Abstract
Aim:
The aim of this study is to determine the current trends in the management and surveillance of the NB population secondary to spinal cord injury (SCI) or myelomeningocele by certified urologist working in Saudi Arabia and to compare it to the current guidelines.
Materials and Methods:
A cross-sectional study was conducted using a 12-points questionnaire distributed to urologists working in Saudi Arabia and registered at the Saudi medical association. The assessment and follow-up of upper and lower urinary tract function in neurogenic bladder patients, their optimal frequency and management of related infections were the topics of inquiry.
Results:
Of the 272 urologists surveyed, 105 responded, yielding a response rate of 38%. Eighty-nine percent of respondents said that ultrasound was their diagnostic tool of choice for upper tract evaluation. Sixty-one percent of respondents said that they would follow their patients with a multichannel urodynamic study. Forty percent of urologists stated that they would treat asymptomatic bacteriuria. Clean intermittent catheterization (CIC) was the most common modality chosen for the management of neurogenic bladder in patients with emptying difficulties.
Conclusion:
This study confirms that most urologists in Saudi Arabia involved with neurogenic bladder management. However, more than one third of the urologists do not have urodynamic machine and only two of the reporting practitioners has a videourodynamic machine. The results emphasize the need for clear guidelines in this field of urology in Saudi Arabia. Highly specialized rehabilitation centers for neurogenic bladder secondary to SCI are required for optimal care and urologist teaching.
Keywords: Spinal cord injury, neurogenic bladder, urologists, Saudi Arabia
INTRODUCTION
As healthcare delivery has recently improved in Saudi Arabia and worldwide, life expectancy after spinal cord injury (SCI) has increased. Living with a disability becomes a fact for many SCI patients, with different problems presenting at different stages in life.
The management of neurogenic bladder (NB) and voiding dysfunction is an important issue in rehabilitation programs for SCI because it affects the morbidity of patients.[1] In a study by the Model Spinal Cord Injury Systems of Care, 81% of patients had some degree of impaired bladder function at one year after injury.[2] The impairment of bladder function in patients with SCI results in a high risk of urinary tract deterioration, which increases morbidity and occasionally increases mortality.[3]
The urological complications of NB consist of an inability to empty the bladder, as well as urinary tract infections (UTIs), incontinence, and upper tract deterioration. The principal goals of managing NB are preservation of renal function and prevention of renal failure. This is achieved via low pressure filling and emptying, combined with minimal residual. The most appropriate methods of bladder management should be implemented based on the findings of a previous urodynamic study.[4] Various approaches to managing urinary disorders have been developed in recent years, and different therapies have become available, ranging from the ingestion of active drugs, as well as the use of clean intermittent catheterization (CIC) and the insertion of endourethral prosthetic devices to surgery.
Urologists who manage SCI patients with NB were surveyed in many countries.[5,6] Surveyed consultant urologists in spinal injuries units in the UK and Ireland with regard to different aspects of NB and voiding dysfunction. In that study, the frequency of visits, protocols for urinary tract infections, and the need for routine urodynamics were the subjects of debate. Blok et al. surveyed Canadian urologists on their management of NB;[8] however, the response rate was low. Methods for evaluating the lower urinary tract and the treatment of symptomatic urinary tract infections were the subjects of debate.
The aim of this study is to determine the current trends in the management and surveillance of the NB population secondary to SCI by urologists working in Saudi Arabia and registered at the Saudi medical council.
MATERIALS AND METHODS
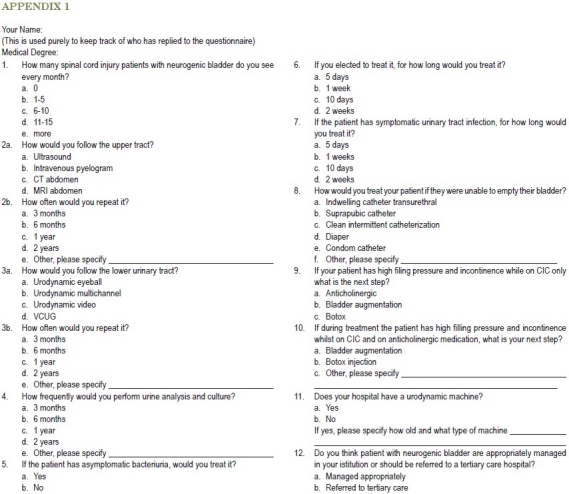
A cross-sectional study was conducted using a 12-points questionnaire [Appendix I] emailed, mailed or faxed to 272 urologists practicing in Saudi Arabia in secondary and tertiary health care facilities. The assessment and follow-up of upper and lower urinary tract function in NB patients, their optimal management of related infections, and common management modalities for NB patients were the topics of inquiry. The survey was undertaken on a voluntary and anonymous basis. No direct patient information was released, and responses were received as return documents.
