-child transmission (PMTCT) and medical male circumcision (MMC). We do not include the recently partially effective vaccine [30], as the vaccine companies are not seeking licensure for marketing of either the prime or boost products. Three RCTs of HSV-2 acyclovir suppressive therapy did not demonstrate impact on HIV acquisition or transmission, while treatment of curable sexually transmitted infections (STIs) was effective in reducing HIV incidence in one out of six RCTs. This has led to recognition that the relative impact of STI treatment will depend on STI prevalence and stage of the respective HIV and STI epidemics [31]. Those interventions with promise—based on preliminary data, observational data, single RCTs, or plausibility based on phase 1 and animal studies—include male condoms, opioid substitution therapy for intravenous drug users, contraception to reduce unintended pregnancies, pre-exposure prophylaxis with antiretroviral therapy (PrEP), and topical ART-based microbicides.
Table 3.
Potential interventions for a combination HIV prevention package
| Intervention | May reduce infectiousness of HIV+ persons? (biologic and/or behavioral mechanisms) |
May reduce susceptibility of HIV− persons? (biologic and/or behavioral mechanisms) |
Epidemiologic context/ target population |
Evidence |
|---|---|---|---|---|
| Sexual transmission | ||||
| ART | Yes | – | HIV+ males and females | 1 RCT ongoing; observational studies in context of CD4<200 |
| Cash transfer | – | Yes | HIV− females | 1 positive RCT in Malawi, others underway |
| Condom use (male and female condoms) | Yes | Yes | HIV− and HIV+ males and females | Multiple observational studies (evidence less strong for female condom) |
| Male circumcision | Unclear | Yes | HIV− males in settings with | 3 positive RCTs; |
| generalized epidemics and low circumcision rates | >30 observational studies | |||
| Microbicides, topical | – | Yes | HIV− women and MSM | 6 non-antiretroviral–based microbicide RCTs have not shown efficacy |
| CAPRISA 004 RCT (1% tenofovir gel) showed positive results (39% overall HIV risk reduction, 54% among consistent user subset; HSV-2 51% risk reduction) | ||||
| PrEP | – | Yes | HIV−, high-risk men and women (eg, sex workers, MSM, HIV serodiscordant couples) | 5 efficacy RCTs ongoing |
| Testing/knowledge of serostatus | Yes | Possibly more for females than males, or for | HIV− and HIV+ males and females | Several meta-analyses of observational data show +s ↓ risk; 1 RCT ongoing; |
| couples | Generalized epidemic, at least one test; concentrated epidemic/risk groups, repeat testing | several RCTs show men may ↑ risk | ||
| Treatment of curable STIs | Yes | Yes | HIV− and HIV+ males and females | 1 positive and 5 flat RCTs |
| 1 RCT demonstrated efficacy in early-stage HIV epidemic setting | ||||
| Vaccine | – | Yes | – | Thai RCT shows possible prophylactic effect but may not be available/brought to market |
| Parenteral transmission | ||||
| Blood and tissue screening | Yes | – | All donors | Strong observational evidence |
| Needle exchange | Yes | Yes | IDUs | Strong observational evidence (published data fulfill 6/9 Bradford Hill criteria on causal inference) |
| Opioid agonist/substitution therapy | Yes (reduces IDU) | Yes | IDUs | Observational studies, systematic reviews, RCTs |
| Vertical transmission | ||||
| Effective contraception | Yes (prevents pregnancy) | – | HIV+ women | Observational evidence for reduction in unintended pregnancy rate |
| PMTCT (HIV screening and ART during ante/intra/postpartum and breastfeeding periods) | Yes | Yes (provided to infant, analogous to PrEP) | Pregnant women | Multiple RCTs |
ART antiretroviral therapy; IDU injecting drug use; MSM men who have sex with men; PMTCT prevention of mother-to-child transmission; PrEP pre-exposure prophylaxis; RCT randomized controlled trial; STI sexually transmitted infection
Reducing Infectiousness
Vertical HIV transmission has been shown in multiple trials of PMTCT interventions to be successfully reduced by 92% to 98%. Sexual and parenteral transmission risk reduction interventions supported by observational evidence include HIV testing, behavioral risk reduction including condom use, treatment of curable STIs, ART, and needle exchange. Additional possible interventions may focus on treatment of other co-infections [14]. This includes HSV-2, for which there are data regarding the magnitude of peripheral and genital viral load reduction that nonetheless have not been shown to translate to HIV transmission reduction. It may also include malaria and helminths for which observational data suggest potential impact in reducing plasma and genital HIV viral load. However, additional data and regimens that better target the underlying mechanisms that increase infectious are needed before these observations can be translated into components of an evidence-based prevention package. Below we summarize the primary target population, supporting evidence, and key considerations with regard to feasibility, coverage, and adherence for several infectiousness-reducing interventions with the strongest evidence basis. We also discuss one example of a potential combination prevention package that has recently received considerable attention.
HIV Testing
Expanding access to HIV serostatus knowledge is an urgent global priority, both to link HIV-infected persons who are unaware of their status to life-saving clinical care and to prevent new infections, given evidence that most individuals testing positive reduce their sexual and other secondary HIV transmission risk behaviors [13, 32]. This is especially the case for sub-Saharan Africa, where two thirds of those with HIV live, but where only 10% to 20% of African adults have been tested for HIV [33]. Thus, the majority of people with HIV are unaware of their status, and even fewer know the status of their partners. Lack of knowledge of one’s own and one’s partner’s serostatus is associated with a 50% to 66% decreased likelihood of condom use [34]. HIV testing includes provider-initiated, routine or opt-out testing (recommended for countries with generalized HIV epidemics), and voluntary, home-based HIV counseling and testing, which may be cost effective [35] for population-level scale-up, especially to increase testing in men and to identify HIV-discordant couples. The impact of expanded community-based testing on HIV seroincidence is being assessed in a four-country, 48-site community RCT (HPTN 043, Project Accept) that will be completed by 2012 [36].
While expanded access to HIV testing leads to behavior change for the majority of those testing positive, studies to date generally have found that testing has not resulted in reduced risk behaviors among those testing negative [37]. Effects of testing on risk behavior may differ among men and women: less risk reduction, or even increased risk behaviors, have been noted among US men who tested HIV-negative in the RESPECT 2 trial, as well as in studies in Zimbabwe and Kenya [38–40]. Whether or not HIV testing itself reduces behavioral risk, it remains a critical entry point for combination prevention packages that aim to link HIV-positive persons to appropriate clinical and prevention services.
HIV Treatment
Learning that one is HIV-positive is a necessary precursor to obtaining HIV treatment, and thereby to reducing morbidity and mortality among PLWHA. However, many PLWHA delay initiation of treatment, even when clinically indicated, and others who start treatment do not always sustain ART (the “drop off cascade” noted in many low-income as well as higher-income settings). Nonetheless, initiation of ART treatment, as well as less expensive and highly effective opportunistic infection prophylaxis such as trimethoprim/sulfamethoxazole, has had a remarkable impact on deaths due to AIDS in high-burden settings [41].
Antiretrovirals reduce plasma HIV levels to undetectable levels in a preponderance of adherent patients. Mounting evidence from prospective studies of HIV-serodiscordant heterosexual couples suggests that ART markedly reduces HIV infectiousness [42, 43], in one study by a stunning 92% [44]. A meta-analysis of five observational studies found an overall risk of HIV heterosexual transmission from someone on ART of 0.46 per 100 person-years [45]. Ecological observations that reported HIV cases have declined contiguous with the expansion of ART in British Columbia and San Francisco also are very encouraging [46, 47].
While not the definitive word on “ART as prevention,” these observational data from multiple studies are compelling. However, it is worth emphasizing that observational studies have documented low rates of ongoing transmission after ART initiation, suggesting that risk is not completely eliminated by ART, either because of persistent production of virus in the genital tract despite ART or because of poor ART adherence [48]. An ongoing randomized trial (HPTN 052) is evaluating the long-term effects of ART on HIV transmission risk in 1500 discordant heterosexual couples in which the infected partner has a 350 to 550 cells/µL CD4 + cell count and is not yet eligible for ART. Results are expected in 2014. The impact of ART on HIV transmission among men who have sex with men (MSM) remains to be rigorously evaluated.
Longitudinal adherence to ART can be achieved but requires investment in evidence-based approaches [49, 50] to support persons staying on medication over long periods of time. Early rollout of ART in low-income countries focused on treatment initiation and must now provide ongoing adherence support to optimize first-line regimens and reduce development of resistance. This will be particularly true if programs shift to earlier initiation of ART for asymptomatic, HIV-infected persons at higher CD4 count levels to reduce transmission and not just for individual health benefits. The World Health Organization (WHO) now recommends initiation of ART at 350 CD4 cells/µL for all HIV-positive patients regardless of symptoms, and for all pregnant women regardless of CD4 count, with prolonged use of ART while breastfeeding to reduce vertical HIV transmission risk [51]. While this may be difficult to achieve given that many low-income countries have not yet provided ART even to those with CD4<200 cells/µL, widespread implementation of this policy might well have important transmission reduction as well as personal health benefits, if adherence were high and drug supplies steady.
Behavioral Risk Reduction
Behavioral interventions, including condom use, have been shown to reduce secondary HIV transmission risk behavior, although no RCTs have demonstrated impact on HIV incidence. Correct and consistent condom use has been shown to reduce both HIV and STI transmission probabilities in observational studies [52]. Prevention with positives counseling support for secondary HIV risk reduction has been shown in two meta-analyses to reduce unprotected sex among persons with HIV, particularly if motivational and skills components are included [53]. Successful interventions were based on behavioral theory; designed to change transmission behaviors; delivered in HIV care settings; and provided skill building and addressed mental health, adherence, and HIV risk behavior [54].
Treatment of Curable STIs
An additional strategy to reduce infectiousness may be curable STI co-infection treatment, as these co-infections increase genital and plasma HIV viral load. This may be particularly important in the pre-ART eligible population of PLWHA. This strategy will be most effective in those epidemiological settings that have subpopulations with a substantial burden of curable STIs.
Vertical Transmission Risk Reduction
Antiretrovirals have been shown to reduce antepartum, intrapartum [10], and postpartum (though breastfeeding [55]) HIV transmission. The challenge now is to deliver effective contraception (to reduce unwanted pregnancies), and HIV screening and ART to pregnant women at levels sufficient to reduce incidence. In settings where high coverage has been achieved, such as in Botswana, vertical transmission rates have been as low as those in high-income countries.