APPENDIX I.
RESULTS
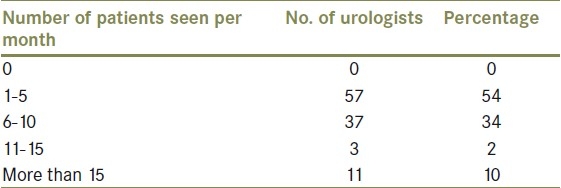
Of the 272 urologists surveyed, 105 responded, yielding a response rate of 38%. Of the respondents, 54% saw one to five NB patients per month, while only 10% saw more than 15 patients per month [Table 1].
Table 1.
Number of neurogenic bladder patients seen by urologists per month
Upper tract evaluation
Eighty-nine percent (n=94) of respondents believed that upper tract ultrasound was the diagnostic tool of choice for routine surveillance of the upper tracts. Eleven percent favored intravenous urograms (IVUs) instead of a renal ultrasound. Computed tomography (CT) scans and magnetic resonance imaging (MRI) were not chosen by any of the respondents. Sixty percent of the respondents planned to repeat their diagnostic study in every six months, while 30 and 10 % planned to do it in every one and two years, respectively.
Lower tract evaluation
With respect to the lower urinary tract, 61% (n=64) of respondents plan to follow their patients with a multichannel urodynamic study, while 34% (n=25) will perform a voiding cystourethrogram (VCUG). Five percents will perform videourodynamics. Sixty-two percent (n=65) will repeat the study every year. The remaining 20% will do it in every two years, and 12% will do it whenever the patients′ symptoms deteriorate. Moreover, 38% of respondents reported that they do not have a urodynamic machine, and two of them had videourodynamics.
Urinary tract infection
Urinalysis was performed by respondents in every three months, six months, one year and two years by 20, 14, 56 and 10% of physicians, respectively. Forty percent (n = 42) of respondents said that they would treat asymptomatic bacteriuria. Symptomatic urinary tract infection (UTIs) would be treated for 5, 7, 10, and 14 days by 20, 33, 17 and 30% of respondents, respectively.
Management
CIC was the most common modality for managing NB in patients with emptying difficulties (90%, or n=94), whereas 85% of respondents plan to add anticholenergic medications to CIC if intravesicle pressures remain high (due to neurogenic detrusor overactivity) after the use of CIC alone. After failure of CIC and anticholoenergics, physicians used Botox injections (43%), bladder augmentation (50%), and Sphincterotomy (7%). Of the respondents, 52% think that they appropriately manage their patients, and 48% think that they should refer their patients to a tertiary care hospital.
DISCUSSION
SCI and voiding dysfunction are closely related, and the follow-up of neurogenic bladder patients is traditionally focused on the prevention of upper tract deterioration and maintaining the quality of life.
Response rate to the survey by Razdan et al.[7] and Kitahara et al.[5] were 60 and 43.2%. In contrast, Blok et al.[8] had a 15% response rate among members of the Canadian Urology Association; however, in this study, urologists from all over Saudi Arabia were asked to complete a survey [Appendix I], and 105 responded, for a response rate of 38%.
Linsenmeyer and Culkin[9] reported the neurologic care of SCI patients in the American Paraplegic Society (APS) Guidelines on urologic care of SCI patients. Annual follow-up including evaluation of upper and lower tract is recommended for the first 5 to 10 years after the injury. If the patient is doing well, then follow-up in every other year is acceptable. However, Burns et al.[10] recommended at least plain films and nuclear renal scans. However, the decrease of more than 20% in renal plasma flow warrants further investigation.
Concerning the evaluation of the upper urinary tract, 89% of our respondents performed an ultrasound examination, with 60% reporting that they would do it in every six months. In Japan,[5] 71.8% reported using ultrasound. Eighty-five percent of Americans will perform an ultrasound examination every year.[7] In contrast, IVU was utilized by 25.8% of responders in Japan, while in Saudi Arabia, 11% said that they would utilize IVU as the initial diagnostic modality. The reason underlying the frequent use of ultrasound is the wide availability of ultrasound in comparison to other radiological investigations. It is recommended to evaluate the upper tract in every six months by ultrasound.[11]
The European Association of Urology (EAU) guidelines[11] advise physicians to classify patients with neurological lesions in low and high-risk bladder categories on the basis of their filling cystometry and pressure flow studies, which should be repeated in every one-two years or when patient's condition deteriorate. Urodynamic evaluation was recommended by the APS at the same intervals as upper and lower tract screening. Cystoscopy was recommended annually for those patients with an indwelling catheter.[9] Regarding the evaluation of the lower urinary tract (LUT), 61% of respondents performed multichannel urodynamic examination in Saudi Arabia, with 65% of respondents saying that they plan to re-evaluate their patients annually, and with only 5% including a videourodynamic examination. In Japan,[5] more than half of the respondents (52.3%) use cystometry, and only 9.9% use videourodynamic techniques. In the USA, 65% of respondents performed a videourodynamic examination.[7] However, 35% of USA respondents examined their patients only when the patients had repeated UTIs or when an abnormality was found in a renal scintigram or ultrasound.[7] Watanabe et al.[4] reported that the most appropriate method of bladder management should be implemented on the basis of urodynamic studies. However, in this study, we found that 38% of respondents do not have a urodynamic study machine and only two have videourodynamic machines. This may be due to lack of resources and/or lack of experts operating urodynamic machines.