Parenteral Transmission Risk Reduction
Secondary transmission from injecting drug use (IDU) occurs both through sharing of needles and paraphernalia, and through unprotected sex. Effective interventions include opioid substitution therapy to reduce drug use [15], needle exchange programs to reduce blood exposure [56], and interventions to reduce risk behaviors [57]. Adherence to infectivity-reducing ART has been show to be similar among HIV-positive IDUs and non-IDUs [58].
Example of a Combination Prevention Package to Reduce Infectiousness: “Testing and Linkage to Care”
Knowledge of HIV serostatus must be linked to promising interventions such as behavioral risk reduction and ART, delivered with high coverage, and sustained with high adherence over time. For HIV-infected persons, this strategy has been called “test and treat” (when the intention is to go beyond current guidelines to treat virtually all seropositive persons) or “Test and Linkage to Care” or “TLC” (when seeking to improve coverage within existing guidelines). Interest in a “test and treat” approach was stimulated in large part by publication of a hypothetical modeling exercise by Granich et al. [28••] in 2009 that proposed that in a generalized epidemic, universal annual HIV testing and uptake of perfectly adhered to ART regardless of CD4 levels could reduce HIV prevalence to less than 1% within 50 years. The unrealistic assumptions of this mathematical model have been noted, given the challenges to date in getting HIV-positive persons to know their serostatus, and the leveling of funds for new treatment initiatives and ART slots in developing countries in the context of a global recession. Even a more realistic TLC strategy would be challenging. It would require the use of ART to reduce HIV transmission at higher CD4 counts, optimal mechanisms to greatly increase knowledge of HIV serostatus, willingness of HIV-positive persons to initiate ART at higher CD4 counts, improved adherence levels even when ART is used by asymptomatic persons, mechanisms to reduce drop-out from ART, and availability of resources to substantially augment ART supplies and systems for HIV prevention.
It is plausible that ART provision can be a highly effective HIV prevention strategy. However, other than the ecological data from British Columbia and San Francisco mentioned above, we do not have data at present to suggest that ART availability, itself, will curb the epidemic, and efforts to expand its potential benefit will depend on demonstrating that PLWHA can be identified and triaged to HIV care on a population scale. An ongoing trial (HPTN 065, “Test, Link to Care, Plus Treat”) will assess the feasibility of testing and linkage to care in the Bronx, NY and in Washington, DC relative to four comparison communities. This community-based study will examine innovative approaches to expanded HIV testing, randomized incentives for newly diagnosed PLWHA to enroll in appropriate care including ART, and use of surveillance data to monitor the average CD4 level at HIV diagnosis and community viral load [59]. It will provide important lessons that would then need to be applied at a broader scale in order to demonstrate actual efficacy of the testing and linkage to care concept to reducing HIV incidence and prevalence [59].
For every HIV-positive person started on ART in 2009, an estimated two to three new HIV infections occurred. Only approximately 40% [60] of HIV-infected persons in sub-Saharan Africa who require ART based on clinical guidelines are receiving it. Achieving increased coverage of ART in an era of tight economic resources, competing health priorities, and potential donor fatigue, remains a concern. A continued scenario of ever-larger numbers of persons testing positive being pushed into systems of care unable to accommodate even those who are clinically eligible for ART, underscores the challenges of TLC.
Reducing Susceptibility
To date, most HIV prevention strategies have targeted risk reduction in HIV-at-risk persons. Behavioral interventions have been shown to have an impact on STI incidence and on HIV-acquisition risk behaviors, although none have been shown to reduce HIV incidence. Meta-analyses indicate that behavioral interventions can be effective for HIV risk reduction among MSM, IDUs, youth, and women [61]. RCTs have demonstrated that male circumcision [11] and ART-containing microbicides [62••] are both proven HIV prevention tools in heterosexual populations, as is curable STI therapy under certain circumstances [17]. A partially effective preventive HIV-1 vaccine also appears promising [30]. Syringe and needle-exchange programs have been found to be not only efficacious, but cost-saving, in one study showing returns of $4 for every dollar invested [16]. Target populations, evidence, and operational issues specific to interventions focused on sexual transmission risk reduction are discussed below.
Medical Male Circumcision
In three randomized trials among heterosexual African males, MMC was consistently demonstrated to be highly efficacious for preventing HIV, with a pooled risk reduction of 56% [63], one of the most effective one-time interventions yet shown to reduce HIV acquisition risk for men. Effects of male circumcision on HIV risk for women are mixed (summary relative risk 0.80, 95% CI=0.53–1.36 in a random-effects meta-analysis) [64]. Large-scale implementation programs to maximize a population-level effect should achieve high coverage by targeting HIV-negative men based on younger age and possibly behavioral risks. While there are challenges to scaling up these services in an integrated fashion, the potential for a synergistic effect of combining MMC with other interventions such as HIV testing, condom promotion, and STI screening and treatment is highly significant.
Treatment of Curable STIs
Treatment of curable STIs to reduce HIV incidence has been evaluated in six randomized trials, of which one showed a substantial reduction in overall HIV incidence [65]. Another of the studies had a significant impact on HIV incidence only in a subgroup of males who attended program meetings [17].
ART-Containing Microbicides
The recently completed CAPRISA 004 trial was a double-blind, randomized, placebo-controlled trial to test the effectiveness and safety of 1% tenofovir gel among 889 HIV-uninfected women in two South African sites. The overall HIV incidence rate ratio was 0.61 (95% CI=0.40–0.96). In women who took at least 80% of the prescribed doses the protective effect was 54%, and in women who took less than 50% of the doses it was 28%. There was a trend toward decreasing effectiveness after 18 months, possibly due to a decline in adherence [16].
Behavioral Risk Reduction
There is some ecologic evidence of population-level effect of HIV risk reduction behavior change beyond meta-analyses of observational data showing the efficacy of behavioral interventions for specific most at-risk populations (MARPs). HIV prevalence data recently released by UNAIDS show that between 2000 and 2008 there was a 25% decline in HIV prevalence among young people aged 15 to 24 years in 10 countries. In eight of these countries, available behavioral data showed a decrease in risky behavior, suggesting that the decline in HIV prevalence was due to a widespread change in behavior [16].
Additional Strategies
Additional strategies being evaluated to reduce susceptibility include PrEP (covered by Golub et al. and Underhill et al. in this journal), topical microbicides other than the tenofovir-containing gel used daily (which will complement the pre and post-coital dosing of tenofovir gel in CAPRISA 004), and HIV vaccines. Structural interventions such as the World Bank evaluation of conditional cash transfer in Malawi that achieved a 60% reduction in HIV incidence and 75% reduction in HSV-2 incidence by paying the families of young girls to stay in school, are promising [66]. Depending on results in the coming years, these may well add to the menu of interventions to put into a combination prevention package.
Cross-cutting approaches to reduce infectiousness and susceptibility
Broader efforts to reduce HIV acquisition and transmission include structural-level efforts such as reducing gender inequalities and supporting income-generating activities for women, addressing HIV stigma, and changing laws that restrict access to efficacious preventive services such as needle exchange and drug treatment programs for IDUs. Structural interventions involving availability of clean syringes and needles have been particularly effective for IDUs [56].
Community engagement is necessary to address social norms, regulatory barriers, and potential distrust during the development and implementation of HIV prevention packages for vulnerable populations such as MSM or sex workers [67]. Implementing and evaluating structural interventions is difficult, which may explain why few such interventions have accumulated in the HIV prevention evidence base, despite calls for such approaches over a decade ago. Furthermore, knowledge of a national epidemic profile, and willingness or resourced ability to act on it, are not always in alignment [68]. However, structural interventions that facilitate healthy behaviors among the MARPs, such as sex workers, IDUs, and MSM, should be considered critical components of HIV combination prevention. Data from the Gates Foundation–funded Avahan trial in India will provide useful information on scaled-up, gender-specific HIV prevention packages that include structural components. Incidence impact will be modeled using antenatal HIV prevalence among 15 to 24-year-olds as a proxy measure.
Methodological Considerations in Combination HIV Prevention
Identifying effective interventions most suitable to specific MARPs requires looking at the strength of the evidence supporting each candidate intervention, tailoring the resulting intervention package to the specific MARP(s), estimating potential effect size and population attributable fraction, defining the expected causal pathway and relevant outcome measures, identifying possible synergies and antagonism among potential intervention package components with appropriate metrics, and addressing feasibility, scale-up, and evaluation of the combination package. Improved assays to ascertain HIV incidence would enable better tracking of where to target recent infections, identify “hot spots” of transmission, and other important trends. Interventions can be sensitive to the epidemiological context (risk behaviors and transmission patterns) in which they operate, so local epidemic drivers should be identified and understand [69]. It will be critical to avoid combining unproven with proven interventions, because the utility of any combination prevention package will be diluted if it becomes an unwieldy amalgam that includes non-evidence-based approaches. Behavioral strategies directly complementary to biomedical ones might gain the greatest synergy—eg, counseling accompanying circumcision, adherence promotion if PrEP or microbicides are found to be efficacious, and counseling and testing of HIV-discordant couples. Operational research demonstrating how best to select, combine, and scale up adherence to both behavioral and biomedical interventions will be useful.
Most study designs for evaluating the impact of a preventive approach on HIV incidence or prevalence have used randomized or quasi-experimental designs. However, not all interventions in a package can be randomized, and even in areas of high HIV burden, the size and duration required for a cluster randomized community-level trial may not be feasible to robustly assess an effect on HIV incidence. Furthermore, as with single-intervention study designs, the ethical mandate to deliver effective interventions such as free condoms, HIV risk reduction counseling, and STI treatment as the standard of care in control communities or populations likely reduces HIV incidence, making it more difficult to detect an intervention effect [17]. Because prevention programs cannot be delivered to all populations simultaneously, designs that make use of randomized rollout, such as stepped-wedge trials [70], can be considered. These have the advantage of allowing evaluation of prevention package effects under real-world program conditions, if feasible for interventions in which the effect on reducing HIV incidence is rapid enough to be measured in sequential steps.