UTIs are one of the important causes of morbidity,[12,13] and they are the most frequent complication in patients with SCI.[14] Asymptomatic bacteriuria reaches prevalence rates of up to 70% in SCI patients undergoing CIC.[15] Factors increasing the risk of infection include over-distention of the bladder, vesico-ureteric reflux, high pressure voiding, large post-void residuals and stones in the urinary tract.[16] Antiseptics have not demonstrated efficacy in preventing UTI in SCI patients.[17] Urinalysis should be performed in every two months.[21] In our study, 40% of respondents said that they treat asymptomatic bacteriuria. Bycroft[6] found that only one unit treated asymptomatica bacteriuria in patients with permanent indwelling catheters. Dutch[18] and Canadian[8] urologists rarely treat asymptomatic urinary tract infections in CIC. The Infectious Disease Society of America (IDSA)[19] does not recommend screening and treatment of asymptomatic bacteriuria since reinfection strains show increased antimicrobial resistance. When 52 patients with a relatively recent onset of SCI were observed prospectively for 4-26 weeks, 78% of weekly urine cultures were positive, but only six symptomatic episodes occurred, all of which responded promptly to antimicrobial treatment.[20] Symptomatic LUT infections were treated for seven-nine days on average by Dutch urologists,[18] while most of our respondents said that they treat the patients for 7 to 14 days. However, the EAU guidelines recommend 7-10 days of treatment for a symptomatic UTI.[21]
For the treatment of NB, CIC was the most common modality for managing patients with emptying difficulties (90%, or n =94), whereas 85% of surveyed participants said that they would add an anticholenergic drug to CIC if intravesicle pressure remained high or the patient remained incontinent due to detrusor overactivity after the use of CIC alone. This is comparable to American respondents, 84% of whom said that they would use a combination of anticholinergic agent(s) with CIC for the treatment of NB overactivity. EAU guidelines recommend anticholenergic drugs for patients with detrusor overactivity, and intermittent catheterization as the first line management for patients who are unable to empty their bladder.[11]
Our study is limited by the low response rate from the urologist; however, majority of the urologists in our study involved with neurogenic bladder management. We strongly recommend that the urologists in Saudi Arabia need to follow a clear guideline in neurogenic bladder management to optimize patient care, and urodynamic machine should be available in every urology department to cover the demand of this investigation to treat this kind of patients.
CONCLUSION
This study confirms that most urologists in Saudi Arabia involved with neurogenic bladder management. However, more than one third of the urologists do not have urodynamic machine and only two of the reporting practitioners has a videourodynamic machine. The results emphasize the need for clear guidelines in this field of urology in Saudi Arabia. The presence of urodynamic machines and training of technicians and urologists to operate them are necessary for effective management of neurogenic bladder in SCI patients; however, highly specialized rehabilitation centers for SCI patients are required for optimal care and teaching.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Frankel HL, Coll JR, Charlifue SW, Whiteneck GG, Gardner BP, Jamous MA, et al. Long-term survival in spinal cord injury: a fifty year investigation. Spinal Cord. 1998;36:266–74. doi: 10.1038/sj.sc.3100638. [DOI] [PubMed] [Google Scholar]
- 2.Stover SL, De Lisa JA, Whiteneck GG. Gaithersburg, Maryland: Aspen Publishers; 1995. Spinal cord injury: Clinical outcomes from the model systems; p. 234. [Google Scholar]
- 3.Menon EB, Tan ES. Bladder training in patients with spinal cord injury. Urology. 1992;40:425–9. doi: 10.1016/0090-4295(92)90456-7. [DOI] [PubMed] [Google Scholar]