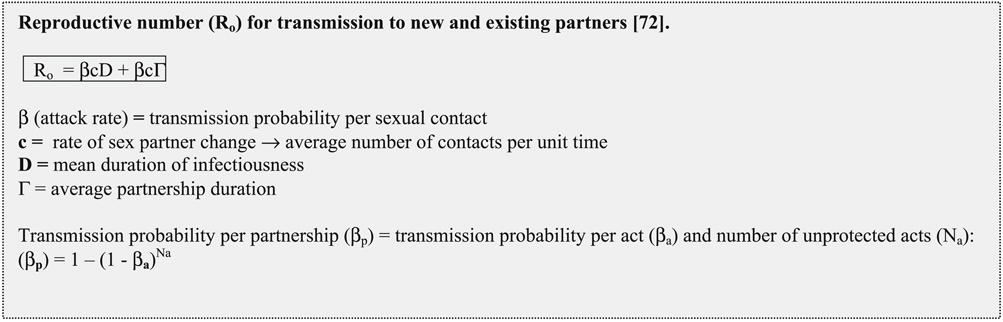
Advanced statistical analysis of the effect of combination prevention packages will be needed to help determine whether the constituent effects were synergistic or antagonistic, multiplicative or additive, and to determine the population attributable effect of the package on HIV spread. Mathematical modeling can serve as a virtual laboratory tool, with sensitivity analyses employed to assess the impact of specific parameters [71]. Innovative approaches such as tracking trends in HIV prevalence among young people may serve as a proxy for expensive incidence cohorts, and may help evaluate combination prevention programs that are rolled out using already collected public health surveillance data.
Conclusions
HIV prevention interventions have been identified that have proven, although partial efficacy. These strategies must be delivered in combination, strategically targeted to HIV-infected individuals and the most at-risk subpopulations, based on knowledge of local and regional HIV epidemiology and mathematical modeling. Combination HIV prevention represents the next generation of HIV prevention science. If designed and implemented effectively, it could stem the HIV epidemic. The move from observational and ecologic data through randomized trials to large-scale programs and policy should not take decades (as was the case for male circumcision as HIV prevention policy). Expanded access to HIV testing and consideration of ART as primary and secondary prevention as a “test and linkage to care” approach is innovative and potentially high impact. There is tremendous potential for synergy in providing populations with appropriately targeted combinations of this strategy together with scale-up of already established, efficacious interventions, such as male circumcision, STI treatment, and condoms. Delivery of effective combination prevention packages could represent a new era for HIV prevention and a turning point for the pandemic. Now is the time for the international community to commit the human, financial, and scientific resources to leverage these advances in partnership with communities.
Acknowledgments
Sources of support: This review was supported by NIH: NICHD grant 1R01 HD058363 (Kurth), NIAID 1RO1AI083034 (Celum, Baeten, Kurth, Wasserheit), and NIAID U01AI068619 (Vermund).
Footnotes
Disclosure No potential conflicts of interest relevant to this article were reported.
Contributor Information
Ann E. Kurth, Email: akurth@nyu.edu, New York University College of Nursing, 726 Broadway, 10th floor, New York, NY 10003, USA; Department of Global Health, University of Washington, Seattle, WA, USA.
Connie Celum, Department of Medicine, University of Washington, Seattle, WA, USA; Department of Global Health, University of Washington, Seattle, WA, USA.
Jared M. Baeten, Department of Medicine, University of Washington, Seattle, WA, USA Department of Global Health, University of Washington, Seattle, WA, USA.
Sten H. Vermund, Vanderbilt Institute for Global Health, Vanderbilt University School of Medicine, Nashville, TN, USA Department of Pediatrics, Vanderbilt University School of Medicine, Nashville, TN, USA.
Judith N. Wasserheit, Department of Medicine, University of Washington, Seattle, WA, USA Department of Global Health, University of Washington, Seattle, WA, USA.
References
Papers of particular interest, published recently, have been highlighted as:
•• Of major importance
- 1.WHO, UNAIDS: AIDS epidemic update: December 2009. Geneva, Switzerland: UNAIDS; 2009
- 2.Vermund SH. Rationale for the testing and use of a partially effective HIV vaccine. AIDS Res Hum Retroviruses. 1998;14 Suppl 3:S321–S323. [PubMed] [Google Scholar]
- 3.Vergidis PI, Falagas ME. Meta-analyses on behavioral interventions to reduce the risk of transmission of HIV. Infect Dis Clin North Am. 2009;23:309–314. doi: 10.1016/j.idc.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Johnson WD, et al. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev. 2008:CD001230. doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Herbst JH, et al. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. J Acquir Immune Defic Syndr. 2005;39:228–241. [PubMed] [Google Scholar]
- 6.Crepaz N, Marshall KJ, Aupont LW, et al. The efficacy of HIV/STI behavioral interventions for African American females in the United States: a meta-analysis. Am J Public Health. 2009;99:2069–2078. doi: 10.2105/AJPH.2008.139519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noar SM, Black HG, Pierce LB. Efficacy of computer technology-based HIV prevention interventions: a meta-analysis. AIDS. 2009;23:107–115. doi: 10.1097/QAD.0b013e32831c5500. [DOI] [PubMed] [Google Scholar]
- 8.Crepaz N, Horn AK, Rama SM, et al. The efficacy of behavioral interventions in reducing HIV risk sex behaviors and incident sexually transmitted disease in black and Hispanic sexually transmitted disease clinic patients in the United States: a meta-analytic review. Sex Transm Dis. 2007;34:319–332. doi: 10.1097/01.olq.0000240342.12960.73. [DOI] [PubMed] [Google Scholar]
- 9.Vergidis PI, Falagas ME, Hamer DH. Meta-analytical studies on the epidemiology, prevention, and treatment of human immunodeficiency virus infection. Infect Dis Clin North Am. 2009;23:295–308. doi: 10.1016/j.idc.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 10.Sturt AS, Dokubo EK, Sint TT. Antiretroviral therapy (ART) for treating HIV infection in ART-eligible pregnant women. Cochrane Database Syst Rev. 2010;3:CD008440. doi: 10.1002/14651858.CD008440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siegfried N, et al. Male circumcision for prevention of heterosexual acquisition of HIV in men. Cochrane Database Syst Rev. 2009;2:CD003362. doi: 10.1002/14651858.CD003362.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chigwedere P, Seage GR, Lee TH, Essex M. Efficacy of antiretroviral drugs in reducing mother-to-child transmission of HIV in Africa: a meta-analysis of published clinical trials. AIDS Res Hum Retroviruses. 2008;24:827–837. doi: 10.1089/aid.2007.0291. [DOI] [PubMed] [Google Scholar]
- 13.Denison JA, O’Reilly KR, Schmid GP, et al. HIV voluntary counseling and testing and behavioral risk reduction in developing countries: a meta-analysis, 1990–2005. AIDS Behav. 2008;12:363–373. doi: 10.1007/s10461-007-9349-x. [DOI] [PubMed] [Google Scholar]
- 14.Modjarrad K, Vermund SH. Effect of treating co-infections on HIV-1 viral load: a systematic review. Lancet Infect Dis. 2010;10:455–463. doi: 10.1016/S1473-3099(10)70093-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gowing L, et al. Substitution treatment of injecting opioid users for prevention of HIV infection. Cochrane Database Syst Rev. 2008;2:CD004145. doi: 10.1002/14651858.CD004145.pub3. [DOI] [PubMed] [Google Scholar]
- 16.Buvé A. Track C Epidemiology and Prevention Sciences Rapporteur Summary. XVIII International AIDS Conference; Vienna. IAS.2010. [Google Scholar]
- 17.Padian NS, McCoy SI, Balkus JE, Wasserheit JN. Weighing the gold in the gold standard: challenges in HIV prevention research. AIDS. 2010;24:621–635. doi: 10.1097/QAD.0b013e328337798a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Piot P, Bartos M, Larson H, et al. Coming to terms with complexity: a call to action for HIV prevention. Lancet. 2008;372:845–859. doi: 10.1016/S0140-6736(08)60888-0. This is a clarion call to utilize the available science and to mobilize an HIV prevention constituency that engages affected communities.
- 19.Holtgrave DR. Is the elimination of HIV infection within reach in the United States? Lessons from an epidemiologic transmission model. Public Health Rep. 2010;125:372–376. doi: 10.1177/003335491012500305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.UNAIDS Prevention Reference Group definition. From UNAIDS Taxonomy of HIV Prevention Activities. Discussion draft for UNAIDS HIV Prevention Reference Group meeting. 2009 March 2–4; [Google Scholar]
- 21.Wingood GM, DiClemente RJ. The ADAPT-ITT model: a novel method of adapting evidence-based HIV interventions. J Acquir Immune Defic Syndr. 2008;47 Suppl 1:S40–S46. doi: 10.1097/QAI.0b013e3181605df1. [DOI] [PubMed] [Google Scholar]
- 22.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Methods for Prevention Packages Program (MP3 II) (R01) [Accessed August 2010]; Available at: http://grants.nih.gov/grants/guide/rfa-files/RFA-AI-10-005.html.
- 24.Wilson D, Halperin DT. “Know your epidemic, know your response”: a useful approach, if we get it right. Lancet. 2008;372:423–426. doi: 10.1016/S0140-6736(08)60883-1. [DOI] [PubMed] [Google Scholar]
- 25.Vandenbruaene M. King Kennard Holmes—chair of the Department of Global Health of The University of Washington. Interviewed by Marc Vandenbruaene. Lancet Infect Dis. 2007;7:516–520. doi: 10.1016/S1473-3099(07)70184-6. [DOI] [PubMed] [Google Scholar]
- 26.Stoneburner RL, Low-Beer D. Sexual partner reductions explain human immunodeficiency virus declines in Uganda: comparative analyses of HIV and behavioural data in Uganda, Kenya, Malawi, and Zambia. Int J Epidemiol. 2004;33:624. doi: 10.1093/ije/dyh141. [DOI] [PubMed] [Google Scholar]
- 27.Blower SM, Gershengorn HB, Grant RM. A tale of two futures: HIV and antiretroviral therapy in San Francisco. Science. 2000;287:650–654. doi: 10.1126/science.287.5453.650. [DOI] [PubMed] [Google Scholar]
- 28. Granich RM, Gilks CF, Dye C, et al. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373:48–57. doi: 10.1016/S0140-6736(08)61697-9. This modeling exercise ignited debate regarding what might be possible for epidemic control if universal HIV testing, treatment, and adherence support were fully accessible.