- 4.Watanabe T, Rivas DA, Chancellor MB. Urodynamics of spinal cord injury. Urol Clin North Am. 1996;23:459–73. doi: 10.1016/s0094-0143(05)70325-6. [DOI] [PubMed] [Google Scholar]
- 5.Kitahara S, Iwatsubo E, Yasuda K, Ushiyama T, Nakai H, Suzuki T, et al. Practice patterns of Japanese physicians in urologic surveillance and management of spinal cord injury patients. Spinal Cord. 2006;44:362–8. doi: 10.1038/sj.sc.3101854. [DOI] [PubMed] [Google Scholar]
- 6.Bycroft J, Hamid R, Bywater H, Patki P, Craggs M, Shah J. Variation in urological practice among spinal injuries units in the UK and Eire. Neurourol Urodyn. 2004;23:252–7. doi: 10.1002/nau.20005. [DOI] [PubMed] [Google Scholar]
- 7.Razdan S, Leboeuf L, Meinbach DS, Weinstein D, Gousse AE. Current practice patterns in the urologic surveillance and management of patients with spinal cord injury. Urology. 2003;61:893–6. doi: 10.1016/s0090-4295(02)02518-9. [DOI] [PubMed] [Google Scholar]
- 8.Blok BF, Karsenty G, Corsos J. Urological surveillance and management of patients with neurogenic bladder: Results of a survey among practicing urologists in Canada. Can J Urol. 2006;13:3239–43. [PubMed] [Google Scholar]
- 9.Linsenmeyer TA, Culkin D. APS recommendations for the urological evaluation of patients with spinal cord injury. J Spinal Cord Med. 1999;22:139–42. doi: 10.1080/10790268.1999.11719561. [DOI] [PubMed] [Google Scholar]
- 10.Burns AS, Rivas DA, Ditunno JF. The management of neurogenic bladder and sexual dysfunction after spinal cord injury. Spine. 2001;26:129–36. doi: 10.1097/00007632-200112151-00022. [DOI] [PubMed] [Google Scholar]
- 11.European Association of Urology. Guidelines on neurogenic lower urinary tract dysfunction. 2009. http://www.campbellsurology.com/storedfiles//15.%20Neurogenic%20Lower%20Urinary%20Tract%20Dysfuntion.pdf?CFID=1971148andCFTOKEN=68113474. [DOI] [PubMed]
- 12.Garcia Leoni ME, Esclarin de Ruz A. Management of urinary tract infection in patients with spinal cord injuries. Clin Microbiol Infect. 2003;9:780–5. doi: 10.1046/j.1469-0691.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- 13.De Ridder DJ, Everaert K, Fernández LG, Valero JV, Durán AB, Abrisqueta ML, et al. Intermittent catheterization with hydrophilic-coated catheters reduces the risk of clinical urinary tract infection in spinal cord injured patients: a prospective randomized parallel comparative trial. Eur Urol. 2005;48:991–5. doi: 10.1016/j.eururo.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 14.Cardenas DD, Hooton TM. Urinary tract infections in persons with spinal cord injury. Arch Phys Med Rehabil. 1995;76:272–80. doi: 10.1016/s0003-9993(95)80615-6. [DOI] [PubMed] [Google Scholar]
- 15.Reid G, Nicolle LE. Asymptomatic bacteriuria in spinal cord patients and the elderly. Urol Clin North Am. 1999;26:789–95. doi: 10.1016/s0094-0143(05)70219-6. [DOI] [PubMed] [Google Scholar]
- 16.Esclarin de Ruz A, Garcia Leoni E, Herruzo Cabrera R. Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J Urol. 2000;164:1285–9. [PubMed] [Google Scholar]
- 17.Agency for Health Care Policy and Research. Prevention and management of urinary tract infections in paralyzed persons. [accessed on 2006 January 1]. http://www.ahcpr.gov/clinic/epsums/utisumm.htm .
- 18.Rikken B, Blok BF. Management of neurogenic bladder patients in the Netherlands: Do urologists follow guidelines? Neurourol Urodyn. 2008;27:758–62. doi: 10.1002/nau.20582. [DOI] [PubMed] [Google Scholar]
- 19.Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Infectious diseases society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40:643–54. doi: 10.1086/427507. [DOI] [PubMed] [Google Scholar]
- 20.Lewis RI, Carrion HM, Lockhart JL, Politano VA. Significance of asymptomatic bacteriuria in neurogenic bladder disease. Urol. 1984;23:343–7. doi: 10.1016/0090-4295(84)90136-5. [DOI] [PubMed] [Google Scholar]
- 21.European Association of Urology; 2009 http://www.campbellsurology? Urological Infections guideline. 2009. http://www.campbellsurology.com/storedfiles//07.%20Urological%20Infections.pdf?CFID=1971148andCFTOKEN=68113474 .