- 29.Dodd PJ, Garnett GP, Hallett TB. Examining the promise of HIV elimination by ‘test and treat’ in hyperendemic settings. AIDS. 2010;24:729–735. doi: 10.1097/QAD.0b013e32833433fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, et al. Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N Engl J Med. 2009;361:2209–2220. doi: 10.1056/NEJMoa0908492. [DOI] [PubMed] [Google Scholar]
- 31.Korenromp EL, White RG, Orroth KK, et al. Determinants of the impact of sexually transmitted infection treatment on prevention of HIV infection: a synthesis of evidence from the Mwanza, Rakai, and Masaka intervention trials. J Infect Dis. 2005;191 Suppl 1:S168–S178. doi: 10.1086/425274. [DOI] [PubMed] [Google Scholar]
- 32.Allen S, Tice J, Van de Perre P, et al. Effect of serotesting with counselling on condom use and seroconversion among HIV discordant couples in Africa. BMJ. 1992;304:1605–1609. doi: 10.1136/bmj.304.6842.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bunnell R, Cherutich P. Universal HIV testing and counselling in Africa. Lancet. 2008;371:2148–2150. doi: 10.1016/S0140-6736(08)60929-0. [DOI] [PubMed] [Google Scholar]
- 34.Celum CL, Robinson NJ, Cohen MS. Potential effect of HIV type 1 antiretroviral and herpes simplex virus type 2 antiviral therapy on transmission and acquisition of HIV type 1 infection. J Infect Dis. 2005;191 Suppl 1:S107–S114. doi: 10.1086/425272. [DOI] [PubMed] [Google Scholar]
- 35.Bassett IV. Integrating HIV screening into routine health care in resource-limited settings. Clin Infect Dis. 2010;50 Suppl 3:S77–S84. doi: 10.1086/651477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khumalo-Sakutukwa G, et al. Project Accept (HPTN 043): a community-based intervention to reduce HIV incidence in populations at risk for HIV in sub-Saharan Africa and Thailand. J Acquir Immune Defic Syndr. 2008;49:422–431. doi: 10.1097/QAI.0b013e31818a6cb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weinhardt LS, et al. Effects of HIV counseling and testing on sexual risk behavior: a meta-analytic review of published research, 1985–1997. Am J Public Health. 1999;89:1397–1405. doi: 10.2105/ajph.89.9.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sherr L, Lopman B, Kakowa M, et al. Voluntary counselling and testing: uptake, impact on sexual behaviour, and HIV incidence in a rural Zimbabwean cohort. AIDS. 2007;21:851–860. doi: 10.1097/QAD.0b013e32805e8711. [DOI] [PubMed] [Google Scholar]
- 39.Corbett EL, Makamure B, Cheung YB, et al. HIV incidence during a cluster-randomized trial of two strategies providing voluntary counselling and testing at the workplace, Zimbabwe. AIDS. 2007;21:483–489. doi: 10.1097/QAD.0b013e3280115402. [DOI] [PubMed] [Google Scholar]
- 40.Huchko MJ, Montandon M, Nguti R, et al. The association of HIV counseling and testing with HIV risk behaviors in a random population-based survey in Kisumu, Kenya. AIDS Behav. 2009 Dec 11; doi: 10.1007/s10461-009-9649-4. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.WHO and UNICEF: Towards universal access: Scaling up priority HIV/AIDS interventions in the health sector: Progress report 2009. Geneva, Switzerland: WHO; 2009
- 42.Bunnell R, Ekwaru JP, Solberg P, et al. Changes in sexual behavior and risk of HIV transmission after antiretroviral therapy and prevention interventions in rural Uganda. AIDS. 2006;20:85–92. doi: 10.1097/01.aids.0000196566.40702.28. [DOI] [PubMed] [Google Scholar]
- 43.Sullivan P, et al. 5th IAS. Cape Town, SA: 2009. Is the reduction of HIV transmission risk while prescribed antiretroviral therapy (ARVT) different for men and women? Results from discordant couples in Rwanda and Zambia. [Google Scholar]
- 44.Donnell D, Baeten JM, Kiarie J, et al. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375:2092–2098. doi: 10.1016/S0140-6736(10)60705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Attia S, Egger M, Müller M, et al. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23:1397–1404. doi: 10.1097/QAD.0b013e32832b7dca. [DOI] [PubMed] [Google Scholar]
- 46.Montaner J, Wood E, Kerr T, et al. Association of expanded HAART coverage with a decrease in new HIV diagnoses, particularly among injection drug users in British Columbia, Canada [Paper 88LB]. Presented at the 17th Conference on Retroviruses and Opportunistic Infections; San Francisco, CA. February 16–19, 2010. [Google Scholar]
- 47.Das-Douglas M, Chu, Santos GM, et al. Decreases in community viral load are associated with a reduction in new HIV diagnoses in San Francisco [Paper #33]; Presented at the 17th Conference on Retroviruses and Opportunistic Infections; San Francisco, CA. February 16–19, 2010. [Google Scholar]
- 48.Kalichman SC, Di Berto G, Eaton L. Human immunodeficiency virus viral load in blood plasma and semen: review and implications of empirical findings. Sex Transm Dis. 2008;35:55–60. doi: 10.1097/olq.0b013e318141fe9b. [DOI] [PubMed] [Google Scholar]
- 49.Amico KR, Harman JJ, Johnson BT. Efficacy of antiretroviral therapy adherence interventions: a research synthesis of trials, 1996 to 2004. J Acquir Immune Defic Syndr. 2006;41:285–297. doi: 10.1097/01.qai.0000197870.99196.ea. [DOI] [PubMed] [Google Scholar]
- 50.Simoni JM, et al. Efficacy of interventions in improving highly active antiretroviral therapy adherence and HIV-1 RNA viral load. A meta-analytic review of randomized controlled trials. J Acquir Immune Defic Syndr. 2006;43 Suppl 1:S23–S35. doi: 10.1097/01.qai.0000248342.05438.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.WHO: Rapid advice: antiretroviral therapy for HIV infection in adults and adolescents. Geneva, Switzerland: WHO;
- 52.Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 2004;82:454–461. [PMC free article] [PubMed] [Google Scholar]
- 53.Johnson BT, et al. Sexual risk reduction for persons living with HIV: research synthesis of randomized controlled trials, 1993 to 2004. J Acquir Immune Defic Syndr. 2006;41:642–650. doi: 10.1097/01.qai.0000194495.15309.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crepaz N, Lyles CM, Wolitski RJ, et al. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20:143–157. doi: 10.1097/01.aids.0000196166.48518.a0. [DOI] [PubMed] [Google Scholar]
- 55.Horvath T, et al. Interventions for preventing late postnatal mother-to-child transmission of HIV. Cochrane Database Syst Rev. 2009:CD006734. doi: 10.1002/14651858.CD006734.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Des Jarlais DC, Marmor M, Paone D, et al. HIV incidence among injecting drug users in New York City syringe-exchange programmes. Lancet. 1996;348:987–991. doi: 10.1016/s0140-6736(96)02536-6. [DOI] [PubMed] [Google Scholar]
- 57.Copenhaver MM, Johnson BT, Lee IC, et al. Behavioral HIV risk reduction among people who inject drugs: meta-analytic evidence of efficacy. J Subst Abuse Treat. 2006;31:163–171. doi: 10.1016/j.jsat.2006.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Malta M, Magnanini MM, Strathdee SA, Bastos FI. Adherence to antiretroviral therapy among HIV-infected drug users: a meta-analysis. AIDS Behav. 2008;14:731–747. doi: 10.1007/s10461-008-9489-7. [DOI] [PubMed] [Google Scholar]
- 59.Vermund SH, et al. Addressing research priorities for prevention of HIV infection in the United States. Clin Infect Dis. 2010;50 Suppl 3:S149–S155. doi: 10.1086/651485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zachariah R, Harries AD, Philips M, et al. Antiretroviral therapy for HIV prevention: many concerns and challenges, but are there ways forward in sub-Saharan Africa? Trans R Soc Trop Med Hyg. 2010;104:387–391. doi: 10.1016/j.trstmh.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 61.McCoy SI, Kangwende RA, Padian NS. Behavior change interventions to prevent HIV infection among women living in low and middle income countries: a systematic review. AIDS Behav. 2010;14:469–482. doi: 10.1007/s10461-009-9644-9. [DOI] [PubMed] [Google Scholar]
- 62. Karim QA, Karim SS, Frohlich JA, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010 Jul 19; doi: 10.1126/science.1193748. (Epub ahead of print) This is the first evidence that a topically applied (ART-containing) microbicide can provide protection from HIV among at-risk women: 1% tenofovir gel reduced HIV acquisition by an estimated 39% overall and by 54% in women with high gel adherence.
- 63.Mills E, Cooper C, Anema A, Guyatt G. Male circumcision for the prevention of heterosexually acquired HIV infection: a metaanalysis of randomized trials involving 11,050 men. HIV Med. 2008;9:332–335. doi: 10.1111/j.1468-1293.2008.00596.x. [DOI] [PubMed] [Google Scholar]
- 64.Weiss HA, Hankins CA, Dickson K. Male circumcision and risk of HIV infection in women: a systematic review and meta-analysis. Lancet Infect Dis. 2009;9:669–677. doi: 10.1016/S1473-3099(09)70235-X. [DOI] [PubMed] [Google Scholar]
- 65.Grosskurth H, Mosha F, Todd J, et al. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: randomised controlled trial. Lancet. 1995;346:530–536. doi: 10.1016/s0140-6736(95)91380-7. [DOI] [PubMed] [Google Scholar]
- 66.Ozler B, et al. Cash payments can reduce HIV/STIs in Africa—New Bank studies; News release No. 2011//027/HDN, at IAS Meeting; Vienna. July 18, 2010. [Google Scholar]
- 67.Merson M, Padian N, Coates TJ, et al. Combination HIV prevention. Lancet. 2008;372:1805–1806. doi: 10.1016/S0140-6736(08)61752-3. [DOI] [PubMed] [Google Scholar]
- 68.Buse K, Dickinson C, Sidibe M. HIV: know your epidemic, act on its politics. J R Soc Med. 2008;101:572–573. doi: 10.1258/jrsm.2008.08k036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grassly NC, Garnett GP, Schwartländer B, et al. The effectiveness of HIV prevention and the epidemiological context. Bull World Health Organ. 2001;79:1121–1132. [PMC free article] [PubMed] [Google Scholar]
- 70.Hughes JP, Kulich M. Cluster randomized trials for HIV prevention. Curr Opin HIV AIDS. 2006;1:471–475. doi: 10.1097/01.COH.0000247387.00862.5f. [DOI] [PubMed] [Google Scholar]
- 71.DeGruttola V, et al. Developing and evaluating comprehensive HIV infection control strategies: issues and challenges. Clin Infect Dis. 2010;50 Suppl 3:S102–S107. doi: 10.1086/651480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Anderson RM. Transmission dynamics of sexually transmitted infections. In: Holmes K, Sparling PF, Mardh PA, et al., editors. Sexually Transmitted Diseases. edn 3. New York: McGraw-Hill; 1998. [Google Scholar]
- 73.Kurth A, Spielberg F. Individual-level risk assessment for STD/HIV infection. In: Holmes K, Sparling PF, Stamm W, et al., editors. Sexually Transmitted Diseases. edn 4. New York: McGraw-Hill; 2008. [Google Scholar]


